Abstract
Background: Little is known regarding the role of nutrition in determining the associations between lifestyle risk factors and depression. Objectives: This study examined whether or not nutritional adequacy modulates the relationship between depression and lifestyle risk factors in Korean adults aged 18-65 years (n = 7446). Methods: Data were obtained from the 2016 and 2018 Korea National Health and Examination Survey. Depression, smoking, at-risk alcohol consumption, physical inactivity, sleep deprivation, and mean adequacy ratio (MAR) were assessed. Results: Individuals with two (OR = 1.960, p < 0.001), three (OR = 4.237, p < 0.001), or four (OR = 5.312, p < 0.001) risk factors had a significantly higher risk of depression compared to individuals with one or zero risk factor. In contrast, individuals with moderate MAR (OR = 0.607, p < 0.001) and high (OR = 0.698, p < 0.001) MAR had a lower depression risk compared to individuals with low MAR. Moderation analysis showed a moderating effect of MAR (coefficient = −0.220, p = 0.007) on the relationship between risk factors and depression. Conclusions: The current findings suggest that overall nutritional adequacy plays a modulating role in determining the relationship between depression and lifestyle risk factors in Korean adults.
1. Introduction
Depression is a common mental disorder and a leading cause of disability worldwide [1]. In South Korea, the prevalence of depression is relatively low but steadily on the rise [2]. Furthermore, among Organization for Economic Co-operation and Development countries, South Korea has the highest suicide rate at 23 deaths per 100,000 persons [3]. The estimated total economic burden of depression is rising steadily, from 4049 million USD in 2005 [4] to 1.331 billion USD in 2012 [5]. Depression in South Korea has been blamed for rising disability and surging economic burden in conjunction with the increasing rate of suicide.
There is a number of well-established risk factors associated with depression and depressive symptoms [6]. The risk factors include current or past smoking [7], heavy alcohol consumption [8], low income [9], unemployment [10], low social support [11], perceived stress [12], physical inactivity [13], sleep deprivation [14], and unhealthy diet [15]. Associations between depression and these risk factors have been reported in Korean populations [16]. Parameters of health behaviors and perceived health status are additional predictors of depression in Korean adults [17].
Nutrition is another important factor to be considered in determining the onset of depression and the severity of depressive symptoms associated with lifestyle risk factors [18]. For example, depression is associated with several nutritional parameters, including dietary intake of nutrients [19], quality of diet [20], dietary habits [21], and food security [22]. The relationship between depression and nutritional parameters has been reviewed and well summarized in previous studies [23]. Overall, the findings from previous studies suggest that nutritional adequacy, which is defined as the sufficient intake of nutrients of interest for optimal health, may play a role in the onset and maintenance of depression as well as in the severity of depressive symptoms associated with lifestyle risk factors. Therefore, examining how nutrition influences the relationship between depression and lifestyle risk factors will provide some critical information for preventive and therapeutic strategies against the mental illness.
To the best of our knowledge, no previous research has examined the potential role of nutrition in determining the relationship between depression and lifestyle risk factors in Korean adults. The current study was conducted to investigate whether or not overall nutritional adequacy moderates the association between depression and unhealthy lifestyle factors in a representative sample of Korean adults.
2. Materials and Methods
2.1. Data Source and Study Participants
As illustrated in Figure 1, we initially selected respondents aged 18–65 years (n = 9609) from the seventh Korea National Health and Examination Survey (KNHANES) in 2016 and 2018, a nationwide survey designed to assess health and nutritional status in the Korean population. Exclusion criteria were missing information or refusal to provide information on depression scores (n = 1178), missing information or refusal to provide information on lifestyle risk factors (n = 1285), and missing information or refusal to provide information on other variables (n = 84). Consequently, the remaining 7446 participants (women, n = 4393; 59%) were included in final data analyses. A detailed description of the KNHANES study design is available elsewhere [24]. The Institutional Review Board of Korea Centers for Disease Control and Prevention reviewed and approved the KNHANES VII surveys (2018-01-03-P-A) in accordance with the Declaration of Helsinki. Informed consent was obtained from all the participants.

Figure 1.
Flow chart of selection for study participants.
