Multi-Trajectories of Macronutrient Intake and Their Associations with Obesity among Chinese Adults from 1991 to 2018: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
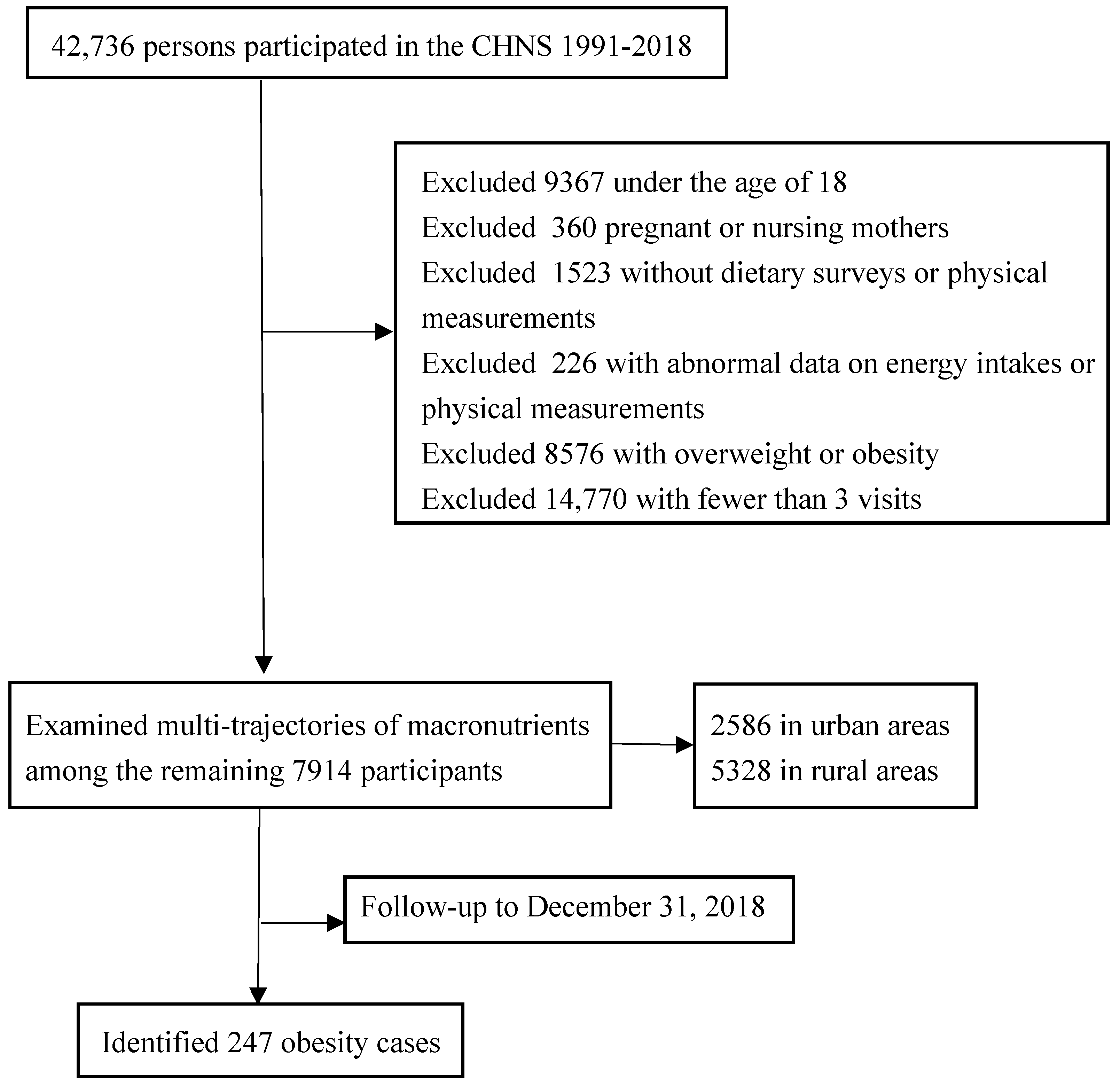
2.1. Study Participants
2.2. Outcome Variables
2.3. Exposure Variables
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics
