Health-Related Quality of Life in Spanish Schoolchildren and Its Association with the Fitness Status and Adherence to the Mediterranean Diet
Abstract
:1. Introduction
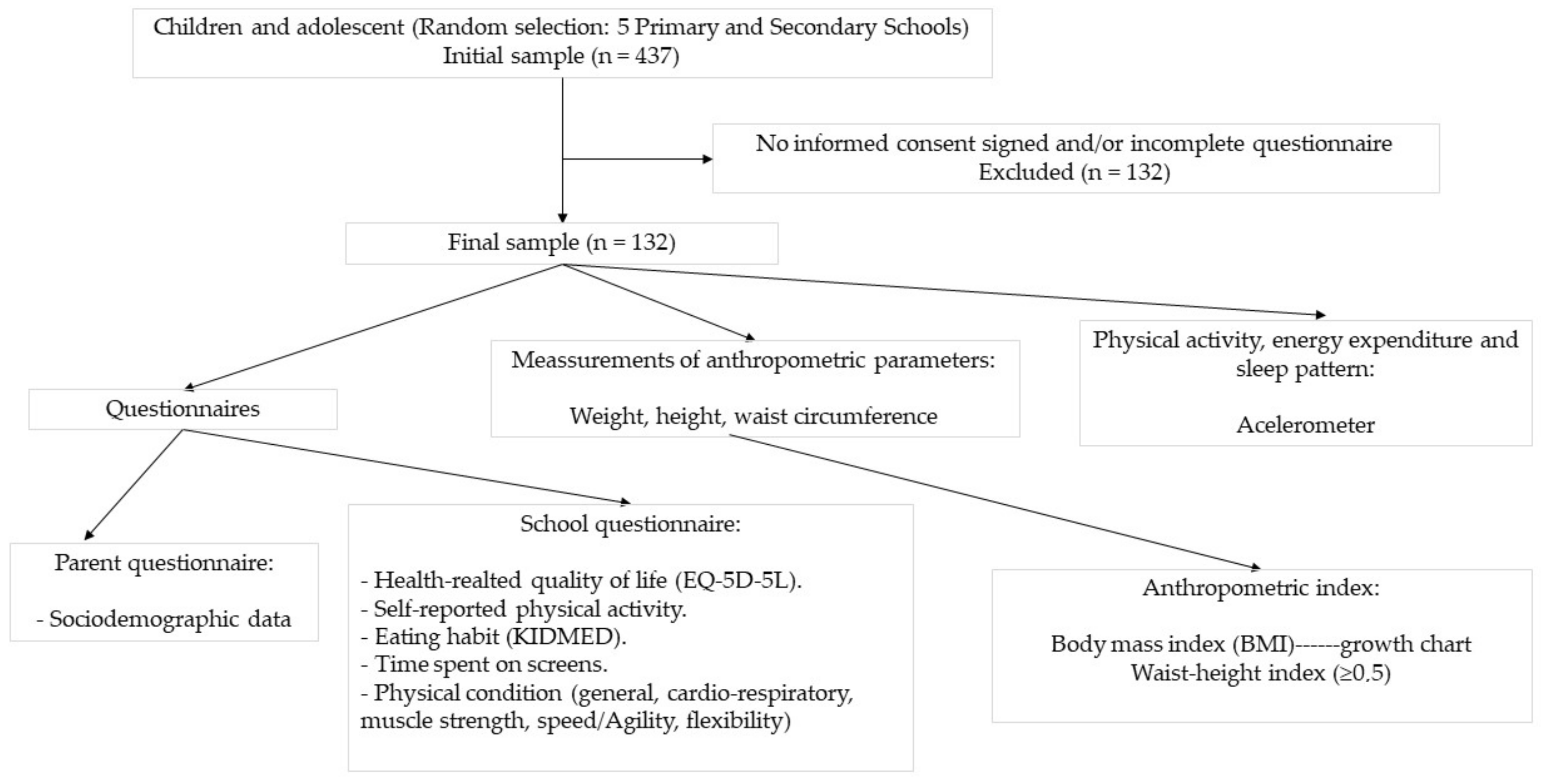
2. Materials and Methods
2.1. Design and Subjects
2.2. Questionnaires
2.2.1. Parent Questionnaire, Study Information Sheet, and Informed Consent
2.2.2. School Questionnaire
- Health-related quality of life: Questions from the EQ-5D-5L questionnaire (EuroQol-5 Dimensions-5 levels), which will be discussed in depth later;
- Self-reported physical activity habits;
- Eating habits: Questionnaire of 16 quality questions of the Mediterranean diet in childhood and adolescence on which the KIDMED index [20] is based, which we will also delve into later;
- Time spent on screens;
- Hours of sleep and quality of rest;
- Questions about physical condition (general, cardio-respiratory, muscle strength, speed/agility, flexibility).
