Astaxanthin Influence on Health Outcomes of Adults at Risk of Metabolic Syndrome: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
| Risk Factor | WHO (1998) [16] | EGIR (1999) [16] | AACE (2003) [1] | CDS (2004) [17] | IDF (2005) [16] | NCEP-ATP III (2005 Revision) [16] | JCDCG (2007) [18] |
|---|---|---|---|---|---|---|---|
| Core element | Insulin resistance (IGT, IFG, T2DM or other evidence of IR) | Hyperinsulinemia (plasma insulin > 75th percentile) | Insulin resistance (IGT, IFG) | None | Central obesity (WC): ≥90 cm (M), ≥80 cm (F) | None | None |
| Criteria | IR or diabetes, plus two of the five criteria below | Hyperinsulinemia, plus two of the four criteria below | IR, final diagnosis is left to physician discretion | Any three of the four criteria below | Obesity, plus two of the four criteria below | Any three of the five criteria below | Any four of the five criteria below |
| Obesity | Waist/hip ratio: >0.90 (M), >0.85 (F); or BMI >30 kg/m2 | WC: ≥94 cm (M), ≥80 cm (F) | BMI >25 kg/m2 or WC: >40 inches (M), >35 inches (F) | BMI > 25 kg/m2 | Central obesity already required | WC: >40 inches (M), >35 inches (F) | WC: ≥90 cm (M), ≥85 cm (F) |
| Hyper-glycemia | IR already required | IR already required | IR already required | Fasting glucose ≥ 110 mg/dL or Tx | Fasting glucose ≥ 100 mg/dL | Fasting glucose ≥ 100 mg/dL or Tx | Fasting glucose ≥ 110 mg/dL or with a history of T2DM |
| Dys-lipidemia | TG ≥150 mg/dL or HDL-C: <35 mg/dL (M), <39 mg/dL (F) | TG ≥117 mg/dL or HDL-C <39 mg/dL | TG ≥150 mg/dL or HDL-C: <40 mg/dL (M), <50 mg/dL (F) | TG ≥150 mg/dL or HDL-C: <35 mg/dL (M), <39 mg/dL (F) | TG ≥150 mg/dL or Tx | TG ≥150 mg/dL or Tx | TG ≥150 mg/dL |
| Dyslipidemia (second separate criteria) | - | - | - | - | HDL-C: <40 mg/dL (M), <50 mg/dL (F); or Tx | HDL-C: <40 mg/dL (M), <50 mg/dL (F); or Tx | HDL-C: <40 mg/dL |
| Hyper-tension | ≥140/90 mmHg | ≥140/90 mmHg or Tx | >130/85 mmHg | ≥140/90 mmHg or Tx | >130/85 mmHg or Tx | >130/85 mmHg or Tx | ≥130/85 mmHg or Tx |
| Other criteria | Microalbuminuria | - | Other features of IR | - | - | - | - |