2.2. Variables
2.2.1. Patient Health Questionnaire-9
The Korean version of the Patient Health Questionnaire (PHQ)-9, which is a self-reported version of the PRIME-MD diagnostic instrument for major depressive disorders [25], was downloaded from the PHQ website (https://www.phqscreeners.com/, accessed on 10 January 2021) and used to score each of the nine items corresponding to the Diagnostic and Statistical Manual of Mental Disorders criteria as “0” (not at all) to “3” (nearly every day). The threshold for identifying major depressive disorders was 5, and its validity was previously tested and reported [26].
2.2.2. Lifestyle Risk Factors
Lifestyle risk factors included in the study were past/current smoking, at-risk alcohol consumption, physical inactivity, and sleep deprivation. For smoking, respondents were dichotomously classified as never smokers and past or current smokers. At-risk alcohol intake was defined as having seven glasses or more (five or more for women) of alcohol per occasion two or more times per week [27]. Physical inactivity was defined as not participating in at least 150 min of moderate physical activity (PA) per week or 75 min of vigorous PA or a combination of moderate and vigorous PA (https://www.who.int/news-room/fact-sheets/detail/physical-activity, accessed on 20 March 2021). Sleep deprivation was defined as inadequate duration of sleep (<7 h) or use of hypnotic medications [28].
2.2.3. Dietary Data
Dietary intake of macronutrients (i.e., carbohydrates, fats, and proteins) and micronutrients (i.e., vitamins A and C, thiamine, riboflavin, niacin, phosphorous, calcium, and iron) was assessed with a 24-h (h) recall method. Trained interviewers conducted computer-assisted personal interviews to assess all food items ingested during the previous 24 h. Mean adequacy ratio (MAR), which is a measure that is used to evaluate an individual’s intake of a nutrients and represents a population’s overall nutritional adequacy, was calculated using the following equation: MAR = (sum of nutrient adequacy ratio (NAR)/number of nutrients) × 100. Nutrient adequacy ratio (NAR) represents an individual’s intake of a nutrient as a percentage of the age- and sex-specific recommended dietary allowance (RDA) for that nutrient [29]. Mean adequacy ratio (MAR) and quantifies the overall nutritional adequacy of a population based on the current recommended allowance of a group of nutrients of interest.
2.2.4. Covariates
Age (continuous), sex (categorical: male or female), body mass index (quantitative), education (categorical: elementary school or lower, middle or high school, university or higher), income (quantitative), and marital status (categorical: yes or no) were included as covariates. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2).
2.3. Statistics
Normality of data distribution was confirmed with QQ plotting, and the absence of multi-collinearity was assessed by variance of inflation factor (VIF). Descriptive statistics were performed with Student’s t-test and Chi-square test for continuous and categorical variables, respectively, which are presented as the mean ± standard deviation (SD) and number (n) or percentage (%), respectively. Linear regression was used to assess the relationship between PHQ-9 scores and other variables. Multivariate logistic regression was performed to estimate the odds ratios (ORs) and 95% confidence intervals (CIs) of depression by number of lifestyle risk factors and MAR level (from low to high) before and after adjustments for the covariates. To find out whether or not the strength of the relationship between lifestyle risk factors and depression risk varies according to overall nutritional adequacy, a moderation analysis with the interaction term between the risk factors and MAR (moderator) was performed with the Hayes PROCESS macro. The significance of the moderator was tested by the change of proportion concerning the explained variance (∆R2). Statistical significance was defined as p < 0.05. All statistical analyses were conducted using PASW SPSS WIN 27.0 (SPSS Inc., Chicago, IL, USA).
3. Results
Table 1 describes the characteristics of study participants by sex. Men had higher BMI, better education levels, and lower rates of marriage in comparison to women, with no differences in mean age and household income. With respect to lifestyle risk factors, men had higher rates of smoking, at-risk alcohol consumption, and sleep deprivation in conjunction with a lower rate of physical inactivity in comparison to women. In addition, men had higher intakes of carbohydrates, proteins, vitamin A, thiamine, riboflavin, niacin, phosphorous, calcium, and iron in conjunction with higher caloric intake in comparison to women. Finally, men had a lower mean PHQ-9 score in comparison to women.

Table 1.
Characteristics of study participants.
