Relationship between Nutritional Status, Body Composition, Muscle Strength, and Functional Recovery in Patients with Proximal Femur Fracture
Abstract
:1. Introduction
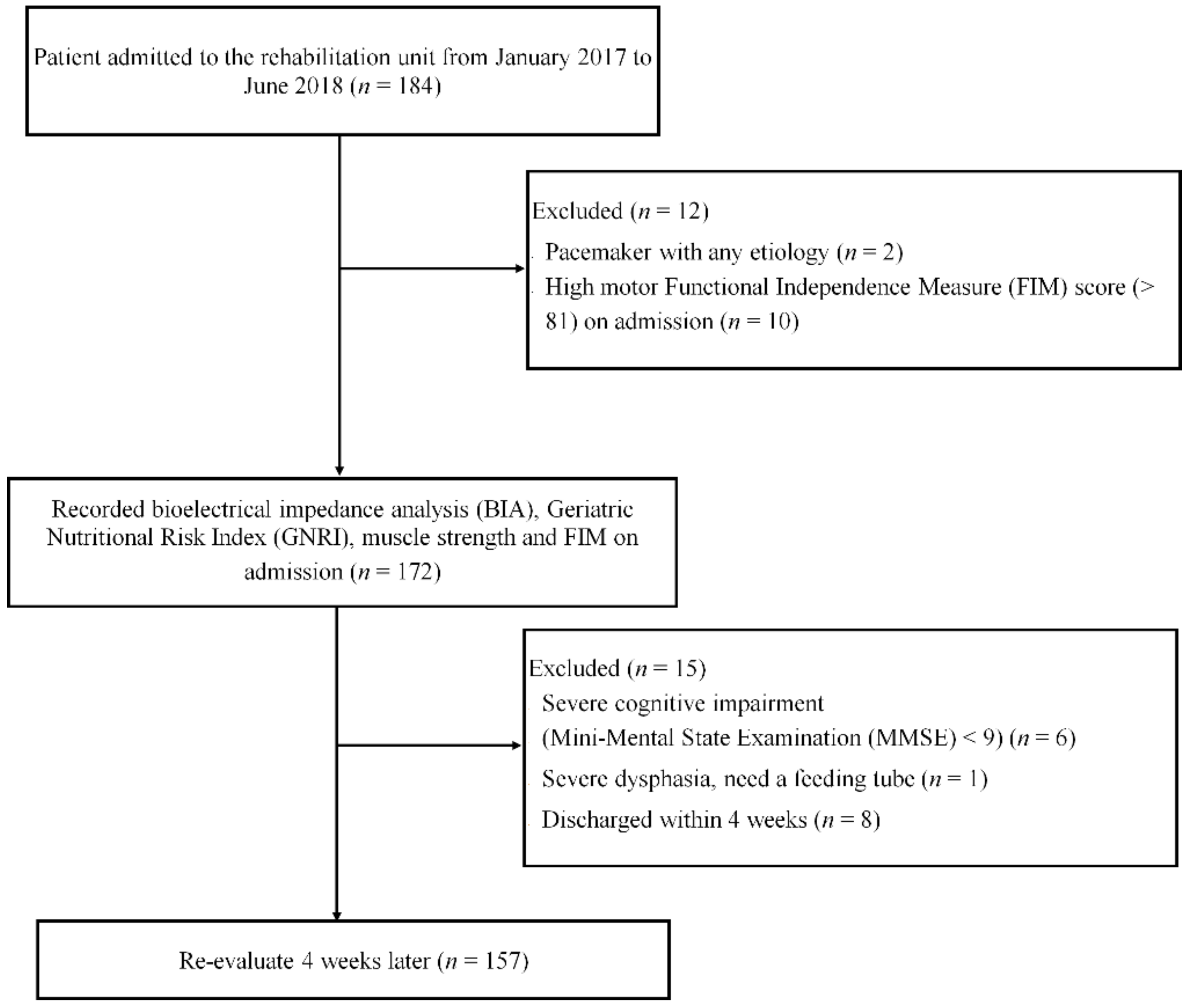
2. Materials and Methods
2.1. Nutritional Status
2.2. Bioelectrical Impedance Analysis (BIA)
2.3. Muscle Strength Assessment
2.4. Functional Measurements
2.5. Statistical Analysis
3. Results
3.1. Descriptive Characteristics
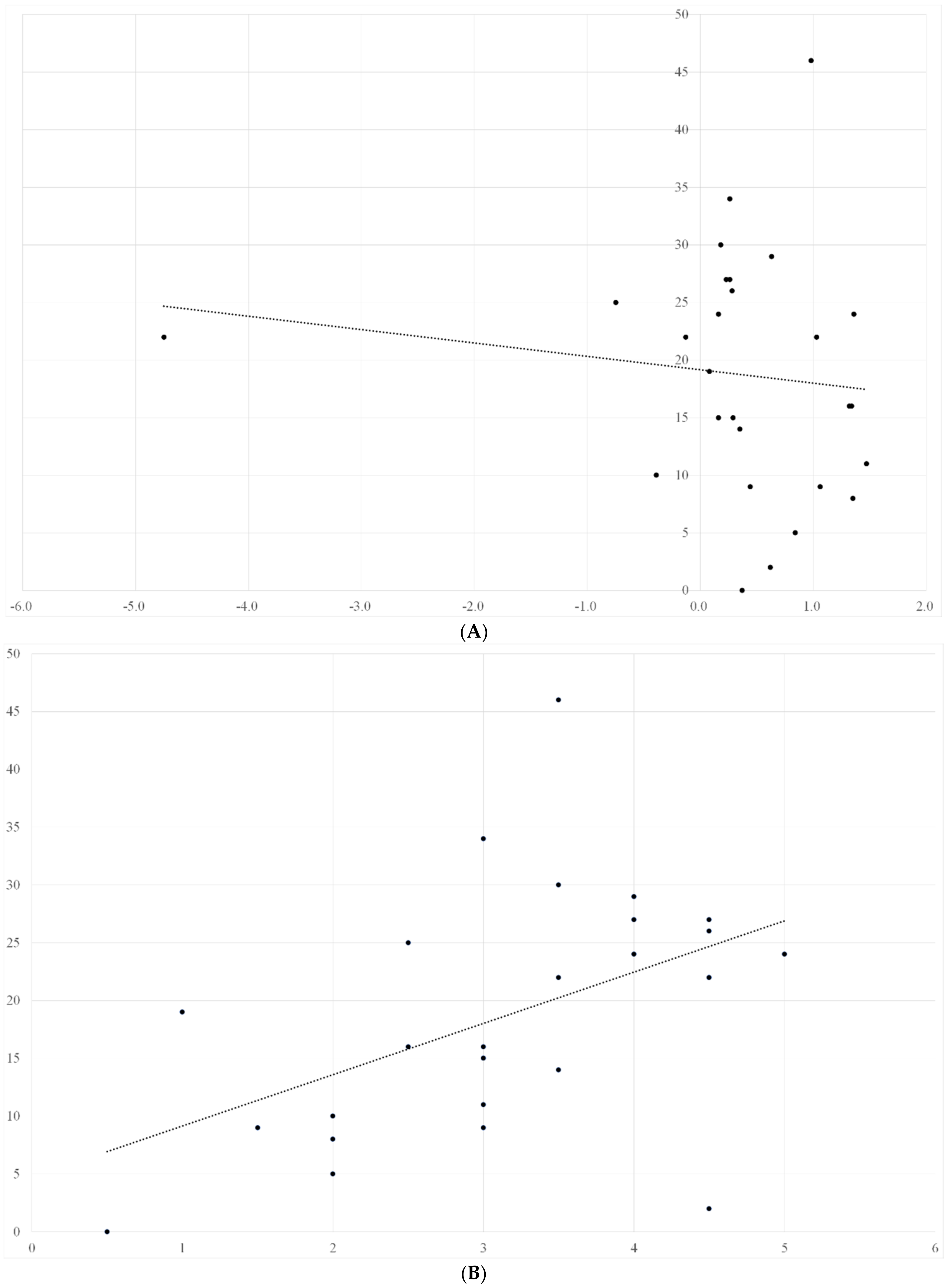
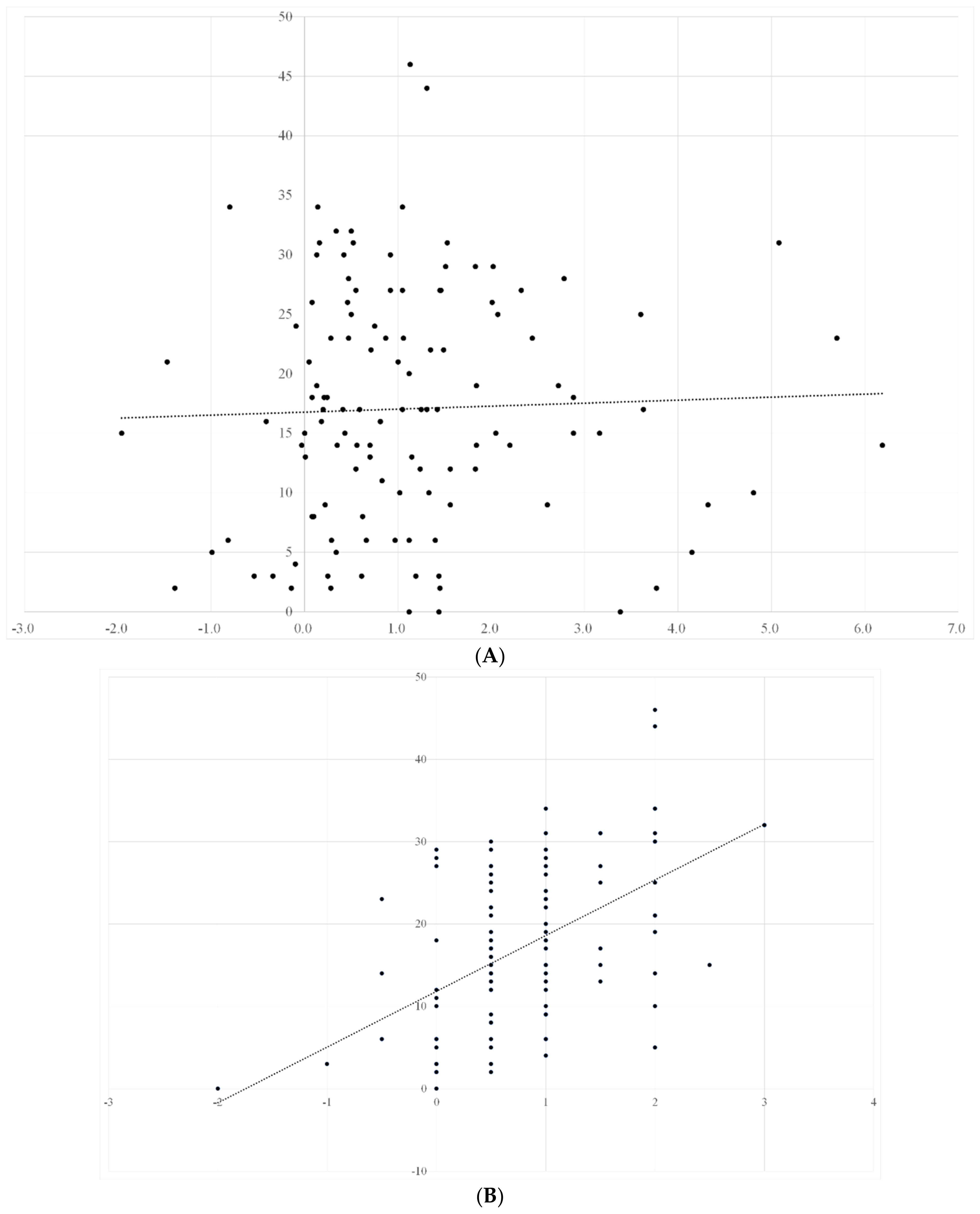
3.2. Univariate Analyses
4. Discussion
4.1. Nutritional Status
4.2. Body Composition
4.3. Muscle Quality
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cooper, C. Bone mass, muscle function and fracture of the proximal femur. Br. J. Hosp. Med. 1989, 42, 277–280. [Google Scholar] [PubMed]
- Fukumoto, Y.; Ikezoe, T.; Yamada, Y.; Tsukagoshi, R.; Nakamura, M.; Takagi, Y.; Kimura, M.; Ichihashi, N. Age-Related Ultrasound Changes in Muscle Quantity and Quality in Women. Ultrasound Med. Biol. 2015, 41, 3013–3017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ota, M.; Ikezoe, T.; Kato, T.; Tateuchi, H.; Ichihashi, N. Age-related changes in muscle thickness and echo intensity of trunk muscles in healthy women: Comparison of 20–60s age groups. Eur. J. Appl. Physiol. 2020, 120, 1805–1814. [Google Scholar] [CrossRef] [PubMed]
- Tomeleri, C.M.; Cavalcante, E.F.; Antunes, M.; Nabuco, H.C.G.; de Souza, M.F.; Teixeira, D.C.; Gobbo, L.A.; Silva, A.M.; Cyrino, E.S. Phase Angle Is Moderately Associated with Muscle Quality and Functional Capacity, Independent of Age and Body Composition in Older Women. J. Geriatr. Phys. Ther. 2019, 42, 281–286. [Google Scholar] [CrossRef]
- Beaupre, L.A.; Binder, E.F.; Cameron, I.D.; Jones, C.A.; Orwig, D.; Sherrington, C.; Magaziner, J. Maximising functional recovery following hip fracture in frail seniors. Best Pract. Res. Clin. Rheumatol. 2013, 27, 771–788. [Google Scholar] [CrossRef] [Green Version]
- Krivickas, L.S.; Dorer, D.J.; Ochala, J.; Frontera, W.R. Relationship between force and size in human single muscle fibres. Exp. Physiol. 2011, 96, 539–547. [Google Scholar] [CrossRef]