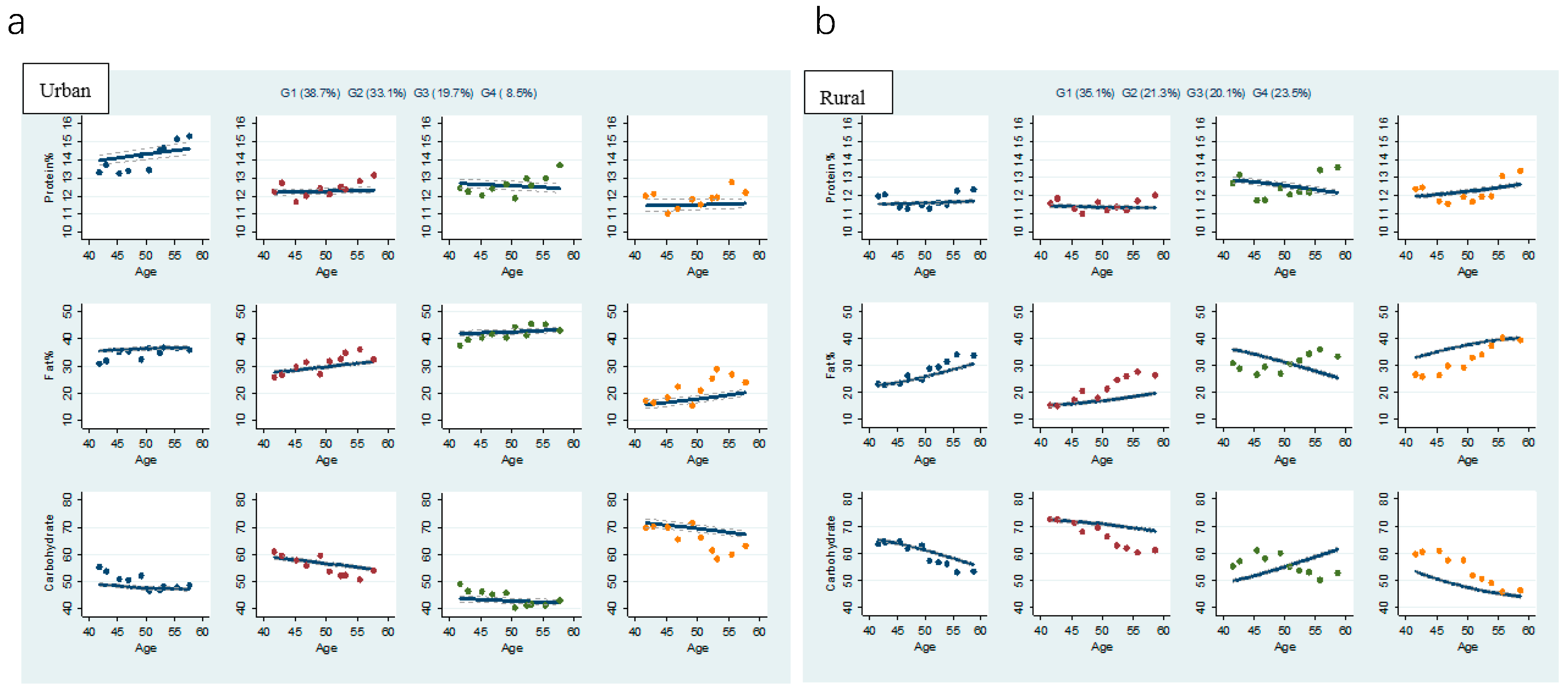
3.2. Multi-Trajectories of Macronutrient Energy Supply Ratios
3.3. Baseline Characteristics by Multi-Trajectories
3.4. Associations between Multi-Trajectories and Obesity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity and overweight. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 9 June 2021).