2.3. Meassurement of Anthropometric Parameters
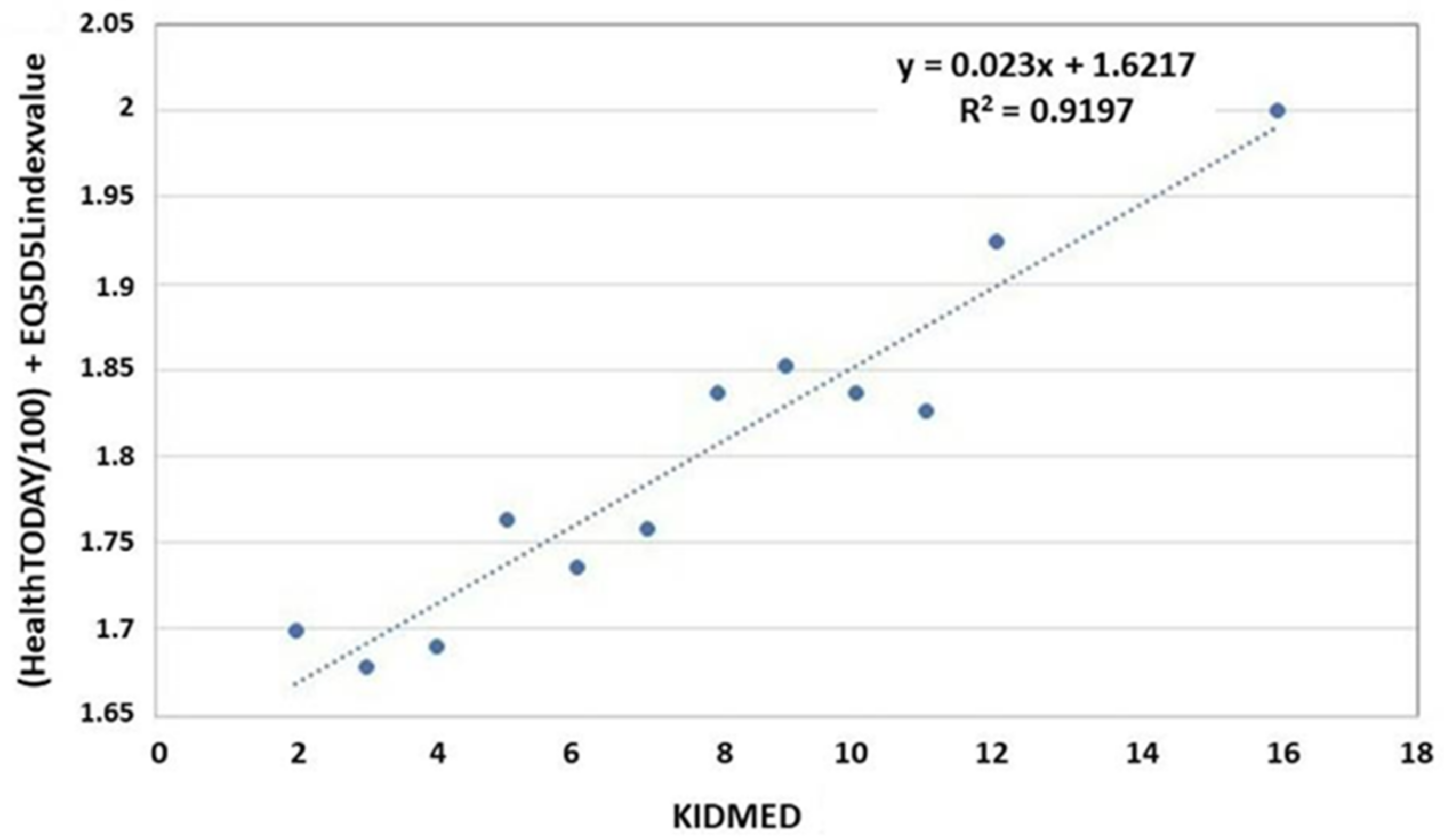
2.4. Adherence to the Mediterranean Diet
2.5. Physical Activity, Energy Expenditure, and Sleep Pattern
2.6. Health-Related Quality of Life
2.7. Statistics
3. Results
3.1. Sociodemographic Characteristics of Parent and Children and Answers to the EQ-5D-5L According to Health-Related Quality of Life
3.2. Health Parameters and Health-Related Behaviours, according to Health-Related Quality of Life
3.3. Fitness Status of Children according to Life Quality
3.4. Association between the Fitness Status of Children and Their Health-Related Quality of Life
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bowling, A. Measuring Disease: A Review of Disease Specific Quality of Life Measurement Scales Maidenhead; Open University Press: Berkshire, UK, 1995. [Google Scholar]
- Dueñas, M.; Ramirez, C.; Arana, R.; Failde, I. Gender differences and determinants of health related to quality of life in coronary patients: A follow up studio. BMC Cardiovasc. Disord. 2011, 11, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Achat, H.; Kawachi, I.; Levine, S.; Berkey, C.; Coakley, E.; Colditz, G. Social networks, stress and health-related quality of life. Qual. Life Res. 1998, 7, 735–750. [Google Scholar] [CrossRef] [PubMed]
- Craig, B.M.; Pickard, A.S.; Lubetkin, E.I. Health problems are more common, but less severe when measured using newer EQ-5D versions. J. Clin. Epidemiol. 2014, 67, 93–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Janabi, H.; van Exel, J.; Brouwer, W.; Coast, J. A Framework for Including Family Health Spillovers in Economic Evaluation. Med. Decis. Mak. 2016, 36, 176–186. [Google Scholar] [CrossRef] [Green Version]
- Ferrans, C.E.; Zerwic, J.J.; Wilbur, J.E.; Larson, J.L. Conceptual Model of Health-Related Quality of Life. J. Nurs. Sch. 2005, 37, 336–342. [Google Scholar] [CrossRef]
- Oster, C.; Gransbury, B.; Anderson, D.; Martin, V.; Pawel, S.; Leibbrandt, R. Development and validation of a self-report social determinants of health questionnaire in Australia. Int. Health Promot. 2022. ahead of print. [Google Scholar] [CrossRef]
- Kanjrawi, A.A.; Mathers, L.; Webster, S.; Corte, T.J.; Carey, S. Nutritional status and quality of life in interstitial lung disease: A prospective cohort study. BMC Pulm. Med. 2021, 21, 51. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [Green Version]