- Visser, M.; Harris, T.B.; Fox, K.M.; Hawkes, W.; Hebel, J.R.; YuYahiro, J.; Michael, R.; Zimmerman, S.I.; Magaziner, J. Change in Muscle Mass and Muscle Strength After a Hip Fracture: Relationship to Mobility Recovery. J. Gerontol. Ser. A 2000, 55, M434–M440. [Google Scholar] [CrossRef]
- Di Monaco, M.; Castiglioni, C. Weakness and Low Lean Mass in Women with Hip Fracture: Prevalence According to the FNIH Criteria and Association with the Short-Term Functional Recovery. J. Geriatr. Phys. Ther. 2017, 40, 80–85. [Google Scholar] [CrossRef]
- Singer, K.P.; Breidahl, P. The Use of Computed Tomography in Assessing Muscle Cross-sectional Area, and the Relationship between Cross-sectional Area and Strength. Aust. J. Physiother. 1987, 33, 75–82. [Google Scholar] [CrossRef] [Green Version]
- Freilich, R.; Kirsner, R.; Byrne, E. Isometric strength and thickness relationships in human quadriceps muscle. Neuromuscul. Disord. 1995, 5, 415–422. [Google Scholar] [CrossRef]
- Fukumoto, Y.; Ikezoe, T.; Yamada, Y.; Tsukagoshi, R.; Nakamura, M.; Mori, N.; Kimura, M.; Ichihashi, N. Skeletal muscle quality assessed from echo intensity is associated with muscle strength of middle-aged and elderly persons. Eur. J. Appl. Physiol. 2012, 112, 1519–1525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akazawa, N.; Harada, K.; Okawa, N.; Tamura, K.; Moriyama, H. Muscle mass and intramuscular fat of the quadriceps are related to muscle strength in non-ambulatory chronic stroke survivors: A cross-sectional study. PLoS ONE 2018, 13, e0201789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris-Love, M.O.; Avila, N.A.; Adams, B.; Zhou, J.; Seamon, B.; Ismail, C.; Zaidi, S.H.; Kassner, C.A.; Liu, F.; Blackman, M.R. The Comparative Associations of Ultrasound and Computed Tomography Estimates of Muscle Quality with Physical Performance and Metabolic Parameters in Older Men. J. Clin. Med. 2018, 7, 340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 601. [Google Scholar] [CrossRef] [Green Version]
- Malafarina, V.; Reginster, J.-Y.; Cabrerizo, S.; Bruyère, O.; Kanis, J.A.; Martinez, J.A.; Zulet, M.A. Nutritional Status and Nutritional Treatment Are Related to Outcomes and Mortality in Older Adults with Hip Fracture. Nutrients 2018, 10, 555. [Google Scholar] [CrossRef] [Green Version]