- The GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhou, B.; Zhao, Z.; Yang, L.; Zhang, M.; Jiang, Y.; Li, Y.; Zhou, M.; Wang, L.; Huang, Z.; et al. Body-mass index and obesity in urban and rural China: Findings from consecutive nationally representative surveys during 2004–18. Lancet 2021, 398, 53–63. [Google Scholar] [CrossRef]
- Ludwig, D.S. Lowering the Bar on the Low-Fat Diet. JAMA 2016, 316, 2087–2088. [Google Scholar] [CrossRef] [PubMed]
- Ge, L.; Sadeghirad, B.; Ball, G.D.C.; Da Costa, B.R.; Hitchcock, C.L.; Svendrovski, A.; Kiflen, R.; Quadri, K.; Kwon, H.Y.; Karamouzian, M.; et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: Systematic review and network meta-analysis of randomised trials. BMJ 2020, 369, m696. [Google Scholar] [CrossRef] [Green Version]
- Willems, A.E.M.; Sura-de Jong, M.; van Beek, A.P.; Nederhof, E.; van Dijk, G. Effects of macronutrient intake in obesity: A me-ta-analysis of low-carbohydrate and low-fat diets on markers of the metabolic syndrome. Nutr. Rev. 2021, 79, 429–444. [Google Scholar] [CrossRef]
- Hu, T.; Mills, K.T.; Yao, L.; Demanelis, K.; Eloustaz, M.; Yancy, W.S., Jr.; Kelly, T.N.; He, J.; Bazzano, L.A. Effects of Low-Carbohydrate Diets Versus Low-Fat Diets on Metabolic Risk Factors: A Meta-Analysis of Randomized Controlled Clinical Trials. Am. J. Epidemiol. 2012, 176 (Suppl. S7), S44–S54. [Google Scholar] [CrossRef] [Green Version]
- Steckhan, N.; Hohmann, C.D.; Kessler, C.; Dobos, G.; Michalsen, A.; Cramer, H. Effects of different dietary approaches on inflam-matory markers in patients with metabolic syndrome: A systematic review and meta-analysis. Nutrition 2016, 32, 338–348. [Google Scholar] [CrossRef]
- Sackner-Bernstein, J.; Kanter, D.; Kaul, S. Dietary Intervention for Overweight and Obese Adults: Comparison of Low-Carbohydrate and Low-Fat Diets. A Meta-Analysis. PLoS ONE 2015, 10, e0139817. [Google Scholar] [CrossRef]
- Halkjær, J.; Olsen, A.; Overvad, K.; Jakobsen, M.U.; Boeing, H.; Buijsse, B.; Palli, D.; Tognon, G.; Du, H.; Van Der A, D.L.; et al. Intake of total, animal and plant protein and subsequent changes in weight or waist circumference in European men and women: The Diogenes project. Int. J. Obes. 2010, 35, 1104–1113. [Google Scholar] [CrossRef] [Green Version]
- Hernández-Alonso, P.; Salas-Salvadó, J.; Ruiz-Canela, M.; Corella, D.; Estruch, R.; Fitó, M.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; Lapetra, J.; et al. High dietary protein intake is asso-ciated with an increased body weight and total death risk. Clin. Nutr. 2016, 35, 496e–506. [Google Scholar] [CrossRef]
- Vergnaud, A.C.; Norat, T.; Mouw, T.; Romaguera, D.; May, A.M.; Bueno-de-Mesquita, H.B.; van der A, D.; Agudo, A.; Wareham, N.; Khaw, K.-T.; et al. Macronutrient Composition of the Diet and Prospective Weight Change in Participants of the EPIC-PANACEA Study. PLoS ONE 2013, 8, e57300. [Google Scholar] [CrossRef] [Green Version]
- Clifton, P.; Condo, D.; Keogh, J. Long term weight maintenance after advice to consume low carbohydrate, higher protein diets —A systematic review and meta analysis. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 224–235. [Google Scholar] [CrossRef]
