The Effects of the Healthy Primary School of the Future on Children’s Fruit and Vegetable Preferences, Familiarity and Intake
Abstract
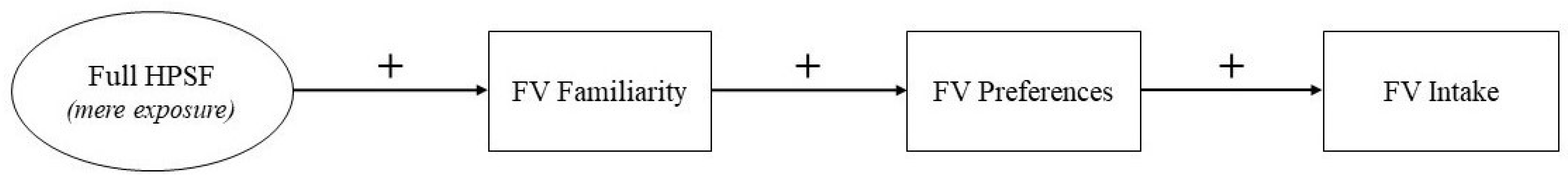
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. The Healthy Primary School of the Future
2.3. Study Population
2.4. Data Collection Procedures and Measures
2.4.1. FV Familiarity and Preferences
2.4.2. FV Intake
2.4.3. Socio-Demographic Characteristics
2.5. Data Processing and Statistical Analyses
3. Results
3.1. Demographic Characteristics
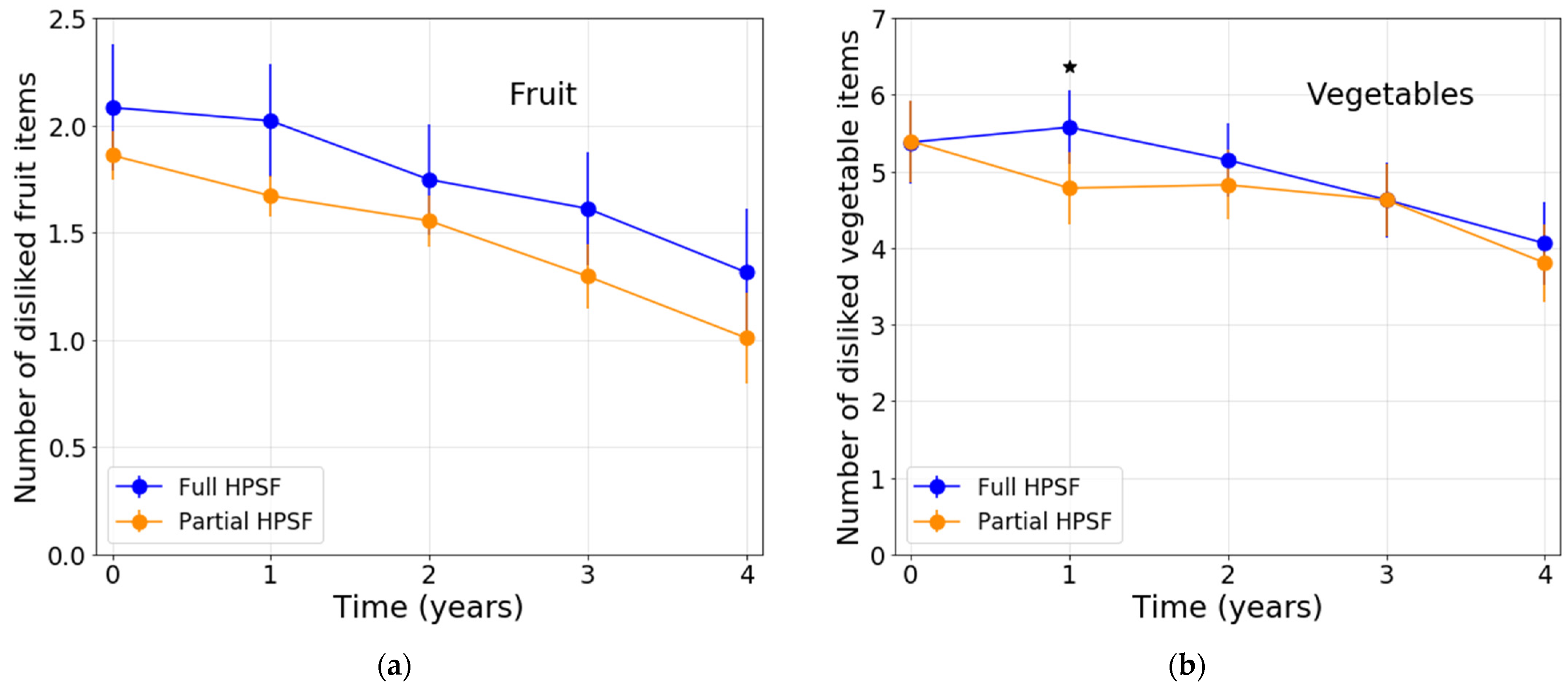
3.2. Intervention Effects on FV Familiarity and Preferences
3.3. Intervention Effects on FV Intake
4. Discussion
4.1. Post Hoc Analyses
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boeing, H.; Bechthold, A.; Bub, A.; Ellinger, S.; Haller, D.; Kroke, A.; Leschik-Bonnet, E.; Müller, M.J.; Oberritter, H.; Schulze, M.B.; et al. Critical review: Vegetables and fruit in the prevention of chronic diseases. Eur. J. Nutr. 2012, 51, 637–663. [Google Scholar] [CrossRef]
- WHO. Increasing Fruit and Vegetable Consumption to Reduce the Risk of Noncommunicable Diseases. Available online: http://www.who.int/elena/titles/fruit_vegetables_ncds/en/ (accessed on 12 August 2019).
- Craigie, A.M.; Lake, A.; Kelly, S.; Adamson, A.; Mathers, J.C. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas 2011, 70, 266–284. [Google Scholar] [CrossRef]
- Goldfield, G.S.; Harvey, A.; Grattan, K.; Adamo, K.B. Physical Activity Promotion in the Preschool Years: A Critical Period to Intervene. Int. J. Environ. Res. Public Health 2012, 9, 1326–1342. [Google Scholar] [CrossRef]
- Yang, X.; Telama, R.; Hirvensalo, M.; Tammelin, T.; Viikari, J.S.; Raitakari, O.T. Active commuting from youth to adulthood and as a predictor of physical activity in early midlife: The Young Finns Study. Prev. Med. 2014, 59, 5–11. [Google Scholar] [CrossRef] [PubMed]
- CBS; RIVM. The Netherlands Nutrition Centre Kinderen Eten te Weinig Fruit, Groente en vis [Children Eat to Less Fruit, Vegetables and Fish]. Available online: https://www.cbs.nl/nl-nl/nieuws/2017/46/kinderen-eten-te-weinig-fruit-groente-en-vis (accessed on 23 August 2019).
- Blanchette, L.; Brug, J. Determinants of fruit and vegetable consumption among 6-12-year-old children and effective interventions to increase consumption. J. Hum. Nutr. Diet. 2005, 18, 431–443. [Google Scholar] [CrossRef] [PubMed]