- Bundhun, D.; Rampadarath, S.; Puchooa, D.; Jeewon, R. Dietary intake and lifestyle behaviors of children in Mauritius. Heliyon 2018, 4, e00546. [Google Scholar] [CrossRef] [Green Version]
- Sharma, S.; Arain, M.; Mathur, P.; Rais, A.; Nel, W.; Sandhu, R.; Haque, M.; Johal, L. Maturation of the adolescent brain. Neuropsychiatr. Dis. Treat. 2013, 9, 449–461. [Google Scholar] [CrossRef] [Green Version]
- Ferrer-Cascales, R.; Albaladejo-Blázquez, N.; Ruiz-Robledillo, N.; Clement-Carbonell, V.; Sánchez-SanSegundo, M.; Zaragoza-Martí, A. Higher Adherence to the Mediterranean Diet is Related to More Subjective Happiness in Adolescents: The Role of Health-Related Quality of Life. Nutrients 2019, 11, 698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Cheung, P.W.H.; Wong, C.K.H.; Samartzis, D.; Luk, K.D.K.; Lam, C.L.K.; Cheung, K.M.C.; Cheung, J.P.Y. Psychometric validation of the EuroQoL 5-Dimension 5-Level (EQ-5D-5L) in Chinese patients with adolescent idiopathic scoliosis. Scoliosis Spinal Disord. 2016, 11, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fardell, J.E.; Wakefield, C.E.; Lourenco, R.D.A.; Signorelli, C.; McCarthy, M.; McLoone, J.; Osborn, M.; Gabriel, M.; Anazodo, A.; Alvaro, F.; et al. Long-term health-related quality of life in young childhood cancer survivors and their parents. Pediatr. Blood Cancer 2021, 68, e29398. [Google Scholar] [CrossRef] [PubMed]
- Hendriksz, C.J.; Lavery, C.; Coker, M.; Ucar, S.K.; Jain, M.; Bell, L.; Lampe, C. Burden of disease in patients with Morquio A syndrome: Results from an international patient-reported outcomes survey. Orphanet J. Rare Dis. 2014, 9, 32. [Google Scholar] [CrossRef] [Green Version]
- Oldenburg, J.; Tran, H.; Peyvandi, F.; Núñez, R.; Trask, P.; Chebon, S.; Mahlangu, J.N.; Lehle, M.; Jiménez-Yuste, V.; von Mackensen, S. Health-related quality of life and health status in adolescent and adult people with haemophilia A without factor VIII inhibitors—A non-interventional study. Haemophilia 2021, 27, 398–407. [Google Scholar] [CrossRef]
- Pérez-Sousa, M.; Olivares, P.R.; Ramírez-Vélez, R.; Gusi, N. Comparison of the Psychometric Properties of the EQ-5D-3L-Y and EQ-5D-5L-Y Instruments in Spanish Children and Adolescents. Value Health 2021, 24, 1799–1806. [Google Scholar] [CrossRef]
- Gasol Fundation. Estudio PASOS. Available online: https://www.gasolfoundation.org/es/estudio-pasos/ (accessed on 5 May 2022).