- Syed-Abdul, M.M.; McClellan, C.L.; Parks, E.J.; Ball, S.D. Effects of a resistance training community programme in older adults. Ageing Soc. 2021, 1–16. [Google Scholar] [CrossRef]
- Wakabayashi, H.; Sakuma, M. Rehabilitation nutrition for sarcopenia with disability: A combination of both rehabilitation and nutrition care management. J. Cachexia Sarcopenia Muscle 2014, 5, 269–277. [Google Scholar] [CrossRef]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.-P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef] [Green Version]
- Janssen, I.; Heymsfield, S.B.; Ross, R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with func-tional impairment and physical disability. J. Am. Geriatr. Soc. 2002, 50, 889–896. [Google Scholar] [CrossRef] [Green Version]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef] [Green Version]
- MacDermid, J.; Solomon, G.; Valdes, K. Clinical Assessment Recommendations, 3rd ed.; American Society of Hand Therapists: Mount Laurel, NJ, USA, 2015. [Google Scholar]
- Granger, C.V.; Hamilton, B.B.; Linacre, J.M.; Heinemann, A.W.; Wright, B.D. Performance Profiles of the Functional Independence Measure. Am. J. Phys. Med. Rehabil. 1993, 72, 84–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haigh, A.T.R. The Use of Outcome Measures in Physical Medicine and Rehabilitation Within Europe. J. Rehabil. Med. 2001, 33, 273–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janssen, I.; Heymsfield, S.B.; Baumgartner, R.N.; Ross, R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. J. Appl. Physiol. 2000, 89, 465–471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kishimoto, M.; Shiude, K.; Tanaka, M.A. A Methodological evaluation of body composition analysis for patients with life-related disorders. J. Jpn. Soc. Nutr. Food Sci. 2009, 62, 253–258. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307. [Google Scholar] [CrossRef]
- Inoue, T.; Misu, S.; Tanaka, T.; Sakamoto, H.; Iwata, K.; Chuman, Y.; Ono, R. Pre-fracture nutritional status is predictive of functional status at discharge during the acute phase with hip fracture patients: A multicenter prospective cohort study. Clin. Nutr. 2017, 36, 1320–1325. [Google Scholar] [CrossRef]
