Nocturnal Lifestyle Behaviours and Risk of Poor Sleep during Pregnancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection and Measures
2.3. Nocturnal Behaviours
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
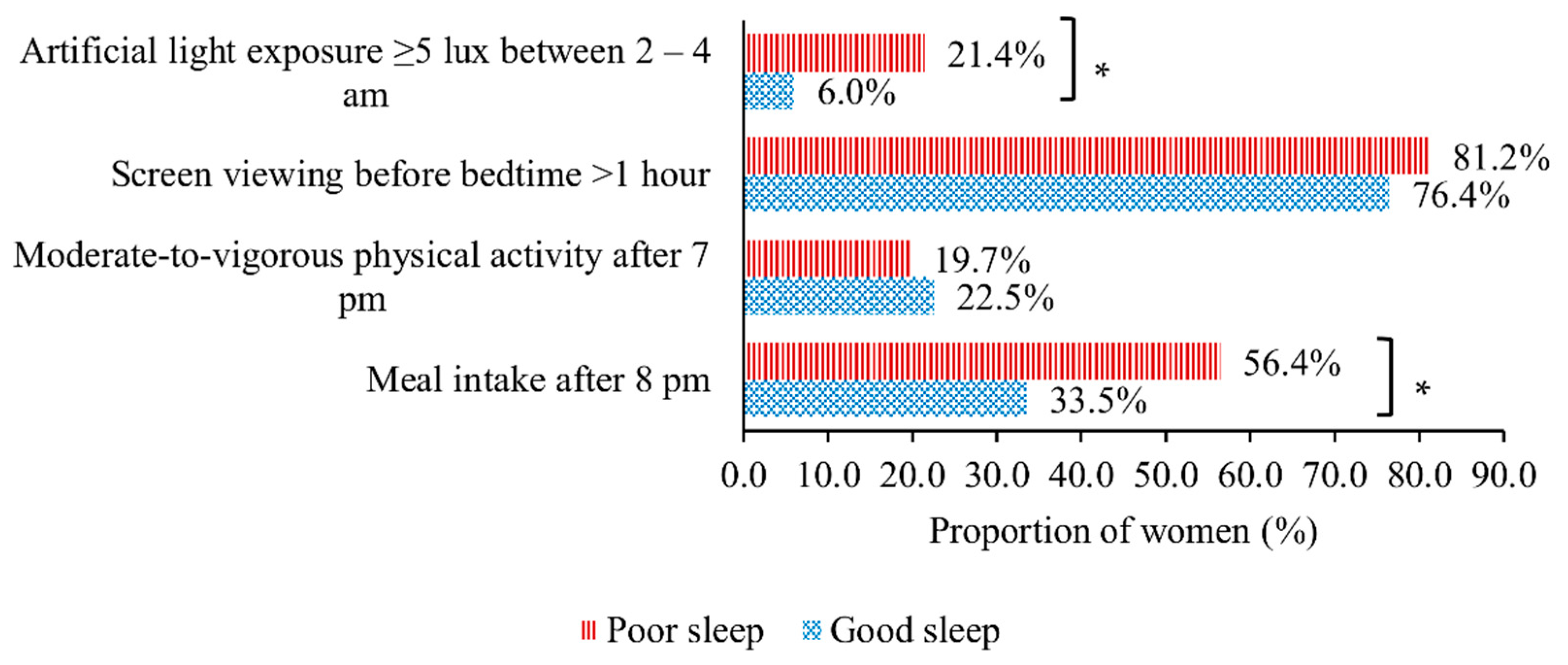
3.2. Associations between Nocturnal Behaviours and Sleep Quality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stranges, S.; Tigbe, W.; Gómez-Olivé, F.X.; Thorogood, M.; Kandala, N.B. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 2012, 35, 1173–1181. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; Smirne, S. Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Med. 2002, 3, 115–120. [Google Scholar] [CrossRef]
- Wong, W.S.; Fielding, R. Prevalence of insomnia among Chinese adults in Hong Kong: A population-based study. J. Sleep Res. 2011, 20, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Felder, J.N.; Baer, R.J.; Rand, L.; Jelliffe-Pawlowski, L.L.; Prather, A.A. Sleep Disorder Diagnosis During Pregnancy and Risk of Preterm Birth. Obs. Gynecol. 2017, 130, 573–581. [Google Scholar] [CrossRef]
- Sedov, I.D.; Cameron, E.E.; Madigan, S.; Tomfohr-Madsen, L.M. Sleep quality during pregnancy: A meta-analysis. Sleep Med. Rev. 2018, 38, 168–176. [Google Scholar] [CrossRef]
- Silvestri, R.; Aricò, I. Sleep disorders in pregnancy. Sleep Sci. 2019, 12, 232–239. [Google Scholar] [CrossRef]
- Bourjeily, G.; Raker, C.A.; Chalhoub, M.; Miller, M.A. Pregnancy and fetal outcomes of symptoms of sleep-disordered breathing. Eur. Respir. J. 2010, 36, 849. [Google Scholar] [CrossRef]
- Adaji, S.E.; Shittu, O.S.; Bature, S.B.; Nasir, S.; Olatunji, O. Bothersome lower urinary symptoms during pregnancy: A preliminary study using the International Consultation on Incontinence Questionnaire. Afr. Health Sci. 2011, 11 (Suppl. 1), S46–S52. [Google Scholar] [CrossRef][Green Version]
- Lee, K.A.; Zaffke, M.E.; Baratte-Beebe, K. Restless Legs Syndrome and Sleep Disturbance during Pregnancy: The Role of Folate and Iron. J. Women’s Health Gend. Based Med. 2001, 10, 335–341. [Google Scholar] [CrossRef]
- Lo, C.M.H.; Lee, P.H. Prevalence and impacts of poor sleep on quality of life and associated factors of good sleepers in a sample of older Chinese adults. Health Qual. Life Outcomes 2012, 10, 72. [Google Scholar] [CrossRef]
- Irish, L.A.; Kline, C.E.; Gunn, H.E.; Buysse, D.J.; Hall, M.H. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med. Rev. 2015, 22, 23–36. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders, Revised: Diagnostic and Coding Manual; AASM: Chicago, IL, USA, 2001. [Google Scholar]