- Serra, L.; Aranceta, J. Alimentación Infantil y Juvenil; Estudio enKid Barcelona: Masson, SA, USA, 2002. [Google Scholar]
- Organización Mundial de la Salud. Manual Step. Guía Para Mediciones Físicas (STEP 2). Available online: https://www.who.int/ncds/surveillance/steps/Parte3_Seccion4.pdf?ua=1 (accessed on 5 May 2022).
- Fernández, C.; Lorenzo, H.; Vrotsou, K.; Aresti, U.; Rica, I.; Sánchez, E. Curvas y Tablas de Crecimiento (Estudio Transversal). 2011. Available online: https://www.fundacionorbegozo.com/wp-content/uploads/pdf/estudios_2011.pdf (accessed on 5 May 2022).
- Taylor, R.W.; Williams, S.M.; Grant, A.M.; Taylor, B.; Goulding, A. Predictive Ability of Waist-to-Height in Relation to Adiposity in Children Is Not Improved With Age and Sex-Specific Values. Obesity 2011, 19, 1062–1068. [Google Scholar] [CrossRef]
- Freedson, P.S.; Melanson, E.; Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef]
- Freedson, P.; Bowles, H.; Troiano, R.; Haskell, W. Assessment of physical activity using wearable monitors: Recommendations for monitor calibration and use in the field. Med. Sci. Sports Exerc. 2012, 44 (Suppl. 1), S1–S4. [Google Scholar] [CrossRef] [Green Version]
- The Euroqol Group. EuroQol–A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Brooks, R. EuroQol: The current state of play. Health Policy 1996, 37, 53–72. [Google Scholar] [CrossRef]
- Welie, A.G.; Stolk, E.; Mukuria, C.; Belay, Y.B.; Krahn, M.D.; Sander, B.; Gebretekle, G.B. Reliability and validity of using EQ-5D-5L among healthy and adolescents with major mental health disorders in Ethiopia. Eur. J. Health Econ. 2022. ahead of print. [Google Scholar] [CrossRef]
- Fitzpatrick, R.; Davey, C.; Buxton, M.; Jones, D. Evaluating patient-based outcome measures for use in clinical trials. Health Tchnol. Assess. 1998, 2, 1–74. [Google Scholar] [CrossRef] [Green Version]
- Torrance, G. Measurement of health state utilities for economic appraisal. J. Health Econ. 1986, 5, 1–30. [Google Scholar] [CrossRef]
- Cheung, P.; Ho Wong, C.; Lau, S.; Cheung, J. Responsiveness of the EuroQoL 5-dimension (EQ-5D) in adolescent idiopathic scoliosis. Eur. Spine 2018, 27, 278–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [Green Version]
- Oppe, M.; Devlin, N.J.; van Hout, B.; Krabbe, P.; de Charro, F. A Program of Methodological Research to Arrive at the New International EQ-5D-5L Valuation Protocol. Value Health 2014, 17, 445–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evaristo, O.S.; Moreira, C.; Lopes, L.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Oliveira, A.; Santos, R.; Mota, J. Associations between physical fitness and adherence to the Mediterranean diet with health-related quality of life in adolescents: Results from the LabMed Physical Activity Study. Eur. J. Public Health 2018, 28, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Evaristo, S.; Moreira, C.; Lopes, L.; Oliveira, A.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Santos, R.; Mota, J. Muscular fitness and cardiorespiratory fitness are associated with health-related quality of life: Results from labmed physical activity study. J. Exerc. Sci. Fit. 2019, 17, 55–61. [Google Scholar] [CrossRef]
- Gu, X.; Chang, M.; Solmon, M.A. Physical Activity, Physical Fitness, and Health-Related Quality of Life in School-Aged Children. J. Teach. Phys. Educ. 2016, 35, 117–126. [Google Scholar] [CrossRef]
