Urinary Aflatoxin M1 Concentration and Its Determinants in School-Age Children in Southern Ethiopia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Description of Study Area and Population
2.2. Study Design
2.3. Questionnaire
2.4. Urinary AFM1 and Creatinine Measurements
3. Statistical Analysis
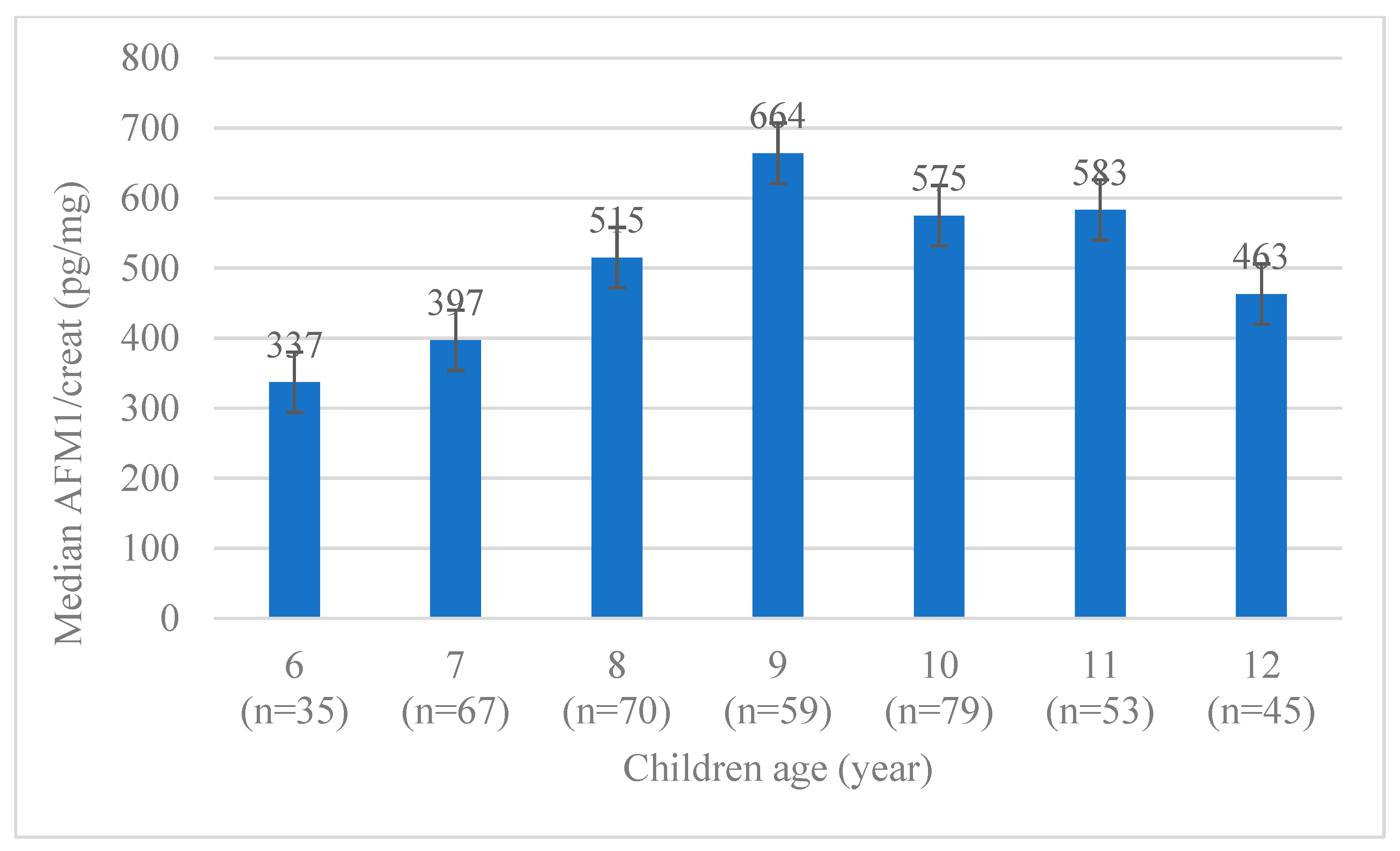
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Frisvad, J.; Skouboe, P.; Samson, R.A. Taxonomic comparison of three different groups of aflatoxin producers and a new efficient producer of aflatoxin B1, sterigmatocystin and 3-O-methylsterigmatocystin, Aspergillus rambellii sp. nov. Syst. Appl. Microbiol. 2005, 28, 442–453. [Google Scholar] [CrossRef] [PubMed]
- Strosnider, H.; Azziz-Baumgartner, E.; Banziger, M.; Bhat, R.V.; Breiman, R.; Brune, M.-N.; DeCock, K.; Dilley, A.; Groopman, J.; Hell, K.; et al. Workgroup Report: Public Health Strategies for Reducing Aflatoxin Exposure in Developing Countries. Environ. Health Perspect. 2006, 114, 1898–1903. [Google Scholar] [CrossRef] [PubMed]
- Coulombe, R.A. Aflatoxins. In Mycotoxins and Phytoalexins; Sharma, R.P., Salunkhe, D.K., Eds.; CRC Press: Boca Raton, FL, USA, 1991; pp. 103–143. ISBN 0849388333. [Google Scholar]
- Khlangwiset, P.; Shephard, G.S.; Wu, F. Aflatoxins and growth impairment: A review. Crit. Rev. Toxicol. 2011, 41, 740–755. [Google Scholar] [CrossRef] [PubMed]
- Mahfuz, M.; Alam, M.A.; Fahim, S.M.; Gazi, M.A.; Raihan, M.J.; Hossain, M.; Egner, P.A.; Bessong, P.O.; Petri, W.A.; Groopman, J.D.; et al. Aflatoxin exposure in children living in Mirpur, Dhaka: Data from MAL-ED companion study. J. Expo. Sci. Environ. Epidemiol. 2019, 29, 655–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chauhan, Y.S.; Wright, G.C.; Rachaputi, N.C. Modelling climatic risks of aflatoxin contamination in maize. Aust. J. Exp. Agric. 2008, 48, 358–366. [Google Scholar] [CrossRef]
- Wild, C.P.; Yin, F.; Turner, P.C.; Chemin, I.; Chapot, B.; Mendy, M.; Whittle, H.; Kirk, G.D.; Hall, A.J. Environmental and genetic determinants of aflatoxin-albumin adducts in The Gambia. Int. J. Cancer 2000, 86, 1–7. [Google Scholar] [CrossRef]
- Leroy, J.L.; Wang, J.-S.; Jones, K. Serum aflatoxin B1-lysine adduct level in adult women from Eastern Province in Kenya depends on household socio-economic status: A cross sectional study. Soc. Sci. Med. 2015, 146, 104–110. [Google Scholar] [CrossRef]
- Liu, Y.; Wu, F. Global Burden of Aflatoxin-Induced Hepatocellular Carcinoma: A Risk Assessment. Environ. Health Perspect. 2010, 118, 818–824. [Google Scholar] [CrossRef] [Green Version]
- Zhu, J.Q.; Zhang, L.S.; Hu, X.; Xiao, Y.; Chen, J.S.; Xu, Y.C.; Fremy, J.; Chu, F.S. Correlation of dietary aflatoxin B1 levels with excretion of aflatoxin M1 in human urine. Cancer Res. 1987, 47, 1848–1852. [Google Scholar]
