5. Discussion
All the international organizations recommend exclusively breastfeeding for the first six months of life and continuation for at least one year once other food is introduced [
3]. The initial six months of life are critical for the infant’s health and development. Achieving optimal development and minimizing the risk for serious disease in the newborn is an important challenge for clinicians. High-risk infants, such as premature twins, may benefit from mothers’ milk; the duration of breastfeeding has remained below that for single, full-term infants.
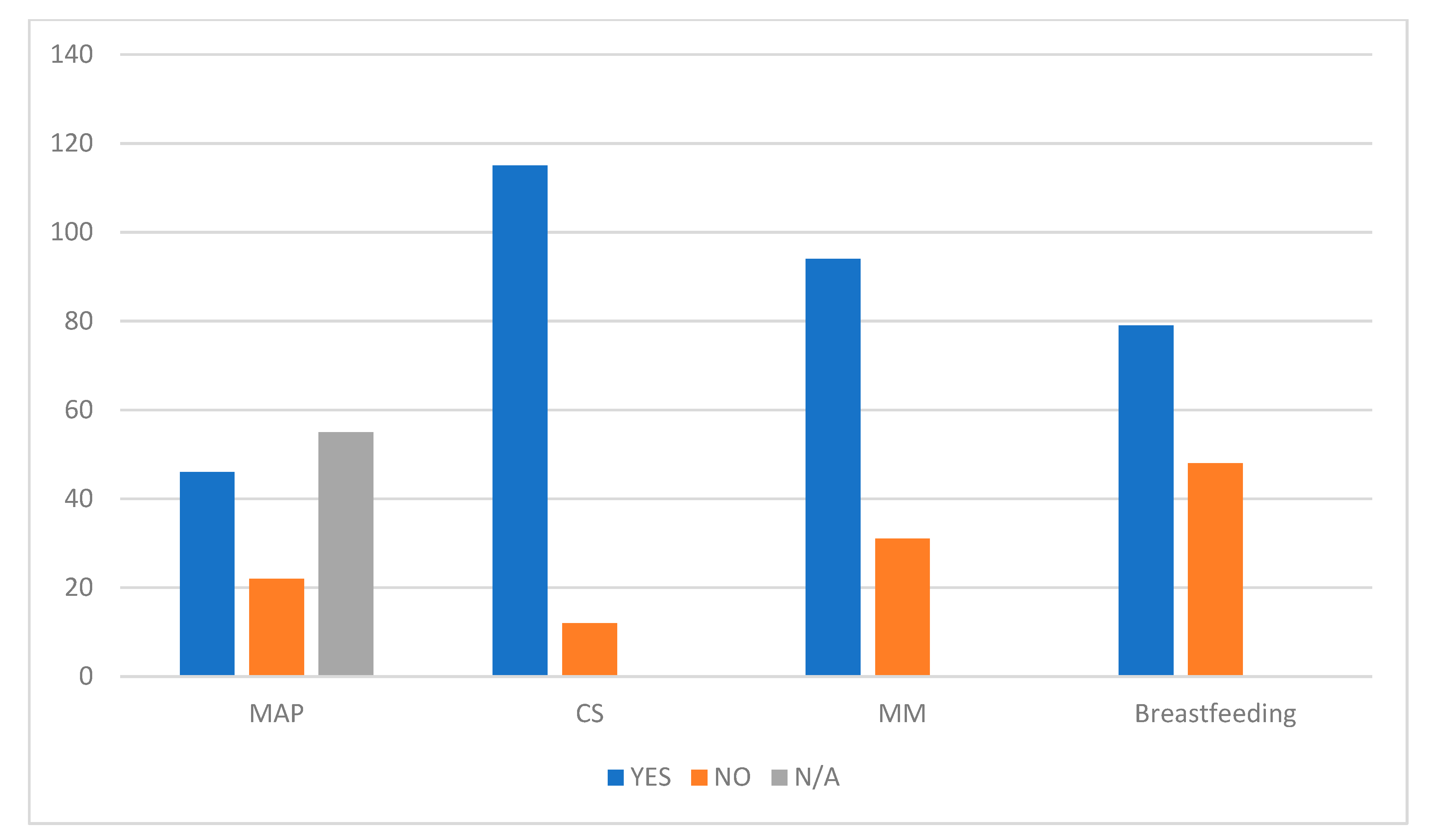
The best data on the rates of twins’ breastfeeding come from Sweden, where breastfeeding frequencies in preterm twins were 79% at 2 months, 58% at 4 months, 39% at 6 months, 14% at 9 months, and 6% at 12 months. In Poland, exclusive breastfeeding among twins and triplets was 4.9%, while that of the singletons was 73.2% [
22]. At six months, the overall breastfeeding rate in twins ranges from 11.1% to 49.6%, and the exclusive breastfeeding rate ranges from 4.1% to 21.5%. Another study [
29] in Denver reported that at six months, about 25% of twins and 15% of triplets receive breast milk. In our population, 22.8% received breast milk at 2 months, 7.9% at 6 months, and 4.7% at 12 months. This percentage is insufficient compared to the recommended standards and suggests that we should identify the factors for which we could intervene to improve it.