- Muros, J.; Salvador, F.; Zurita, F.; Gámez, V. The association between healthy lifestyle behaviors and health-related quality of life among adolescents. J. Pediatr. 2017, 93, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Knox, E.; Muros, J.J. Association of lifestyle behaviours with self-esteem through health-related quality of life in Spanish adolescents. Eur. J. Pediatr. 2017, 176, 621–628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiménez, R.; Gargallo, E.; Dalmau, J.; Arriscado, D. Actores asociados a un bajo nivel de actividad física en adolescentes de la Rioja (España). An. Pediatría 2022, 96, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Basterfield, L.; Burn, N.L.; Galna, B.; Batten, H.; Goffe, L.; Karoblyte, G.; Lawn, M.; Weston, K.L. Changes in children’s physical fitness, BMI and health-related quality of life after the first 2020 COVID-19 lockdown in England: A longitudinal study. J. Sports Sci. 2022, 40, 1088–1096. [Google Scholar] [CrossRef] [PubMed]
- Lek, D.; Haveman-Nies, A.; Bezem, J.; Zainalabedin, S.; Schetters-Mouwen, S.; Saat, J.; van Setten, P. Two-year effects of the community-based overweight and obesity intervention program Gezond Onderweg! (GO!) in children and adolescents living in a low socioeconomic status and multi-ethnic district on Body Mass Index-Standard Deviation Score and quality of life. eClinicalMedicine 2021, 42, 101217. [Google Scholar] [PubMed]
- Floody, P.A.D.; Navarrete, F.C.; Mayorga, D.J.; Cofré-Lizama, A.; Guzmán, I.G. The association between children’l food habits, anthropometric parameters and health-related quality of life in Chilean school-age children. Nutr. Hosp. 2019, 36, 1061–1066. [Google Scholar] [CrossRef] [Green Version]
- Zanganeh, M.; Adab, P.; Li, B.; Pallan, M.; Liu, W.J.; Rong, L.; Martin, J.; Cheng, K.K.; Frew, E. Relationship Between Weight Status and Health-Related Quality of Life in School-age Children in China. J. Health Econ. Outcomes Res. 2022, 9, 75–81. [Google Scholar] [CrossRef]
- Basterfield, L.; Burn, N.L.; Galna, B.; Karoblyte, G.; Weston, K.L. The association between physical fitness, sports club participation and body mass index on health-related quality of life in primary school children from a socioeconomically deprived area of England. Prev. Med. Rep. 2021, 24, 101557. [Google Scholar] [CrossRef]
- Mastorci, F.; Piaggi, P.; Doveri, C.; Trivellini, G.; Marinaro, I.; Casu, A.; Pingitore, A.; Vassalle, C. Relationship between Weight Status and Health-Related Quality of Life in a Sample of Early Adolescents from Central and Northern Italy: A Cross-Sectional Study of the AVATAR Project Participants. Int. J. Environ. Res. Public Health 2021, 18, 8782. [Google Scholar] [CrossRef]
- Yackobovitch-Gavan, M.; Nagelberg, N.; Phillip, M.; Ashkenazi-Hoffnung, L.; Hershkovitz, E.; Shalitin, S. The influence of diet and/or exercise and parental compliance on health-related quality of life in obese children. Nutr. Res. 2009, 29, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Shoup, J.A.; Gattshall, M.; Dandamudi, P.; Estabrooks, P. Physical activity, quality of life, and weight status in overweight children. Qual. Life Res. 2008, 17, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Crosbie, A. The Effect of Physical Training in Children With Asthma on Pulmonary Function, Aerobic Capacity and Health-Related Quality of Life: A Systematic Review of Randomized Control Trials. Pediatr. Exerc. Sci. 2012, 24, 472–489. [Google Scholar] [CrossRef] [PubMed]
- Paxton, R.J.; Jones, L.W.; Rosoff, P.M.; Bonner, M.; Ater, J.L.; Demark-Wahnefried, W. Associations between leisure-time physical activity and health-related quality of life among adolescent and adult survivors of childhood cancers. Psycho-Oncology 2010, 19, 997–1003. [Google Scholar] [CrossRef] [Green Version]
- Bize, R.; Johnson, J.; Plotnikoff, R.C. Physical activity level and health-related quality of life in the general adult population: A systematic review. Prev. Med. 2007, 45, 401–415. [Google Scholar] [CrossRef]
