Usage of Mobile Applications or Mobile Health Technology to Improve Diet Quality in Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Eligibility Criteria
2.4. Data Extraction and Outcomes
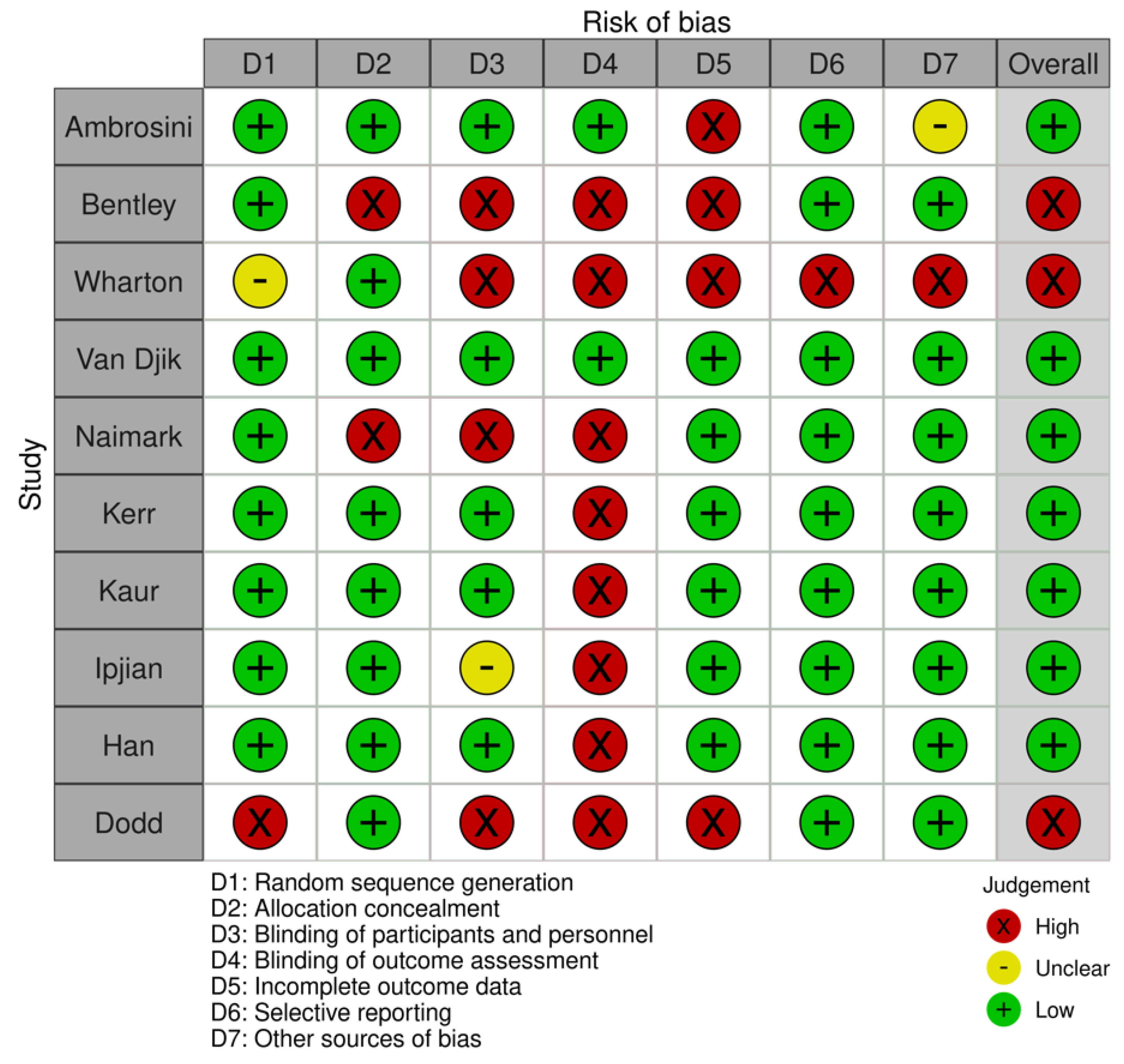
2.5. Quality Assessment
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Participants and Interventions
3.4. Risk of Bias within Studies
3.5. Study Outcomes
3.6. Secondary Findings
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adams, M.L.; Grandpre, J.; Katz, D.L.; Shenson, D. The impact of key modifiable risk factors on leading chronic conditions. Prev. Med. 2019, 120, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Wirt, A.; Collins, C.E. Diet quality—What is it and does it matter? Public Health Nutr. 2009, 12, 2473–2492. [Google Scholar] [CrossRef] [PubMed]
- Changizi, M.; Kaveh, M.H. Effectiveness of the mHealth technology in improvement of healthy behaviors in an elderly population—a systematic review. mHealth 2017, 3, 51. [Google Scholar] [CrossRef] [PubMed]
- Guenther, P.M.; Reedy, J.; Krebs-Smith, S.M. Development of the Healthy Eating Index-2005. J. Am. Diet. Assoc. 2008, 108, 1896–1901. [Google Scholar] [CrossRef]
- Perry, C.P.; Keane, E.; Layte, R.; Fitzgerald, A.P.; Perry, I.J.; Harrington, J.M. The use of a dietary quality score as a predictor of childhood overweight and obesity. BMC Public Health 2015, 15, 581. [Google Scholar] [CrossRef]
- Ryu, S. Book Review: mHealth: New Horizons for Health through Mobile Technologies: Based on the Findings of the Second Global Survey on eHealth (Global Observatory for eHealth Series, Volume 3). Healthc. Inform. Res. 2012, 18, 231. [Google Scholar] [CrossRef]
- Rollo, M.E.; Aguiar, E.J.; Williams, R.L.; Wynne, K.; Kriss, M.; Callister, R.; Collins, C.E. eHealth technologies to support nutrition and physical activity behaviors in diabetes self-management. Diabetes Metab. Syndr. Obes. Targets Ther. 2016, 9, 381–390. [Google Scholar] [CrossRef]
- Coughlin, S.S.; Whitehead, M.; Sheats, J.Q.; Mastromonico, J.; Hardy, D.; Smith, S.A. Smartphone Applications for Promoting Healthy Diet and Nutrition: A Literature Review. Jacobs J. Food Nutr. 2015, 2, 21. [Google Scholar]
- Flaherty, S.-J.; McCarthy, M.; Collins, A.; McAuliffe, F. Can existing mobile apps support healthier food purchasing behaviour? Content analysis of nutrition content, behaviour change theory and user quality integration. Public Health Nutr. 2017, 21, 288–298. [Google Scholar] [CrossRef]
