Oxygen Sparing Effect of Bacteriotherapy in COVID-19
Abstract
:1. Introduction
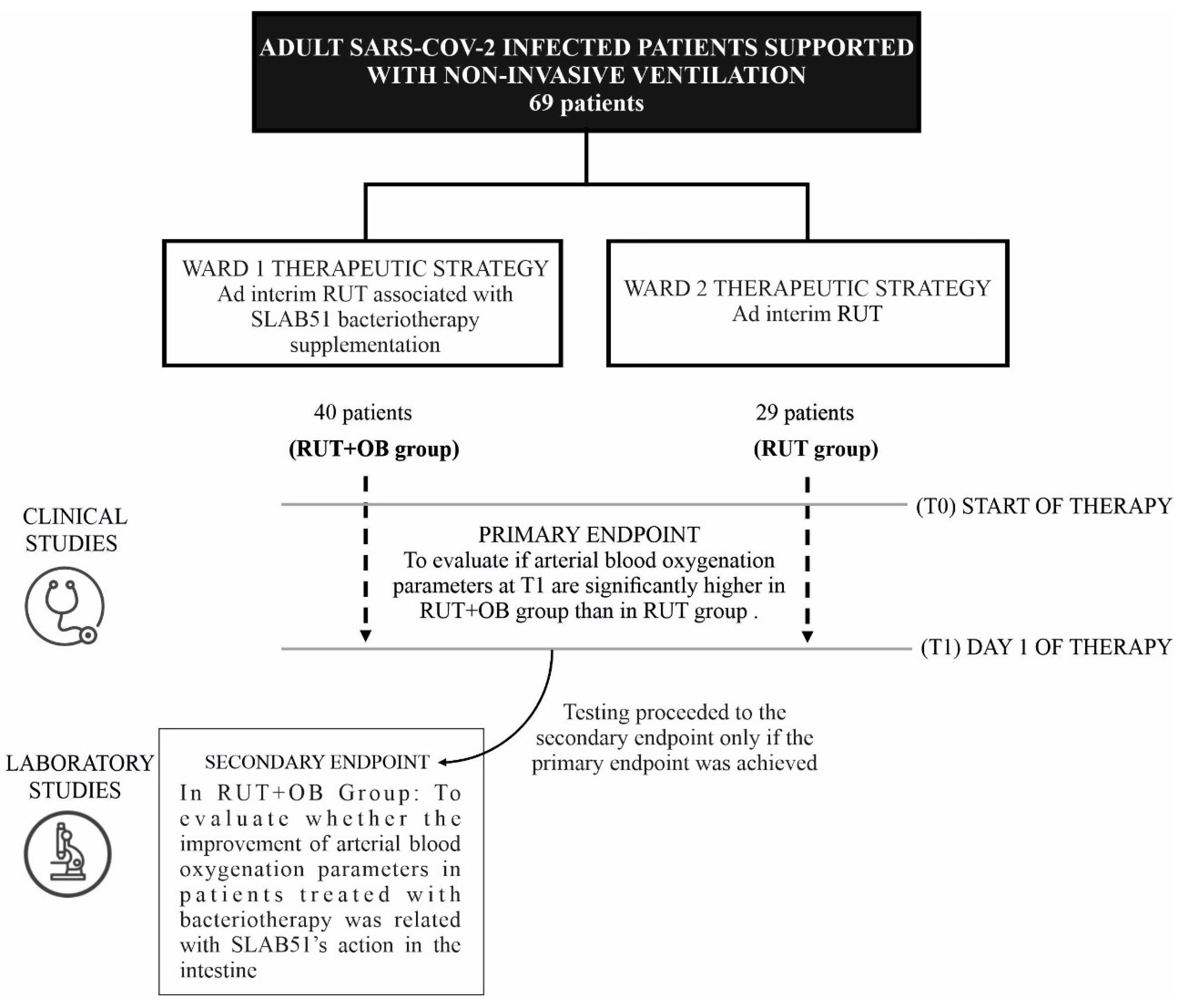
2. Materials and Methods
2.1. Design of the Study, Population, Settings and Data Collection
2.2. Diagnosis of SARS-CoV-2 Infection
2.3. COVID-19 Treatments
2.4. Supplemental Oxygen
2.5. Ethics Committee Approval
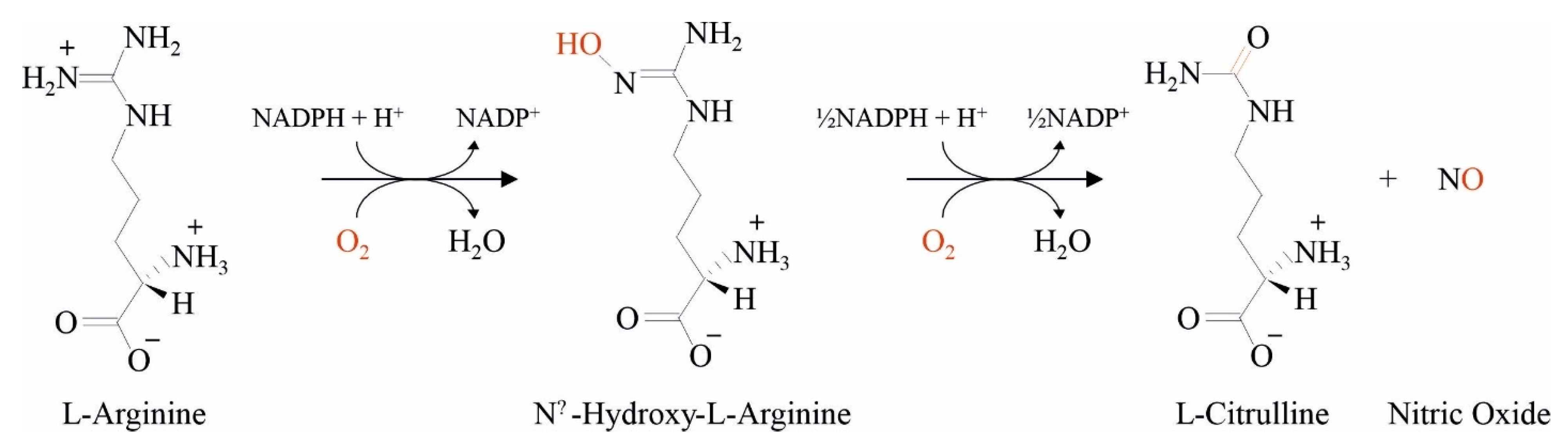
2.6. Arginine Deiminase (ADI) Assay
2.7. Cell Line, Culture Condition and Treatment
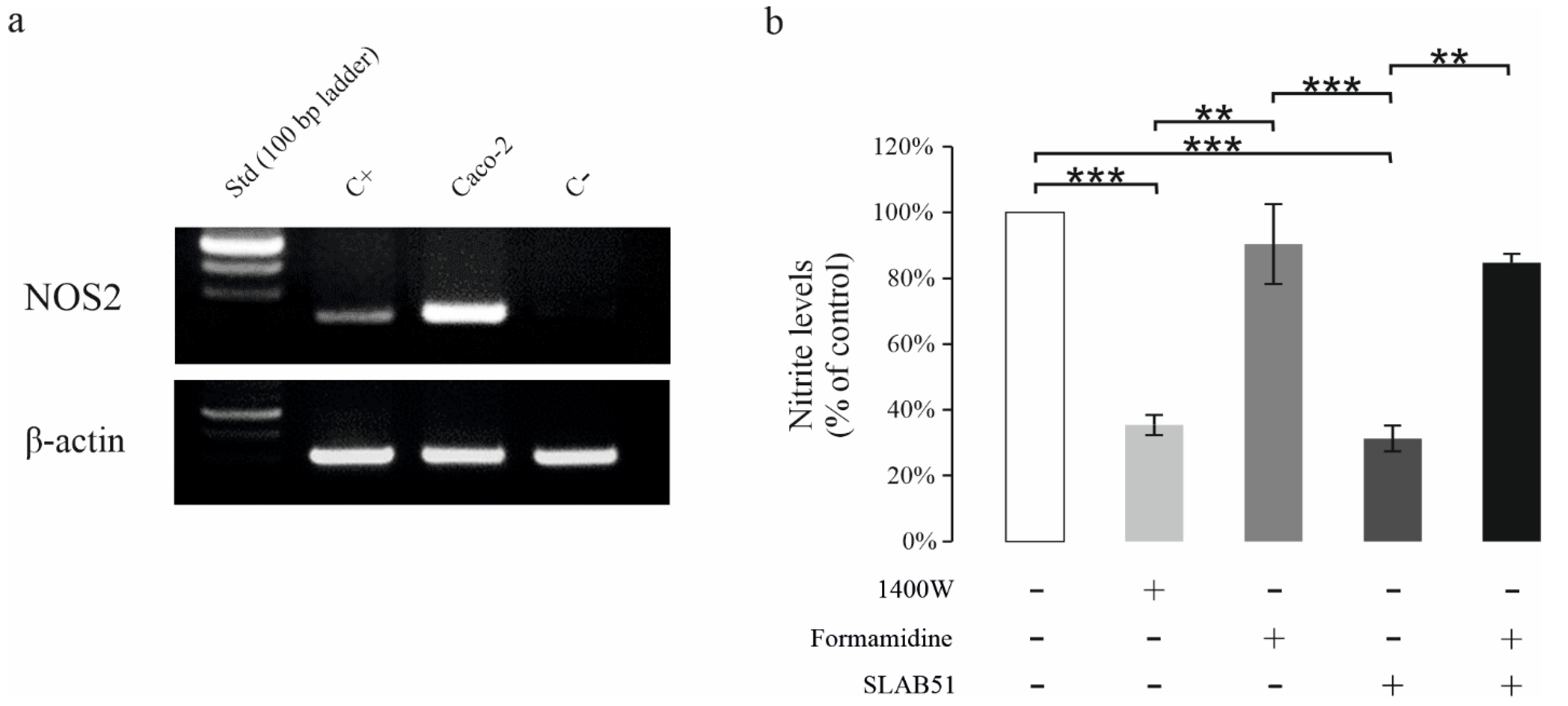
2.8. Total RNA Extraction and NOS2 Expression by RT-PCR
2.9. Nitrite Level Assay
2.10. Statistical Analysis