- Stepanski, E.J.; Wyatt, J.K. Use of sleep hygiene in the treatment of insomnia. Sleep Med. Rev. 2003, 7, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Tan, E.; Healey, D.; Gray, A.R.; Galland, B.C. Sleep hygiene intervention for youth aged 10 to 18 years with problematic sleep: A before-after pilot study. BMC Pediatrics 2012, 12, 189. [Google Scholar] [CrossRef] [PubMed]
- Murawski, B.; Wade, L.; Plotnikoff, R.C.; Lubans, D.R.; Duncan, M.J. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med. Rev. 2018, 40, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Herscher, M.; Mikhaylov, D.; Barazani, S.; Sastow, D.; Yeo, I.; Dunn, A.S.; Cho, H.J. A Sleep Hygiene Intervention to Improve Sleep Quality for Hospitalized Patients. Jt. Comm. J. Qual. Patient Saf. 2021, 47, 343–346. [Google Scholar] [CrossRef]
- Loy, S.L.; Cheung, Y.B.; Chong, M.; Müller-Riemenschneider, F.; Lek, N.; Lee, Y.; Tan, K.H.; Chern, B.; Yap, F.; Chan, J. Maternal night-eating pattern and glucose tolerance during pregnancy: Study protocol for a longitudinal study. BMJ Open 2019, 9, e030036. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, A.; Rosner, B.; Lockley, S.W.; Schernhammer, E.S. Validation of a light questionnaire with real-life photopic illuminance measurements: The Harvard Light Exposure Assessment questionnaire. Cancer Epidemiol. Biomark. Prev. 2011, 20, 1341–1349. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Skouteris, H.; Wertheim, E.H.; Germano, C.; Paxton, S.J.; Milgrom, J. Assessing sleep during pregnancy: A study across two time points examining the Pittsburgh Sleep Quality Index and associations with depressive symptoms. Womens Health Issues 2009, 19, 45–51. [Google Scholar] [CrossRef]
- Zhong, Q.Y.; Gelaye, B.; Sánchez, S.E.; Williams, M.A. Psychometric Properties of the Pittsburgh Sleep Quality Index (PSQI) in a Cohort of Peruvian Pregnant Women. J. Clin. Sleep Med. 2015, 11, 869–877. [Google Scholar] [CrossRef]
- Loy, S.L.; Cheung, Y.B.; Cai, S.; Colega, M.T.; Godfrey, K.M.; Chong, Y.S.; Shek, L.P.; Tan, K.H.; Chong, M.F.; Yap, F.; et al. Maternal night-time eating and sleep duration in relation to length of gestation and preterm birth. Clin. Nutr. 2020, 39, 1935–1942. [Google Scholar] [CrossRef] [PubMed]
- Stutz, J.; Eiholzer, R.; Spengler, C.M. Effects of Evening Exercise on Sleep in Healthy Participants: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 269–287. [Google Scholar] [CrossRef] [PubMed]
- Hale, L.; Kirschen, G.W.; LeBourgeois, M.K.; Gradisar, M.; Garrison, M.M.; Montgomery-Downs, H.; Kirschen, H.; McHale, S.M.; Chang, A.-M.; Buxton, O.M. Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child Adolesc. Psychiatr. Clin. N. Am. 2018, 27, 229–245. [Google Scholar] [CrossRef] [PubMed]