- Haß, J.; Hartmann, M. What determines the fruit and vegetables intake of primary school children?—An analysis of personal and social determinants. Appetite 2018, 120, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Fischer, J.A. Appetite and eating behaviors in children. In The Pediatric Clinics of North America: Pediatric Nutrition; Gaull, G.E., Ed.; Saunders: Philadelphia, PA, USA, 1995; pp. 931–953. [Google Scholar]
- Birch, L.L. Development of Food Preferences. Annu. Rev. Nutr. 1999, 19, 41–62. [Google Scholar] [CrossRef]
- Drewnowski, A. Taste Preferences and Food Intake. Annu. Rev. Nutr. 1997, 17, 237–253. [Google Scholar] [CrossRef]
- Resnicow, K.; Davis-Hearn, M.; Smith, M.; Baranowski, T.; Lin, L.S.; Baranowski, J.; Doyle, C.; Wang, D.T. Social-Cognitive Predictors of Fruit and Vegetable Intake in Children. Health Psychol. 1997, 16, 272–276. [Google Scholar] [CrossRef]
- Capaldi, E.D. Why We Eat What We Eat: The Psychology of Eating, 1st ed.; American Psychological Association: Washington, DC, USA, 1996. [Google Scholar]
- Cooke, L. The importance of exposure for healthy eating in childhood: A review. J. Hum. Nutr. Diet. 2007, 20, 294–301. [Google Scholar] [CrossRef]
- Birch, L.L. Dimensions of preschool children’s food preferences. J. Nutr. Educ. 1979, 11, 77–80. [Google Scholar] [CrossRef]
- Contento, I.R. Nutrition Education: Linking Research, Theory, and Practice, 2nd ed.; Jones & Bartlett Publishers: Sudbury, MA, USA, 2011; ISBN 9780763775087. [Google Scholar]
- Birch, L.L. Developmental aspects of eating. In Handbook of the Psychophysiology of Human Eating; Shepherd, R., Ed.; Wiley: Chichester, UK, 1989; pp. 179–203. [Google Scholar]
- Westenhoefer, J. Establishing good dietary habits–Capturing the minds of children. Public Health Nutr. 2001, 4, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Appleton, K.M.; Hemingway, A.; Rajska, J.; Hartwell, H. Repeated exposure and conditioning strategies for increasing vegetable liking and intake: Systematic review and meta-analyses of the published literature. Am. J. Clin. Nutr. 2018, 108, 842–856. [Google Scholar] [CrossRef]
- Ventura, A.K.; Worobey, J. Early Influences on the Development of Food Preferences. Curr. Biol. 2013, 23, R401–R408. [Google Scholar] [CrossRef] [PubMed]
- Aldridge, V.; Dovey, T.M.; Halford, J.C. The role of familiarity in dietary development. Dev. Rev. 2009, 29, 32–44. [Google Scholar] [CrossRef]