- Tchana, A.N.; Moundipa, P.F.; Tchouanguep, F.M. Aflatoxin Contamination in Food and Body Fluids in Relation to Malnutrition and Cancer Status in Cameroon. Int. J. Environ. Res. Public Health 2010, 7, 178–188. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. Agents Classified by the IARC Monographs; World Health Organization: Geneva, Switzerland, 2010; Volumes 1–100. [Google Scholar]
- Wielogorska, E.; Mooney, M.H.; Eskola, M.; Ezekiel, C.N.; Stranska, M.; Krska, R.; Elliott, C.T. Occurrence and Human-Health Impacts of Mycotoxins in Somalia. J. Agric. Food Chem. 2019, 67, 2052–2060. [Google Scholar] [CrossRef] [PubMed]
- Mupunga, I.; Mngqawa, P.; Katerere, D.R. Peanuts, Aflatoxins and Undernutrition in Children in Sub-Saharan Africa. Nutrients 2017, 9, 1287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lauer, J.M.; Duggan, C.P.; Ausman, L.M.; Griffiths, J.K.; Webb, P.; Wang, J.; Xue, K.S.; Agaba, E.; Nshakira, N.; Ghosh, S. Maternal aflatoxin exposure during pregnancy and adverse birth outcomes in Uganda. Matern. Child Nutr. 2019, 15, 12701. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yenasew, A. Aflatoxin Contamination Level of Different Crops in Ethiopia. Int. J. Bioorg. Chem. 2019, 4, 42–46. [Google Scholar] [CrossRef]
- Eshete, M.; Gebremedhin, S.; Alemayehu, F.R.; Taye, M.; Boshe, B.; Stoecker, B.J. Aflatoxin contamination of human breast milk and complementary foods in southern Ethiopia. Matern. Child Nutr. 2021, 17, 13081. [Google Scholar] [CrossRef]
- Gizachew, D.; Szonyi, B.; Tegegne, A.; Hanson, J.; Grace, D. Aflatoxin contamination of milk and dairy feeds in the Greater Addis Ababa milk shed, Ethiopia. Food Control 2016, 59, 773–779. [Google Scholar] [CrossRef]
- Zewdie, E.; Sivakumar, S. Determinants of off farm participation of rural farm households in Shebedino district of Sidama zone, southern Ethiopia. Int. J. Dev. Res. 2017, 7, 15157–15165. [Google Scholar]
- Elias, E.; Tsegaye, W.; Stoecker, B.J.; Gebreegziabher, T. Excessive intake of iodine and low prevalence of goiter in school age children five years after implementation of national salt iodization in Shebedino woreda, southern Ethiopia. BMC Public Health 2021, 21, 165. [Google Scholar] [CrossRef]
- CSA; ICF. Ethiopia Demographic and Health Survey 2011; Central Statistical Agency: Addis Ababa, Ethiopia; ICF International: Calverton, MD, USA, 2012. [Google Scholar]
- Gibson, R.S. Principles of Nutritional Assessment, 2nd ed.; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Coates, J.; Swindale, A.; Blinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Household Food Access: Indicator Guide (v.3); Food and Nutrition Technical Assistance Project, Academy for Educational Development: Washington, DC, USA, 2007. [Google Scholar]
- FAO. Guidelines for Measuring Household and Individual Dietary Diversity; FAO: Rome, Italy, 2011. [Google Scholar]