3. Results
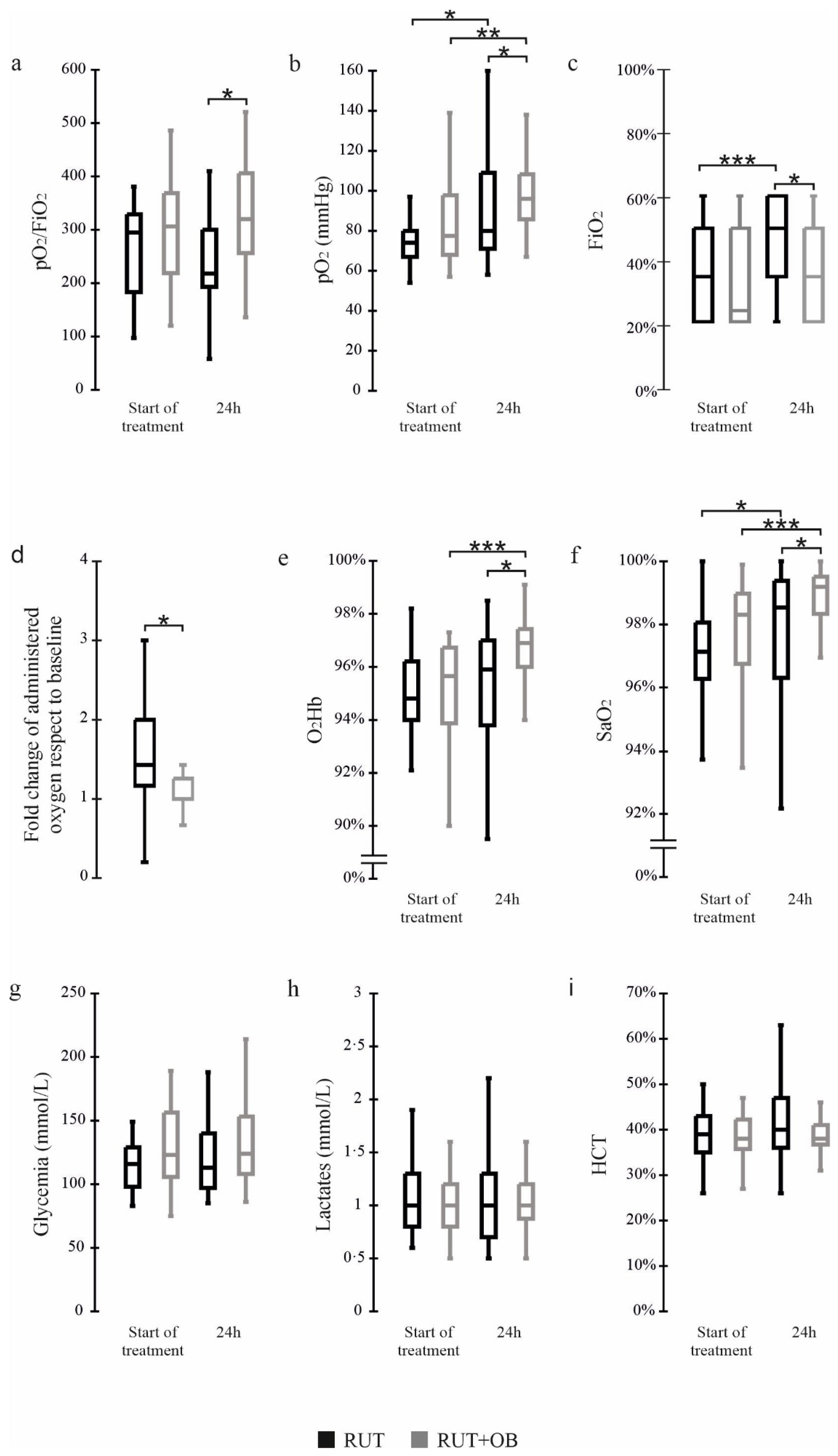
3.1. Primary Endpoint
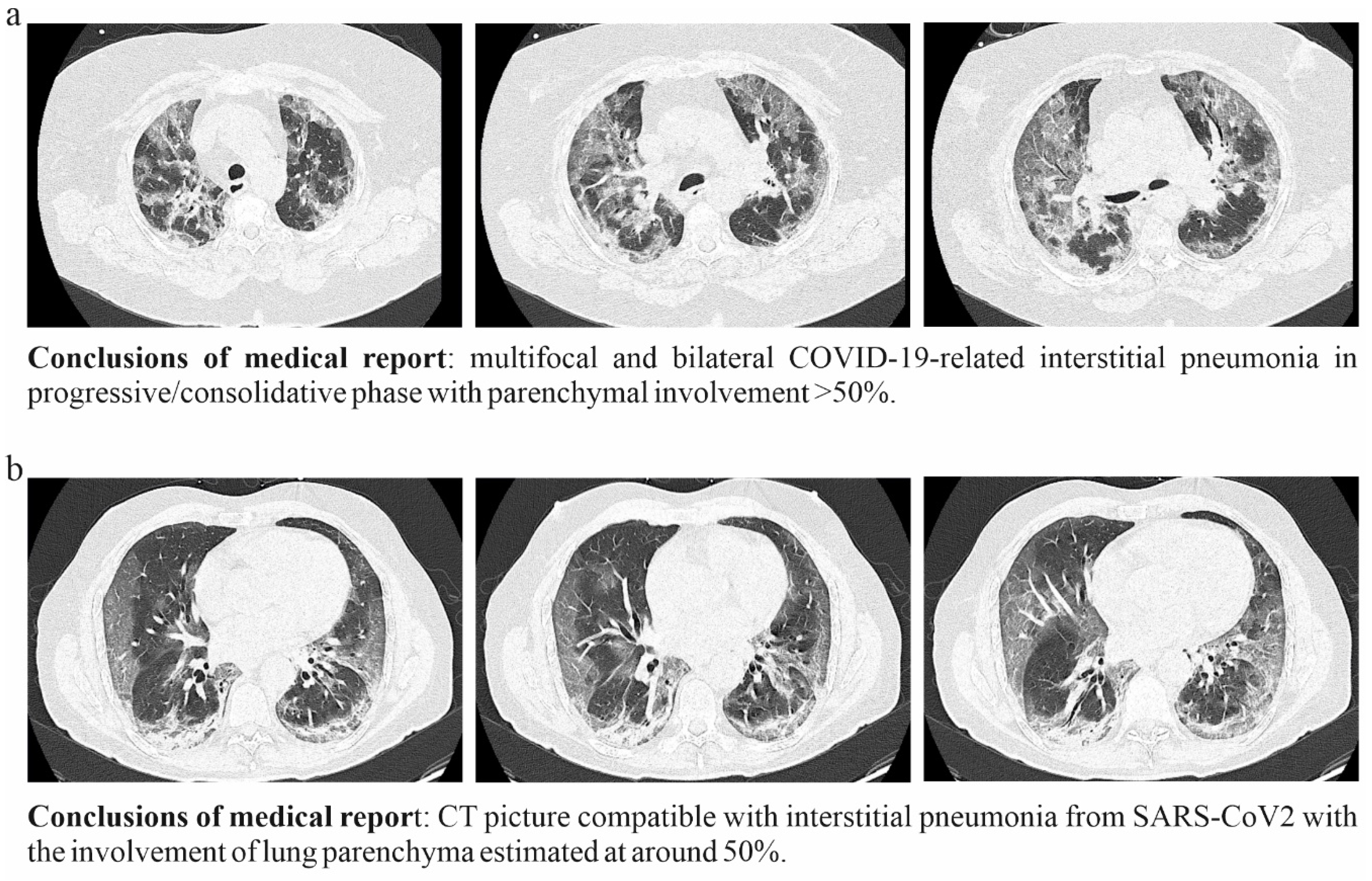
3.2. Secondary Endpoint
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sundararaman, A.; Ray, M.; Ravindra, P.V.; Halami, P.M. Role of probiotics to combat viral infections with emphasis on COVID-19. Appl Microbiol. Biotechnol. 2020, 104, 8089–8104. [Google Scholar] [CrossRef]
- Giannoni, E.; Baud, D.; Agri, V.D.; Gibson, G.R.; Reid, G. Probiotics and COVID-19. Lancet Gastroenterol. Hepatol. 2020, 5, 720–721. [Google Scholar] [CrossRef]