Table 2 presents the outcomes of linear regression analysis for PQH-9 scores. Depression risk was positively associated with age, female, unmarried, smoking, at-risk alcohol consumption, physical inactivity, and sleep deprivation, while it was negatively associated with education level, income, and MAR.

Table 2.
Linear regression analysis for the determinants of depression in study participants.
Table 3 presents the outcomes of logistic regression for depression risk by lifestyle risk factors and MAR, respectively. Individuals with two (OR = 1.65, 95% CI = 1.24~2.20, p < 0.001), three (OR = 2.97, 95% CI = 2.21~3.98, p < 0.001), and four lifestyle risk factors (OR = 3.19, 95% CI = 2.09~4.868, p < 0.001) had higher risks of depression in comparison to individuals with one or zero risk factors (OR = 1). Increased ORs for the two-risk factors (p < 0.001), the three-risk factors (p < 0.001), and the four-risk factors (p < 0.001) remained statistically significant even after adjustments for age, sex, income, education, marital status, and MAR. On the other hand, individuals with middle 50 percentile MAR (OR = 0.45, 95% CI = 0.36~0.58, p < 0.001) or highest 25 percentile MAR (OR = 0.46, 95% CI = 0.34~0.62, p < 0.001) had significantly lower risks of depression in comparison to individuals with lowest 25 percentile MAR (OR = 1). Decreased ORs for the middle 50 percentile MAR and highest 25 percentile MAR remained statistically significant even after adjustments for age, sex, income, education, marital status, and lifestyle risk factors (i.e., smoking, at-risk alcohol consumption, physical inactivity, and sleep deprivation).

Table 3.
Odds ratios (ORs) and 95% confidence intervals (CIs) of depression by lifestyle risk factors and nutritional adequacy ratio.
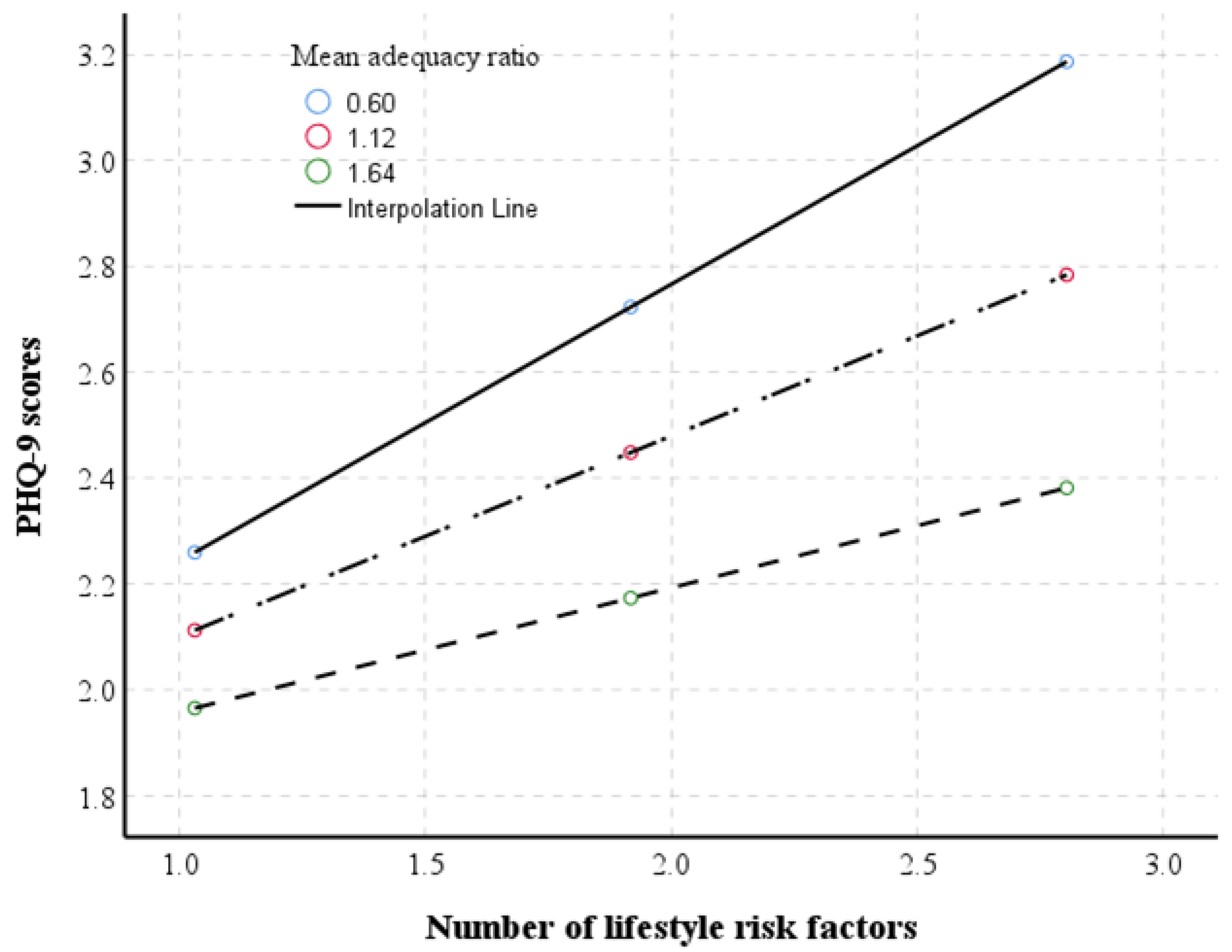
Table 4 presents the outcomes of a moderating analysis of MAR for the relationships between depression and lifestyle risk factors. There was a significant interaction between lifestlye risk factors and nutrition (coefficient = −0.259, 95% CI = −0.423~−0.094, p = 0.002) on MAR, observed by increasing a part of the explained variability up to 2% (∆R2 = 0.018). The moderating effect of MAR remained significant (coefficient = −0.220, 95% CI = −0.380~−0.061, p = 0.007) even after adjustments for the covariates, observed by further increasing a part of the explained variability up to 8% (∆R2 = 0.001). As illustrated in Figure 2, overall nutritional adequacy attenuates the strength of the relationship between PHQ-9 score and lifestyle risk factors—the higher was the MAR, the less steep was the slope of the relationship.