- Ayelign, A.; Woldegiorgis, A.Z.; Adish, A.; de Boevre, M.; Heyndrickx, E.; de Saeger, S. Assessment of aflatoxin exposure among young children in Ethiopia using urinary biomarkers. Food Addit. Contam. 2017, 34, 1606–1616. [Google Scholar] [CrossRef]
- Boshe, B.; Gebremedhin, S.; Alemayehu, F.; Eshete, M.; Taye, M.; Stoecker, B.J. Aflatoxin exposure among lactating women in southern Ethiopia. Food Sci. Nutr. 2020, 8, 6738–6745. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. Mycotoxin Control in Low- and Middle-Income Countries; IARC Working Group Report; International Agency for Research on Cancer: Lyon, France, 2015; ISBN 9789283225102. [Google Scholar]
- Schleicher, R.L.; McCoy, L.F.; Powers, C.D.; Sternberg, M.R.; Pfeiffer, C.M. Serum concentrations of an aflatoxin-albumin adduct in the National Health and Nutrition Examination Survey (NHANES) 1999–2000. Clin. Chim. Acta 2013, 423, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Chang, C.-C.H.; Marsh, G.M.; Wu, F. Population attributable risk of aflatoxin-related liver cancer: Systematic review and meta-analysis. Eur. J. Cancer 2012, 48, 2125–2136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, N.; Hossain, K.; Blaszkewicz, M.; Rahman, M.; Mohanto, N.C.; Alim, A.; Degen, G.H. Occurrence of aflatoxin M1 in urines from rural and urban adult cohorts in Bangladesh. Arch. Toxicol. 2016, 90, 1749–1755. [Google Scholar] [CrossRef]
- Wangia-Dixon, R.N.; Quach, T.H.T.; Song, X.; Ombaka, J.; Githanga, D.P.; Anzala, O.A.; Wang, J.-S. Determinants of aflatoxin exposures in Kenyan School-aged children. Int. J. Environ. Health Res. 2022, 32, 1183–1191. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, S.H.; Jamaluddin, R.; Sabran, M.R. Association between urinary aflatoxin (AFM₁) and dietary intake among adults in hulu langat district, Selangor, Malaysia. Nutrients 2018, 10, 460. [Google Scholar] [CrossRef] [Green Version]
- Ephrem, G. Implication of aflatoxin contamination in agricultural products. Am. J. Food Nutr. 2015, 3, 12–20. [Google Scholar]
- Jaiswal, P.; Jha, S.N.; Kaur, J.; Borah, A.; Ramya, H.G. Detection of aflatoxin M1 in milk using spectroscopy and multivariate analyses. Food Chem. 2018, 238, 209–214. [Google Scholar] [CrossRef]
- Mohammed, S.; Munissi, J.J.E.; Nyandoro, S.S. Aflatoxin M1 in raw milk and aflatoxin B1 in feed from household cows in Singida, Tanzania. Food Addit. Contam. 2016, 9, 85–90. [Google Scholar] [CrossRef]
- Kang’Ethe, E.K.; Lang’a, K.A. Aflatoxin B1 and M1 contamination of animal feeds and milk from urban centers in Kenya. Afr. Health Sci. 2009, 9, 218–226. [Google Scholar]
- Sahin, H.Z.; Celik, M.; Kotay, S.; Kabak, B. Aflatoxins in dairy cow feed, raw milk and milk products from Turkey. Food Addit. Contam. 2016, 9, 152–158. [Google Scholar] [CrossRef]