- Sacks Frank, M.; Bray George, A.; Carey Vincent, J.; Smith, S.R.; Ryan, D.H.; Anton, S.D.; McManus, K.; Champagne, C.M.; Bishop, L.M.; Laranjo, N.; et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N. Engl. J. Med. 2009, 360, 859–873. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Z.; Yang, X.; Fang, Y.; Zhang, J.; Yang, Z.; Wang, Z.; Liu, A.; He, L.; Sun, J.; Lian, Y.; et al. Trends and Disparities of Energy Intake and Macronutrient Composition in China: A Series of National Surveys, 1982–2012. Nutrients 2020, 12, 2168. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey—Monitoring and understanding socio-economic and health change in China, 1989-2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef] [Green Version]
- Word Health Organization. Diet, Nutrition and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation; WHO Technical Report Series, No.916; WHO: Geneva, Switzerland, 2003. [Google Scholar]
- Yao, M.; Lichtenstein, A.H.; Roberts, S.B.; Ma, G.; Gao, S.; Tucker, K.L.; McCrory, M.A. Relative influence of diet and physical ac-tivity on cardiovascular risk factors in urban Chinese adults. Int. J. Obes. Relat. Metab. Disord. 2003, 27, 920–932. [Google Scholar] [CrossRef] [Green Version]
- Du, S.; Neiman, A.; Batis, C.; Wang, H.; Zhang, B.; Zhang, J.; Popkin, B.M. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am. J. Clin. Nutr. 2013, 99, 334–343. [Google Scholar] [CrossRef] [Green Version]
- Zhai, F.; Guo, X.; Popkin, B.M.; Ma, L.; Wang, Q.; Yu, W.; Jin, S.; Ge, K. Evaluation of the 24-hour individual recall method in China. Food Nutr. Bull. 1996, 17, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Miller, M.A.; Kruisbrink, M.; Wallace, J.; Ji, C.; Cappuccio, F.P. Sleep duration and incidence of obesity in infants, children, and ad-olescents: A systematic review and meta-analysis of prospective studies. Sleep 2018, 41, 10. [Google Scholar] [CrossRef]
- St-Onge, M.-P. Sleep-obesity relation: Underlying mechanisms and consequences for treatment. Obes. Rev. 2017, 18, 34–39. [Google Scholar] [CrossRef]
- Nagin, D.S.; Jones, B.L.; Passos, V.L.; Tremblay, E.R. Group-based multi-trajectory modeling. Stat. Methods Med Res. 2016, 27, 2015–2023. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.L.; Nagin, D.S. A Note on a Stata Plugin for Estimating Group-based Trajectory Models. Sociol. Methods Res. 2013, 42, 608–613. [Google Scholar] [CrossRef]
- Andruff, H.; Carraro, N.; Thompson, A.; Gaudreau, P.; Louvet, B. Latent Class Growth Modelling: A Tutorial. Tutor. Quant. Methods Psychol. 2009, 5, 11–24. [Google Scholar] [CrossRef]
- Chinese Nutrition Soceity. Chinese Dietary Reference Intakes; Science Publishing House: Beijing, China, 2014. [Google Scholar]
- Shan, Z.; Rehm, C.D.; Rogers, G.; Ruan, M.; Wang, D.D.; Hu, F.B.; Mozaffarian, D.; Zhang, F.F.; Bhupathiraju, S.N. Trends in Dietary Carbohydrate, Protein, and Fat Intake and Diet Quality Among US Adults, 1999–2016. JAMA 2019, 322, 1178–1187. [Google Scholar] [CrossRef] [Green Version]
- Grech, A.; Rangan, A.; Allman-Farinelli, M. Macronutrient Composition of the Australian Population’s Diet; Trends from Three National Nutrition Surveys 1983, 1995 and 2012. Nutrients 2018, 10, 1045. [Google Scholar] [CrossRef] [Green Version]