Table 4.
Moderation analyses of mean adequacy ratio for the relationship of depression with lifestyle risk factors.

Figure 2.
Illustration of the moderating effect of mean adequacy ratio on the relationship between lifestyle risk factors and patient health questionnaire (PHQ)-9 scores.
4. Discussion
This study examines whether or not overall nutritional adequacy modulates the relationships of depression with lifestyle risk factors (i.e., past/current smoking, at-risk alcohol consumption, physical inactivity, and sleep deprivation) in 7446 Korean adults who participated in the 2016 and 2018 KNHANES. The findings of the current study show that depression risk is positively associated with all the four risk factors and negatively associated with overall nutritional adequacy. Novel to our study is that overall nutritional adequacy attenuates the adverse effect of lifestyle risk factors on depression in Korean adults.
Consistent with the current findings, previous studies have reported a significant association between depression and lifestyle factors in Western populations [30,31,32]. The associations between lifestyle risk factors and depression are also observed in Korean populations. In a representative sample of 4093 Korean adults who participated in the 2014 KNHANES, Jung et al. [33] showed that both hypertension and dyslipidemia were independent determinants of depression in women, and that dyslipidemia alone was an independent determinant of depression in men. Kim and Kim [34] showed that depression risk was significantly associated with metabolic syndrome risk factors in Korean adults by analyzing data (n = 10,459) from the 2014 and 2016 KNHANES. By analyzing data from the 2012 Korean Community Health Survey in adults aged 19 years and older (n = 10,081), Won et al. [35] showed that depression was significantly associated with subjective health, drinking of alcohol, smoking, hypertension, diabetes mellitus, total hours of sleep, activity impairments, and stress in Korean adults. Taken together, these previous findings support the current findings in which lifestyle risk factors are significantly associated with increased risk of depression.