- Birch, L.L.; Marlin, D.W. I don’t like it; I never tried it: Effects of exposure on two-year-old children’s food preferences. Appetite 1982, 3, 353–360. [Google Scholar] [CrossRef]
- Birch, L.L.; McPhee, L.; Shoba, B.; Pirok, E.; Steinberg, L. What kind of exposure reduces children’s food neophobia?: Looking vs. tasting. Appetite 1987, 9, 171–178. [Google Scholar] [CrossRef]
- Sullivan, S.A.; Birch, L.L. Pass the sugar, pass the salt: Experience dictates preference. Dev. Psychol. 1990, 26, 546–551. [Google Scholar] [CrossRef]
- Liem, D.G.; De Graaf, C. Sweet and sour preferences in young children and adults: Role of repeated exposure. Physiol. Behav. 2004, 83, 421–429. [Google Scholar] [CrossRef]
- Loewen, R.; Pliner, P. Effects of Prior Exposure to Palatable and Unpalatable Novel Foods on Children’s Willingness to Taste Other Novel Foods. Appetite 1999, 32, 351–366. [Google Scholar] [CrossRef]
- Langford, R.; Bonnell, C.P.; Jones, H.E.; Pouliou, T.; Murphy, S.M.; Waters, E.; Komro, K.A.; Gibbs, L.F.; Magnus, D.; Campbell, R. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst. Rev. 2014, 4, CD008958. [Google Scholar] [CrossRef]
- FAO. Nutrition Education in Primary Schools; FAO: Rome, Italy, 2005; Volume 1, ISBN 9251054541. [Google Scholar]
- Lakkakula, A.; Geaghan, J.; Zanovec, M.; Pierce, S.; Tuuri, G. Repeated taste exposure increases liking for vegetables by low-income elementary school children. Appetite 2010, 55, 226–231. [Google Scholar] [CrossRef]
- Schindler, J.M.; Corbett, D.; Forestell, C.A. Assessing the effect of food exposure on children’s identification and acceptance of fruit and vegetables. Eat. Behav. 2013, 14, 53–56. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Willeboordse, M.; Jansen, M.W.; Heijkant, S.N.V.D.; Simons, A.; Winkens, B.; De Groot, R.; Bartelink, N.; Kremers, S.P.; Van Assema, P.; Savelberg, H.H.; et al. The Healthy Primary School of the Future: Study protocol of a quasi-experimental study. BMC Public Health 2016, 16, 1–13. [Google Scholar] [CrossRef]
- Bartelink, N.H.M.; Van Assema, P.; Jansen, M.W.J.; Savelberg, H.H.C.M.; Willeboordse, M.; Kremers, S.P.J. The Healthy Primary School of the Future: A Contextual Action-Oriented Research Approach. Int. J. Environ. Res. Public Health 2018, 15, 2243. [Google Scholar] [CrossRef]