- Bert, F.; Giacometti, M.; Gualano, M.R.; Siliquini, R. Smartphones and Health Promotion: A Review of the Evidence. J. Med. Syst. 2013, 38, 9995. [Google Scholar] [CrossRef]
- Ferrara, G.; Kim, J.; Lin, S.; Hua, J.; Seto, E. A Focused Review of Smartphone Diet-Tracking Apps: Usability, Functionality, Coherence with Behavior Change Theory, and Comparative Validity of Nutrient Intake and Energy Estimates. JMIR Mhealth Uhealth 2019, 7, e9232. [Google Scholar] [CrossRef] [PubMed]
- Gilliland, J.; Sadler, R.; Clark, A.; O’Connor, C.; Milczarek, M.; Doherty, S. Using a Smartphone Application to Promote Healthy Dietary Behaviours and Local Food Consumption. BioMed Res. Int. 2015, 2015, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stehr, P.; Karnowski, V.; Rossmann, C. The multi-faceted usage patterns of nutrition apps: A survey on the appropriation of nutrition apps among German-speaking users of MyFitnessPal. BMC Med. Inform. Decis. Mak. 2020, 20, 279. [Google Scholar] [CrossRef] [PubMed]
- McKay, F.H.; Wright, A.; Shill, J.; Stephens, H.; Uccellini, M. Using Health and Well-Being Apps for Behavior Change: A Systematic Search and Rating of Apps. JMIR Mhealth Uhealth 2019, 7, e11926. [Google Scholar] [CrossRef]
- Eikey, E.V. Effects of diet and fitness apps on eating disorder behaviours: Qualitative study. BJPsych. Open 2021, 7, e176. [Google Scholar] [CrossRef]
- Levinson, C.A.; Fewell, L.; Brosof, L.C. My Fitness Pal calorie tracker usage in the eating disorders. Eat. Behav. 2017, 27, 14–16. [Google Scholar] [CrossRef]
- Hall, K.D.; Kahan, S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med. Clin. N. Am. 2018, 102, 183–197. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, n71. [Google Scholar] [CrossRef]
- Cade, J.E. Measuring diet in the 21st century: Use of new technologies. Proc. Nutr. Soc. 2016, 76, 276–282. [Google Scholar] [CrossRef]
- Scarry, A.; Rice, J.; Connor, E.M.O.; Tierney, A.C. Does the use of mobile applications or mobile health technology improve diet quality in adults? A protocol for a systematic literature review. HRB Open Res. 2022, 5, 1. [Google Scholar] [CrossRef]
- Rayyan—Intelligent Systematic Review. Available online: www.rayyan.ai (accessed on 20 October 2020).