- Zhao, J.; Zuo, L.; Sun, J.; Su, C.; Wang, H. Trends and Urban-Rural Disparities of Energy Intake and Macronutrient Composition among Chinese Children: Findings from the China Health and Nutrition Survey (1991 to 2015). Nutrients 2021, 13, 1933. [Google Scholar] [CrossRef]
- Xu, Y.; Zhu, S.; Zhou, Y.; Pramono, A.; Zhou, Z. Changing Income-Related Inequality in Daily Nutrients Intake: A Longitudinal Analysis from China. Int. J. Environ. Res. Public Health 2020, 17, 7627. [Google Scholar] [CrossRef]
- Cai, J.; Coyte, P.C.; Zhao, H. Decomposing the causes of socioeconomic-related health inequality among urban and rural popula-tions in China: A new decomposition approach. Int. J. Equity Health 2017, 16, 128. [Google Scholar] [CrossRef]
- Kelly, T.; Unwin, D.; Finucane, F. Low-Carbohydrate Diets in the Management of Obesity and Type 2 Diabetes: A Review from Clinicians Using the Approach in Practice. Int. J. Environ. Res. Public Health 2020, 17, 2557. [Google Scholar] [CrossRef] [Green Version]
- Hall, K.D.; Chung, S.T. Low-carbohydrate diets for the treatment of obesity and type 2 diabetes. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 308–312. [Google Scholar] [CrossRef]
- Cai, L.; Yin, J.; Ma, X.; Mo, Y.; Li, C.; Lu, W.; Bao, Y.; Zhou, J.; Jia, W. Low-carbohydrate diets lead to greater weight loss and better glucose homeostasis than exercise: A randomized clinical trial. Front. Med. 2021, 15, 460–471. [Google Scholar] [CrossRef]
- Yamada, S.; Inoue, G.; Ooyane, H.; Nishikawa, H. Changes in Body Weight, Dysglycemia, and Dyslipidemia After Moderately Low-Carbohydrate Diet Education (LOCABO Challenge Program) Among Workers in Japan. Diabetes Metab. Syndr. Obes. Targets Ther. 2021, 14, 2863–2870. [Google Scholar] [CrossRef]
- Feinman, R.D.; Fine, E.J. Thermodynamics and Metabolic Advantage of Weight Loss Diets. Metab. Syndr. Relat. Disord. 2003, 1, 209–219. [Google Scholar] [CrossRef]
- Ludwing, D.S. Always Hungry? Conquer Cravings, Retrain Your Fat Cells and Lose Weight Permanently; Grand Central Life & Style: New York, NY, USA, 2016; p. 357. [Google Scholar]
- Leidy, H.J.; Clifton, P.M.; Astrup, A.; Wycherley, T.P.; Westerterp-Plantenga, M.S.; Luscombe-Marsh, N.D.; Woods, S.C.; Mattes, R.D. The role of protein in weight loss and maintenance. Am. J. Clin. Nutr. 2015, 101, 1320S–1329S. [Google Scholar] [CrossRef] [Green Version]
- Hall, K.D.; Bemis, T.; Brychta, R.; Chen, K.Y.; Courville, A.; Crayner, E.J.; Goodwin, S.; Guo, J.; Howard, L.; Knuth, N.D.; et al. Calorie for Calorie, Dietary Fat Restriction Results in More Body Fat Loss than Carbohy-drate Restriction in People with Obesity. Cell Metab. 2015, 22, 427–436. [Google Scholar] [CrossRef] [Green Version]
- Hall, K.D.; Chen, K.Y.; Guo, J.; Lam, Y.Y.; Leibel, R.L.; Mayer, L.E.; Reitman, M.L.; Rosenbaum, M.; Smith, S.R.; Walsh, B.T.; et al. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am. J. Clin. Nutr. 2016, 104, 324–333. [Google Scholar] [CrossRef] [Green Version]
- Freedhoff, Y.; Hall, K.D. Weight loss diet studies: We need help not hype. Lancet 2016, 388, 849–851. [Google Scholar] [CrossRef]