- Bartelink, N.H.M.; Van Assema, P.; Jansen, M.W.J.; Savelberg, H.H.C.M.; Moore, G.F.; Hawkins, J.; Kremers, S.P.J. Process evaluation of the Healthy Primary School of the Future: The key learning points. BMC Public Health 2019, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Boudewijns, E.; Pepels, J.; Van Kann, D.; Konings, K.; Van Schayck, C.; Willeboordse, M. Non-response and external validity in a school-based quasi-experimental study ’The Healthy Primary School of the Future’: A cross-sectional assessment. Prev. Med. Rep. 2019, 14, 100874. [Google Scholar] [CrossRef] [PubMed]
- Bartelink, N.H.M.; van Assema, P.; Kremers, S.P.J.; Savelberg, H.H.C.M.; Oosterhoff, M.; Willeboordse, M.; van Schayck, O.C.P.; Winkens, B.; Jansen, M.W.J. Can the Healthy Primary School of the Future offer perspective in the ongoing obesity epidemic in young children? A Dutch quasi-experimental study. BMJ Open 2019, 9, e030676. [Google Scholar] [CrossRef]
- Bartelink, N.H.M.; Van Assema, P.; Kremers, S.P.J.; Savelberg, H.H.C.M.; Oosterhoff, M.; Willeboordse, M.; Van Schayck, O.C.P.; Winkens, B.; Jansen, M.W.J. One- and Two-Year Effects of the Healthy Primary School of the Future on Children’s Dietary and Physical Activity Behaviours: A Quasi-Experimental Study. Nutrients 2019, 11, 689. [Google Scholar] [CrossRef] [PubMed]
- Bartelink, N.; Van Assema, P.; Kremers, S.; Savelberg, H.; Gevers, D.; Jansen, M. Unravelling the Effects of the Healthy Primary School of the Future: For Whom and Where Is It Effective? Nutrients 2019, 11, 2119. [Google Scholar] [CrossRef] [PubMed]
- Bartelink, N.; Van Assema, P.; Jansen, M.; Savelberg, H.; Kremers, S. The Moderating Role of the School Context on the Effects of the Healthy Primary School of the Future. Int. J. Environ. Res. Public Health 2019, 16, 2432. [Google Scholar] [CrossRef]
- Vermeer, A.; Boot, N.; Hesdahl, M.; Janssen-Goffin, M.; Linssen, E.; Rutten, N.; Hajema, K. Local Reports on Public Health Development: A New Perspective on Health in Heerlen, Kerkrade, Landgraaf and Brunssum; GGD Zuid Limburg: Geleen, The Netherlands, 2014. [Google Scholar]
- Kromhout, D.; Spaaij, C.J.K.; de Goede, J.; Weggemans, R.M. The 2015 Dutch food-based dietary guidelines. Eur. J. Clin. Nutr. 2016 708 2016, 70, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Smaaklessen [Taste Lessons]. Available online: https://www.smaaklessen.nl/nl/smaaklessen.htm (accessed on 9 April 2021).