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Selection Process
2.4. Data Collection Process and Data Extraction
2.5. Data Synthesis and Statistical Analysis
2.6. Risk of Bias in Individual Studies
3. Results
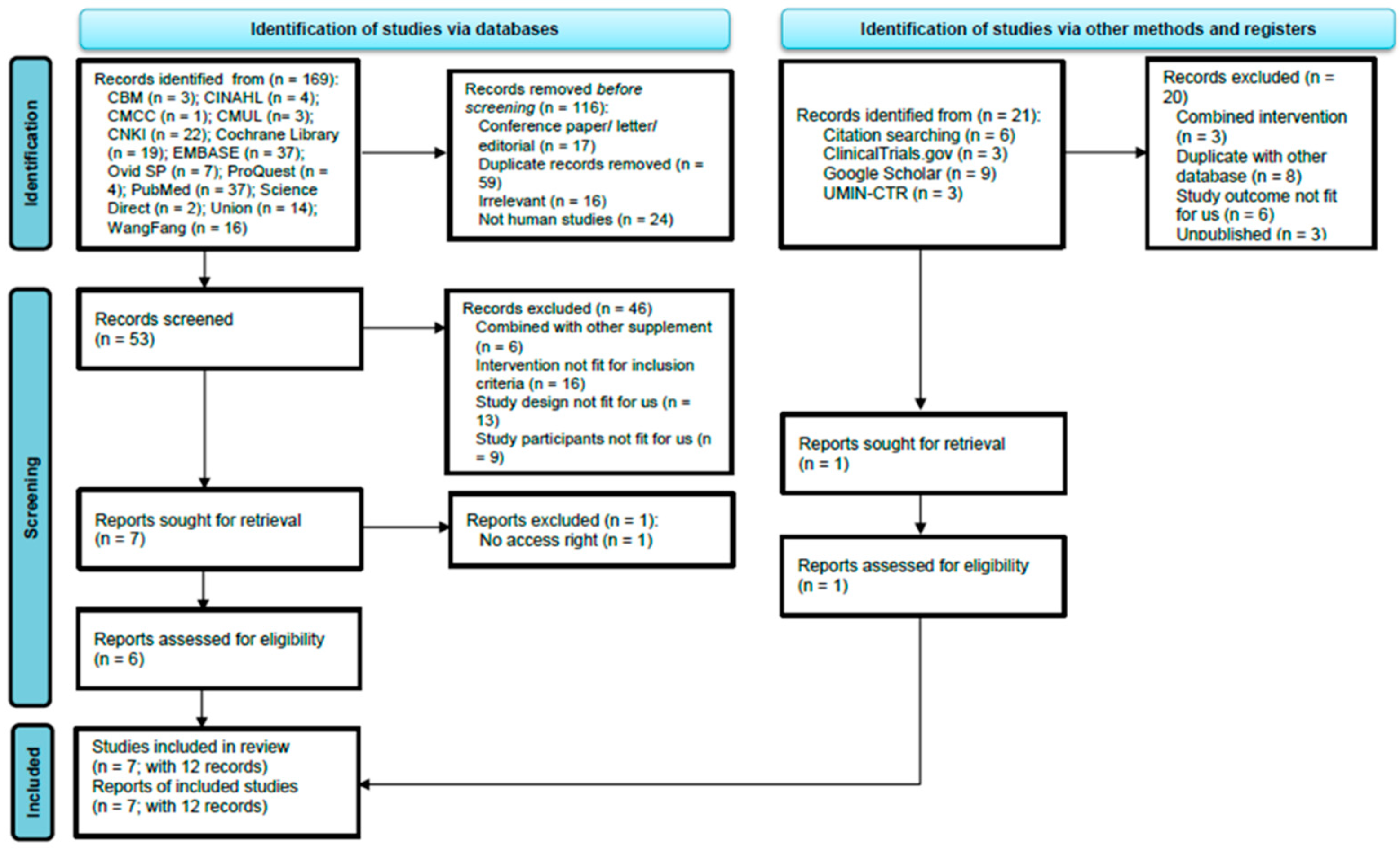
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality of the Included Studies
3.4. Meta-Analsysis Results—Primary Outcomes
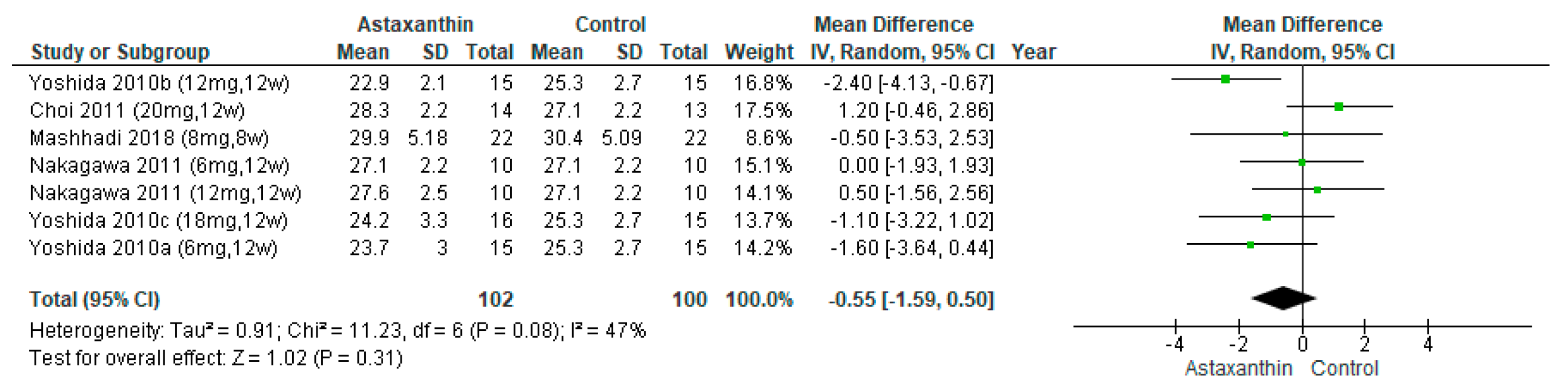
3.4.1. Body Mass Index (BMI)
3.4.2. Fasting Blood Glucose (FBG)
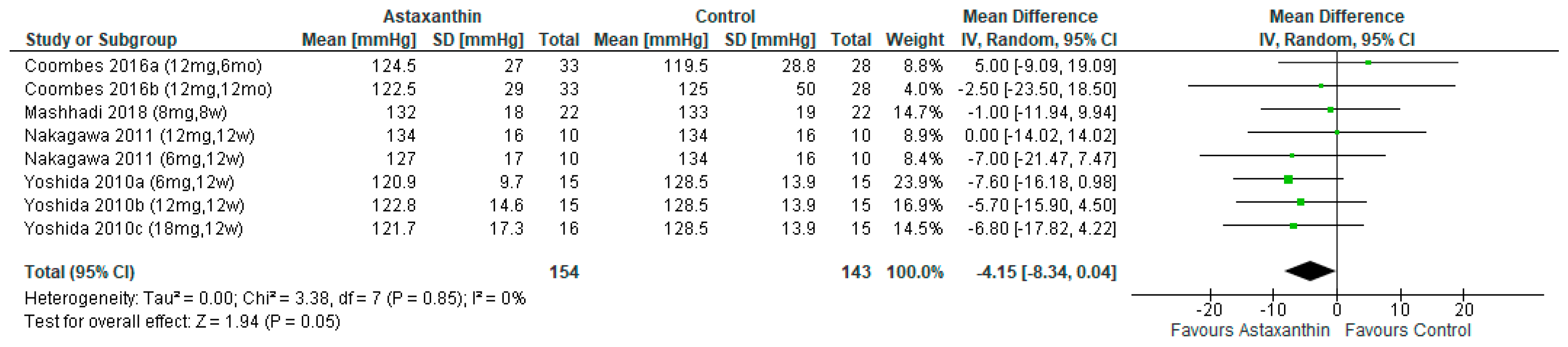
3.4.3. Systolic Blood Pressure (SBP)
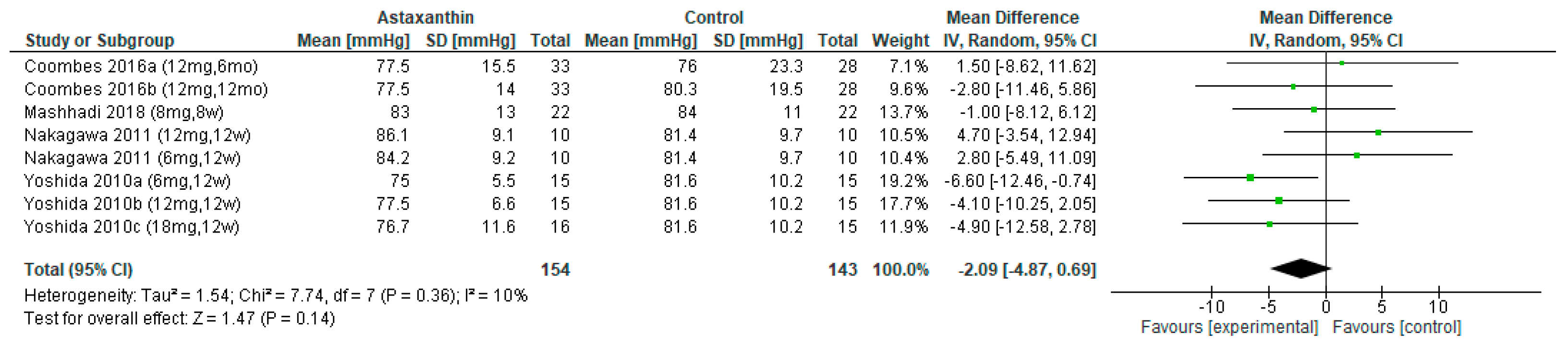
3.4.4. Diastolic Blood Pressure (DBP)
3.4.5. Total Cholesterol (TC)
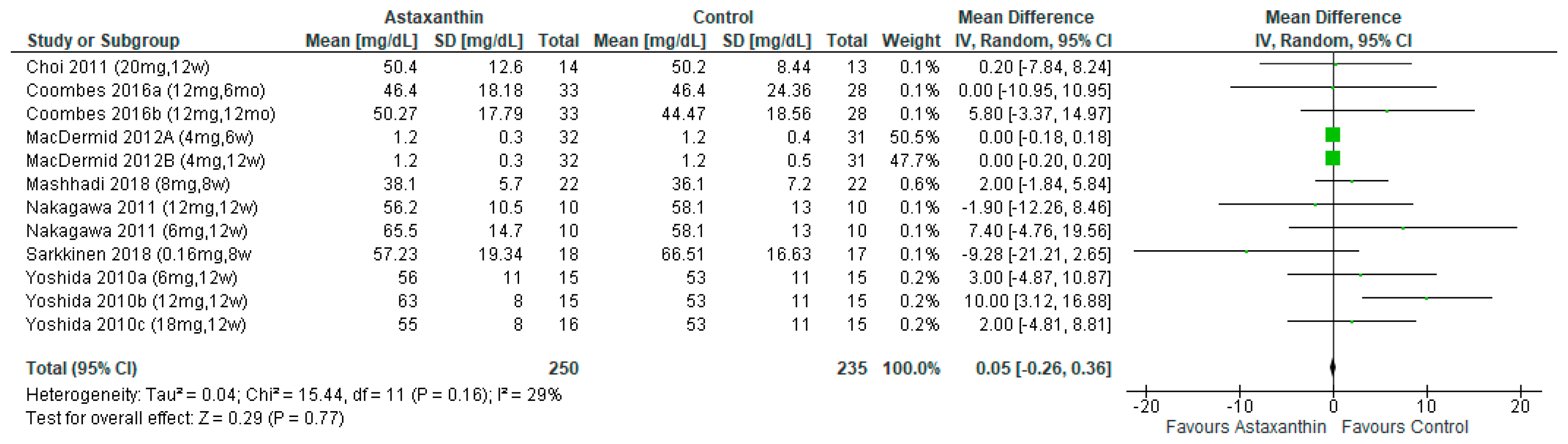
3.4.6. High-density Lipoprotein Cholesterol (HDL-C)
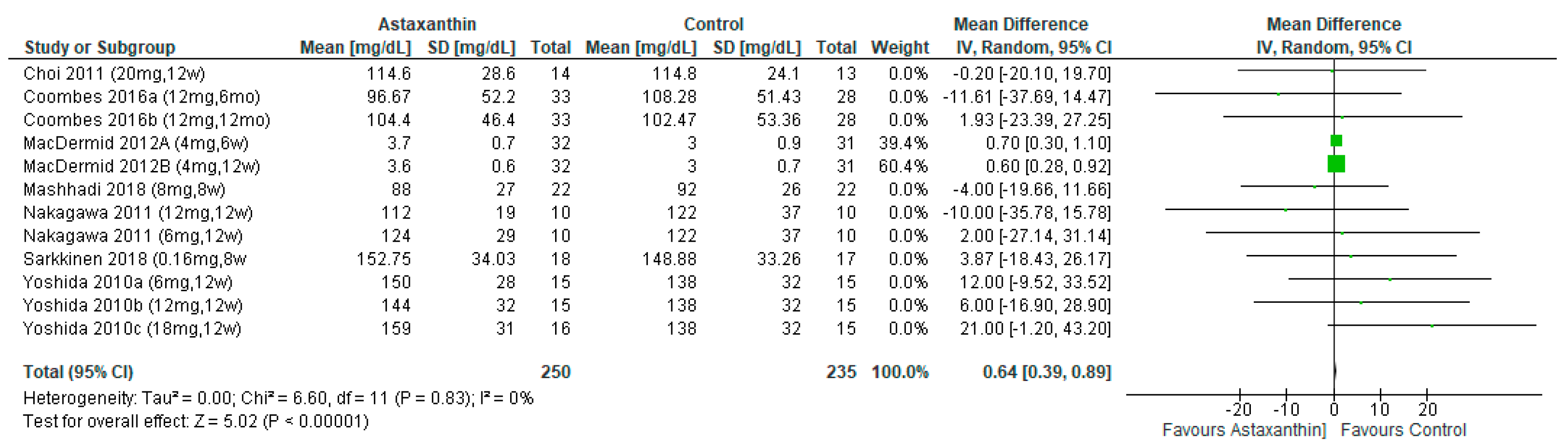
3.4.7. Low-density Lipoprotein Cholesterol (LDL-C)
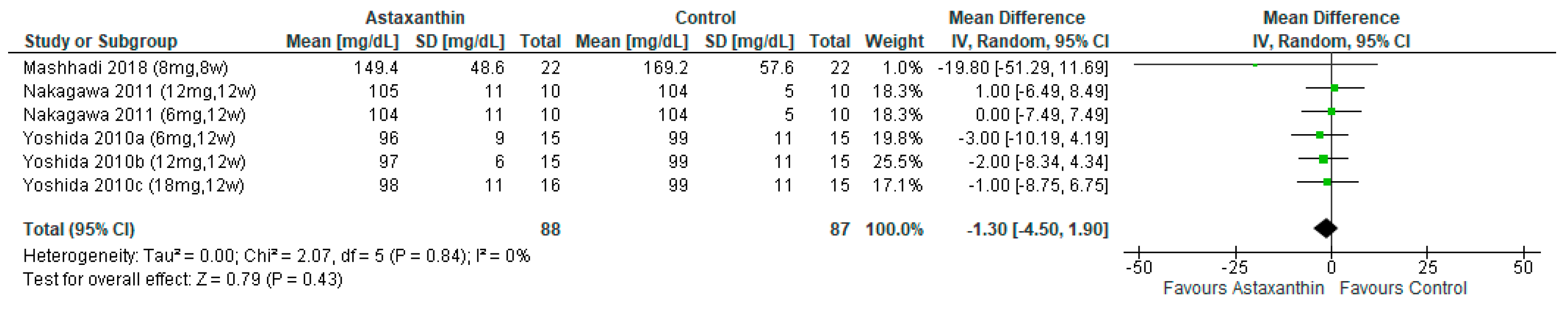
3.4.8. Triglyceride (TG)
3.4.9. Waist Circumference (WC)
3.5. Secondary Outcome
4. Discussion
4.1. Reporting Biases
4.2. Strengths
4.3. Limitations
4.4. Implication for Future Studies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Cornier, M.A.; Dabelea, D.; Hernandez, T.L.; Lindstrom, R.C.; Steig, A.J.; Stob, N.R.; Van Pelt, R.E.; Wang, H.; Eckel, R.H. The metabolic syndrome. Endocr. Rev. 2008, 29, 777–822. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Regufe, V.M.G.; Pinto, C.; Perez, P. Metabolic syndrome in type 2 diabetic patients: A review of current evidence. Porto Biomed. J. 2020, 5, 101. [Google Scholar] [CrossRef]
- Shirouchi, B.; Matsuoka, R. Alleviation of Metabolic Syndrome with Dietary Egg White Protein. J. Oleo Sci. 2019, 68, 517–524. [Google Scholar] [CrossRef]
- Hess, P.L.; Al-Khalidi, H.R.; Friedman, D.J.; Mulder, H.; Kucharska-Newton, A.; Rosamond, W.R.; Lopes, R.D.; Gersh, B.J.; Mark, D.B.; Curtis, L.H.; et al. The Metabolic Syndrome and Risk of Sudden Cardiac Death: The Atherosclerosis Risk in Communities Study. J. Am. Heart Assoc. 2017, 6, 006103. [Google Scholar] [CrossRef]
- Swarup, S.; Goyal, A.; Grigorova, Y.; Zeltser, R. Metabolic Syndrome. In Treasure Island; StatPearls: Tampa, FL, USA, 2022. [Google Scholar]