- Word Health Organization. Healthy Diet. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 24 August 2020).
- Wang, L.; Wang, H.; Zhang, B.; Popkin, B.M.; Du, S. Elevated Fat Intake Increases Body Weight and the Risk of Overweight and Obesity among Chinese Adults: 1991–2015 Trends. Nutrients 2020, 12, 3272. [Google Scholar] [CrossRef]
- Wan, Y.; Wang, F.; Yuan, J.; Li, J.; Jiang, D.; Zhang, J.; Huang, T.; Zheng, J.; Mann, J.; Li, D. Effects of Macronutrient Distribution on Weight and Related Cardiometabolic Profile in Healthy Non-Obese Chinese: A 6-month, Randomized Controlled-Feeding Trial. EBioMedicine 2017, 22, 200–207. [Google Scholar] [CrossRef] [Green Version]
- US Department of Health and Human Services and US Department of Agriculture. 2015—2020 Dietary Guidelines for Americans, 8th ed.; USDA: Washington, DC, USA, 2015. [Google Scholar]
- Noakes, T.D.; Windt, J. Evidence that supports the prescription of low-carbohydrate high-fat diets: A narrative review. Br. J. Sports Med. 2017, 51, 133–139. [Google Scholar] [CrossRef]
- Bueno, N.B.; de Melo, I.S.; de Oliveira, S.L.; da Rocha Ataide, T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2013, 110, 1178–1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bazzano, L.A.; Hu, T.; Reynolds, K.; Yao, L.; Bunol, C.; Liu, Y.; Chen Ch Klag, M.J.; Whelton, P.K.; He, J. Effects of low-carbohydrate and low-fat diets: A randomized trial. Ann. Intern. Med. 2014, 161, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Willett, W.C.; Volek, J.S.; Neuhouser, M.L. Dietary fat: From foe to friend? Science 2018, 362, 764–770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Survey Year | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1991 | 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | 2011 | 2015 | 2018 | |
| (n = 3541) | (n = 3732) | (n = 4062) | (n = 4414) | (n = 4429) | (n = 4314) | (n = 4216) | (n = 4183) | (n = 3501) | (n = 2711) | |
| Age 1 (years) | 42.1 ± 13.6 | 43.3 ± 14.0 | 45.9 ± 14.5 | 47.3 ± 14.5 | 49.7 ± 14.6 | 51.3 ± 14.5 | 52.9 ± 14.6 | 54.2 ± 14.6 | 55.3 ± 14.2 | 58.8 ± 13.8 |
| Men (%) | 51.2 | 50.6 | 53.0 | 50.7 | 49.2 | 48.6 | 48.3 | 47.1 | 41.9 | 42.8 |
| Urban (%) | 26.3 | 26.2 | 29.8 | 30.2 | 30.3 | 30.6 | 30.1 | 32.6 | 32.3 | 32.5 |
| North (%) | 26.7 | 26.9 | 27.3 | 32.9 | 35.2 | 35.3 | 36.5 | 34.2 | 31.3 | 30.1 |
| Education (%) | ||||||||||
| Primary and below | 61.6 | 59.7 | 58.6 | 52.7 | 48.8 | 47.4 | 47.8 | 45.2 | 39.3 | 37.5 |
| Junior high | 25.2 | 26.0 | 26.5 | 28.6 | 30.0 | 29.2 | 31.0 | 29.8 | 33.2 | 33.1 |
| Senior high and above | 13.2 | 14.3 | 14.9 | 18.8 | 21.2 | 23.4 | 21.2 | 25.0 | 27.5 | 29.4 |
| Annual per capita family income (%) | ||||||||||
| Low (<10,000 RMB) | 88.1 | 60.1 | 62.3 | 55.9 | 51.0 | 46.4 | 43.4 | 39.2 | 36.1 | 34.5 |
| Middle (10,000–20,000 RMB) | 7.5 | 21.7 | 19.4 | 23.0 | 23.6 | 24.7 | 25.5 | 24.6 | 23.9 | 23.2 |
| High (>20,000 RMB) | 4.3 | 18.2 | 18.3 | 21.1 | 25.4 | 28.9 | 31.0 | 36.2 | 40.0 | 42.3 |
| Smoker (%) | 39.2 | 37.7 | 37.4 | 35.5 | 36.1 | 34.7 | 34.3 | 33.4 | 25.7 | 23.1 |
| Alcohol drinker (%) | 40.1 | 38.0 | 39.0 | 36.3 | 33.5 | 32.9 | 32.5 | 31.9 | 25.7 | 22.6 |