- Sherwood, N.E.; Story, M.; Neumark-Sztainer, D.; Adkins, S.; Davis, M. Development and implementation of a visual card-sorting technique for assessing food and activity preferences and patterns in African American girls. J. Am. Diet. Assoc. 2003, 103, 1473–1479. [Google Scholar] [CrossRef]
- De Bourdeaudhuij, I.; Klepp, K.-I.; Due, P.; Rodrigo, C.P.; De Almeida, M.; Wind, M.; Krølner, R.; Sandvik, C.; Brug, J. Reliability and validity of a questionnaire to measure personal, social and environmental correlates of fruit and vegetable intake in 10–11-year-old children in five European countries. Public Health Nutr. 2005, 8, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Shavers, V.L. Measurement of socioeconomic status in health disparities research. J. Natl. Med. Assoc. 2007, 99, 1013–1023. [Google Scholar]
- Keij, I. How does CBS work? Standard definition immigrants. In Index: Feiten en Cijfers over onze Samenleving; CBS: New York, NY, USA, 2000; Volume 7, pp. 24–255. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Taylor and Francis: Hoboken, NJ, USA, 1988; ISBN 9781134742707. [Google Scholar]
- Beauchamp, G.K.; Mennella, J. Early Flavor Learning and Its Impact on Later Feeding Behavior. J. Pediatr. Gastroenterol. Nutr. 2009, 48, S25–S30. [Google Scholar] [CrossRef]
- Domínguez, P.R.; Gámiz, F.; Gil, M.; Moreno, H.; Zamora, R.M.; Gallo, M.; de Brugada, I. Providing choice increases children’s vegetable intake. Food Qual. Pref. 2013, 30, 108–113. [Google Scholar] [CrossRef]
- Rabia, M.; Knäuper, B.; Miquelon, P. The eternal quest for optimal balance between maximizing pleasure and minimizing harm: The compensatory health beliefs model. Br. J. Health Psychol. 2006, 11, 139–153. [Google Scholar] [CrossRef]
- Berli, C.; Loretini, P.; Radtke, T.; Hornung, R.; Scholz, U. Predicting physical activity in adolescents: The role of compensatory health beliefs within the Health Action Process Approach. Psychol. Health 2013, 29, 458–474. [Google Scholar] [CrossRef] [PubMed]
- Amrein, M.A.; Rackow, P.; Inauen, J.; Radtke, T.; Scholz, U. The role of Compensatory Health Beliefs in eating behavior change: A mixed method study. Appetite 2017, 116, 1–10. [Google Scholar] [CrossRef]
- Radtke, T.; Kaklamanou, D.; Scholz, U.; Hornung, R.; Armitage, C.J. Are diet-specific compensatory health beliefs predictive of dieting intentions and behaviour? Appetite 2014, 76, 36–43. [Google Scholar] [CrossRef] [PubMed]
- European Commission School Scheme Explained. Available online: https://ec.europa.eu/info/food-farming-fisheries/key-policies/common-agricultural-policy/market-measures/school-fruit-vegetables-and-milk-scheme/school-scheme-explained_en (accessed on 22 April 2021).
- Schönbeck, Y.; Talma, H.; Van Dommelen, P.; Bakker, B.; Buitendijk, S.E.; HiraSing, R.A.; van Buuren, S. Increase in Prevalence of Overweight in Dutch Children and Adolescents: A Comparison of Nationwide Growth Studies in 1980, 1997 and 2009. PLoS ONE 2011, 6, e27608. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, M.; Krølner, R.; Klepp, K.-I.; Lytle, L.; Brug, J.; Bere, E.; Due, P. Determinants of fruit and vegetable consumption among children and adolescents: A review of the literature. Part I: Quantitative studies. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 22. [Google Scholar] [CrossRef]