- Phillips, A.J.K.; Vidafar, P.; Burns, A.C.; McGlashan, E.M.; Anderson, C.; Rajaratnam, S.M.W.; Lockley, S.W.; Cain, S.W. High sensitivity and interindividual variability in the response of the human circadian system to evening light. Proc. Natl. Acad. Sci. USA 2019, 116, 12019–12024. [Google Scholar] [CrossRef]
- Grivas, T.B.; Savvidou, O.D. Melatonin the “light of night” in human biology and adolescent idiopathic scoliosis. Scoliosis 2007, 2, 6. [Google Scholar] [CrossRef]
- Touitou, Y.; Reinberg, A.; Touitou, D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life Sci. 2017, 173, 94–106. [Google Scholar] [CrossRef]
- Walbeek, T.J.; Harrison, E.M.; Gorman, M.R.; Glickman, G.L. Naturalistic Intensities of Light at Night: A Review of the Potent Effects of Very Dim Light on Circadian Responses and Considerations for Translational Research. Front. Neurol. 2021, 12, 625334. [Google Scholar] [CrossRef]
- Zou, G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 2004, 159, 702–706. [Google Scholar] [CrossRef]
- Loy, S.L.; Loo, R.S.X.; Godfrey, K.M.; Chong, Y.S.; Shek, L.P.; Tan, K.H.; Chong, M.F.; Chan, J.K.Y.; Yap, F. Chrononutrition during Pregnancy: A Review on Maternal Night-Time Eating. Nutrients 2020, 12, 2783. [Google Scholar] [CrossRef]
- Zhang, H.; Li, P.; Fan, D.; Wu, S.; Rao, J.; Lin, D.; Huang, Q.; Liu, Z. Prevalence of and Risk Factors for Poor Sleep During Different Trimesters of Pregnancy Among Women in China: A Cross-Sectional Study. Nat. Sci. Sleep 2021, 13, 811–820. [Google Scholar] [CrossRef] [PubMed]
- Kroeger, E.N.; Carson, T.L.; Baskin, M.L.; Langaigne, A.; Schneider, C.R.; Bertrand, B.; Herbey, I.I.; Harper, L.M.; Biggio, J.R.; Chandler-Laney, P.C. Reasons for Late-Night Eating and Willingness to Change:A Qualitative Study in Pregnant Black Women. J. Nutr. Educ. Behav. 2019, 51, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Wołyńczyk-Gmaj, D.; Różańska-Walędziak, A.; Ziemka, S.; Ufnal, M.; Brzezicka, A.; Gmaj, B.; Januszko, P.; Fudalej, S.; Czajkowski, K.; Wojnar, M. Insomnia in Pregnancy Is Associated With Depressive Symptoms and Eating at Night. J. Clin. Sleep Med. 2017, 13, 1171–1176. [Google Scholar] [CrossRef]
- Lindseth, G.; Lindseth, P.; Thompson, M. Nutritional Effects on Sleep. West. J. Nurs. Res. 2013, 35, 497–513. [Google Scholar] [CrossRef]
- Wurtman, R.J.; Wurtman, J.J.; Regan, M.M.; McDermott, J.M.; Tsay, R.H.; Breu, J.J. Effects of normal meals rich in carbohydrates or proteins on plasma tryptophan and tyrosine ratios. Am. J. Clin. Nutr. 2003, 77, 128–132. [Google Scholar] [CrossRef]
