Independent Determinants of Appetite Impairment among Patients with Stage 3 or Higher Chronic Kidney Disease: A Prospective Study
Abstract
:1. Introduction
2. Methods
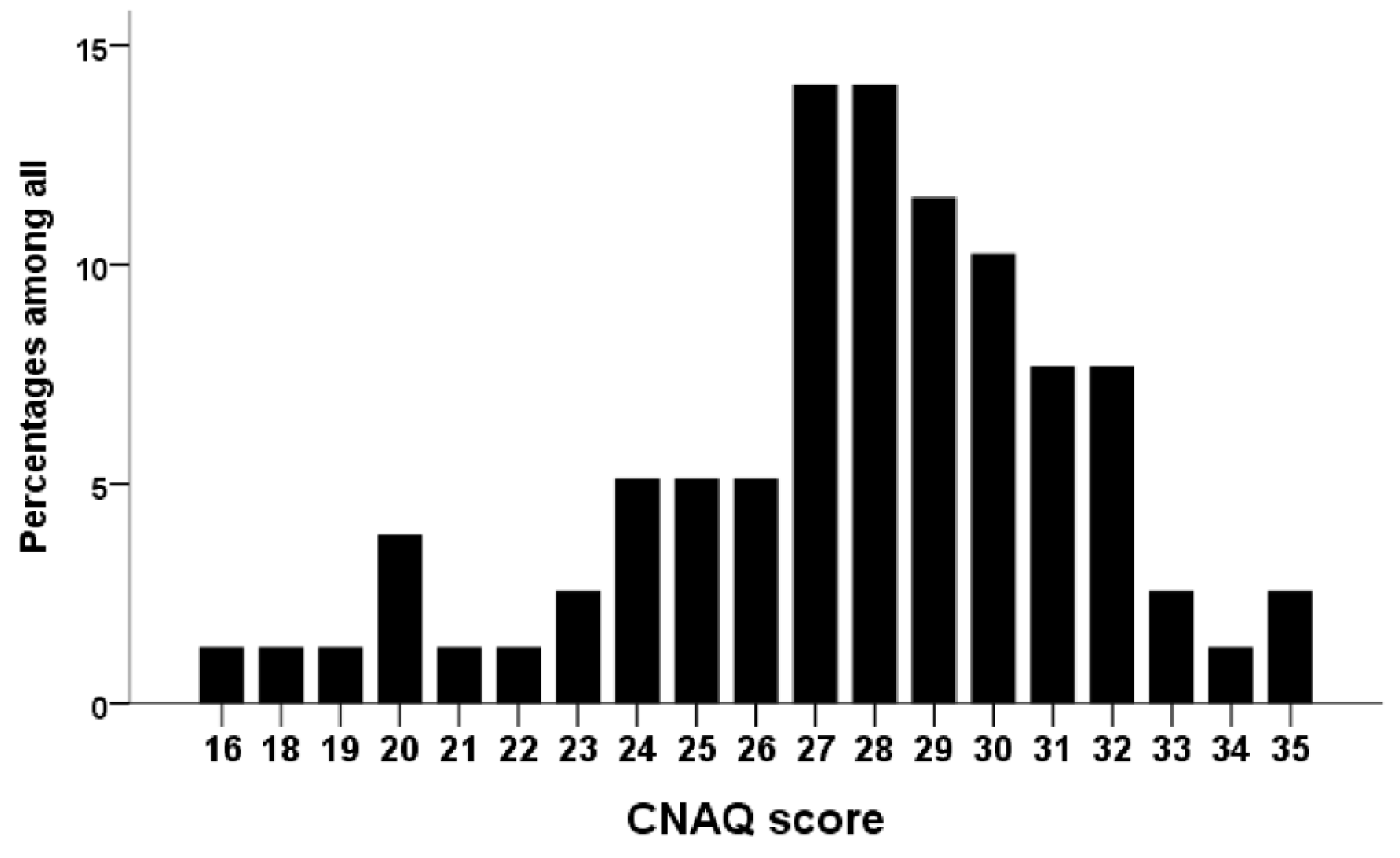
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Coresh, J.; Selvin, E.; Stevens, L.A.; Manzi, J.; Kusek, J.W.; Eggers, P.; van Lente, F.; Levey, A.S. Prevalence of Chronic Kidney Disease in the United States. JAMA 2007, 298, 2038–2047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanna, R.M.; Ghobry, L.; Wassef, O.; Rhee, C.M.; Kalanter-Zadeh, K. A Practical Approach to Nutrition, Protein-Energy Wasting, Sarcopenia, and Cachexia in Patients with Chronic Kidney Disease. Blood Purif. 2020, 49, 202–211. [Google Scholar] [CrossRef]
- Chao, C.T.; Tang, C.H.; Cheng, R.W.Y.; Wang, M.Y.H.; Hung, K.Y. Protein-energy wasting significantly increases healthcare utilisation and costs among patients with chronic kidney disease: A propensity-score matched cohort study. Curr. Med. Res. Opin. 2017, 33, 1705–1713. [Google Scholar] [CrossRef]
- Carrero, J.J.; Stenvinkel, P.; Cuppari, L.; Ikizler, T.A.; Kalantar-Zadeh, K.; Kaysen, G.; Mitch, W.E.; Price, S.R.; Wanner, C.; Wang, A.Y.M.; et al. Etiology of the Protein-Energy Wasting Syndrome in Chronic Kidney Disease: A Consensus Statement From the International Society of Renal Nutrition and Metabolism (ISRNM). J. Ren. Nutr. 2013, 23, 77–90. [Google Scholar] [CrossRef] [Green Version]
- Sabatino, A.; Piotti, G.; Cosola, C.; Gandolfini, I.; Kooman, J.P.; Fiaccadori, E. Dietary protein and nutritional supplements in conventional hemodialysis. Semin. Dial. 2018, 31, 583–591. [Google Scholar] [CrossRef]
- Carrero, J.J. Identification of Patients with Eating Disorders: Clinical and Biochemical Signs of Appetite Loss in Dialysis Patients. J. Ren. Nutr. 2009, 19, 10–15. [Google Scholar] [CrossRef]
- Chao, C.T.; Lin, S.H. Uremic toxins and frailty in patients with chronic kidney disease: A molecular insight. Int. J. Mol. Sci. 2021, 22, 6270. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.I.; Chiang, C.L.; Chao, C.T.; Chiang, C.K.; Huang, J.W. Gustatory Dysfunction Is Closely Associated with Frailty in Patients with Chronic Kidney Disease. J. Ren. Nutr. 2021, 31, 49–56. [Google Scholar] [CrossRef]
- Stevens, P.E.; Levin, A. Evaluation and Management of Chronic Kidney Disease: Synopsis of the Kidney Disease: Improving Global Outcomes 2012 Clinical Practice Guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.I.; Chiang, C.L.; Chao, C.T.; Chiang, C.K.; Huang, J.W. Gustatory Function and the Uremic Toxin, Phosphate, Are Modulators of the Risk of Vascular Calcification among Patients with Chronic Kidney Disease: A Pilot Study. Toxins 2020, 12, 420. [Google Scholar] [CrossRef]