Previous researches [
30,
31,
32,
33,
34,
35,
36,
37] have identified associations between breastfeeding in the NICU and maternal characteristics, infant characteristics, and environmental factors. Many studies [
38,
39,
40,
41,
42,
43] reported the risk factors for early interruption of breastfeeding in mothers of singletons, and the most common are young age, low education, and single marital status.
Findings from a Swedish study [
19] indicate that maternal factors, such as educational level, smoking, and maternal age, were all individually related to the interruption of breastfeeding before six months of age, with low maternal educational level being an especially important factor.
In 2018, it was reported that there was a statistically significant impact of maternal age and profession on the volume of milk donation [
38].
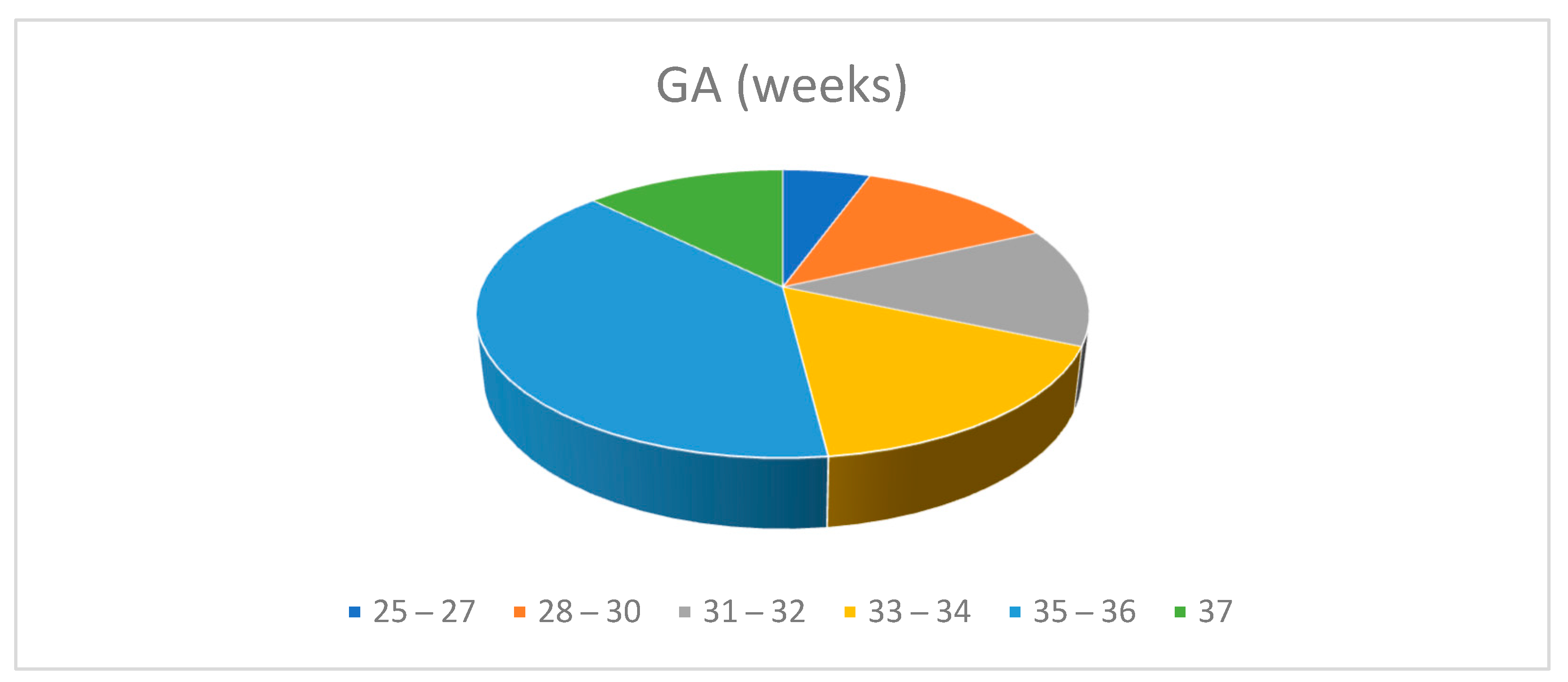
In this study, the correlation between the variables education, maternal age, parity, profession, type of birth, birth weight, gestational age, and the months of breastfeeding was statistically significant.