- Sugiyama, K.-I.; Hiraoka, H.; Sugita-Konishi, Y. Aflatoxin M1 Contamination in Raw Bulk Milk and the Presence of Aflatoxin B1 in Corn Supplied to Dairy Cattle in Japan. J. Food Hyg. Soc. Jpn. 2008, 49, 352–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tadesse, S.; Berhanu, T.; Woldegiorgis, A.Z. Aflatoxin M1 in milk and milk products marketed by local and industrial producers in Bishoftu town of Ethiopia. Food Control 2020, 118, 107386. [Google Scholar] [CrossRef]
- Oliveira, B.R.; Mata, A.T.; Ferreira, J.P.; Crespo, M.T.B.; Pereira, V.J.; Bronze, M.R. Production of mycotoxins by filamentous fungi in untreated surface water. Environ. Sci. Pollut. Res. 2018, 25, 17519–17528. [Google Scholar] [CrossRef]
- Mhlongo, T.N.; Ogola, H.J.O.; Selvarajan, R.; Sibanda, T.; Kamika, I.; Tekere, M. Occurrence and diversity of waterborne fungi and associated mycotoxins in treated drinking water distribution system in South Africa: Implications on water quality and public health. Environ. Monit. Assess 2020, 192, 519. [Google Scholar] [CrossRef] [PubMed]
- Mata, A.T.; Ferreira, J.P.; Oliveira, B.R.; Batoréu, M.C.; Barreto Crespo, M.T.; Pereira, V.J.; Bronze, M.R. Bottled water: Analysis of mycotoxins by LC–MS/MS. Food Chem. 2015, 176, 455–464. [Google Scholar] [CrossRef]
- Leong, Y.-H.; Rosma, A.; Latiff, A.A.; Ahmad, N.I. Exposure assessment and risk characterization of aflatoxin B1 in Malaysia. Mycotoxin Res. 2011, 27, 207–214. [Google Scholar] [CrossRef]
- Schwartzbord, J.R.; Leroy, J.L.; Severe, L.; Brown, D.L. Urinary aflatoxin M1 in Port-au-Prince and a rural community in north-east Haiti. Food Addit. Contam. 2016, 33, 1036–1042. [Google Scholar] [CrossRef]
- Nugraha, A.; Khotimah, K.; Rietjens, I.M. Risk assessment of aflatoxin B1 exposure from maize and peanut consumption in Indonesia using the margin of exposure and liver cancer risk estimation approaches. Food Chem. Toxicol. 2018, 113, 134–144. [Google Scholar] [CrossRef]
- Turner, P.C.; Sylla, A.; Gong, Y.Y.; Diallo, M.S.; Sutcliffe, A.E.; Hall, A.J.; Wild, C.P. Reduction in exposure to carcinogenic aflatoxins by postharvest intervention measures in west Africa: A community-based intervention study. Lancet 2005, 365, 1950–1956. [Google Scholar] [CrossRef]
- Chauhan, N.M.; Washe, A.P.; Minota, T. Fungal infection and aflatoxin contamination in maize collected from Gedeo zone, Ethiopia. SpringerPlus 2016, 5, 753. [Google Scholar] [CrossRef] [Green Version]
- Turner, P.C.; Collinson, A.C.; Cheung, Y.B.; Gong, Y.Y.; Hall, A.J.; Prentice, A.M.; Wild, C.P. Aflatoxin exposure in utero causes growth faltering in Gambian infants. Int. J. Epidemiol. 2007, 36, 1119–1125. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.; Mitchell, N.J.; Gratz, J.; Houpt, E.R.; Gong, Y.Y.; Egner, P.A.; Groopman, J.D.; Riley, R.T.; Showker, J.L.; Svensen, E.; et al. Exposure to aflatoxin and fumonisin in children at risk for growth impairment in rural Tanzania. Environ. Int. 2018, 115, 29–37. [Google Scholar] [CrossRef]