| Protein 1 (%) | 12.2 ± 2.5 | 12.4 ± 2.7 | 11.6 ± 2.4 | 11.7 ± 2.5 | 12.2 ± 2.8 | 11.8 ± 2.7 | 12.2 ± 2.9 | 12.2 ± 3.1 | 13.0 ± 3.3 | 13.2 ± 3.3 |
| Fat1 (%) | 24.1± 11.9 | 23.9 ± 12.4 | 25.4 ± 11.9 | 28.3 ± 11.1 | 26.3 ± 12.2 | 30.4 ± 11.8 | 31.4 ± 10.6 | 34.2 ± 11.9 | 35.9 ± 12.3 | 34.7 ± 12.0 |
| Carbohydrate 1 (%) | 62.7 ± 13.0 | 62.7 ± 13.4 | 62.2 ± 12.4 | 59.2 ± 11.8 | 60.6 ± 12.7 | 55.1 ± 13.4 | 53.7 ± 12.0 | 52.7 ± 12.1 | 50.4 ± 12.5 | 51.5 ± 12.3 |
| Energy intake 1 (kcal/d) | 2423.9 ± 700.5 | 2380.3 ± 673.0 | 2486.1 ± 737.5 | 2371.6 ± 690.0 | 2303.1 ± 720.9 | 2315.5 ± 737.1 | 2194.9 ± 678.6 | 2060.5 ± 706.4 | 1990.6 ± 690.7 | 1971.1 ± 656.9 |
| PA 2 (METs/week) | 488.3 (257.5, 660.4) | 373.1 (217.8, 550.0) | 368.0 (164.6, 534.2) | 273.8 (122.7, 435.6) | 164.5 (62.1, 346.2) | 158.3 (56.7, 331.0) | 155.9 (61.7, 314.7) | 153.4 (63.2, 290.9) | 99.3 (38.6, 209.7) | 103.7 (43.7, 207.7) |
| ST 2 (hours/week) | — | — | — | — | 14.0 (7.0, 21.0) | 14.0 (7.0, 21.0) | 14.0 (9.0, 23.0) | 19.5 (14.0, 28.0) | 15.9 (9.0, 28.0) | 14.0 (7.0, 25.3) |
| BMI 1 (kg/m2) | 20.4 ± 1.7 | 20.6 ± 1.7 | 20.8 ± 1.8 | 21.0 ± 1.8 | 21.0 ± 1.8 | 21.1 ± 1.8 | 21.1 ± 1.9 | 21.2 ± 1.8 | 21.3 ± 1.8 | 21.4 ± 1.8 |
| WC 1 (cm) | 72.9 ± 6.7 | 74.2 ± 6.8 | 75.5 ± 7.3 | 76.3 ± 7.6 | 76.8 ± 7.4 | 77.6 ± 7.6 | 78.0 ± 8.2 | 77.6 ±10.4 | 79.2 ± 9.5 | |
| Trajectories in Urban Areas | Trajectories in Rural Areas | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IMP&H&LC | ABM | MP&VHF&VLC | MP&ILF&DHC | p | BM | MP&ILF&DHC | DMP&DHF&IMC | IMP&IHF&DLC | p | |
| (n = 1001, 38.7%) | (n = 857, 33.1%) | (n = 509, 19.7%) | (n = 219, 8.5%) | (n = 1870, 35.1%) | (n = 1135, 21.3%) | (n = 1071, 20.1%) | (n = 1252, 23.5%) | |||
| Age 1 (years) | 40.7 ± 15.3 | 45.5± 14.3 | 38.2 ± 14.6 | 51.9 ± 14.5 | <0.001 | 40.4 ± 11.9 | 47.0 ± 14.5 | 39.4 ± 15.0 | 35.7 ± 12.4 | <0.001 |
| Men (%) | 45.1 | 48.2 | 43.1 | 47.3 | 0.283 | 50.6 | 48.7 | 42.8 | 51.8 | <0.001 |
| North (%) | 31.7 | 39.0 | 19.4 | 43.8 | <0.001 | 36.5 | 47.8 | 24.8 | 29.7 | <0.001 |
| Education (%) | — | — | — | — | <0.001 | — | — | — | — | <0.001 |
| Primary and below | 21.0 | 51.0 | 26.2 | 76.3 | 62.2 | 79.6 | 42.4 | 42.0 | ||
| Junior high | 34.0 | 25.7 | 27.4 | 15.8 | 28.6 | 16.6 | 34.3 | 37.8 | ||
| Senior high and above | 45.0 | 23.3 | 46.4 | 7.9 | 9.2 | 3.8 | 23.3 | 20.2 | ||
| Annual per capita family income (%) | <0.001 | <0.001 | ||||||||
| Low (<10,000 RMB) | 53.2 | 72.1 | 53.8 | 85.7 | 80.6 | 87.1 | 64.0 | 70.9 | ||
| Middle (10,000–20,000 RMB) | 22.0 | 14.3 | 22.1 | 9.8 | 10.4 | 6.9 | 19.2 | 15.4 | ||
| High (>20,000 RMB) | 24.8 | 13.6 | 24.1 | 4.4 | 9.0 | 6.0 | 16.8 | 13.7 | ||
| Smoker 2 (%) | 29.5 | 35.8 | 31.1 | 35.5 | 0.020 | 38.3 | 37.6 | 31.2 | 35.0 | <0.001 |
| Alcohol drinker 3 (%) | 35.6 | 39.9 | 35.1 | 47.7 | 0.004 | 36.3 | 35.6 | 32.4 | 33.9 | 0.136 |
| Protein1 (%) | 13.9 ± 3.1 | 12.1 ± 2.3 | 12.4 ± 3.0 | 11.8 ± 1.9 | <0.001 | 11.7 ± 2.4 | 11.6 ± 1.8 | 12.7 ± 3.2 | 12.0 ± 2.7 | <0.001 |
| Fat 1 (%) | 32.7 ± 9.3 | 27.1 ± 9.7 | 42.2 ± 10.2 | 17.3± 10.0 | <0.001 | 23.0 ± 10.2 | 14.1 ± 7.4 | 34.1 ± 12.1 | 26.6 ± 11.8 | <0.001 |