The presence of other children served as a stimulus for the mothers who wanted to give the twins the same health opportunity as the other children, or the older siblings were of help in the management of younger twins. For others, it represented a cause of stress and regret for not having been able to breastfeed for the same duration as for the previous child.
Women who have previous breastfeeding experience might be more prepared to breastfeed in a subsequent pregnancy and feel safer starting and maintaining breastfeeding two infants.
“I have been nursing the twins for about three months. I had to stop because my two other children cried. They always wanted to be with me. As you well know, you need to be tranquil if you breastfeed because it is a time you want to dedicate exclusively to your newborn. I missed this as I found myself with four small children together. I was very sorry but I had to make a choice: they would have risked having an exhausted mother!”
In the practice of the human milk bank, multiparous women were more numerous than primiparous ones [
38].
The Swedish study [
19] indicated that term infants had longer breastfeeding duration if the mother was multiparous, in agreement with other studies on the impact of parity on breastfeeding duration [
22,
33]. However, there is an opposite outcome [
23,
26] if the infants are born preterm; then, being multiparous may not be as beneficial.
This is because multiparous mothers of preterm twins may experience a greater deal of exhaustion with older children at home and newborns admitted to a neonatal unit [
39], whereas primiparous mothers of preterm twins may have more time for the infants and can be focused on breastfeeding.
Our results suggest intensifying care aimed at promoting breastfeeding for primiparous mothers.
Prematurity adds to the already significant challenges of initiating and maintaining lactation for twins and higher order multiples [
23]. Preterm twins showed an increased risk of being weaned compared to term [
19] and twin infants born prematurely, who are less likely than twins born at term to be breastfed.
Some studies [
40,
41,
42,
43] reported that higher gestational age is associated with higher rates of breastfeeding.
The data are, however, contradictory since some authors [
43] reported that 70% of mothers did not practice exclusive breastfeeding as a result of NICU admission, while others [
44] found 68% of mothers practiced exclusive breastfeeding at NICU.
In our study, there was a higher incidence of exclusive breast milk feeding among multiples with preterm gestational age < 33 weeks. It is further confirmation of another work [
45] where we highlighted that, if motivated and if breast stimulation is initiated early on, mothers of extremely premature infants can exclusively feed their infants in NICU with breast milk. This is in agreement with others studies [
24] that have found that mothers of VLBW infants acknowledge that human milk is a unique factor in improving outcomes for their infant, and consequently, breastfeeding rates in such cases are higher.
Probably, as for VLBW, gestational age-specific breastfeeding promotion protocols should also be intensified for twins of greater GA.
Older women breastfeed longer. This advocates the need for greater support for breastfeeding twins for younger women.
In this analysis, the main reason for interrupting breastfeeding was insufficient milk production.
Studies confirmed that the most common reason given for the interruption of breastfeeding by mothers of multiples [
46] is insufficient milk production. Mothers may associate infants’ excessive crying or irritability with symptoms of hunger and, consequently, with insufficient human milk supply [
28]. It is estimated [
47] that six months after childbirth, the body of a mother of twins can produce from 1.0 to 2.0 kg of milk per day, while a body of a mother of triplets can produce more than 3.0 kg. Instead, in our experience, the idea of insufficient milk production for two or more newborns is considered a common opinion of many mothers and caregivers. Nevertheless, it has no scientific support.
One of the lessons that comes from this work is that communicative effort must be intensified to convey the message of the adequacy of the amount of milk that the mothers of the twins can produce.
Some authors [
23] are convinced that the gap between breastfeeding of twins and that of singletons and that between the percentages of onset and duration may be reduced by evidence-based interventions tailored to families with multiples. Mothers of twins may benefit from breastfeeding support approaches tailored to their needs.
In addition to the family context, educated healthcare professionals should give relevant information about the adequacy criteria for mother’s milk and encourage the mothers in breastfeeding during the early stages of the establishment of breastfeeding. Since in the area there are no experts who can provide breastfeeding assistance at home, illustrated documents and videos about nourishment and nursing for the multiple babies should be offered to the mothers.