- Brug, J.; Tak, N.I.; Velde, S.J.T.; Bere, E.; De Bourdeaudhuij, I. Taste preferences, liking and other factors related to fruit and vegetable intakes among schoolchildren: Results from observational studies. Br. J. Nutr. 2008, 99, S7–S14. [Google Scholar] [CrossRef] [PubMed]
- Lohrmann, D.K. A Complementary Ecological Model of the Coordinated School Health Program. Public Health Rep. 2008, 123, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Davison, K.K.; Birch, L.L. Childhood overweight: A contextual model and recommendations for future research. Obes. Rev. 2001, 2, 159–171. [Google Scholar] [CrossRef]
- Bronfenbrenner, U.; Morris, P.A.; Damon, W.; Lerner, R.M. The ecology of human developmental processes. In The Handbook of Child Psychology; John Wiley & Sons: New York, NY, USA, 1988; pp. 993–1027. [Google Scholar]

| Number of Included Participants, Divided Per Study Year (Study Year at T0 in Brackets) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study Year 4 | Study Year 5 | Study Year 6 | Study Year 7 | Study Year 8 1 | ||||||
| Full HPSF | Partial HPSF | Full HPSF | Partial HPSF | Full HPSF | Partial HPSF | Full HPSF | Partial HPSF | Full HPSF | Partial HPSF | |
| Timepoint | ||||||||||
| T0 (2015) | 48 | 53 | 53 | 61 | 51 | 45 | 58 | 67 | ||
| T1 (2016) | 51 (3) | 59 (3) | 50 (4) | 56 (4) | 57 (5) | 62 (5) | 53 (6) | 45 (6) | 60 (7) | 67 (7) |
| T2 (2017) | 60 (2) | 80 (2) | 52 (3) | 64 (3) | 55 (4) | 59 (4) | 59 (5) | 62 (5) | 53 (6) | 47 (6) |
| T3 (2018) | 48 (1) | 49 (1) | 60 (2) | 80 (2) | 52 (3) | 64 (3) | 55 (4) | 59 (4) | 59 (5) | 62 (5) |
| T4 (2019) | 3 (1) 2 | 6 (1) 2 | 48 (1) | 52 (1) | 63 (2) | 82 (2) | 53 (3) | 62 (3) | 56 (4) | 60 (4) |
| Fruit | Vegetables |
|---|---|
| Apple | Cucumber |
| Banana | Tomato |
| Grapes | Carrot |
| Kiwi | Bell pepper |
| Mango | Lettuce |
| Tangerine | Zucchini |
| Pear | Spinach |
| Orange | Eggplant |
| Melon | Onion |
| Pineapple | Leek |
| Peach | Peas |
| Strawberries | Brussels sprouts |
| Broccoli | |
| Green beans | |
| Cauliflower | |
| Kale |
| Total (n = 833) | Full HPSF (n = 394) With Exposure to FV | Partial HPSF (n = 439) Without Exposure to FV | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % Missing Values | %/M | SD | n | % Missing Values | %/M | SD | n | % Missing Values | %/M | SD | X2/t-Value | p | |
| Sex (% boys) 1 | 833 | 0 | 48 | 394 | 0 | 47 | 439 | 0 | 49 | 0.267 | 0.605 | |||
| Age (years) | 833 | 0 | 7.5 | 2.2 | 394 | 0 | 7.5 | 2.1 | 439 | 0 | 7.5 | 2.2 | 0.534 | 0.593 |
| Ethnicity (% Western) 1 | 599 | 28 | 96 | 287 | 27 | 94 | 312 | 29 | 97 | 2.566 | 0.109 | |||
| SES (%) 1 Lowest tertile | 629 189 | 25 | 30 | 292 82 | 26 | 28 | 337 107 | 23 | 32 | 1.180 | 0.554 | |||
| Middle tertile | 233 | 37 | 109 | 37 | 124 | 37 | ||||||||
| Highest tertile | 207 | 33 | 101 | 35 | 106 | 32 | ||||||||
| Familiarity (mean n unfamiliar items) 2 Fruit (range 0–12) | 418 | 50 | 0.9 | 1.6 | 198 | 50 | 1.0 | 1.6 | 220 | 50 | 0.9 | 1.5 | 0.155 | 0.877 |
| Vegetables (range 0–16) | 420 | 50 | 1.8 | 2.2 | 199 | 50 | 1.8 | 2.1 | 221 | 50 | 1.7 | 2.3 | 0.231 | 0.818 |
| Preference (mean n disliked items) 2 Fruit (range 0–12) | 393 | 53 | 1.4 | 1.8 | 184 | 53 | 1.5 | 1.9 | 209 | 52 | 1.3 | 1.7 | 0.982 | 0.327 |
| Vegetables (range 0–16) | 376 | 55 | 4.1 | 3.1 | 177 | 55 | 4.1 | 3.1 | 199 | 55 | 4.1 | 3.2 | −0.235 | 0.814 |