- Morley, J.E.; Malmstrom, T.K.; Miller, D.K. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J. Nutr. Health Aging 2012, 16, 601–608. [Google Scholar] [CrossRef] [Green Version]
- Ensrud, K.E.; Ewing, S.K.; Taylor, B.C.; Fink, H.A.; Cawthon, P.M.; Stone, K.L.; Hillier, T.A.; Cauley, J.A.; Hochberg, M.C.; Rodondi, N.; et al. Comparison of 2 Frailty Indexes for Prediction of Falls, Disability, Fractures, and Death in Older Women. Arch. Intern. Med. 2008, 168, 382–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.Y.; Chao, C.T.; Huang, J.W.; Huang, K.C. Vascular Calcification as an Underrecognised Risk Factor for Frailty in 1783 Community-Dwelling Elderly Individuals. J. Am. Heart Assoc. 2020, 9, e017308. [Google Scholar] [CrossRef] [PubMed]
- Chao, C.T.; Hsu, Y.H.; Chang, P.Y.; He, Y.T.; Ueng, R.S.; Lai, C.F.; Chiang, C.K.; Huang, J.W.; Huang, S.J. Simple self-report FRAIL scale might be more closely associated with dialysis complications than other frailty screening instruments in rural chronic dialysis patients. Nephrology 2015, 20, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Coresh, J.; Greene, T.; Stevens, L.A.; Zhang, Y.L.; Hendriksen, S.; Kusek, J.W.; van Lente, F. Chronic Kidney Disease Epidemiology Collaboration. Using Standardised Serum Creatinine Values in the Modification of Diet in Renal Disease Study Equation for Estimating Glomerular Filtration Rate. Ann. Intern. Med. 2006, 145, 247–254. [Google Scholar] [CrossRef]
- Wilson, M.M.G.; Thomas, D.R.; Rubenstein, L.Z.; Chibnall, J.T.; Anderson, S.; Baxi, A.; Diebold, M.R.; Morley, J.E. Appetite assessment: Simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am. J. Clin. Nutr. 2005, 82, 1074–1081. [Google Scholar] [CrossRef]
- Lee, T.C.; Lo, L.C.; Wu, F.C. Traditional Chinese Medicine for Metabolic Syndrome via TCM Pattern Differentiation: Tongue Diagnosis for Predictor. Evid. Based Complement. Alternat. Med. 2016, 2016, 1971295. [Google Scholar] [CrossRef] [Green Version]
- Grove, B.E.; Schougaard, L.M.; Hjollund, N.H.; Ivarsen, P. Self-rated health, quality of life and appetite as predictors of initiation of dialysis and mortality in patients with chronic kidney disease stages 4–5: A prospective cohort study. BMC Res. Notes 2018, 11, 371. [Google Scholar] [CrossRef] [Green Version]
- Gama-Axelsson, T.; Lindholm, B.; Bárány, P.; Heimburger, O.; Stenvinkel, P.; Qureshi, A.R. Self-Rated Appetite as a Predictor of Mortality in Patients With Stage 5 Chronic Kidney Disease. J. Ren. Nutr. 2013, 23, 106–113. [Google Scholar] [CrossRef]