Another proposal that is being planned is the activation of a telephone number dedicated to breastfeeding: each mother who needs advice, verbal help, comfort, or reassurance on issues concerning breastfeeding can contact the nursery and find a doctor or nurse who is ready to provide the necessary support.
From the qualitative analysis of the answers, it emerged that the second deterrent to the prolongation of breastfeeding is the stress associated with managing two or more babies.
The women who had help available received it from family members. In our study, those who received help breastfed the longest. Nevertheless, a certain percentage of women stopped breastfeeding despite having the help of family members. This is because they felt unprepared to breastfeed two babies at the same time.
Correct training of pregnant women may play a positive role with multiple pregnancies. This training must see the necessary involvement of the family, which must be material and motivational. Sometimes the invitation to abandon breastfeeding in favour of formula milk comes from family members because they are convinced that, in a way, the stress of managing twins can be reduced, while on the contrary, breastfeeding, if fully utilized, is a method of reducing stress for the mother and the little ones. Exploring the topic of possible methods of reducing stress after a twin birth and their possible factors can be a way to extend the duration of breastfeeding at least up to six months, the same as for single-born babies.
In our area, there is little presence of breastfeeding experts who, on the other hand, would be crucial for the goal of improving breastfeeding for twins. The ideal would be that of a multidisciplinary team that supports mother and family in dealing with the clinical, psychological, and practical management difficulties in the weeks following the birth from the moment of discharge.
In the experience of the women interviewed, it emerged that there is a lack of proper breastfeeding preparation during pregnancy and an absence of expert voices after returning home.
The keywords of the approach to pregnancy and childbirth are information and support. We would like these to become a mantra for the care of women who live this intense experience of life that is the birth of twins. This could lead to greater personal conviction.
In our experience, mothers who have breastfed for more than 12 months are those who initially had a strong personal belief that breast milk was a unique opportunity for their children and strongly believed in the power of breastfeeding.
Women with a stronger motivation gave priority to breastfeeding in the management of twins, and this has led to brilliant results in terms of breastfeeding duration.
“I wanted to pump my milk immediately after the birth of my 900 g twins, be-cause I only wanted to give my milk and, as soon as it was possible, I attached them to the breast. They still are and are 4 years old. Then I felt sorry for the other babies and I donated my milk to them too”.
In another interview:
“I breastfed both twins until the twentieth month of life then I voluntarily decided to stop even if I still had milk. The breastfeeding experience of the twins is unique, I often used the rugby position to please both at the same time even though I much preferred exclusive breastfeeding with each one to fully enjoy that intimate and unrepeatable moment”.
Did you have any help with the twins?
“Yes, of course, the two grandmothers”
A weaker motivation, despite the awareness of the benefits of breast milk, often gives way to fears of not being able to feed the twins with their own milk or manage family life. This context triggered regrets and guilt and led to the abandonment of breastfeeding in the first 2–3 months. Women who were convinced that enough milk could not be produced for more babies abandoned breastfeeding early.
When a mother is pregnant with twins (or multiples), a screening to select whether a mother needs a low, moderate, or higher level of support might be useful.
Limits and Opportunities
One of the limits of this study is represented by the fact that the data came from a single centre, while a survey on the whole national territory would be useful. The valuable information resulting from this experience could represents a useful opportunity for improving the breastfeeding rate of twins.