In particular, the current findings suggest the potential role of dietary intake of nutrients in determining the relationship between lifestyle risk factors and depression. By conducting a community-based study involving three age-based Australian groups, for example, Jacka et al. [36] showed that unhealthy dietary patterns were significantly and independently associated with increased depressive symptoms, especially in the oldest cohort. In the Japan Multi-Institutional Collaborative Cohort Study involving 4701 Japanese adults aged 35–69 years, Choda et al. [37] showed that depression risk was inversely associated with dietary intake of vegetables, protein, calcium (Ca), vitamin D, carotene, and n-3 high-polyunsaturated fatty acids and positively associated with monounsaturated fatty acids. In a cohort study of 13,983 Spanish university graduates, Sánchez-Villegas et al. [38] found that inadequate intake of ≥four micronutrients out of a collection of vitamins, including vitamins B1, B2, B3, B6, B12, C, A, D, E, folic acid (FA), zinc (Zn), iodine (I), selenium (Se), iron (Fe), Ca, potassium (K), phosphorus (P), magnesium (Mg), and chrome (Cr), was associated with increased risk of depression. By comparing depressive patients with their healthy counterparts, Kaner et al. [39] found that depression was significantly associated with lower intakes of micronutrients, such as vitamin A, thiamine, riboflavin, vitamin B6, folate, vitamin C, Na, K, Mg, Ca, P, Fe, Zn, and fiber. Consequently, the findings from the current and previous studies suggest that the sufficient intake of those essential nutrients may function to minimize the adverse effects of lifestyle risk factors on depression. In addition, the current findings also suggest that dietary interventions may be a promising intervention for reducing depression and/or depressive symptoms associated with lifestyle risk factors.
Protective effects of healthy dietary intake and habits against depression risk are also observed in Korean populations. For example, Park et al. [40] reported that low dietary intake of fiber and vitamin C was significantly associated with depression risk in Korean women by analyzing data from the 2014 KNHANES (n = 5897). By analyzing data from the sixth (2014) and seventh (2016, 2018) KNHANES (n = 19,106), Yun et al. [41] found that adverse dietary intake (i.e., dietary intake of sugar, carbohydrates, sodium, and others) and habits (i.e., dining out and dining frequency) were significantly associated with depression risk in Korean adults, with age- and sex-based differences in the strength of the association. By analyzing data (n = 5103) from the 2018 KNHANES, Lee and Kim [42] showed that dietary intake of phosphorus, potassium, and vitamin A was inversely associated with depression risk in men, while dietary intake of phosphorus was inversely associated with depression risk in women. That study also found that eating behaviors, such as skipping lunch, frequency of daily meals, and frequency of weekly lunches out, were significantly associated with a higher prevalence of depression in Korean women only. Protective effects of dietary intake against depression were observed for various micronutrients such as riboflavin, thiamin, vitamin C, polyunsaturated fatty acids, fibers, fruits, and vegetables in Korean populations [43,44]. Taken together, findings from the current and previous studies suggest that unhealthy dietary intake and habits are significantly associated with the onset of depression and the severity of depressive symptoms in Korean adults.
Some explanations can be given to the modulating effects of overall nutritional adequacy on the relationship between the four lifestyle risk factors and depression. First, overall nutritional adequacy may have protective effects against depression by securing sufficient dietary intake of anti-depressant and anti-oxidant nutrients [45]. Second, overall nutritional adequacy may reflect the sufficient intake of other essential nutrients needed to fulfill nutritional requirements for good mental health [46]. Third, it is also possible that overall nutritional adequacy has an indirectly protective effect against depression by minimizing clinical consequences of unhealthy behaviors such as obesity and metabolic diseases [47].
This study has some limitations. First, the cross-sectional nature of the study does not allow any cause-and-effect explanation regarding the modulating effect of overall nutritional adequacy on the relationship between depression and lifestyle risk factors. Second, a bidirectional relationship between depression and lifestyle risk factors seems possible-depression can lead to an increase in lifestyle risk factors, or vice versa, and this remains to be further addressed. Third, it is possible that the modulating effect of overall nutritional adequacy on the relationship between lifestyle risk factors and depression differ by some confounders such as age and sex. This should be addressed by including demographics as additional modulators. Fourth, the PHQ-9 used in the current study is a self-reported diagnosis of depression. Therefore, the possibility of type 2 errors or false negatives cannot be completely ruled out. Lastly, we did not consider other potential risk factors involved in depression, including brain neurotransmitters, genetic vulnerability, medications, substance misuse, and others. Caution is necessary in interpreting the relationship of depression with nutritional adequacy and lifestyle risk factors observed in the current study.