- Higgins, J.P.T.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, B.M.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. 2018, 106, 420. [Google Scholar] [CrossRef] [PubMed]
- Ipjian, L.M.; Johnston, C.S. Smartphone technology facilitates dietary change in healthy adults. Nutrition 2017, 33, 343–347. [Google Scholar] [CrossRef]
- Kerr, D.A.; Harray, A.J.; Pollard, C.M.; Dhaliwal, S.S.; Delp, E.J.; Howat, P.A.; Pickering, M.R.; Ahmad, Z.; Meng, X.; Pratt, I.S.; et al. The connecting health and technology study: A 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 52. [Google Scholar] [CrossRef]
- Wharton, C.M.; Johnston, C.S.; Cunningham, B.K.; Sterner, D. Dietary self-monitoring, but not dietary quality, improves with use of smartphone app technology in an 8-week weight loss trial. J. Nutr. Educ. Behav. 2014, 46, 440–444. [Google Scholar] [CrossRef]
- Dodd, J.M.; Louise, J.; Cramp, C.; Grivell, R.M.; Moran, L.J.; Deussen, A.R. Evaluation of a smartphone nutrition and physical activity application to provide lifestyle advice to pregnant women: The SNAPP randomised trial. Matern. Child Nutr. 2017, 14, e12502. [Google Scholar] [CrossRef]
- Safran Naimark, J.; Madar, Z.; Shahar, D.R. The Impact of a Web-Based App (eBalance) in Promoting Healthy Lifestyles: Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e56. [Google Scholar] [CrossRef]
- Kaur, J.; Kaur, M.; Chakrapani, V.; Webster, J.; Santos, J.A.; Kumar, R. Effectiveness of information technology–enabled ‘SMART Eating’ health promotion intervention: A cluster randomized controlled trial. PLoS ONE 2020, 15, e0225892. [Google Scholar] [CrossRef]
- Van Dijk, M.R.; Koster, M.P.H.; Oostingh, E.C.; Willemsen, S.P.; Steegers, E.A.P.; Steegers-Theunissen, R.P.M. A Mobile App Lifestyle Intervention to Improve Healthy Nutrition in Women Before and During Early Pregnancy: Single-Center Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e15773. [Google Scholar] [CrossRef]
- Ambrosini, G.L.; Hurworth, M.; Giglia, R.; Trapp, G.; Strauss, P. Feasibility of a commercial smartphone application for dietary assessment in epidemiological research and comparison with 24-h dietary recalls. Nutr. J. 2018, 17, 5. [Google Scholar] [CrossRef] [PubMed]
- Bentley, C.L.; Otesile, O.; Bacigalupo, R.; Elliott, J.; Noble, H.; Hawley, M.S.; Williams, E.A.; Cudd, P. Feasibility study of portable technology for weight loss and HbA1c control in type 2 diabetes. BMC Med. Inform. Decis. Mak. 2016, 16, 92. [Google Scholar] [CrossRef] [PubMed]
- Han, M.K.; Cho, B.; Kwon, H.; Son, K.Y.; Lee, H.; Lee, J.K.; Park, J. A Mobile-Based Comprehensive Weight Reduction Program for the Workplace (Health-On): Development and Pilot Study. JMIR Mhealth Uhealth 2019, 7, e11158. [Google Scholar] [CrossRef] [PubMed]
- Parmenter, K.; Wardle, J. Development of a general nutrition knowledge questionnaire for adults. Eur. J. Clin. Nutr. 1999, 53, 298–308. [Google Scholar] [CrossRef]
- Villinger, K.; Wahl, D.R.; Boeing, H.; Schupp, H.T.; Renner, B. The effectiveness of app-based mobile interventions on nutrition behaviours and nutrition-related health outcomes: A systematic review and meta-analysis. Obes. Rev. 2019, 20, 1465–1484. [Google Scholar] [CrossRef]
- Klasnja, P.; Pratt, W. Managing health with mobile technology. Interactions 2014, 21, 66–69. [Google Scholar] [CrossRef]
- Ahmed, M.; Mandic, I.; Lou, W.; Goodman, L.; Jacobs, I.; L’Abbé, M. Validation of a Tablet Application for Assessing Dietary Intakes Compared with the Measured Food Intake/Food Waste Method in Military Personnel Consuming Field Rations. Nutrients 2017, 9, 200. [Google Scholar] [CrossRef]
- Chiu, M.-C.; Chang, S.-P.; Chang, Y.-C.; Chu, H.-H.; Chen, C.C.-H.; Hsiao, F.-H. Playful bottle. In Proceedings of the Ubicomp ′09: 11th International Conference on Ubiquitous Computing, Orlando, FL, USA, 30 September–3 October 2009; Association for Computing Machinery: New York, NY, USA, 2009. [Google Scholar] [CrossRef]