- Admasu, F.T.; Melak, A.; Demissie, B.; Yenew, C.; Habtie, M.L.; Bekele, T.T.; Feyesa, T.O.; Chanie, E.S.; Medhin, M.T.G.; Malik, T.; et al. Occurrence and associated factors of aflatoxin M1 in raw cow milk in South Gondar Zone, North West Ethiopia, 2020. Food Sci. Nutr. 2021, 9, 6286–6293. [Google Scholar] [CrossRef]
- Ayalew, A. Mycotoxins and surface and internal fungi of maize from Ethiopia. Afr. J. Food Agric. Nutr. Dev. 2010, 10, 4109–4123. [Google Scholar] [CrossRef]
- Mamo, F.T.; Abate, B.A.; Tesfaye, K.; Nie, C.; Wang, G.; Liu, Y. Mycotoxins in Ethiopia: A Review on Prevalence, Economic and Health Impacts. Toxins 2020, 12, 648. [Google Scholar] [CrossRef]
- Cervini, C.; Verheecke-Vaessen, C.; He, T.; Mohammed, A.; Magan, N.; Medina, A. Improvements within the peanut production chain to minimize aflatoxins contamination: An Ethiopian case study. Food Control 2022, 136, 108622. [Google Scholar] [CrossRef]
- Wagacha, J.; Muthomi, J. Mycotoxin problem in Africa: Current status, implications to food safety and health and possible management strategies. Int. J. Food Microbiol. 2008, 124, 1–12. [Google Scholar] [CrossRef]
- Matendo, R.; Imathiu, S.; Udomkun, P.; Mugumaarhahama, Y.; Akullo, J.; Ishara, J.; Atehnkeng, J.; Owino, W. Aflatoxin and fumonisen mycotoxins contamination along the maize value chain in the eastern Democratic Republic of Congo. Afr. J. Food Agric. Nutr. Dev. 2022, 22, 19801–19821. [Google Scholar]
- Groopman, J.D.; Kensler, T.W.; Wild, C.P. Protective Interventions to Prevent Aflatoxin-Induced Carcinogenesis in Developing Countries. Annu. Rev. Public Health 2008, 29, 187–203. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.-G.; Egner, P.A.; Ng, D.; Jacobson, L.P.; Muñoz, A.; Zhu, Y.-R.; Qian, G.-S.; Wu, F.; Yuan, J.-M.; Groopman, J.D.; et al. Reduced Aflatoxin Exposure Presages Decline in Liver Cancer Mortality in an Endemic Region of China. Cancer Prev. Res. 2013, 6, 1038–1045. [Google Scholar] [CrossRef] [Green Version]
- Wu, F.; Mitchell, N.J.; Male, D.; Kensler, T.W. Reduced Foodborne Toxin Exposure Is a Benefit of Improving Dietary Diversity. Toxicol. Sci. 2014, 141, 329–334. [Google Scholar] [CrossRef] [Green Version]
- Omara, T.; Nassazi, W.; Omute, T.; Awath, A.; Laker, F.; Kalukusu, R.; Musau, B.; Nakabuye, B.V.; Kagoya, S.; Otim, G.; et al. Aflatoxins in Uganda: An Encyclopedic Review of the Etiology, Epidemiology, Detection, Quantification, Exposure Assessment, Reduction, and Control. Int. J. Microbiol. 2020, 2020, 4723612. [Google Scholar] [CrossRef] [Green Version]
- Katerere, D.R.; Shephard, G.S.; Faber, M. Infant malnutrition and chronic aflatoxicosis in Southern African: Is there a link? Int. J. Food Saf. Nutr. Public Health 2008, 1, 126–136. [Google Scholar]
| Variables | Frequency (%) | Mean (SD) |