Despite limitations, this study also has strengths. First, it is a population-based study with a relatively high response rate and large sample size. “Second, to the best of our knowledge, we are the first to report the potential of overall nutritional adequacy as a modulator in determining the relationship between lifestyle risk factors and depression. At the same time, we also recognize that the interaction between lifestyle risk factors and overall nutritional adequacy on depression cannot be explained in a cause-and-effect manner due to the cross-sectional nature of this study. Consequently, a randomized controlled trial is warranted to investigate the protective role of healthy dietary intake and habits against the adverse effects of lifestyle risk factors on the onset of depression and/or the severity of depressive symptoms. Third, the relationship between lifestyle risk factors and depression may imply adverse effects secondary to the risk factors such as metabolic complications.
5. Conclusions
This population-based study finds that overall nutritional adequacy can attenuate the adverse effect of lifestyle risk factors on depression in Korean adults, implying the importance of nutrition as a therapeutic strategy against the mental illness.
Author Contributions
M.K. and H.K. contributed to conception and design, data analyses, data interpretation, and writing of the manuscript. M.J. and H.H. contributed to statistical analyses, data interpretation, and preparation of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a National Research Foundation grant funded by the Korean government (NRF-2020R1A2C1009365).
Institutional Review Board Statement
The Sungkunwan University’s institutional review board of human studies reviewed and approved the study protocol (SKKU 2017-06-009). Written informed consent was obtained from all participants. All methods were performed in accordance with the relevant guidelines and regulations (Declaration of Helsinki).
Informed Consent Statement
All participants provided written informed consent.
Data Availability Statement
Data can be accessible upon request to corresponding author (hkang@skku.edu).
Conflicts of Interest
All the authors declare that they have no conflicts of interest.
References
- World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice (Summary Report); World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Kim, G.; Jo, M.; Shin, Y. Increased prevalence of depression in South Korea from 2002 to 2013. Sci. Rep. 2020, 10, 16979. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.M.; Hong, J.P.; Cho, M.J. Economic burden of depression in South Korea. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Park, J.; Lee, S.; Oh, I.; Choi, J.; Oh, C. Changing trends in suicide rates in South Korea from 1993 to 2016: A descriptive study. BMJ Open 2018, 8, e023144. [Google Scholar] [CrossRef] [Green Version]
- Shin, D.; Kim, N.; Kim, M.; Rhee, S.; Park, S.H.; Kim, H.; Yang, B.; Kim, M.; Choi, G.; Koh, M.; et al. Cost analysis of depression using the national insurance system in South Korea: A comparison of depression and treatment-resistant depression. BMC Health Serv. Res. 2020, 20, 286. [Google Scholar] [CrossRef] [Green Version]
- Schaakxs, R.; Comijs, H.C.; van der Mast, R.C.; Schoevers, R.A.; Beekman, A.T.F.; Penninx, B.W.J.H. Risk factors for depression: Differential across age? Am. J. Geriatr. Psychiatry 2017, 25, 966–977. [Google Scholar] [CrossRef]
- He, Q.; Yang, L.; Shi, S.; Gao, J.; Tao, M.; Zhang, K.; Gao, C.; Yang, L.; Li, K.; Shi, J.; et al. Smoking and major depressive disorder in Chinese women. PLoS ONE 2014, 9, e106287. [Google Scholar] [CrossRef]
- Manninen, A.; Poikolainen, K.; Vartiainen, E.; Laatikainen, T. Heavy drinking occasions and depression. Alcohol Alcohol. 2006, 41, 293–299. [Google Scholar] [CrossRef] [Green Version]
- Salkever, D.S.; Gibbons, B.; Drake, R.E.; Frey, W.D.; Hale, T.W.; Karakus, M. Increasing earnings of social security disability income beneficiaries with serious mental disorder. J. Ment. Health Policy Econ. 2014, 17, 75–90. [Google Scholar]