- Karnani, M.M.; Apergis-Schoute, J.; Adamantidis, A.; Jensen, L.T.; de Lecea, L.; Fugger, L.; Burdakov, D. Activation of central orexin/hypocretin neurons by dietary amino acids. Neuron 2011, 72, 616–629. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.-P.; Roberts, A.; Shechter, A.; Choudhury, A.R. Fiber and Saturated Fat Are Associated with Sleep Arousals and Slow Wave Sleep. J. Clin. Sleep Med. 2016, 12, 19–24. [Google Scholar] [CrossRef]
- Katagiri, R.; Asakura, K.; Kobayashi, S.; Suga, H.; Sasaki, S. Low intake of vegetables, high intake of confectionary, and unhealthy eating habits are associated with poor sleep quality among middle-aged female Japanese workers. J. Occup. Health 2014, 56, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Kräuchi, K.; Cajochen, C.; Werth, E.; Wirz-Justice, A. Alteration of internal circadian phase relationships after morning versus evening carbohydrate-rich meals in humans. J. Biol. Rhythm 2002, 17, 364–376. [Google Scholar] [CrossRef]
- Guerrero-Vargas, N.N.; Espitia-Bautista, E.; Buijs, R.M.; Escobar, C. Shift-work: Is time of eating determining metabolic health? Evidence from animal models. Proc. Nutr. Soc. 2018, 77, 199–215. [Google Scholar] [CrossRef]
- McMullan, C.J.; Curhan, G.C.; Schernhammer, E.S.; Forman, J.P. Association of Nocturnal Melatonin Secretion With Insulin Resistance in Nondiabetic Young Women. Am. J. Epidemiol. 2013, 178, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Reschke, L.; McCarthy, R.; Herzog, E.D.; Fay, J.C.; Jungheim, E.S.; England, S.K. Chronodisruption: An untimely cause of preterm birth? Best Prac. Res. Clin. Obs. Gynaecol. 2018, 52, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Maria Siega-Riz, A.; Herrmann, T.S.; Savitz, D.A.; Thorp, J.M. Frequency of Eating During Pregnancy and Its Effect on Preterm Delivery. Am. J. Epidemiol. 2001, 153, 647–652. [Google Scholar] [CrossRef]
- Kinsey, A.W.; Ormsbee, M.J. The Health Impact of Nighttime Eating: Old and New Perspectives. Nutrients 2015, 7, 2648–2662. [Google Scholar] [CrossRef]
- Lin, H.H.; Tsai, P.S.; Fang, S.C.; Liu, J.F. Effect of kiwifruit consumption on sleep quality in adults with sleep problems. Asia Pac. J. Clin. Nutr. 2011, 20, 169–174. [Google Scholar] [PubMed]
- Meng, X.; Li, Y.; Li, S.; Zhou, Y.; Gan, R.-Y.; Xu, D.-P.; Li, H.-B. Dietary Sources and Bioactivities of Melatonin. Nutrients 2017, 9, 367. [Google Scholar] [CrossRef]
- Cho, Y.; Ryu, S.H.; Lee, B.R.; Kim, K.H.; Lee, E.; Choi, J. Effects of artificial light at night on human health: A literature review of observational and experimental studies applied to exposure assessment. Chronobiol. Int. 2015, 32, 1294–1310. [Google Scholar] [CrossRef]