| Carbohydrate 1 (%) | 52.3 ± 9.9 | 59.9 ± 10.0 | 43.9 ± 10.1 | 69.7 ± 9.9 | <0.001 | 64.4 ± 11.0 | 73.9 ± 7.8 | 52.1 ± 12.5 | 60.1 ± 13.0 | <0.001 |
| Energy intake 1 (kcal/d) | 2232.2 ± 710.7 | 2293.0 ± 668.9 | 2408.8 ± 772.8 | 2,331.1 ± 708.6 | <0.001 | 2422.5 ± 722.1 | 2493.0 ± 745.4 | 2282.8 ± 753.4 | 2345.4 ± 674.3 | <0.001 |
| PA 4 (METs/week) | 146.8 (92.5,241.8) | 251.1 (109.3, 519.9) | 152.3 (88.7, 269.9) | 439.8 (168.0, 667.5) | <0.001 | 475.5 (270.0, 656.0) | 530.6 (348.0, 690.6) | 270.2 (118.0, 480.3) | 340.5 (159.6, 545.6) | <0.001 |
| ST 4 (hours/week) | 21.0 (14.0, 30.5) | 16.0 (8.9, 24.5) | 23.0 (14.0, 33.0) | 9.0 (0.0, 18.5) | <0.001 | 14.0 (7.0, 21.0) | 9.0 (3.5, 15.0) | 14.0 (7.0, 23.0) | 14.0 (7.0, 21.0) | <0.001 |
| BMI 1 (kg/m2) | 20.7 ± 1.8 | 20.9 ± 1.8 | 20.7 ± 1.8 | 20.8 ±1.6 | 0.139 | 20.7 ± 1.7 | 20.6 ± 1.7 | 20.5 ± 1.8 | 20.6 ± 1.7 | 0.060 |
| WC 1 (cm) | 74.9 ± 8.1 | 75.4 ± 7.5 | 74.4 ± 7.8 | 74.6 ±7.5 | 0.131 | 73.6 ± 6.6 | 74.1 ± 7.1 | 73.8 ± 7.1 | 73.4 ± 7.0 | 0.089 |
| Trajectories | Model 1 1 | Model 2 2 | Model 3 3 | |||
|---|---|---|---|---|---|---|
| p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | |
| Urban trajectories | ||||||
| IMP&HF&LC (versus (vs.) ABM) | 0.605 | 0.85 (0.45, 1.59) | 0.532 | 0.79 (0.38, 1.64) | 0.671 | 0.85 (0.41, 1.79) |
| MP&VHF&VLC (vs. ABM) | 0.945 | 0.97 (0.41, 2.31) | 0.915 | 1.05 (0.40, 2.78) | 0.912 | 1.06 (0.39, 2.85) |
| MP&ILF&DHC (vs. ABM) | 0.423 | 0.65 (0.22, 1.88) | 0.798 | 0.86 (0.28, 2.66) | 0.709 | 0.80 (0.26, 2.52) |
| Rural trajectories | ||||||
| MP&ILF&DHC (vs. BM) | 0.681 | 1.08 (0.74, 1.57) | 0.716 | 1.09 (0.69, 1.73) | 0.948 | 0.98 (0.61, 1.58) |
| DMP&DHF&IMC (vs. BM) | 0.168 | 0.72 (0.45, 1.15) | 0.106 | 0.62 (0.35, 1.11) | 0.034 | 0.50 (0.27, 0.95) |
| IMP&IHF&DLC (vs. BM) | 0.052 | 0.67 (0.45, 1.00) | 0.017 | 0.53 (0.32, 0.89) | 0.008 | 0.48 (0.28, 0.83) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, X.; Zhang, J.; Du, W.; Su, C.; Ouyang, Y.; Huang, F.; Jia, X.; Li, L.; Bai, J.; Zhang, B.; et al. Multi-Trajectories of Macronutrient Intake and Their Associations with Obesity among Chinese Adults from 1991 to 2018: A Prospective Study. Nutrients 2022, 14, 13. https://doi.org/10.3390/nu14010013
Zhang X, Zhang J, Du W, Su C, Ouyang Y, Huang F, Jia X, Li L, Bai J, Zhang B, et al. Multi-Trajectories of Macronutrient Intake and Their Associations with Obesity among Chinese Adults from 1991 to 2018: A Prospective Study. Nutrients. 2022; 14(1):13. https://doi.org/10.3390/nu14010013
Chicago/Turabian StyleZhang, Xiaofan, Jiguo Zhang, Wenwen Du, Chang Su, Yifei Ouyang, Feifei Huang, Xiaofang Jia, Li Li, Jing Bai, Bing Zhang, and et al. 2022. "Multi-Trajectories of Macronutrient Intake and Their Associations with Obesity among Chinese Adults from 1991 to 2018: A Prospective Study" Nutrients 14, no. 1: 13. https://doi.org/10.3390/nu14010013
APA StyleZhang, X., Zhang, J., Du, W., Su, C., Ouyang, Y., Huang, F., Jia, X., Li, L., Bai, J., Zhang, B., Wang, Z., Du, S., & Wang, H. (2022). Multi-Trajectories of Macronutrient Intake and Their Associations with Obesity among Chinese Adults from 1991 to 2018: A Prospective Study. Nutrients, 14(1), 13. https://doi.org/10.3390/nu14010013