- Deutz, N.E.; Bauer, J.M.; Barazzoni, R.; Biolo, G.; Boirie, Y.; Bosy-Westphal, A.; Cederholm, T.; Cruz-Jentoft, A.J.; Krznariç, Z.; Nair, K.S.; et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the ESPEN Expert Group. Clin. Nutr. 2014, 33, 929–936. [Google Scholar] [CrossRef] [Green Version]
- Tieland, M.; Dirks, M.L.; Van Der Zwaluw, N.; Verdijk, L.B.; Van De Rest, O.; de Groot, L.C.; van Loon, L.J. Protein Supplementation Increases Muscle Mass Gain During Prolonged Resistance-Type Exercise Training in Frail Elderly People: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Am. Med. Dir. Assoc. 2012, 13, 713–719. [Google Scholar] [CrossRef]
- von Haehling, S.; Anker, S.D. Treatment of Cachexia: An Overview of Recent Developments. J. Am. Med. Dir. Assoc. 2014, 15, 866–872. [Google Scholar] [CrossRef] [Green Version]
- Del Fabbro, E. Combination therapy in cachexia. Ann. Palliat. Med. 2019, 8, 59–66. [Google Scholar] [CrossRef]
- Bera, T.K. Bioelectrical Impedance Methods for Noninvasive Health Monitoring: A Review. J. Med. Eng. 2014, 2014, 381251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosaeus, I.; Wilcox, G.; Rothenberg, E.; Strauss, B.J. Skeletal muscle mass in hospitalized elderly patients: Comparison of measurements by single-frequency BIA and DXA. Clin. Nutr. 2014, 33, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Stobäus, N.; Pirlich, M.; Bosy-Westphal, A. Bioelectrical phase angle and impedance vector analysis—Clinical relevance and applicability of impedance parameters. Clin. Nutr. 2012, 31, 854–861. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Silva, M.C.G.; Barros, A.J.D.; Wang, J.; Heymsfield, S.B.; Pierson, R.N. Bioelectrical impedance analysis: Population reference values for phase angle by age and sex. Am. J. Clin. Nutr. 2005, 82, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Lammersfeld, C.A.; Vashi, P.G.; King, J.; Dahlk, S.L.; Grutsch, J.F.; Lis, C.G. Bioelectrical impedance phase angle in clinical practice: Implications for prognosis in stage IIIB and IV non-small cell lung cancer. BMC Cancer 2009, 9, 37. [Google Scholar] [CrossRef] [Green Version]
- Norman, K.; Wirth, R.; Neubauer, M.; Eckardt, R.; Stobäus, N. The Bioimpedance Phase Angle Predicts Low Muscle Strength, Impaired Quality of Life, and Increased Mortality in Old Patients with Cancer. J. Am. Med. Dir. Assoc. 2015, 16, 173.e17–173.e22. [Google Scholar] [CrossRef] [PubMed]