- Hengeveld, L.M.; Boer, J.M.A.; Gaudreau, P.; Heymans, M.W.; Jagger, C.; Mendonca, N.; Ocke, M.C.; Presse, N.; Sette, S.; Simonsick, E.M.; et al. Prevalence of protein intake below recommended in community-dwelling older adults: A meta-analysis across cohorts from the PROMISS consortium. J. Cachexia Sarcopenia Muscle 2020, 11, 1212–1222. [Google Scholar] [CrossRef]
- Hanisah, R.; Shahar, S.; Lee, F.S. Validation of screening tools to assess appetite among geriatric patients. J. Nutr. Health Aging 2012, 16, 660–665. [Google Scholar] [CrossRef]
- Guigoz, Y.; Vellas, B.; Garry, P.J. Assessing the Nutritional Status of the Elderly: The Mini Nutritional Assessment as Part of the Geriatric Evaluation. Nutr. Rev. 1996, 54, S59–S65. [Google Scholar] [CrossRef] [PubMed]
- Adame Perez, S.I.; Senior, P.A.; Field, C.J.; Jindal, K.; Mager, D.R. Frailty, Health-Related Quality of Life, Cognition, Depression, Vitamin D and Health-Care Utilisation in an Ambulatory Adult Population With Type 1 or Type 2 Diabetes Mellitus and Chronic Kidney Disease: A Cross-Sectional Analysis. Can. J. Diabetes 2019, 43, 90–97. [Google Scholar] [CrossRef] [PubMed]
- McMahon, E.J.; Campbell, K.L.; Bauer, J.D. Taste perception in kidney disease and relationship to dietary sodium intake. Appetite 2014, 83, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Hurley, S.W.; Johnson, A.K. The biopsychology of salt hunger and sodium deficiency. Pflug. Arch. 2015, 467, 445–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanbay, M.; Yilmaz, S.; Dincer, N.; Ortiz, A.; Sag, A.A.; Covic, A.; Sanchez-Lozada, L.G.; Lanaspa, M.A.; Cherney, D.Z.I.; Johnson, R.J.; et al. Antidiuretic Hormone and Serum Osmolarity Physiology and Related Outcomes: What Is Old, What Is New, and What Is Unknown? J. Clin. Endocrinol. Metab. 2019, 104, 5406–5420. [Google Scholar] [CrossRef]
- Guillon, G.; Grazzini, E.; Andrez, M.; Breton, C.; Trueba, M.; Serradeil-LeGal, C.; Boccara, G.; Derick, S.; Chouinard, L.; Gallo-Payet, N. Vasopressin: A potent autocrine/paracrine regulator of mammal adrenal functions. Endocr. Res. 1998, 24, 703–710. [Google Scholar] [CrossRef]
- Iwakura, H.; Bando, M.; Ueda, Y.; Akamizu, T. The effects of inflammatory cytokines on the expression of ghrelin. Endocr. J. 2017, 64, S25–S26. [Google Scholar] [CrossRef]
- Winkler, S.; Garg, A.K.; Mekayarajjananonth, T.; Bakaeen, L.G.; Khan, E. Depressed Taste and Smell in Geriatric Patients. J. Am. Dent. Assoc. 1999, 130, 1759–1765. [Google Scholar] [CrossRef]