- Connor, S. Underreporting of Dietary Intake: Key Issues for Weight Management Clinicians. Curr. Cardiovasc. Risk Rep. 2020, 14, 16. [Google Scholar] [CrossRef]
- Lee, M.; Lee, H.; Kim, Y.; Kim, J.; Cho, M.; Jang, J.; Jang, H. Mobile App-Based Health Promotion Programs: A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2018, 15, 2838. [Google Scholar] [CrossRef]
- Chiarini, G.; Ray, P.; Akter, S.; Masella, C.; Ganz, A. mHealth Technologies for Chronic Diseases and Elders: A Systematic Review. IEEE J. Sel. Areas Commun. 2013, 31, 6–18. [Google Scholar] [CrossRef]
- Xiong, S.; Berkhouse, H.; Schooler, M.; Pu, W.; Sun, A.; Gong, E.; Yan, L.L. Effectiveness of mHealth Interventions in Improving Medication Adherence Among People with Hypertension: A Systematic Review. Curr. Hypertens. Rep. 2018, 20, 86. [Google Scholar] [CrossRef] [PubMed]
- Thiele, S.; Mensink, G.B.M.; Beitz, R. Determinants of diet quality. Public Health Nutr. 2004, 7, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Harrington, J.; Fitzgerald, A.P.; Layte, R.; Lutomski, J.; Molcho, M.; Perry, I.J. Sociodemographic, health and lifestyle predictors of poor diets. Public Health Nutr. 2011, 14, 2166–2175. [Google Scholar] [CrossRef] [PubMed]
- Vlahu-Gjorgievska, E.; Unnikrishnan, S.M.; Win, K.T. mHealth applications: A tool for behaviour change in weight management. Stud. Health Technol. Inform. 2018, 252, 158–163. [Google Scholar]
- Walsh, J.C.; Corbett, T.; Hogan, M.; Duggan, J.; McNamara, A. An mHealth Intervention Using a Smartphone App to Increase Walking Behavior in Young Adults: A Pilot Study. JMIR Mhealth Uhealth 2016, 4, e109. [Google Scholar] [CrossRef]
- Rossi, G.M.; Bigi, S. mHealth for diabetes support: A systematic review of apps available on the Italian market. mHealth 2017, 3, 16. [Google Scholar] [CrossRef][Green Version]
- Spillers, F.; Asimakopoulos, S. Does Social User Experience Improve Motivation for Runners? In Design, User Experience, and Usability. User Experience Design Practice; Springer International Publishing: Cham, Switzerland, 2014. [Google Scholar]
- Pfaeffli, L.; Maddison, R.; Whittaker, R.; Stewart, R.; Kerr, A.; Jiang, Y.; Kira, G.; Carter, K.; Dalleck, L. A mHealth cardiac rehabilitation exercise intervention: Findings from content development studies. BMC Cardiovasc. Disord. 2012, 12, 36. [Google Scholar] [CrossRef]
- Dekker, J.; de Groot, V.; ter Steeg, A.M.; Vloothuis, J.; Holla, J.; Collette, E.; Satink, T.; Post, L.; Doodeman, S.; Littooij, E. Setting meaningful goals in rehabilitation: Rationale and practical tool. Clin. Rehabil. 2019, 34, 3–12. [Google Scholar] [CrossRef]
- Castelnuovo, G.; Manzoni, G.M.; Pietrabissa, G.; Corti, S.; Giusti, E.M.; Molinari, E.; Simpson, S. Obesity and outpatient rehabilitation using mobile technologies: The potential mHealth approach. Front. Psychol. 2014, 5, 559. [Google Scholar] [CrossRef]
- Kim, H.; Faw, M.; Michaelides, A. Mobile But Connected: Harnessing the Power of Self-Efficacy and Group Support for Weight Loss Success through mHealth Intervention. J. Health Commun. 2017, 22, 395–402. [Google Scholar] [CrossRef]
- Patel, M.L.; Hopkins, C.M.; Bennett, G.G. Early weight loss in a standalone mHealth intervention predicting treatment success. Obes. Sci. Pract. 2019, 5, 231–237. [Google Scholar] [CrossRef]