|---|---|---|
| Child age (years) | 9 (1.8) | |
| 231 (56.6) | |
| 177 (43.4) | |
| Child sex | ||
| 202 (49.5) | |
| 206 (50.5) | |
| HAZ score a | ||
| 83 (20.3) | |
| 325 (79.7) | |
| Mother’s age (years) | 35.0 (7.7) | |
| 78 (19.1) | |
| 229 (56.1) | |
| 77 (18.9) | |
| 24 (5.9) | |
| Household size | 5.9 (1.7) | |
| 177 (43.4) | |
| 203 (49.8) | |
| 28 (6.8) | |
| Mother’s education | ||
| 214 (52.5) | |
| 194 (47.5) | |
| Mother’s occupation | ||
| 198 (48.5) | |
| 210 (51.5) | |
| HFIAS b | ||
| 63 (15.4) | |
| 123 (30.2) | |
| 149 (36.5) | |
| 73 (17.9) | |
| Frequency of maize consumption | ||
| 387 (94.9) | |
| 14 (3.4) | |
| 7 (1.7) | |
| Frequency of haricot bean consumption | ||
| 107 (26.2) | |
| 95 (23.2) | |
| 206 (50.6) | |
| Frequency of milk consumption | ||
| 14 (3.4) | |
| 17 (4.2) | |
| 377 (92.4) | |
| Frequency of enset consumption | ||
| 352 (86.3) | |
| 46 (11.3) | |
| 10 (2.4) | |
| Frequency of kale consumption | ||
| 202 (49.5) | |
| 184 (45.1) | |
| 22 (5.4) |
| Variable | β | 95% (CI) | p |
|---|---|---|---|
| Constant | 1.92 | 1.31, 2.56 | |
| Children age | −0.021 | −0.05, 0.036 | 0.36 |
| Maternal education | −0.13 | −0.19, −0.011 | 0.025 * |
| Father’s education | 0.034 | −0.05, 0.11 | 0.56 |
| Household size | 0.36 | 0.10, 0.64 | 0.020 * |
| HFIAS a | 0.18 | 0.058, 0.24 | 0.001 *** |
| DDS b | −0.13 | −0.25, −0.035 | 0.004 ** |
| Frequency of wheat consumption | 0.074 | −0.023, −0.149 | 0.148 |
| Frequency of haricot bean consumption | 0.087 | 0.012, 0.171 | 0.025 * |
| Frequency of cow milk consumption | 0.045 | 0.008, 0.084 | 0.026 * |
| Frequency of maize consumption | −0.01 | −0.096, 0.08 | 0.45 |
| Frequency of enset consumption | −0.05 | −0.098, 0.07 | 0.52 |
| Source of drinking water c | 0.11 | 0.064, 0.495 | 0.01 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gebreegziabher, T.; Dean, M.; Elias, E.; Tsegaye, W.; Stoecker, B.J. Urinary Aflatoxin M1 Concentration and Its Determinants in School-Age Children in Southern Ethiopia. Nutrients 2022, 14, 2580. https://doi.org/10.3390/nu14132580
Gebreegziabher T, Dean M, Elias E, Tsegaye W, Stoecker BJ. Urinary Aflatoxin M1 Concentration and Its Determinants in School-Age Children in Southern Ethiopia. Nutrients. 2022; 14(13):2580. https://doi.org/10.3390/nu14132580
Chicago/Turabian StyleGebreegziabher, Tafere, Melanie Dean, Elilta Elias, Workneh Tsegaye, and Barbara J. Stoecker. 2022. "Urinary Aflatoxin M1 Concentration and Its Determinants in School-Age Children in Southern Ethiopia" Nutrients 14, no. 13: 2580. https://doi.org/10.3390/nu14132580
APA StyleGebreegziabher, T., Dean, M., Elias, E., Tsegaye, W., & Stoecker, B. J. (2022). Urinary Aflatoxin M1 Concentration and Its Determinants in School-Age Children in Southern Ethiopia. Nutrients, 14(13), 2580. https://doi.org/10.3390/nu14132580