- Pompili, M.; Innamorati, M.; Di Vittorio, C.; Baratta, S.; Masotti, V.; Badaracco, A.; Wong, P.; Lester, D.; Yip, P.; Girardi, P.; et al. Unemployment as a risk factor for completed suicide: A psychological autopsy study. Arch. Suicide Res. 2014, 18, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cai, L.; Qian, J.; Peng, J. Social support moderates stress effects on depression. Int. J. Ment. Health Syst. 2014, 8, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapero, B.G.; Black, S.K.; Liu, R.T.; Klugman, J.; Bender, R.E.; Abramson, L.Y.; Alloy, L.B. Stressful life events and depression symptoms: The effect of childhood emotional abuse on stress reactivity. J. Clin. Psychol. 2014, 70, 209–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, X.; D’Arcy, C. The projected effect of increasing physical activity on reducing the prevalence of common mental disorders among Canadian men and women: A national population-based community study. Prev. Med. 2013, 56, 59–63. [Google Scholar] [CrossRef]
- Nutt, D.; Wilson, S.; Paterson, L. Sleep disorders as core symptoms of depression. Dialogues Clin. Neurosci. 2008, 10, 329–336. [Google Scholar] [CrossRef]
- Khosravi, M.; Sotoudeh, G.; Majdzadeh, R.; Nejati, S.; Darabi, S.; Raisi, F.; Esmaillzadeh, A.; Sorayani, M. Healthy and unhealthy dietary patterns are related to depression: A case-control study. Psychiatry Investig. 2015, 12, 434–442. [Google Scholar] [CrossRef] [Green Version]
- Cho, Y.; Lee, J.K.; Kim, D.H.; Park, J.H.; Choi, M.; Kim, H.J.; Nam, M.J.; Lee, K.U.; Han, K.; Park, Y.G. Factors associated with quality of life in patients with depression: A nationwide population-based study. PLoS ONE 2019, 14, e0219455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, B.N.; Lee, H.J.; Joo, J.H.; Park, E.C.; Jang, S.I. Association between health behaviours and depression: Findings from a national cross-sectional study in South Korea. BMC Psychiatry 2020, 20, 238. [Google Scholar] [CrossRef] [PubMed]
- Lang, U.E.; Beglinger, C.; Schweinfurth, N.; Walter, M.; Borgwardt, S. Nutritional aspects of depression. Cell Physiol. Biochem. 2015, 37, 1029–1043. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lv, M.R.; Wei, Y.J.; Sun, L.; Zhang, J.X.; Zhang, H.G.; Li, B. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017, 253, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, M.; Molero, P.; Ortuño Sánchez-Pedreño, F.; Van der Does, W.; Angel Martínez-González, M. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 2018, 226, 346–354. [Google Scholar] [CrossRef] [Green Version]
- Yun, H.; Kim, D.W.; Lee, E.J.; Jung, J.; Yoo, S. Analysis of the effects of nutrient intake and dietary habits on depression in Korean adults. Nutrients 2021, 13, 1360. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Lee, K.W.; Cho, M.S. Association of food insecurity with nutrient intake and depression among Korean and US adults: Data from the 2014 Korea and the 2013–2014 US National Health and Nutrition Examination Surveys. Int. J. Environ. Res. Public Health 2021, 18, 506. [Google Scholar] [CrossRef] [PubMed]
- Lassale, C.; Batty, G.D.; Baghdadli, A.; Jacka, F.; Sánchez-Villegas, A.; Kivimäki, M.; Akbaraly, T. Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 965–986. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korean Ministry of Health and Welfare, Korea Center for Disease Control and Prevention. Korea Health Statistics 2018: Korea National Health and Nutrition Examination Survey (KNHANES VII). Available online: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do (accessed on 20 May 2021).
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Jo, S.A.; Kwak, J.H.; Pae, C.U.; Steffens, D.; Jo, I.; Park, M.H. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: The Ansan Geriatric study. Compr. Psychiatry 2008, 49, 218–223. [Google Scholar] [CrossRef]
- Shin, C.; Kim, Y.; Park, S.; Yoon, S.; Ko, Y.H.; Kim, Y.K.; Kim, S.H.; Jeon, S.W.; Han, C. Prevalence and associated factors of depression in general population of Korea: Results from the Korea National Health and Nutrition Examination Survey, 2014. J. Korean Med. Sci. 2017, 32, 1861–1869. [Google Scholar] [CrossRef]
- Shin, Y.-C.; Kim, J.-W.; Seol, J.-M.; Oh, K.-S.; Shin, D.-W.; Kim, E.-J.; Lim, S.-W. Long and short sleep duration are both associated with suicidal ideation in Korean employees. Sleep Biol. Rhythm. 2017, 15, 81–86. [Google Scholar] [CrossRef]
- INDDEX Project. Data4Diets. Building Blocks for Diet. Related Food Security Analysis; Tufts University: Boston, MA, USA, 2018; Available online: https://inddex.nutrition.tufts.edu/data4diets (accessed on 24 May 2021).