- Zhang, Y.; Mei, S.; Yang, R.; Chen, L.; Gao, H.; Li, L. Effects of lifestyle intervention using patient-centered cognitive behavioral therapy among patients with cardio-metabolic syndrome: A randomized, controlled trial. BMC Cardiovasc. Disord. 2016, 16, 227. [Google Scholar] [CrossRef][Green Version]
- Mallappa, R.H.; Rokana, N.; Duary, R.K.; Panwar, H.; Batish, V.K.; Grover, S. Management of metabolic syndrome through probiotic and prebiotic interventions. Indian J. Endocrinol. Metab. 2012, 16, 20–27. [Google Scholar] [CrossRef]
- Haswell, C.; Ali, A.; Page, R.; Hurst, R.; Rutherfurd-Markwick, K. Potential of Beetroot and Blackcurrant Compounds to Improve Metabolic Syndrome Risk Factors. Metabolites 2021, 11, 338. [Google Scholar] [CrossRef]
- Vergara, D.; Scoditti, E.; Aziz, A.A.; Giudetti, A.M. Editorial: Dietary Antioxidants and Metabolic Diseases. Front. Nutr. 2021, 8, 617859. [Google Scholar] [CrossRef]
- Ursoniu, S.; Sahebkar, A.; Serban, M.C.; Banach, M. Lipid profile and glucose changes after supplementation with astaxanthin: A systematic review and meta-analysis of randomized controlled trials. Arch. Med. Sci. AMS 2015, 11, 253–266. [Google Scholar] [CrossRef] [PubMed]
- Davinelli, S.; Nielsen, M.E.; Scapagnini, G. Astaxanthin in Skin Health, Repair, and Disease: A Comprehensive Review. Nutrients 2018, 10, 522. [Google Scholar] [CrossRef] [PubMed]
- Donoso, A.; Gonzalez-Duran, J.; Munoz, A.A.; Gonzalez, P.A.; Agurto-Munoz, C. Therapeutic uses of natural astaxanthin: An evidence-based review focused on human clinical trials. Pharmacol. Res. 2021, 166, 105479. [Google Scholar] [CrossRef] [PubMed]
- Brendler, T.; Williamson, E.M. Astaxanthin: How much is too much? A safety review. Phytother. Res. PTR 2019, 33, 3090–3111. [Google Scholar] [CrossRef]
- Huang, P.L. A comprehensive definition for metabolic syndrome. Dis. Models Mech. 2009, 2, 231–237. [Google Scholar] [CrossRef]
- Metabolic Syndrome Study Group of the Chinese Diabetes Society. Metabolic syndrome: Chinese Diabetes Society consultation. Chin. J. Diabetes 2004, 12, 156–161. [Google Scholar]