6. Conclusions
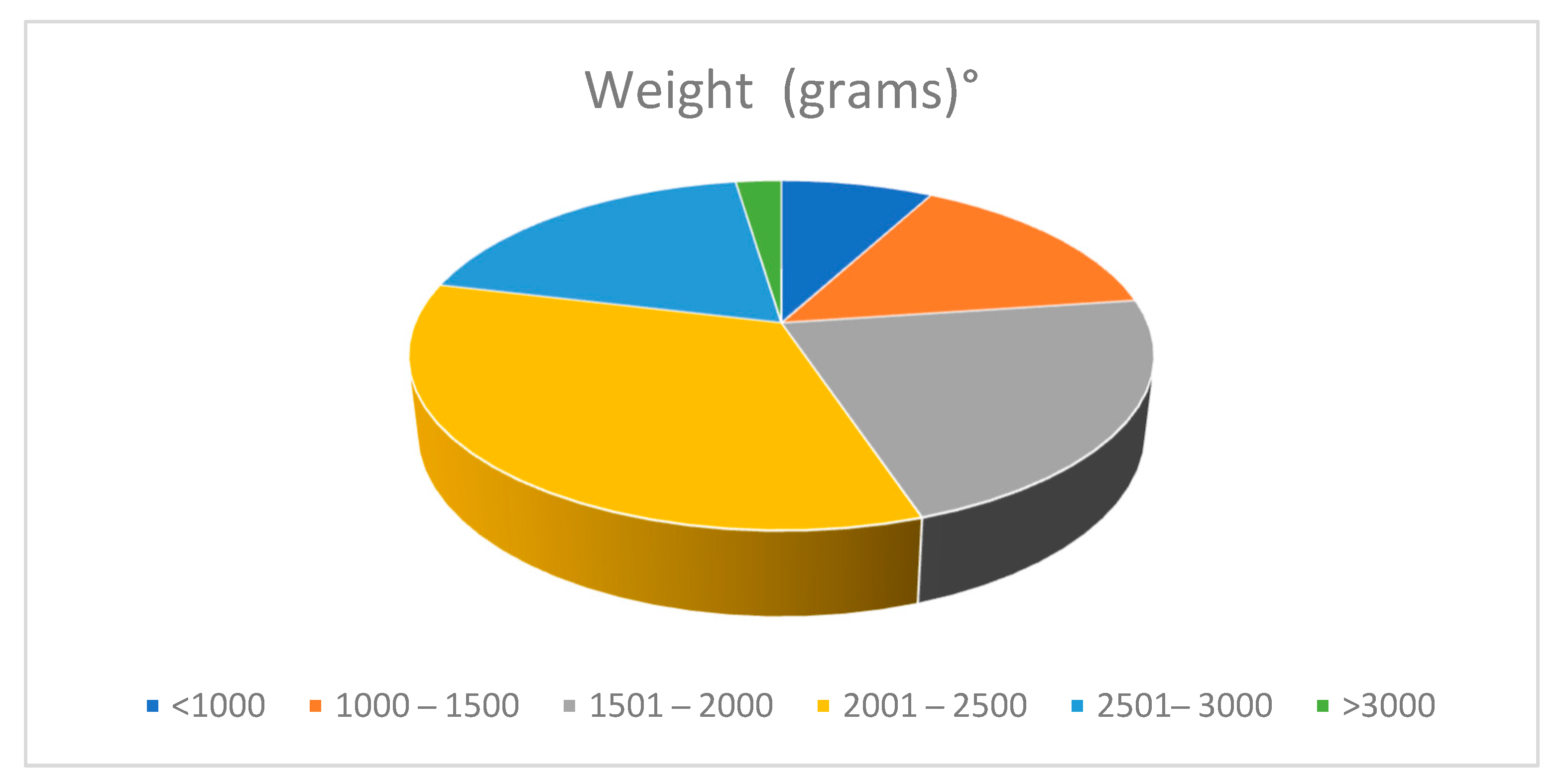
The incidence in our clinical centre of twin births doubled in six years, in line with Italian and European data. The use of breast milk and the breastfeeding of twins recorded percentages below the standards indicated by the WHO. The age, the educational level, and the parity were the maternal factors statistically correlated with the duration of breastfeeding. Better results were obtained with older mothers, a higher educational level, and multiple parity. These data suggest the desirability of greater support for mothers who are younger and with a lower educational level. Multiparity, on the other hand, did not represent a prejudice to prolonged breastfeeding.
The neonatal factors that impacted breastfeeding rates were birth weight and gestational age, with the best performance observed for the lower weight and lower gestational age categories of newborns. Care dedicated to breastfeeding should be intensified for mothers of siblings of greater weight and gestational age.
The main reasons for interrupting breastfeeding are insufficient milk production, stress and difficulties in managing the twins. The concept that breast milk may be sufficient to breastfeed twins should be more widespread, as reiterated by the WHO.
About 50% of mothers of twins did not receive any help. The presence of experts for the support of mothers was not even named in our results, confirming a welfare gap in the area. Support was provided within the family, and the most important role was played by grandparents, who are traditionally fundamental social figures, particularly in this historical period in our area. Family support had a statistically significant impact on the duration of breastfeeding. Support implementation programs run by health professionals in the first months after delivery are desirable for stress containment.
Qualitative analysis revealed that, for many mothers, there was an awareness of the importance of breastfeeding and efforts made to try to give breast milk, but there were also fears about the quantity of milk and satiety of their children.
It would be interesting to evaluate the outcome of twins fed with breast milk and those with formula milk, and this will be the subject of a future study.