- Yun, X.; Hui, L.; Hua, J.; Luo, S.; Wei, J.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar]
- Shin, H.; Jeon, S.; Cho, I. Factors influencing health-related quality of life in adolescent girls: A path analysis using a multi-mediation model. Health Qual. Life Outcomes 2022, 20, 50. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.S.; Turakhia, B.S.; Miller, M.; Johnston, D.; Maddalozzo, J.; Thompson, D.; Trosman, I.; Grandner, M.; Sheldon, S.H.; Ahluwalia, V.; et al. Association of obstructive sleep apnea and total sleep time with health-related quality of life in children undergoing a routine polysomnography: A PROMIS approach. J. Clin. Sleep Med. 2022, 18, 801–808. [Google Scholar] [CrossRef]
- Kenđel Jovanović, G.; Dragaš Zubalj, N.; Klobučar Majanović, S.; Rahelić, D.; Rahelić, V.; Vučak Lončar, J.; Pavičić Žeželj, S. The Outcome of COVID-19 Lockdown on Changes in Body Mass Index and Lifestyle among Croatian Schoolchildren: A Cross-Sectional Study. Nutrients 2021, 13, 3788. [Google Scholar] [CrossRef]
- Pujia, R.; Ferro, Y.; Maurotti, S.; Khoory, J.; Gazzaruso, C.; Pujia, A.; Montalcini, T.; Mazza, E. The Effects of COVID-19 on the Eating Habits of Children and Adolescents in Italy: A Pilot Survey Study. Nutrients 2021, 13, 2641. [Google Scholar] [CrossRef]
- Chi, X.; Liang, K.; Chen, S.T.; Huang, Q.; Huang, L.; Yu, Q.; Zou, L. Mental health problems among Chinese adolescents during the COVID-19: The importance of nutrition and physical activity. Int. J. Clin. Health Psychol. 2021, 21, 100218. [Google Scholar] [CrossRef] [PubMed]
- Carrillo, P.; García, F. Anxiety levels according to weight status and diet quality during alarm state in primary school children. Nutr. Clín. Diet. Hosp. 2020, 40, 53–59. [Google Scholar]
- López-Bueno, R.; López-Sánchez, G.F.; Casajús, J.A.; Calatayud, J.; Gil-Salmerón, A.; Grabovac, I.; Smith, L. Health-Related Behaviors Among School-Aged Children and Adolescents During the Spanish Covid-19 Confinement. Pediatría Front. 2020, 8, 573. [Google Scholar] [CrossRef] [PubMed]
- Ventura, P.S.; Ortigoza, A.F.; Castillo, Y.; Bosch, Z.; Casals, S.; Girbau, C.; Siurana, J.M.; Arce, A.; Torres, M.; Herrero, F.J. Children’s Health Habits and COVID-19 Lockdown in Catalonia: Implications for Obesity and Non-Communicable Diseases. Nutrients 2021, 13, 1657. [Google Scholar] [CrossRef] [PubMed]
- Łuszczki, E.; Bartosiewicz, A.; Pezdan-Śliż, I.; Kuchciak, M.; Jagielski, P.; Oleksy, Ł.; Dereń, K. Children’s Eating Habits, Physical Activity, Sleep, and Media Usage before and during COVID-19 Pandemic in Poland. Nutrients 2021, 13, 2447. [Google Scholar] [CrossRef] [PubMed]
| Group 1 § (n = 106) | Group 2 § (n = 100) | Group 3 § (n = 99) | p-Value ‡ | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Parent age (years) | 44.65 (4.7) | 44.77 (5.5) | 43.81 (7.0) | >0.05 |
| Parent BMI (kg/m2) | 25.56 (4.4) | 24.35 (4.7) | 25.25 (4.0) | >0.05 |
| Child age | 10.42 (1.7) | 10.47 (1.4) | 11.04 (1.9) | 0.016 |
| n (%) | n (%) | n (%) | ||
| Child gender (female) | 54 (50.9) | 49 (49.0) | 41 (41.4) | >0.05 |
| Parent education level | >0.05 | |||
| Illiterate | 2 (1.9) | 2 (2.0) | 0 (0.0) | |
| Primary school | 14 (13.2) | 7 (7.0) | 4 (4.0) | |
| Middle school | 10 (9.4) | 6 (6.0) | 12 (12.1) | |
| Vocational training | 19 (17.9) | 18 (18.0) | 17 (17.2) | |
| High school | 9 (8.5) | 13 (13.0) | 15 (15.2) | |
| University studies | 38 (35.9) | 35 (35.0) | 27 (27.3) | |
| Not reported | 14 (13.2) | 19 (19.0) | 24 (24.3) | |
| Parent employment status | >0.05 | |||
| Homemaker | 7 (6.6) | 4 (4.0) | 4 (4.0) | |
| Working | 77 (72.7) | 70 (70.0) | 59 (59.6) | |
| Unemployed | 7 (6.6) | 4 (4.0) | 8 (8.1) | |
| Others | 1 (0.9) | 3 (3.0) | 4 (4.0) | |