- Arikawa, E.; Kaneko, N.; Nohara, K.; Yamaguchi, T.; Mitsuyama, M.; Sakai, T. Influence of Olfactory Function on Appetite and Nutritional Status in the Elderly Requiring Nursing Care. J. Nutr. Health Aging 2020, 24, 398–403. [Google Scholar] [CrossRef]
- Chao, C.T.; Wang, J.; Chien, K.L. COhort of GEriatric Nephrology in NTUH (COGENT) study group. Both pre-frailty and frailty increase healthcare utilization and adverse health outcomes in patients with type 2 diabetes mellitus. Cardiovasc. Diabetol. 2018, 17, 130. [Google Scholar] [CrossRef]
- Wu, P.Y.; Chao, C.T.; Chan, D.C.; Huang, J.W.; Hung, K.Y. Contributors, risk associates, and complications of frailty in patients with chronic kidney disease: A scoping review. Ther. Adv. Chronic. Dis. 2019, 10, 2040622319880382. [Google Scholar] [CrossRef] [Green Version]
- Chao, C.T.; Wang, J.; Huang, J.W.; Chan, D.C.; Chien, K.L. Frailty predicts an increased risk of end-stage renal disease with risk competition by mortality among 165,461 diabetic kidney disease patients. Aging Dis. 2019, 10, 1270–1281. [Google Scholar] [CrossRef] [Green Version]
- Li, C.M.; Chao, C.T.; Chen, S.I.; Han, D.S.; Huang, K.C. Elevated red cell distribution width is independently associated with a higher frailty risk among 2932 community-dwelling older adults. Front. Med. 2020, 7, 470. [Google Scholar] [CrossRef]
- Chao, C.T.; Wang, J.; Huang, J.W.; Chan, D.C.; Chien, K.L. COhort of GEriatric Nephrology in NTUH (COGENT) study group. Hypoglycemic episodes are associated with an increased risk of incident frailty among new onset diabetic patients. J. Diabetes Complicat. 2020, 34, 107492. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Wang, J.; Tsai, H.B.; Chao, C.T.; Chien, K.L.; Huang, J.W. Muscle relaxant use and the associated risk of incident frailty in patients wth diabetic kidney disease: A longitudinal cohort study. Ther. Adv. Drug Saf. 2021, 12, 20420986211014639. [Google Scholar] [CrossRef] [PubMed]
- Marcucci, M.; Franchi, C.; Nobili, A.; Mannuci, P.M.; Ardoino, I. REPOSI Investigators. Defining aging phenotypes and related outcomes: Clues to recognize frailty in hospitalized older patients. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 395–402. [Google Scholar]
- Sasso, F.C.; Pafundi, P.C.; Simeon, V.; De Nicola, L.; Chiodini, P.; Galiero, R.; Rinaldi, L.; Nevola, R.; Salvatore, T.; Sardu, C.; et al. NID-2 Study Group Investigators. Efficacy and durability of multifactorial intervention on mortality and MACEs: A randomized clinical trial in type-2 diabetic kidney disease. Cardiovasc. Diabetol. 2021, 20, 145. [Google Scholar] [CrossRef]