- Hou, X.; Lu, J.; Weng, J.; Ji, L.; Shan, Z.; Liu, J.; Tian, H.; Ji, Q.; Zhu, D.; Ge, J.; et al. Impact of waist circumference and body mass index on risk of cardiometabolic disorder and cardiovascular disease in Chinese adults: A national diabetes and metabolic disorders survey. PLoS ONE 2013, 8, 57319. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Pearson, A.; Field, J.; Jordan, Z. Evidence-Based Clinical Practice in Nursing and Health Care: Assimilating Research, Experience and Expertise; Blackwell Publishing: Malden, MA, USA, 2006. [Google Scholar]
- Aromataris, E.; Munn, Z. JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2020. [Google Scholar]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Chen, H.; Manning, A.K.; Dupuis, J. A method of moments estimator for random effect multivariate meta-analysis. Biometrics 2012, 68, 1278–1284. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; The Cochrane Collaboration and John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, H.; Yanai, H.; Ito, K.; Tomono, Y.; Koikeda, T.; Tsukahara, H.; Tada, N. Administration of natural astaxanthin increases serum HDL-cholesterol and adiponectin in subjects with mild hyperlipidemia. Atherosclerosis 2010, 209, 520–523. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, K.; Kiko, T.; Miyazawa, T.; Burdeos, G.C.; Kimura, F.; Satoh, A.; Miyazawa, T. Antioxidant effect of astaxanthin on phospholipid peroxidation in human erythrocytes. Br. J. Nutr. 2011, 105, 1563–1571. [Google Scholar] [CrossRef]
- Mashhadi, N.S.; Zakerkish, M.; Mohammadiasl, J.; Zarei, M.; Mohammadshahi, M.; Haghighizadeh, M.H. Astaxanthin improves glucose metabolism and reduces blood pressure in patients with type 2 diabetes mellitus. Asia Pac. J. Clin. Nutr. 2018, 27, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Sarkkinen, E.S.; Savolainen, M.J.; Taurio, J.; Marvola, T.; Bruheim, I. Prospective, randomized, double-blinded, placebo-controlled study on safety and tolerability of the krill powder product in overweight subjects with moderately elevated blood pressure. Lipids Health Dis. 2018, 17, 287. [Google Scholar] [CrossRef]