- Xu, Z.; Steffen, L.M.; Selvin, E.; Rebholz, C.M. Diet quality, change in diet quality and risk of incident CVD and diabetes. Public Health Nutr. 2020, 23, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Norris, A.C.; Stockdale, R.S.; Sharma, S. A strategic approach to m-health. Health Inform. J. 2009, 15, 244–253. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, S.W.; Henderson, S.; Young, H.M.; Pande, A.; Han, J.J. Tracking Health Data Is Not Enough: A Qualitative Exploration of the Role of Healthcare Partnerships and mHealth Technology to Promote Physical Activity and to Sustain Behavior Change. JMIR Mhealth Uhealth 2016, 4, e5. [Google Scholar] [CrossRef] [PubMed]
- Eikey, V.E.; Reddy, M.C. “It’s Definitely Been a Journey”: A Qualitative Study on How Women with Eating Disorders Use Weight Loss Apps. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, Denver, CO, USA, 6–11 May 2017; Association for Computing Machinery: Denver, CO, USA; pp. 642–654. [Google Scholar]
- Lieffers, J.R.; Arocha, J.F.; Grindrod, K.; Hanning, R.M. Experiences and Perceptions of Adults Accessing Publicly Available Nutrition Behavior-Change Mobile Apps for Weight Management. J. Acad. Nutr. Diet. 2018, 118, 229–239. [Google Scholar] [CrossRef]
- McCaig, D.; Elliott, M.T.; Prnjak, K.; Walasek, L.; Meyer, C. Engagement with MyFitnessPal in eating disorders: Qualitative insights from online forums. Int. J. Eat. Disord. 2020, 53, 404–411. [Google Scholar] [CrossRef]
- Feldhege, J.; Moessner, M.; Bauer, S. Detrimental Effects of Online Pro–Eating Disorder Communities on Weight Loss and Desired Weight: Longitudinal Observational Study. J. Med. Internet Res. 2021, 23, e27153. [Google Scholar] [CrossRef]
- Woodruff, S.J.; Hanning, R.M.; Lambraki, I.; Storey, K.E.; McCargar, L. Healthy Eating Index-C is compromised among adolescents with body weight concerns, weight loss dieting, and meal skipping. Body Image 2008, 5, 404–408. [Google Scholar] [CrossRef]
- Santiago, A.; Zimmerman, J.; Feinstein, R.; Fisher, M. Diet quality of adolescents with eating disorders. Int. J. Adolesc. Med. Health 2019, 31. [Google Scholar] [CrossRef]
- König, L.M.; Attig, C.; Franke, T.; Renner, B. Barriers to and Facilitators for Using Nutrition Apps: Systematic Review and Conceptual Framework. JMIR Mhealth Uhealth 2021, 9, e20037. [Google Scholar] [CrossRef]

| Author (Year) | Country | Study Design: Size, Gender and Age | Participant Characteristics | Duration | Application | Intervention | Control | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Ambrosini et al. (2018) [32] | Australia | Short report | 50 adults, 82% women mean age, 31. Majority female. Mean BMI, 22.4 | 4 days | Easy Diet Diary app | The Australian Calorie Counter—Easy Diet Diary smartphone app is a commercial calorie counter and food diary. Study participants completed a 4 d food diary using a modified version of the Easy Diet Diary app. The quality of diet was measured by both the intervention and control | Two 24 h recall | Average energy ratios were used to measure the quality of the participant’s diet from macronutrient fibre, iron, and calcium densities from the app and the 24 h recalls. The study using mean daily nutrient intakes from mobile applications and dietary recalls indicated no distinct differences between the app and the 24 h recalls for protein, saturated fat, carbohydrate and iron density. Added sugar intake was recorded higher in participants in the 24 h recalls. |
| Bentley C. L., et al. (2016) [33] | United Kingdom | Feasibility study | 27 adults, Female, mean 52.9 BMI between 25 and 40 (for inclusion in the study) | 39 weeks | AiperMotion 500 | The intervention was a small wearable M-health device used over 12 weeks by overweight people with T2DM with the intent to lose weight and reduce their HbA1c level. This study was split into three groups, each with additional resources. Group one received advice on diet and exercise; groups two and three could track dietary information whenever food or drink was consumed. | No intervention or intervention plus weekly motivational support (group three) | This paper showed that the groups using the app benefited from weight loss and their diet management and HbA1c control. This study showed that mobile app users had a more significant reduction in HbA1c. The feedback highlighted user preference for using the mobile app to improve diet. |