- Baud, D.; Dimopoulou Agri, V.; Gibson, G.R.; Reid, G.; Giannoni, E. Using Probiotics to Flatten the Curve of Coronavirus Disease COVID-2019 Pandemic. Front. Public Health. 2020, 8, 186. [Google Scholar] [CrossRef]
- Ceccarelli, G.; Borrazzo, C.; Pinacchio, C.; Santinelli, L.; Innocenti, G.P.; Cavallari, E.N.; Celani, L.; Marazzato, M.; Alessandri, F.; Ruberto, F.; et al. Oral Bacteriotherapy in Patients With COVID-19: A Retrospective Cohort Study. Front. Nutr. 2021, 7, 613928. [Google Scholar] [CrossRef]
- d’Ettorre, G.; Ceccarelli, G.; Marazzato, M.; Campagna, G.; Pinacchio, C.; Alessandri, F.; Ruberto, F.; Rossi, G.; Celani, L.; Scagnolari, C.; et al. Challenges in the Management of SARS-CoV2 Infection: The Role of Oral Bacteriotherapy as Complementary Therapeutic Strategy to Avoid the Progression of COVID-19. Front. Med. 2020, 7, 389. [Google Scholar] [CrossRef]
- Grimes, J.M.; Khan, S.; Badeaux, M.; Rao, R.M.; Rowlinson, S.W.; Carvajal, R.D. Arginine depletion as a therapeutic approach for patients with COVID-19. Int J. Infect. Dis. 2021, 102, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Abruzzo, A.; Vitali, B.; Lombardi, F.; Guerrini, L.; Cinque, B.; Parolin, C.; Bigucci, F.; Cerchiara, T.; Arbizzani, C.; Gallucci, M.C.; et al. Mucoadhesive Buccal Films for Local Delivery of Lactobacillus brevis. Pharmaceutics 2020, 12, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palumbo, P.; Miconi, G.; Cinque, B.; Lombardi, F.; La Torre, C.; Dehcordi, S.R.; Galzio, R.; Cimini, A.; Giordano, A.; Cifone, M.G. NOS2 expression in glioma cell lines and glioma primary cell cultures: Correlation with neurosphere generation and SOX-2 expression. Oncotarget 2017, 8, 25582–25598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014; Available online: http://www.R-project.org/ (accessed on 1 May 2021).