| With Impaired Appetite (n = 33) | Without Impaired Appetite (n = 45) | p-Value | |
|---|---|---|---|
| Baseline features | |||
| Age (years) | 71.8 ± 14.4 (34.1, 92.8) | 72.1 ± 9.3 (48.8, 87.9) | 0.93 |
| Male sex (%) | 19 (58) | 36 (80) | 0.03 |
| Religion | 0.28 | ||
| None (%) | 8 (24) | 6 (13) | |
| Buddhism (%) | 14 (42) | 24 (53) | |
| Taoism (%) | 8 (24) | 14 (31) | |
| Christianity (%) | 3 (9) | 1 (2) | |
| Concurrent illnesses | |||
| Coronary artery disease (%) | 3 (9) | 2 (4) | 0.41 |
| Hypertension (%) | 28 (85) | 35 (78) | 0.44 |
| Prior MI (%) | 2 (6) | 2 (4) | 0.75 |
| Heart failure (%) | 1 (3) | 1 (2) | 0.83 |
| Atrial fibrillation (%) | 2 (6) | 1 (2) | 0.39 |
| Prior cerebrovascular events (%) | 3 (9) | 8 (18) | 0.28 |
| Diabetes mellitus (%) | 19 (58) | 35 (78) | 0.71 |
| Cirrhosis (%) | 1 (3) | 0 (0) | 0.25 |
| COPD (%) | 0 (0) | 1 (2) | 0.40 |
| Malignancy (%) | 6 (18) | 4 (9) | 0.23 |
| Autoimmune diseases (%) | 2 (6) | 3 (7) | 0.92 |
| Gastric/duodenal ulcer (%) | 2 (6) | 6 (13) | 0.30 |
| Dementia (%) | 1 (3) | 0 (0) | 0.25 |
| Anthropometric parameters and physical status | |||
| Systolic BP (mmHg) | 129.7 ± 14.9 (100, 158) | 128.5 ± 16.8 (97, 174) | 0.76 |
| Diastolic BP (mmHg) | 68.9 ± 12.9 (42, 92) | 69.3 ± 13.4 (43, 116) | 0.39 |
| Heart rate (per min) | 75.7 ± 11.1 (58, 99) | 75.0 ± 9.5 (56, 95) | 0.76 |
| Weight (kg) | 66.5 ± 13.6 (41, 96) | 68.0 ± 11.0 (48, 92) | 0.60 |
| Height (cm) | 161.0 ± 9.1 (145, 178) | 164.0 ± 6.7 (149, 179) | 0.10 |
| Body mass index (kg/m2) | 25.5 ± 4.3 (18.2, 37) | 25.2 ± 3.2 (18.8, 32.6) | 0.68 |
| Waist circumference (cm) | 91.8 ± 12.7 (63, 115) | 91.2 ± 9.6 (66, 110) | 0.83 |
| Grip strength (kg) | 21.3 ± 9.4 (8.1, 45.5) | 25.6 ± 8.6 (10.7, 42.6) | 0.04 |
| Time up-and-go (s) | 4.9 ± 3.9 (1.5, 16) | 3.5 ± 2.6 (1.3, 16.6) | 0.06 |
| Timed chair stand (s) | 14.4 ± 6.2 (8.3, 34.3) | 11.8 ± 4.6 (5.4, 27.1) | 0.04 |
| Gait speed (m/s) | 0.8 ± 0.4 (0.21, 1.58) | 1.0 ± 0.4 (0.16, 1.83) | 0.11 |
| Functional status and frailty | |||
| ECOG | 0.76 ± 0.83 (0, 3) | 0.36 ± 0.65 (0, 2) | 0.02 |
| Karnofsky performance scores | 89.4 ± 13.7 (50, 100) | 95.1 ± 9.9 (60, 100) | 0.04 |
| SOF scores | 0.88 ± 0.89 (0, 3) | 0.33 ± 0.48 (0, 1) | <0.01 |
| FRAIL scores | 0.91 ± 1.18 (0, 4) | 0.44 ± 0.62 (0, 2) | 0.03 |
| Sensory function (self-rated) | |||
| Any nasal complaint (0–100) | 74.8 ± 17.9 (20, 100) | 81.8 ± 14.9 (50, 100) | 0.07 |
| Any taste complaint (0–100) | 75.6 ± 16.9 (30, 100) | 82.8 ± 14.0 (30, 100) | 0.04 |
| Any oral cavity complaint (0–100) | 67.6 ± 19.8 (20, 100) | 77.9 ± 19.2 (30, 100) | 0.02 |