- Santhi, N.; Thorne, H.C.; van der Veen, D.R.; Johnsen, S.; Mills, S.L.; Hommes, V.; Schlangen, L.J.M.; Archer, S.N.; Dijk, D.-J. The spectral composition of evening light and individual differences in the suppression of melatonin and delay of sleep in humans. J. Pineal Res. 2012, 53, 47–59. [Google Scholar] [CrossRef]
- Blask, D.E.; Dauchy, R.T.; Sauer, L.A.; Krause, J.A.; Brainard, G.C. Light during darkness, melatonin suppression and cancer progression. Neurol. Endocrinol. Lett. 2002, 23 (Suppl. 2), 52–56. [Google Scholar]
- Schernhammer, E.S.; Hankinson, S.E. Urinary melatonin levels and breast cancer risk. J. Natl. Cancer Inst. 2005, 97, 1084–1087. [Google Scholar] [CrossRef]
- Reiter, R.J.; Tan, D.X.; Korkmaz, A.; Erren, T.C.; Piekarski, C.; Tamura, H.; Manchester, L.C. Light at night, chronodisruption, melatonin suppression, and cancer risk: A review. Crit. Rev. Oncog. 2007, 13, 303–328. [Google Scholar] [CrossRef] [PubMed]
- Lyssenko, V.; Nagorny, C.L.; Erdos, M.R.; Wierup, N.; Jonsson, A.; Spégel, P.; Bugliani, M.; Saxena, R.; Fex, M.; Pulizzi, N.; et al. Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat. Genet. 2009, 41, 82–88. [Google Scholar] [CrossRef]
- Bouatia-Naji, N.; Bonnefond, A.; Cavalcanti-Proença, C.; Sparsø, T.; Holmkvist, J.; Marchand, M.; Delplanque, J.; Lobbens, S.; Rocheleau, G.; Durand, E.; et al. A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat. Genet. 2009, 41, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Lanoix, D.; Guérin, P.; Vaillancourt, C. Placental melatonin production and melatonin receptor expression are altered in preeclampsia: New insights into the role of this hormone in pregnancy. J. Pineal Res. 2012, 53, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Reiter, R.J.; Tamura, H.; Tan, D.X.; Xu, X.Y. Melatonin and the circadian system: Contributions to successful female reproduction. Fertil. Steril. 2014, 102, 321–328. [Google Scholar] [CrossRef]
- Tamura, H.; Nakamura, Y.; Terron, M.P.; Flores, L.J.; Manchester, L.C.; Tan, D.-X.; Sugino, N.; Reiter, R.J. Melatonin and pregnancy in the human. Reprod. Toxicol. 2008, 25, 291–303. [Google Scholar] [CrossRef]
- Brown, T.M.; Brainard, G.C.; Cajochen, C.; Czeisler, C.A.; Hanifin, J.P.; Lockley, S.W.; Lucas, R.J.; Münch, M.; O’Hagan, J.B.; Peirson, S.N.; et al. Recommendations for daytime, evening, and nighttime indoor light exposure to best support physiology, sleep, and wakefulness in healthy adults. PLoS Biol. 2022, 20, e3001571. [Google Scholar] [CrossRef]
- Gradisar, M.; Wolfson, A.R.; Harvey, A.G.; Hale, L.; Rosenberg, R.; Czeisler, C.A. The Sleep and Technology Use of Americans: Findings from the National Sleep Foundation’s 2011 Sleep in America Poll. J. Clin. Sleep Med. 2013, 09, 1291–1299. [Google Scholar] [CrossRef]