- Panaro, M.A.; Carofiglio, V.; Acquafredda, A.; Cavallo, P.; Cianciulli, A. Anti-inflammatory effects of resveratrol occur via inhibition of lipopolysaccharide-induced NF-κB activation in Caco-2 and SW480 human colon cancer cells. Br. J. Nutr. 2012, 108, 1623–1632. [Google Scholar] [CrossRef] [Green Version]
- Palumbo, P.; Lombardi, F.; Augello, F.R.; Giusti, I.; Luzzi, S.; Dolo, V.; Cifone, M.G.; Cinque, B. NOS2 inhibitor 1400 W Induces Autophagic Flux and Influences Extracellular Vesicle Profile in Human Glioblastoma U87MG Cell Line. Int J. Mol. Sci. 2019, 20, 3010. [Google Scholar] [CrossRef] [Green Version]
- Riccia, D.N.; Bizzini, F.; Perilli, M.G.; Polimeni, A.; Trinchieri, V.; Amicosante, G.; Cifone, M.G. Anti-inflammatory effects of Lactobacillus brevis (CD2) on periodontal disease. Oral Dis. 2007, 13, 376–385. [Google Scholar] [CrossRef]
- Rabi, F.A.; Al Zoubi, M.S.; Kasasbeh, G.A.; Salameh, D.M.; Al-Nasser, A.D. SARS-CoV-2 and Coronavirus Disease 2019: What We Know So Far. Pathogens 2020, 9, 231. [Google Scholar] [CrossRef]
- Mach, W.J.; Thimmesch, A.R.; Pierce, J.T.; Pierce, J.D. Consequences of hyperoxia and the toxicity of oxygen in the lung. Nurs Res. Pract. 2011, 2011, 260482. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Bellan, M.; Soddu, D.; Balbo, P.E.; Baricich, A.; Zeppegno, P.; Avanzi, G.C.; Baldon, G.; Bartolomei, G.; Battaglia, M.; Battistini, S.; et al. Respiratory and Psychophysical Sequelae Among Patients with COVID-19 Four Months after Hospital Discharge. JAMA Netw. Open 2021, 4, e2036142. [Google Scholar] [CrossRef] [PubMed]
- Lundquist, P.; Artursson, P. Oral absorption of peptides and nanoparticles across the human intestine: Opportunities, limitations and studies in human tissues. Adv. Drug Deliv. Rev. 2016, 106 Pt B, 256–276. [Google Scholar] [CrossRef]
- Moncada, S.; Palmer, R.M.; Higgs, E.A. The discovery of nitric oxide as the endogenous nitrovasodilator. Hypertension 1988, 12, 365–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ignarro, L.J. Nitric oxide as a unique signaling molecule in the vascular system: A historical overview. J. Physiol. Pharmacol. 2002, 53 Pt 1, 503–514. [Google Scholar] [PubMed]
- Singhal, R.; Shah, Y.M. Oxygen battle in the gut: Hypoxia and hypoxia-inducible factors in metabolic and inflammatory responses in the intestine. J. Biol. Chem. 2020, 295, 10493–10505. [Google Scholar] [CrossRef] [PubMed]
- Zuo, T.; Zhang, F.; Lui, G.C.Y.; Yeoh, Y.K.; Li, A.Y.L.; Zhan, H.; Wan, Y.; Chung, A.C.K.; Cheung, C.P.; Chen, N.; et al. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization. Gastroenterology 2020, 159, 944–955.e8. [Google Scholar] [CrossRef]
- Perrone, L.A.; Belser, J.A.; Wadford, D.A.; Katz, J.M.; Tumpey, T.M. Inducible nitric oxide contributes to viral pathogenesis following highly pathogenic influenza virus infection in mice. J. Infect. Dis. 2013, 207, 1576–1584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Izzo, F.; Marra, P.; Beneduce, G.; Castello, G.; Vallone, P.; De Rosa, V.; Cremona, F.; Ensor, C.M.; Holtsberg, F.W.; Bomalaski, J.S.; et al. Pegylated arginine deiminase treatment of patients with unresectable hepatocellular carcinoma: Results from phase I/II studies. J. Clin. Oncol. 2004, 22, 1815–1822. [Google Scholar] [CrossRef] [PubMed]