- Choi, H.D.; Kim, J.H.; Chang, M.J.; Kyu-Youn, Y.; Shin, W.G. Effects of astaxanthin on oxidative stress in overweight and obese adults. Phytother. Res. 2011, 25, 1813–1818. [Google Scholar] [CrossRef] [PubMed]
- Coombes, J.S.; Sharman, J.E.; Fassett, R.G. Astaxanthin has no effect on arterial stiffness, oxidative stress, or inflammation in renal transplant recipients: A randomized controlled trial (the XANTHIN trial). Am. J. Clin. Nutr. 2016, 103, 283–289. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Vincent, J.I.; Gan, B.S.; Grewal, R. A blinded placebo-controlled randomized trial on the use of astaxanthin as an adjunct to splinting in the treatment of carpal tunnel syndrome. Hand 2012, 7, 1–9. [Google Scholar] [CrossRef]
- Yanai, H.; Ito, K.; Yoshida, H.; Tada, N. Antihypertensive effects of astaxanthin. Integr. Blood Press. Control. 2008, 1, 1–3. [Google Scholar] [CrossRef]
- Xia, W.; Tang, N.; Kord-Varkaneh, H.; Low, T.Y.; Tan, S.C.; Wu, X.; Zhu, Y. The effects of astaxanthin supplementation on obesity, blood pressure, CRP, glycemic biomarkers, and lipid profile: A meta-analysis of randomized controlled trials. Pharmacol. Res. 2020, 161, 105113. [Google Scholar] [CrossRef]
- Probst, P.; Grummich, K.; Heger, P.; Zaschke, S.; Knebel, P.; Ulrich, A.; Buchler, M.W.; Diener, M.K. Blinding in randomized controlled trials in general and abdominal surgery: Protocol for a systematic review and empirical study. Syst. Rev. 2016, 5, 48. [Google Scholar] [CrossRef]


| Design, Country, No. Study Site | Number of Participants (% Female) | Mean Age in Years (SD) | Study Population | Primary Aim | Outcomes | Attrition Rate (%) | ITT | Protocol | |
|---|---|---|---|---|---|---|---|---|---|
| Choi et al. (2011) [30] | Double-blind RCT
| 27 (n = 4, 14.81%) | Placebo 30.1 ± 9.5; Ix 31.1 ± 9.4 | Overweight adults (aged 20–55 years; BMI > 25.0 kg/m2); and overweight (BMI > 25.0 kg/m2) | Evaluate positive effects of AST on LPs and OS state in overweight adults | At baseline and week 12: anthropometric data, LPs, apolipidprotein A1, apolipidprotein B MDA, 15-isoprostane F2t (ISP; also known as 8-epi-PGF2α, 8-iso-PGF2α, or 8-isoprostane), SOD, TAC measured to evaluate OS at baseline and at 4, 8, and 12 weeks | Adherence rate: Ix 93.4 and placebo 92.9% | 27 | No information |