- De Blasio, F.; Santaniello, M.G.; Mazzarella, G.; Bianco, A.; Lionetti, L.; Franssen, F.M.E.; Scalfi, L. Raw BIA variables are predictors of muscle strength in patients with chronic obstructive pulmonary disease. Eur. J. Clin. Nutr. 2017, 71, 1336–1340. [Google Scholar] [CrossRef]
- Di Vincenzo, O.; Marra, M.; Scalfi, L. Bioelectrical impedance phase angle in sport: A systematic review. J. Int. Soc. Sports Nutr. 2019, 16, 49. [Google Scholar] [CrossRef] [Green Version]
- Norman, K.; Stobäus, N.; Zocher, D.; Bosy-Westphal, A.; Szramek, A.; Scheufele, R.; Smoliner, C.; Pirlich, M. Cutoff percentiles of bioelectrical phase angle predict functionality, quality of life, and mortality in patients with cancer. Am. J. Clin. Nutr. 2010, 92, 612–619. [Google Scholar] [CrossRef] [Green Version]
- Bering, T.; Diniz, K.G.D.; Coelho, M.P.P.; de Souza, A.C.M.; de Melo, L.F.; Vieira, D.A.; Soares, M.M.S.; Kakehasi, A.M.; Correia, M.I.T.D.; Teixeira, R.; et al. Bioelectrical Impedance Analysis–Derived Measurements in Chronic Hepatitis C: Clinical Relevance of Fat-Free Mass and Phase Angle Evaluation. Nutr. Clin. Pract. 2017, 33, 238–246. [Google Scholar] [CrossRef]
- de Blasio, F.; Di Gregorio, A.; de Blasio, F.; Bianco, A.; Bellofiore, B.; Scalfi, L. Malnutrition and sarcopenia assessment in patients with chronic obstructive pulmonary disease according to international diagnostic criteria, and evaluation of raw BIA variables. Respir. Med. 2018, 134, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pena, N.F.; Mauricio, S.F.; Rodrigues, A.M.; Carmo, A.S.; Coury, N.C.; Correia, M.I.; Generoso, S.V. Association Between Standardized Phase Angle, Nutrition Status, and Clinical Outcomes in Surgical Cancer Patients. Nutr. Clin. Pract. 2018, 34, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Kilic, M.K.; Kizilarslanoglu, M.C.; Arik, G.; Bolayir, B.; Kara, O.; Varan, H.D.; Sumer, F.; Kuyumcu, M.E.; Halil, M.; Ulger, Z. Association of Bioelectrical Impedance Analysis–Derived Phase Angle and Sarcopenia in Older Adults. Nutr. Clin. Pract. 2016, 32, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Uemura, K.; Yamada, M.; Okamoto, H. Association of bioimpedance phase angle and prospective falls in older adults. Geriatr. Gerontol. Int. 2019, 19, 503–507. [Google Scholar] [CrossRef]