| Laboratory test results | |||
| Nutrition | |||
| Albumin (g/L) | 41 ± 3 (33, 48) | 42 ± 3 (34, 49) | 0.18 |
| Fasting glucose (mmol/L) | 6.6 ± 2.0 (4.3, 12.5) | 6.5 ± 1.9 (4.1, 14.9) | 0.72 |
| Total cholesterol (mmol/L) | 4.4 ± 1.4 (2.5, 9.4) | 4.4 ± 0.8 (2.1, 6.1) | 0.99 |
| Triglyceride (mmol/L) | 1.6 ± 0.8 (0.6, 4.0) | 1.5 ± 0.8 (0.6, 4.1) | 0.81 |
| Rheologic | |||
| Leukocyte (K/μL) | 6.6 ± 2.0 (1.5, 11.7) | 6.4 ± 1.6 (3.2, 9.6) | 0.61 |
| Hemoglobin (mmol/L) | 7.1 ± 1.1 (5.1, 10.2) | 7.6 ± 1.1 (4.8, 10.1) | 0.06 |
| Platelet (K/μL) | 214.4 ± 69.8 (29, 385) | 213.9 ± 67.6 (78, 405) | 0.98 |
| Electrolyte | |||
| Sodium (meq/L) | 136.9 ± 2.9 (128, 141) | 138.4 ± 2.4 (133, 145) | 0.02 |
| Potassium (meq/L) | 4.6 ± 0.4 (3.9, 5.5) | 4.5 ± 0.5 (3.1, 5.5) | 0.53 |
| Calcium (mmol/L) | 2.3 ± 0.1 (1.9, 2.6) | 2.3 ± 0.1 (1.8, 2.6) | 0.72 |
| Phosphorus (mmol/L) | 1.2 ± 0.2 (0.9, 1.7) | 1.2 ± 0.3 (0.8, 1.8) | 0.99 |
| Renal function | |||
| Urea nitrogen (mmol/L) | 15.4 ± 6.6 (6.5, 36.4) | 13.9 ± 5.4 (5.3, 34.3) | 0.25 |
| Creatinine (μmol/L) | 300.6 ± 380.2 (88.4, 1830) | 282.9 ± 344.8 (106.1, 2299) | 0.82 |
| eGFR (mL/min/1.73 m2) | 31.7 ± 16.1 (3, 58.5) | 30.4 ± 14.5 (2, 63.1) | 0.71 |
| Variables | OR | 95% CI | p-Value |
|---|---|---|---|
| Model 1 * | |||
| Hemoglobin | 0.76 | 0.57–1.01 | 0.06 |
| SOF score | 3.42 | 1.54–7.60 | <0.01 |
| Model 2: Model 1 + Sensory function variables | |||
| Sodium (meq/L) | 0.76 | 0.60–0.97 | 0.03 |
| SOF score | 2.74 | 1.15–6.57 | 0.02 |
| Any nasal complaint | 0.96 | 0.92–0.995 | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sung, C.-C.; Liao, M.-T.; Chao, C.-T. Independent Determinants of Appetite Impairment among Patients with Stage 3 or Higher Chronic Kidney Disease: A Prospective Study. Nutrients 2021, 13, 2863. https://doi.org/10.3390/nu13082863
Sung C-C, Liao M-T, Chao C-T. Independent Determinants of Appetite Impairment among Patients with Stage 3 or Higher Chronic Kidney Disease: A Prospective Study. Nutrients. 2021; 13(8):2863. https://doi.org/10.3390/nu13082863
Chicago/Turabian StyleSung, Chih-Chien, Min-Tser Liao, and Chia-Ter Chao. 2021. "Independent Determinants of Appetite Impairment among Patients with Stage 3 or Higher Chronic Kidney Disease: A Prospective Study" Nutrients 13, no. 8: 2863. https://doi.org/10.3390/nu13082863
APA StyleSung, C.-C., Liao, M.-T., & Chao, C.-T. (2021). Independent Determinants of Appetite Impairment among Patients with Stage 3 or Higher Chronic Kidney Disease: A Prospective Study. Nutrients, 13(8), 2863. https://doi.org/10.3390/nu13082863