| Coombes et al. (2016) [31] | Double-blind RCT
| 33 (n = 16, 26%) | All 49.9 ± 12.2; (Placebo 50.9 ± 13.4; Ix 49.1 ± 11.2) | Age > 18 and <85 y and having undergone renal transplantation | Assess the effect of AST on arterial stiffness, OS, and inflammation in renal transplant recipients | Primary outcomes: PWV, OS (total F2-isoprostanes), and inflammation (pentraxin-3) Secondary outcomes: Vascular function, CIMT, Aix, CBP, SERV, and additional measures of OS and inflammation | 3 (4.92%) | 58 | No information |
| MacDermid et al. (2012) [32] | Double-blind RCT
| 63 (n = 18, 28.57%) | Control 49 ± 9; Ix 49 ± 7 | CTS clinically diagnosed by hand surgeons and supported by electrophysiological abnormality; competent to comply with treatment and complete study evaluations; aged 18–65 years | Evaluate effectiveness of food additive AST as adjunct in management of CTS | Primary outcome: severity of symptoms of CTS (symptom severity scale) Secondary outcomes: physical impairments, disability and health status measures | 0 (0%) | 63 | No information |
| Mashhadi et al. (2018) [28] | Double-blind RCT
| 44 (n = 27, 61.36%) | Placebo 54 ± 8; Ix 51 ± 9.7 | Adults aged 30–60 years; definitive diagnosis of T2DM with no insulin therapy; no pregnancy or lactation; absence of self-reported specific diseases and malignancies, kidney failure, heart disease, thyroid, and other inflammatory diseases; not taking vitamin and antioxidant supplements during the last 6 months; and no smoking or drinking | Investigate potential effects of AST on participants with T2DM | Adiponectin concentration, lipid peroxidation, glycemic control, insulin sensitivity, and anthropometric indices | 1 (2.38%) | 43 | Yes |
| Nakagawa et al. (2011) [27] | Double-blind RCT