- West, K.E.; Jablonski, M.R.; Warfield, B.; Cecil, K.S.; James, M.; Ayers, M.A.; Maida, J.; Bowen, C.; Sliney, D.H.; Rollag, M.D.; et al. Blue light from light-emitting diodes elicits a dose-dependent suppression of melatonin in humans. J. Appl. Physiol. 2011, 110, 619–626. [Google Scholar] [CrossRef]
- Chang, A.-M.; Aeschbach, D.; Duffy, J.F.; Czeisler, C.A. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc. Natl. Acad. Sci. USA 2015, 112, 1232–1237. [Google Scholar] [CrossRef]
- Huang, L.; Fan, L.; Ding, P.; He, Y.H.; Xie, C.; Niu, Z.; Tian, F.Y.; Yuan, S.X.; Jia, D.Q.; Chen, W.Q. Maternal exercise during pregnancy reduces the risk of preterm birth through the mediating role of placenta. J. Matern. Fetal Neonatal. Med. 2019, 32, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Smyka, M.; Kosińska-Kaczyńska, K.; Sochacki-Wójcicka, N.; Zgliczyńska, M.; Wielgoś, M. Sleep Problems in Pregnancy—A Cross-Sectional Study in over 7000 Pregnant Women in Poland. Int. J. Environ. Res. Public Health 2020, 17, 5306. [Google Scholar] [CrossRef] [PubMed]
- Honma, K.; Honma, S.; Kohsaka, M.; Fukuda, N. Seasonal variation in the human circadian rhythm: Dissociation between sleep and temperature rhythm. Am. J. Physiol. 1992, 262, R885–R891. [Google Scholar] [CrossRef]
- Riccobono, G.; Iannitelli, A.; Pompili, A.; Iorio, C.; Stratta, P.; Rossi, R.; Bersani, G.; Pacitti, F. Night Eating Syndrome, circadian rhythms and seasonality: A study in a population of Italian university students. Riv. Psichiatr. 2020, 55, 47–52. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 299) | Good Sleep Quality (n = 182; 60.9%) | Poor Sleep Quality (n = 117; 39.1%) | p | |
|---|---|---|---|---|
| Maternal Characteristics | Mean (SD) | Mean (SD) | Mean (SD) | |
| PSQI score | 5.43 (2.81) | 3.60 (1.20) | 8.27 (2.15) | <0.001 |
| Gestational age, weeks | 20.36 (0.54) | 20.34 (0.54) | 20.38 (0.54) | 0.557 |
| Age, years | 31.09 (4.24) | 31.32 (4.28) | 30.73 (4.17) | 0.236 |
| Education, years | 14.29 (2.52) | 14.38 (2.59) | 14.15 (2.39) | 0.430 |
| Pre-pregnancy body mass index, kg/m2 | 22.89 (4.14) | 22.22 (3.90) | 23.92 (4.32) | <0.001 |
| n (%) | n (%) | n (%) | ||
| Ethnicity | 0.001 | |||
| Chinese | 245 (81.9) | 160 (87.9) | 85 (72.7) | |
| Non-Chinese | 54 (18.1) | 22 (12.1) | 32 (27.4) | |
| Employment status | 0.240 | |||
| Unemployed | 47 (15.7) | 25 (13.7) | 22 (18.0) | |
| Employed | 252 (84.3) | 157 (86.3) | 95 (81.2) | |
| Working overtime | 0.551 | |||
| <3 times per week | 255 (85.3) | 157 (86.3) | 98 (83.8) | |
| ≥3 times per week | 44 (14.7) | 25 (13.7) | 19 (16.2) | |