| Not reported | 14 (13.2) | 19 (19.0) | 24 (24.2) | |
| Parent smoking habit | >0.05 | |||
| Current smoker | 17 (16.0) | 11 (11.0) | 20 (20.2) | |
| Former smoker (0–1 year) | 2 (1.9) | 0 (0.0) | 3 (3.0) | |
| Former smoker (1–5 years) | 5 (4.7) | 3 (3.0) | 6 (6.1) | |
| Former smoker (>5 years) | 17 (16.0) | 16 (16.0) | 13 (13.1) | |
| Never smoked | 51 (48.2) | 52 (52.0) | 32 (32.3) | |
| Not reported | 14 (13.2) | 18 (18.0) | 25 (25.3) |
| Group 1 § (n = 106) | Group 2 § (n = 100) | Group 3 § (n = 99) | p-Value ‡ | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Health Index (HI) | 98.3 (2.1) a,b | 88.9 (5.8) a,c | 69.2 (16.0) b,c | <0.001 |
| Domains of the questionnaire | n (%) | n (%) | n (%) | |
| 1. Mobility (walking) TODAY | <0.001 | |||
| I can’t/Very bad | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Many problems/Bad | 0 (0.0) | 0 (0.0) | 1 (1.0) | |
| Quite a few problems/Acceptable | 0 (0.0) | 0 (0.0) | 1 (1.0) | |
| Any problem/Good | 0 (0.0) | 2 (2.0) | 20 (20.2) | |
| No problems/Very good | 106 (100.0) | 98 (98.0) | 77 (77.8) | |
| 2. Self-care TODAY | 0.001 | |||
| I can’t/Very bad | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Many problems/Bad | 0 (0.0) | 0 (0.0) | 1 (1.0) | |
| Quite a few problems/Acceptable | 0 (0.0) | 0 (0.0) | 1 (1.0) | |
| Any problem/Good | 0 (0.0) | 2 (2.0) | 11 (11.1) | |
| No problems/Very good | 106 (100.0) | 98 (98.0) | 86 (86.9) | |
| 3. Daily activities TODAY | <0.001 | |||
| I can’t/Very bad | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Many problems/Bad | 0 (0.0) | 0 (0.0) | 2 (2.0) | |
| Quite a few problems/Acceptable | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Any problem/Good | 0 (0.0) | 7 (7.0) | 23 (23.3) | |
| No problems/Very good | 106 (100.0) | 93 (93.0) | 74 (74.7) | |
| 4. Pain/discomfort or feeling bad TODAY | <0.001 | |||
| I can’t/Very bad | 0 (0.0) | 0 (0.0) | 2 (2.0) | |
| Many problems/Bad | 0 (0.0) | 0 (0.0) | 2 (2.0) | |
| Quite a few problems/Acceptable | 0 (0.0) | 1 (1.0) | 3 (3.0) | |
| Any problem/Good | 0 (0.0) | 12 (12.0) | 26 (26.3) | |
| No problems/Very good | 106 (100.0) | 87 (87.0) | 66 (66.7) | |
| 5. Concerns/sadness TODAY | <0.001 | |||
| I can’t/Very bad | 0 (0.0) | 0 (0.0) | 3 (3.0) | |
| Many problems/Bad | 0 (0.0) | 0 (0.0) | 3 (3.0) | |
| Quite a few problems/Acceptable | 0 (0.0) | 4 (4.0) | 4 (4.0) | |
| Any problem/Good | 8 (7.5) | 18 (18.0) | 22 (22.3) | |
| No problems/Very good | 98 (92.5) | 78 (78.0) | 67 (67.7) | |
| 6. Overall health category rating scales (CRS) | <0.001 | |||
| Poor (<53) | 0 (0.0) | 0 (0.0) | 22 (22.2) | |
| Fair (≥53 y <76) | 0 (0.0) | 0 (0.0) | 47 (47.5) | |
| Good (≥76 y <80) | 0 (0.0) | 1 (1.0) | 1 (1.0) | |
| Very Good (≥80 y <90) | 0 (0.0) | 38 (38.0) | 18 (18.2) | |
| Excellent (≥90) | 106 (100.0) | 61 (61.0) | 11 (11.1) |
| Group 1 § (n= 106) | Group 2 § (n = 100) | Group 3 § (n = 99) | p-Value ‡ | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Energy expenditure (kcal/day) * | 568.9 (332.9) | 491.8 (97.25) | 866 (558.9) | >0.05 |
| Physical activity (minute/day) * | ||||
| Sedentary | 474.2 (183.7) | 563.4 (73.7) | 588.5 (33.4) | >0.05 |
| Light | 424.8 (149) | 476.2 (50.2) | 499.5 (56.8) | >0.05 |
| Moderate to vigorous | 256.5 (78.9) | 265.8 (52.8) | 257.3 (73.4) | >0.05 |
| Sleeping pattern * | ||||
| Sleep efficiency (%/day) | 92.3 (3.0) | 91 (4.0) | 92.7 (3.2) | >0.05 |
| Sleeping time (min/day) | 399.1 (99.6) | 408.6 (102.9) | 400.7 (33.1) | >0.05 |
| n (%) | n (%) | n (%) | ||
| BMI percentile * | >0.05 | |||
| Underweight | 6 (7.7) | 8 (11.4) | 5 (8.2) | |
| Normal weight | 55 (70.5) | 48 (68.6) | 40 (65.6) | |
| Overweight | 12 (15.4) | 8 (11.4) | 12 (19.7) | |