| 30 (n = 15, 50%) | All 56.3 ± 5.3; (Control 56.6 ± 4.4; 6 mg/day 56.3 ± 6.6; 12 mg/day; 56.1 ± 5.1) | Healthy subjects (fifteen men and fifteen women), between 50 and 69 years of age, with a BMI of 27·5 (SD 2·1) kg/m2 | Assess the efficacy of 12-week AST (6 or 12 mg/d) on both AST and PLOOH levels in the erythrocytes of thirty middle-aged and senior subjects | Erythrocyte AST, phospholipid hydroperoxides, blood biochemical | 0 (0%) | 30 | No information |
| Sarkkinen et al. (2018) [29] | Double-blind RCT
| 35 (n = 17, 48.57 %) | All 55.4 ± 8.6 (Placebo 55.3 ± 8.4; Ix 55.5 ± 9.0) | (1) age 18–65 years, (2) overweight female or male (BMI between 25 and 30 kg/m2), (3) mildly or moderately elevated BP (systolic 140–159/ diastolic 90–99 mmHg) | Compare the amount and the type of adverse events during 8-week follow-up after ingestion of krill powder preparation in comparison to ingestion of respective amount of placebo in overweight study subjects with mildly or moderately elevated BP | • Anthropometric data, BP Routine clinical chemistry and haematology (day 0 and 56) Plasma total and lipoprotein lipids; total TGs and TC with enzymatic, colorimetric test and LDL-C and HDL-C concentrations with homogenous • enzymatic colorimetric method | 0 (0%) | 35 | Yes |
| Yoshida et al. (2010) [26] | Double-blind RCT
| 61 (n = 20, 32.79%) | All 44 ± 8 (18 mg/day 43.8 ± 10.4; 12 mg/day 42.8 ± 8.8; 6 mg/day 47.0 ± 7.0; 0 mg/day 44.3 ± 7.0) | Healthy subjects (41 men and 20 women) with TG levels of 120–200 mg/dL | Investigate AST consumption ameliorates dyslipidemia and the association with an increase in serum adiponectin levels | FPG, TC, TG, LDL-C, and HDL-C | 0 (0%) | 61 | No information |
| Items | Choi et al. (2011) [30] | Coombes et al. (2016) [31] | MacDermid et al. (2012) [32] | Mashhadi et al. (2018) [28] | Nakagawa et al. (2011) [27] | Sarkkinen et al. (2018) [29] | Yoshida et al. (2010) [26] |
|---|---|---|---|---|---|---|---|
| 1. Eligibility criteria were specified | Y | Y | Y | Y | Y | Y | Y |
| 2. Subjects were randomly allocated to groups (in a crossover study, subjects were randomly allocated an order in which treatments were received) | Y | Y | Y | Y | Y | Y | Y |