- Uemura, K.; Doi, T.; Tsutsumimoto, K.; Nakakubo, S.; Kim, M.; Kurita, S.; Ishii, H.; Shimada, H. Predictivity of bioimpedance phase angle for incident disability in older adults. J. Cachex-Sarcopenia Muscle 2019, 11, 46–54. [Google Scholar] [CrossRef] [Green Version]
- Wirth, R.; Volkert, D.; Rösler, A.; Sieber, C.C.; Bauer, J. Bioelectric impedance phase angle is associated with hospital mortality of geriatric patients. Arch. Gerontol. Geriatr. 2010, 51, 290–294. [Google Scholar] [CrossRef]
- Lukaski, H.C.; Kyle, U.G.; Kondrup, J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: Phase Angle and Impedance Ratio. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 330–339. [Google Scholar] [CrossRef]
- Irisawa, H.; Mizushima, T. Correlation of body composition and nutritional status with functional recovery in stroke reha-bilitation patients. Nutrients 2020, 12, 1923. [Google Scholar] [CrossRef]
- Moritani, T.; Devries, H.A. Potential for Gross Muscle Hypertrophy in Older Men. J. Gerontol. 1980, 35, 672–682. [Google Scholar] [CrossRef]
- Scott, D.; Trbojevic, T.; Skinner, E.; Clark, R.; Levinger, P.; Haines, T.; Sanders, K.; Ebeling, P. Associations of calf inter- and intra-muscular adipose tissue with cardiometabolic health and physical function in community-dwelling older adults. J. Musculoskelet. Neuronal Interact. 2015, 15, 350–357. [Google Scholar]
- Correa-De-Araujo, R.; Harris-Love, M.O.; Miljkovic, I.; Fragala, M.S.; Anthony, B.W.; Manini, T.M. The Need for Standardized Assessment of Muscle Quality in Skeletal Muscle Function Deficit and Other Aging-Related Muscle Dysfunctions: A Symposium Report. Front. Physiol. 2017, 8, 87. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Mean | SD |
|---|---|---|
| Number of patients | 148 | |
| Age (years) | 84.1 | 7.8 |
| Sex (F/M) | 121/27 | |
| Femoral neck fracture | 84 | |
| Trochanteric fracture | 64 | |
| BHA | 76 | |
| Osteosynthesis | 72 | |
| Days after PFF onset | 22.6 | 8.7 |
| Rehabilitation Program Time (min/day) | 139.8 | 18.6 |
| Serum albumin (g/dL) | 3.6 | 0.4 |
| GNRI on admission | 94.3 | 10.9 |
| GNRI at 4 weeks | 96.8 | 12.8 |
| Motor FIM score on admission | 49.4 | 13.7 |
| Motor FIM score at 4 weeks | 66.8 | 16.4 |