- Sekirov, I.; Russell, S.L.; Antunes, L.C.; Finlay, B.B. Gut microbiota in health and disease. Physiol. Rev. 2010, 90, 859–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ceccarelli, G.; Scagnolari, C.; Pugliese, F.; Mastroianni, C.M.; D’Ettorre, G. Probiotics and COVID-19. Lancet Gastroenterol. Hepatol. 2020, 5, 721–722. [Google Scholar] [CrossRef]

| Parameter | RUT (No. = 29) | RUT + OB (No. = 40) | p-Value | ||
|---|---|---|---|---|---|
| Median (IQR) | No. (%) | Median (IQR) | No. (%) | ||
| Age (years) | 70 (60–77) | 61 (51–74·3) | 0.09 | ||
| Sex (Male) | 25 (86·2) | 22 (55) | 0.01 | ||
| BMI–kg/m3 | 20 (20–22) | 20 (18·8–22) | 0.47 | ||
| Alanine aminotransferase (ALT)–IU/L | 25 (18–40) | 30 (23·5–45) | 0.17 | ||
| Aspartate aminotransferase (AST)–IU/L | 21 (19–38) | 26 (18–36.3) | 0.95 | ||
| CT score | 16.5 (15–18) | 16.5 (15–18) 5 | 0.91 | ||
| Charlson index | 3 (1–4) | 1 (1–5) | 0.24 | ||
| Drug therapy | |||||
| Antiviral (Remdesivir) | 10 (34.4) | 8 (20) | 0.28 | ||
| Antibiotic | 25 (86.2) | 39 (97.5) | 0.19 | ||
| pO2/FiO2 | pO2 (mmHg) | FiO2 (%) | O2Hb (%) | SaO2 (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 h | 6 h | 0 h | 6 h | 0 h | 6 h | 0 h | 6 h | 0 h | 6 h | ||
| RUT | Patient 1 | 319 | 278 | 96 | 63 | 21 | 28 | 96.6 | 92 | 98 | 93 |
| Patient 2 | 310 | 175 | 65 | 35 | 21 | 40 | 93 | 94.2 | 98.8 | 98.2 | |
| RUT+OB | Patient 3 | 352 | 390 | 76 | 86 | 21 | 21 | 95.3 | 96.9 | 96.9 | 98.9 |
| Patient 4 | 328 | 354 | 69 | 89 | 21 | 21 | 82 | 96 | 96 | 98 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceccarelli, G.; Marazzato, M.; Celani, L.; Lombardi, F.; Piccirilli, A.; Mancone, M.; Trinchieri, V.; Pugliese, F.; Mastroianni, C.M.; d’Ettorre, G. Oxygen Sparing Effect of Bacteriotherapy in COVID-19. Nutrients 2021, 13, 2898. https://doi.org/10.3390/nu13082898
Ceccarelli G, Marazzato M, Celani L, Lombardi F, Piccirilli A, Mancone M, Trinchieri V, Pugliese F, Mastroianni CM, d’Ettorre G. Oxygen Sparing Effect of Bacteriotherapy in COVID-19. Nutrients. 2021; 13(8):2898. https://doi.org/10.3390/nu13082898
Chicago/Turabian StyleCeccarelli, Giancarlo, Massimiliano Marazzato, Luigi Celani, Francesca Lombardi, Alessandra Piccirilli, Massimo Mancone, Vito Trinchieri, Francesco Pugliese, Claudio M. Mastroianni, and Gabriella d’Ettorre. 2021. "Oxygen Sparing Effect of Bacteriotherapy in COVID-19" Nutrients 13, no. 8: 2898. https://doi.org/10.3390/nu13082898
APA StyleCeccarelli, G., Marazzato, M., Celani, L., Lombardi, F., Piccirilli, A., Mancone, M., Trinchieri, V., Pugliese, F., Mastroianni, C. M., & d’Ettorre, G. (2021). Oxygen Sparing Effect of Bacteriotherapy in COVID-19. Nutrients, 13(8), 2898. https://doi.org/10.3390/nu13082898