| 3. Allocation was concealed | Y | Y | Y | Y | Y | Y | Y |
| 4. The groups were similar at baseline regarding the most important prognostic indicators | N | Y | Y | Y | Y | Y | Y |
| 5. There was blinding of all subjects | Y | Y | Y | Y | Y | Y | Y |
| 6. There was blinding of all therapists who administered the therapy | Y | Y | Y | Y | N | Y | Y |
| 7. There was blinding of all assessors who measured at least one key outcome | N | Y | Y | Y | N | Y | N |
| 8. Measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups | Y | Y | Y | Y | Y | Y | Y |
| 9. All subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome was analysed by “intention to treat” | Y | Y | Y | Y | Y | Y | Y |
| 10. The results of between-group statistical comparisons are reported for at least one key outcome | Y | Y | Y | Y | Y | Y | Y |
| 11. The study provides both point measures and measures of variability for at least one key outcome | Y | Y | Y | Y | Y | Y | Y |
| Overall score | 8 | 10 | 10 | 10 | 8 | 10 | 9 |
| Quality | Good | Excellent | Excellent | Excellent | Good | Excellent | Excellent |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leung, L.Y.-L.; Chan, S.M.-N.; Tam, H.-L.; Wong, E.S.-W. Astaxanthin Influence on Health Outcomes of Adults at Risk of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 2050. https://doi.org/10.3390/nu14102050
Leung LY-L, Chan SM-N, Tam H-L, Wong ES-W. Astaxanthin Influence on Health Outcomes of Adults at Risk of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Nutrients. 2022; 14(10):2050. https://doi.org/10.3390/nu14102050
Chicago/Turabian StyleLeung, Leona Yuen-Ling, Sidney Man-Ngai Chan, Hon-Lon Tam, and Emily Sze-Wan Wong. 2022. "Astaxanthin Influence on Health Outcomes of Adults at Risk of Metabolic Syndrome: A Systematic Review and Meta-Analysis" Nutrients 14, no. 10: 2050. https://doi.org/10.3390/nu14102050
APA StyleLeung, L. Y.-L., Chan, S. M.-N., Tam, H.-L., & Wong, E. S.-W. (2022). Astaxanthin Influence on Health Outcomes of Adults at Risk of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Nutrients, 14(10), 2050. https://doi.org/10.3390/nu14102050