| Male (n = 27) | Female (n = 121) | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (years) | 82.6 | 9.3 | 84.7 | 9.4 |
| Height (cm) | 162.1 | 12.8 | 154.2 * | 9.2 |
| Weight (kg) | 53.6 | 14.3 | 48.9 * | 9.8 |
| BMI (kg/m2) | 20.4 | 3.8 | 20.6 | 3.9 |
| Nutritional Status (GNRI) | Muscle Strength (kgw) | Muscle Quality (Degree) | SMI (kg/m2) | Motor FIM Items | |
|---|---|---|---|---|---|
| On admission | 93.6 | 24.7 | 4.2 | 7.4 | 47.6 |
| After 4 weeks | 95.8 | 27.9 | 4.4 | 7.3 | 66.4 |
| p | <0.001 | <0.001 | <0.001 | 0.21 | <0.001 |
| Nutritional Status (GNRI) | Muscle Strength (kgw) | Muscle Quality (Degree) | SMI (kg/m2) | Motor FIM Items | |
|---|---|---|---|---|---|
| On admission | 94.6 | 18.2 | 3.3 | 5.7 | 49.8 |
| After 4 weeks | 95.7 | 19.1 | 3.4 | 5.6 | 66.9 |
| p | <0.001 | <0.001 | <0.001 | 0.24 | <0.001 |
| Variables | Odds Ratios | 95% CI | p |
|---|---|---|---|
| No malnutrition (GNRI > 92) | 3.917 | 1.224–4.745 | 0.02 |
| High muscle strength (male > 26.0 kgw, female > 18.0 kgw) | 1.340 | 0.651–2.758 | 0.43 |
| High muscle quality (male > 3.5°, female > 3.0°) | 7.929 | 3.047–20.589 | <0.01 |
| High SMI (male > 7.0 kg/m2, female > 5.7 kg/m2) | 0.859 | 0.417–1.773 | 0.68 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Irisawa, H.; Mizushima, T. Relationship between Nutritional Status, Body Composition, Muscle Strength, and Functional Recovery in Patients with Proximal Femur Fracture. Nutrients 2022, 14, 2298. https://doi.org/10.3390/nu14112298
Irisawa H, Mizushima T. Relationship between Nutritional Status, Body Composition, Muscle Strength, and Functional Recovery in Patients with Proximal Femur Fracture. Nutrients. 2022; 14(11):2298. https://doi.org/10.3390/nu14112298
Chicago/Turabian StyleIrisawa, Hiroshi, and Takashi Mizushima. 2022. "Relationship between Nutritional Status, Body Composition, Muscle Strength, and Functional Recovery in Patients with Proximal Femur Fracture" Nutrients 14, no. 11: 2298. https://doi.org/10.3390/nu14112298
APA StyleIrisawa, H., & Mizushima, T. (2022). Relationship between Nutritional Status, Body Composition, Muscle Strength, and Functional Recovery in Patients with Proximal Femur Fracture. Nutrients, 14(11), 2298. https://doi.org/10.3390/nu14112298