| Dodd et al. (2017) [28] | Australia | Randomised Controlled Trial | 162 Pregnant women. Approximately 43% of women were of normal BMI, 19% were overweight, and 38% were obese | 26 weeks | Lifestyle Advice plus Smartphone Application | The trial evaluated the impact of a smartphone application as an adjunct to face-to-face consultations in facilitating dietary and physical activity change among pregnant women. The intervention study examined both the use of a mobile application and lifestyle advice, while the control group only received lifestyle advice. | Lifestyle Advice | No difference between quality of diet between intervention and control. All participants in the trial showed increases in milk and whole grains consumption and a decrease in sodium consumption over the trial. Although all women improved their quality of diet across pregnancy, use of the smartphone application was poor at 31%. |
| Han et al. (2019) [34] | Republic of Korea | Pilot Study | 30 volunteers 93.3% were male and the median age was 39. Majority male. BMI 28.0 (27.2–30.3) (kg/m2) | 12 weeks | Health-On | A weight reduction app Health-On was prescribed to the intervention group for Weight Reduction. The Health-On app has four theme pages: main, diet, physical activity, challenge and ranking. Each page allows users to see their achievements easily and maximise user convenience and app effectiveness with a simple user interface. | Did not use mobile intervention | The primary aim of this research was to examine the impact of mobile technology on weight loss, which was achieved in the study. Participants used the Health-On program to track their diet and manage their daily calorie intake; this highlighted improved diet quality when comparing outcomes before and after the Health-On program. |
| Ipjian et al. (2016) [25] | United States | Randomised Controlled Trial | 30 adults 7 males and 23 female, mean age 34.4 majority Female. BMI 25.6 ± 4.3 kg/m2 | 4 weeks | MyFitnessPal app | Participants were instructed to reduce their sodium intake to ≤2300 mg/d by using the MyFitnessPal app to receive feedback on the sodium content of foods. | Journal tallying of foods | Participants completed a brief health history questionnaire and the Rapid Eating and Activity Assessment for Patients at the initial visit, a short, one-page, validated questionnaire to assess diet quality. At baseline, sodium intake was inversely related to diet quality. Throughout the trial, the change in diet quality scores did not differ between groups, and urinary sodium excretion decreased in the app group only compared with baseline values. |
| Kaur et al. (2020) [30] | India | Randomised controlled trial | 732 participants 76% women, mean age 53. Majority female. Baseline 27.45 Kg/m2 and change −0.25 kg/m2 | 6 months | ‘SMART Eating’ intervention | The intervention included information technology SMS, email, social networking app and ‘SMART Eating’ website, interpersonal communication, and distribution of a ‘SMART Eating’ kit—kitchen calendar, dining table mat, and measuring spoons. The intervention was executed at the household level over six months. | Pictorial pamphlet on the dietary recommendations of National Institute of Nutrition, India, with information written in Hindi language | Primary outcomes were changes in mean dietary intakes of fat, sugar, salt, and fruit and vegetables, there was a secondary improvement of changes in BMI, blood pressure, haemoglobin, FPG, and serum lipids. This study used M-health and showed improvement in diet quality concerning their intake in fruit and vegetables. |