| Negative emotion | <0.001 | |||
| No | 168 (56.2) | 128 (70.3) | 40 (34.2) | |
| Yes | 131 (43.8) | 54 (29.7) | 77 (65.8) |
| Model 1 a | Model 2 b | Model 3 c | Model 4 d | |
|---|---|---|---|---|
| Nocturnal Lifestyle Behaviour | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) |
| Meal intake after 8 p.m. | 1.75 (1.32, 2.33) | 1.66 (1.25, 2.21) | 1.51 (1.12, 2.04) | 1.33 (1.00, 1.78) |
| Moderate-to-vigorous physical activity after 7 p.m. | 0.90 (0.62, 1.29) | 0.84 (0.60, 1.17) | 0.85 (0.61, 1.18) | 0.91 (0.67, 1.24) |
| Screen viewing >1 h before bedtime | 1.20 (0.83, 1.74) | 1.16 (0.80, 1.69) | 1.12 (0.77, 1.63) | 1.02 (0.70, 1.48) |
| Artificial light exposure ≥5 lux between 2 and 4 a.m. | 1.99 (1.51, 2.61) | 1.79 (1.36, 2.35) | 1.63 (1.24, 2.13) | 1.34 (1.02, 1.76) |
| Model 1 a | Model 2 b | Model 3 c | Model 4 d | |
|---|---|---|---|---|
| Nocturnal Lifestyle Behaviour | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) |
| Meal intake after 8 p.m. | 1.21 (0.58, 1.85) | 1.03 (0.41, 1.65) | 0.68 (0.03, 1.32) | 0.36 (−0.24, 0.97) |
| Moderate-to-vigorous physical activity after 7 p.m. | 0.07 (−0.71, 0.85) | −0.11 (−0.85, 0.64) | −0.16 (−0.90, 0.58) | −0.01 (−0.70, 0.68) |
| Screen viewing >1 h before bedtime | 0.33 (−0.44, 1.11) | 0.27 (−0.47, 1.01) | 0.24 (−0.51, 0.99) | −0.01 (−0.70, 0.69) |
| Artificial light exposure ≥5 lux between 2 and 4 a.m. | 2.45 (1.51, 3.39) | 2.22 (1.27, 3.17) | 1.99 (1.04, 2.94) | 1.51 (0.61, 2.41) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ku, C.W.; Loo, R.S.X.; Tiong, M.M.Y.; Eng, S.Y.C.; Cheung, Y.B.; Ong, L.S.; Tan, K.H.; Chong, M.F.-F.; Chan, J.K.Y.; Yap, F.; et al. Nocturnal Lifestyle Behaviours and Risk of Poor Sleep during Pregnancy. Nutrients 2022, 14, 2348. https://doi.org/10.3390/nu14112348
Ku CW, Loo RSX, Tiong MMY, Eng SYC, Cheung YB, Ong LS, Tan KH, Chong MF-F, Chan JKY, Yap F, et al. Nocturnal Lifestyle Behaviours and Risk of Poor Sleep during Pregnancy. Nutrients. 2022; 14(11):2348. https://doi.org/10.3390/nu14112348
Chicago/Turabian StyleKu, Chee Wai, Rachael Si Xuan Loo, Michelle Mei Ying Tiong, Sing Yee Clara Eng, Yin Bun Cheung, Lay See Ong, Kok Hian Tan, Mary Foong-Fong Chong, Jerry Kok Yen Chan, Fabian Yap, and et al. 2022. "Nocturnal Lifestyle Behaviours and Risk of Poor Sleep during Pregnancy" Nutrients 14, no. 11: 2348. https://doi.org/10.3390/nu14112348
APA StyleKu, C. W., Loo, R. S. X., Tiong, M. M. Y., Eng, S. Y. C., Cheung, Y. B., Ong, L. S., Tan, K. H., Chong, M. F.-F., Chan, J. K. Y., Yap, F., & Loy, S. L. (2022). Nocturnal Lifestyle Behaviours and Risk of Poor Sleep during Pregnancy. Nutrients, 14(11), 2348. https://doi.org/10.3390/nu14112348