| Obesity | 5 (6.4) | 6 (8.6) | 4 (6.5) | |
| Abdominal obesity (yes) * | 11 (55) | 12 (50) | 4 (22) | >0.05 |
| MedDiet adherence | 0.001 | |||
| Low adherence | 3 (2.8) | 3 (3.0) | 9 (9.1) | |
| Medium adherence | 28 (26.4) | 42 (42.0) | 47 (47.5) | |
| High adherence | 75 (70.8) | 55 (55.0) | 43 (43.4) |
| Group 1 § (n = 106) | Group 2 § (n = 100) | Group 3 § (n = 99) | p-Value ‡ | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Muscle strength | 0.001 | |||
| Very bad | 0 (0) | 0 (0) | 2 (2.0) | |
| Bad | 4 (3.8) | 2 (2.0) | 5 (5.1) | |
| Acceptable | 10 (9.4) | 19 (19.0) | 31 (31.3) | |
| Good | 45 (42.5) | 49 (49.0) | 36 (36.4) | |
| Very good | 47 (44.3) | 30 (30.0) | 25 (25.2) | |
| Speed and agility | 0.005 | |||
| Very bad | 1 (0.9) | 0 (0) | 2 (2.0) | |
| Bad | 3 (2.8) | 2 (2.0) | 8 (8.1) | |
| Acceptable | 10 (9.4) | 13 (13.0) | 17 (17.2) | |
| Good | 40 (37.7) | 49 (49.0) | 50 (50.5) | |
| Very good | 52 (49.0) | 36 (36.0) | 22 (22.2) | |
| Flexibility | 0.004 | |||
| Very bad | 3 (2.8) | 4 (4.0) | 6 (6.1) | |
| Bad | 7 (6.6) | 11 (11.0) | 12 (12.1) | |
| Acceptable | 26 (24.5) | 27 (27.0) | 35 (35.4) | |
| Good | 31 (29.3) | 39 (39.0) | 23 (23.2) | |
| Very good | 39 (36.8) | 19 (19.0) | 23 (23.2) | |
| Pain/discomfort | 0.010 | |||
| None | 106 (100) | 92 (92.0) | 83 (83.8) | |
| Some | 0 (0) | 6 (6.0) | 14 (14.2) | |
| A lot | 0 (0) | 2 (2.0) | 2 (2.0) | |
| Concerns/sadness | 0.010 | |||
| None | 106 (100) | 84 (84.0) | 74 (74.8) | |
| Some | 0 (0) | 15 (15.0) | 24 (24.2) | |
| A lot | 0 (0) | 1 (1.0) | 1 (1.0) |
| Group 1 § (n =106) | Group 2 § (n = 100) | Group 3 § (n = 99) | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) p-Value | OR (95% CI) p-Value | |
| Muscle strength | 1.00 (ref.) | 0.535 (0.303–0.955) 0.034 | 0.424 (0.234–0.768) 0.005 |
| Speed and Agility | 1.00 (ref.) | 0.584 (0.334–1.021) 0.059 | 0.297 (0.162–0.545) < 0.001 |
| Flexibility | 1.00 (ref.) | 0.403 (0.213–0.762) 0.005 | 0.520 (0.282–0.958) 0.036 |
| Pain/discomfort | 1.00 (ref.) | 1.506 (0.866–2.620) 0.147 | 1.065 (0.616–1.843) 0.821 |
| Concerns/sadness | 1.00 (ref.) | 1.053 (0.608–1.825) 0.853 | 0.916 (0.529–1.586) 0.753 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pastor, R.; Bouzas, C.; Albertos, I.; García, C.; García, Á.; Prieto, T.; Velázquez, J.; Sánchez-Jiménez, E.; Rodríguez, R.; Martín, F.J.; et al. Health-Related Quality of Life in Spanish Schoolchildren and Its Association with the Fitness Status and Adherence to the Mediterranean Diet. Nutrients 2022, 14, 2322. https://doi.org/10.3390/nu14112322
Pastor R, Bouzas C, Albertos I, García C, García Á, Prieto T, Velázquez J, Sánchez-Jiménez E, Rodríguez R, Martín FJ, et al. Health-Related Quality of Life in Spanish Schoolchildren and Its Association with the Fitness Status and Adherence to the Mediterranean Diet. Nutrients. 2022; 14(11):2322. https://doi.org/10.3390/nu14112322
Chicago/Turabian StylePastor, Rosario, Cristina Bouzas, Irene Albertos, Carolina García, Ángela García, Teresa Prieto, Jorge Velázquez, Elena Sánchez-Jiménez, Rocío Rodríguez, Francisco Javier Martín, and et al. 2022. "Health-Related Quality of Life in Spanish Schoolchildren and Its Association with the Fitness Status and Adherence to the Mediterranean Diet" Nutrients 14, no. 11: 2322. https://doi.org/10.3390/nu14112322
APA StylePastor, R., Bouzas, C., Albertos, I., García, C., García, Á., Prieto, T., Velázquez, J., Sánchez-Jiménez, E., Rodríguez, R., Martín, F. J., Campón, A. M., & Tur, J. A. (2022). Health-Related Quality of Life in Spanish Schoolchildren and Its Association with the Fitness Status and Adherence to the Mediterranean Diet. Nutrients, 14(11), 2322. https://doi.org/10.3390/nu14112322