| Kerr et al. (2016) [26] | Australia | Randomised Controlled Trial | 247 participants 162 women and 85 men. Mean age (years) 24.2 ± 3.2, 23.7 ± 3.4, 25.0 ± 3.5 in groups a, b and c respectively. Majority female. Dietary feedback only group showed the weight change from baseline = −1.75 kg and BMI change, BMI (p = 0.01) | 6 months | Mobile food record App (mFR) | (A). Dietary feedback and weekly text messages, (B) dietary feedback. Dietary intake was assessed using a mobile food record App (mFR) where participants captured images of foods and beverages consumed over 4-days at baseline and post-intervention. | Control did not receive any dietary feedback or text messages. | This study showed improvement in diet quality related to the use of mFR application. This included uptake of fruit and veg and a decrease in EDNP foods in men and SSB in women and a reduction in body weight |
| Naimark et al. (2015) [29] | Israel | Randomised Controlled Trial | 85 participants 64% women and 36% men. The mean age was 47.9 (SD 12.3) years. BMI was 26.2 (SD 3.9) | 14 weeks | Web-based app | Access to the app without any face-to-face support. | The control subjects continued their standard lifestyle | The study noted that the app users increased their diet quality score by the end of the study. Based on guidelines from a 16-item questionnaire based on Parmenter’s general nutrition knowledge questionnaire for adults, diet quality was measured using an online self-reported questionnaire. The improvement in diet quality scores was no difference between light and heavy users of the mobile application. |
| van Dijk et al. (2020) [31] | Netherlands | Randomised Controlled Trial | 218 participants Women between aged 18 and 45, median age 30.6 (5.3) 30.7 (5.7) years. BMI Not measured | 24 weeks | The Smarter Pregnancy program. | Intervention group received personal online coaching based on identified inadequate intakes of vegetables, fruits, and folic acid supplement | No coaching or application | Dietary risk score (DRS), improved in the women using the mobile application, this was due to larger intake of fruit and vegetables |
| Wharton et al. (2014) [27] | United States | Randomised Controlled Trial | 57 participants Age years 43.7 ± 3.5, 41.5 ± 4.0, 40.8 ± 3.8. (Group a, b and c respectively). Gender, 12 male, 35 female. | 8 week | Lose it | The intervention group used the mobile app Lose It (group 1) | Groups 2 and 3 used the memo feature on a smartphone, or a traditional paper-and-pencil method, respectively. | Weight loss was the measurement of this study, however, it was noted the participants using the app had an increase in the consumption of fruit and veg and the research suggests that mobile applications improve diet quality. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarry, A.; Rice, J.; O’Connor, E.M.; Tierney, A.C. Usage of Mobile Applications or Mobile Health Technology to Improve Diet Quality in Adults. Nutrients 2022, 14, 2437. https://doi.org/10.3390/nu14122437
Scarry A, Rice J, O’Connor EM, Tierney AC. Usage of Mobile Applications or Mobile Health Technology to Improve Diet Quality in Adults. Nutrients. 2022; 14(12):2437. https://doi.org/10.3390/nu14122437
Chicago/Turabian StyleScarry, Alan, Jennifer Rice, Eibhlís M. O’Connor, and Audrey C. Tierney. 2022. "Usage of Mobile Applications or Mobile Health Technology to Improve Diet Quality in Adults" Nutrients 14, no. 12: 2437. https://doi.org/10.3390/nu14122437
APA StyleScarry, A., Rice, J., O’Connor, E. M., & Tierney, A. C. (2022). Usage of Mobile Applications or Mobile Health Technology to Improve Diet Quality in Adults. Nutrients, 14(12), 2437. https://doi.org/10.3390/nu14122437