| Fruit intake (%) 1 (almost) Never | 403 21 | 52 | 5 | 190 11 | 52 | 6 | 213 10 | 52 | 5 | 3.684 | 0.298 | |||
| Sometimes (1–3 days per week) | 82 | 20 | 31 | 16 | 51 | 24 | ||||||||
| Often (4–6 days per week) | 125 | 31 | 62 | 33 | 63 | 30 | ||||||||
| Every day | 175 | 43 | 86 | 45 | 89 | 42 | ||||||||
| Vegetable intake (%) 1 (almost) Never | 380 15 | 54 | 4 | 184 8 | 53 | 4 | 196 7 | 55 | 4 | 5.026 | 0.170 | |||
| Sometimes (1–3 days per week) | 62 | 16 | 22 | 12 | 40 | 20 | ||||||||
| Often (4–6 days per week) | 143 | 38 | 72 | 39 | 71 | 36 | ||||||||
| Every day | 160 | 42 | 82 | 45 | 78 | 40 | ||||||||
| Full HPSF vs. Partial HPSF | |||||
|---|---|---|---|---|---|
| B (95% CI) | p | ES | |||
| Familiarity | Number of unfamiliar fruit items | T0–T1 | −0.222 (−0.487; −0.043) | 0.101 | −0.16 |
| T0–T2 | 0.031 (−0.271; 0.332) | 0.841 | 0.02 | ||
| T0–T3 | −0.102 (−0.426; 0.223) | 0.538 | −0.07 | ||
| T0–T4 | 0.351 (−0.005; 0.708) | 0.053 | 0.25 | ||
| Number of unfamiliar vegetable items | T0–T1 | −0.604 (−1.058; −0.150) | 0.009 * | −0.28 | |
| T0–T2 | −0.465 (−0.990; 0.060) | 0.083 | −0.21 | ||
| T0–T3 | −0.768 (−1.333; −0.203) | 0.008 * | −0.35 | ||
| T0–T4 | −0.469 (−1.083; 0.146) | 0.135 | −0.22 | ||
| Preferences | Number of disliked fruit items | T0–T1 | 0.127 (−0.203; 0.457) | 0.450 | 0.07 |
| T0–T2 | −0.031 (−0.423; 0.361) | 0.877 | −0.02 | ||
| T0–T3 | 0.094 (−0.335; 0.523) | 0.667 | 0.05 | ||
| T0–T4 | 0.083 (−0.391; 0.558) | 0.730 | 0.04 | ||
| Number of disliked vegetable items | T0–T1 | 0.808 (0.151; 1.464) | 0.016 * | 0.24 | |
| T0–T2 | 0.336 (−0.431; 1.103) | 0.390 | 0.10 | ||
| T0–T3 | 0.016 (−0.821; 0.853) | 0.970 | 0.00 | ||
| T0–T4 | 0.266 (−0.651; 1.184) | 0.569 | 0.08 | ||
| Full HPSF vs. Partial HPSF | |||
|---|---|---|---|
| OR (95% CI) | p | ||
| Fruit intake | T0–T1 | 0.609 (0.389; 0.952) | 0.030 * |
| T0–T2 | 0.626 (0.383; 1.021) | 0.061 | |
| T0–T3 | 0.798 (0.478; 1.334) | 0.390 | |
| T0–T4 | 0.451 (0.259; 0.786) | 0.005 * | |
| Vegetable intake | T0–T1 | 0.828 (0.490; 1.402) | 0.483 |
| T0–T2 | 1.330 (0.750; 2.359) | 0.329 | |
| T0–T3 | 1.009 (0.548; 1.856) | 0.978 | |
| T0–T4 | 1.008 (0.538; 1.887) | 0.981 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hahnraths, M.T.H.; Willeboordse, M.; van Assema, P.; Winkens, B.; van Schayck, C.P. The Effects of the Healthy Primary School of the Future on Children’s Fruit and Vegetable Preferences, Familiarity and Intake. Nutrients 2021, 13, 3241. https://doi.org/10.3390/nu13093241
Hahnraths MTH, Willeboordse M, van Assema P, Winkens B, van Schayck CP. The Effects of the Healthy Primary School of the Future on Children’s Fruit and Vegetable Preferences, Familiarity and Intake. Nutrients. 2021; 13(9):3241. https://doi.org/10.3390/nu13093241
Chicago/Turabian StyleHahnraths, Marla T. H., Maartje Willeboordse, Patricia van Assema, Bjorn Winkens, and Constant P. van Schayck. 2021. "The Effects of the Healthy Primary School of the Future on Children’s Fruit and Vegetable Preferences, Familiarity and Intake" Nutrients 13, no. 9: 3241. https://doi.org/10.3390/nu13093241
APA StyleHahnraths, M. T. H., Willeboordse, M., van Assema, P., Winkens, B., & van Schayck, C. P. (2021). The Effects of the Healthy Primary School of the Future on Children’s Fruit and Vegetable Preferences, Familiarity and Intake. Nutrients, 13(9), 3241. https://doi.org/10.3390/nu13093241