- Sarris, J.; Thomson, R.; Hargraves, F.; Eaton, M.; de Manincor, M.; Veronese, N.; Solmi, M.; Stubbs, B.; Yung, A.R.; Firth, J. Multiple lifestyle factors and depressed mood: A cross-sectional and longitudinal analysis of the UK Biobank (n = 84,860). BMC Med. 2020, 18, 354. [Google Scholar] [CrossRef]
- Atzendorf, J.; Apfelbacher, C.; Gomes de Matos, E.; Kraus, L.; Piontek, D. Patterns of multiple lifestyle risk factors and their link to mental health in the German adult population: A cross-sectional study. BMJ Open 2018, 8, e022184. [Google Scholar] [CrossRef] [Green Version]
- Bruin, M.C.; Comijs, H.C.; Kok, R.M.; Van der Mast, R.C.; Van den Berg, J.F. Lifestyle factors and the course of depression in older adults: A NESDO study. Int. J. Geriatr Psychiatry. 2018, 33, 1000–1008. [Google Scholar] [CrossRef] [Green Version]
- Jung, Y.; Shin, H.; Kim, Y.; Shin, H.; Linton, J. The association of depression and cardiovascular risk factors in Korean adults: The Sixth Korea National Health and Nutrition Examination Survey, 2014. Korean J. Fam. Pract. 2017, 7, 308–314. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, H.Y. Association between depression and metabolic syndrome in Korean adults: Data from the 2014 and 2016 Korea National Health and Nutrition Examination Survey. Asia Pac. J. Public Health 2019, 31, 18–29. [Google Scholar] [CrossRef]
- Won, M.R.; Ahn, M.S.; Choi, Y.J. Factors associated with perceived depression of Korean adults: Secondary data from the Korean community health survey. Commun. Ment. Health J. 2017, 53, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Jacka, F.N.; Cherbuin, N.; Anstey, K.J.; Butterworth, P. Dietary patterns and depressive symptoms over time: Examining the relationship between socioeconomic position, health behaviours and cardiovascular risk. PLoS ONE 2014, 9, e87657. [Google Scholar] [CrossRef] [PubMed]
- Choda, N.; Wakai, K.; Naito, M.; Imaeda, N.; Goto, C.; Maruyama, K.; Kadomatsu, Y.; Tsukamoto, M.; Sasakabe, T.; Kubo, Y.; et al. Associations between diet and mental health using the 12-item General Health Questionnaire: Cross-sectional and prospective analyses from the Japan Multi-Institutional Collaborative Cohort Study. Nutr. J. 2020, 19, 2. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Villegas, A.; Pérez-Cornago, A.; Zazpe, I.; Santiago, S.; Lahortiga, F.; Martínez-González, M.A. Micronutrient intake adequacy and depression risk in the SUN cohort study. Eur. J. Nutr. 2018, 57, 2409–2419. [Google Scholar] [CrossRef] [PubMed]
- Kaner, G.; Soylu, M.; Yüksel, N.; Inanç, N.; Ongan, D.; Başmısırlı, E. Evaluation of nutritional status of patients with depression. Biomed. Res. Int. 2015, 2015, 521481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.; Han, A.; Shin, S.; Eo, J. Relationship between dietary intake and depression among Korean adults: Korea National Health and Nutrition Examination Survey 2014. Korean J. Fam. Pract. 2019, 9, 139–146. [Google Scholar] [CrossRef]
- Lee, E.; Kim, J.M. Association between depression and eating behavior factors in Korean adults: The Korea National Health and Nutrition Examination Survey 2018. J. Nutr. Health 2021, 54, 152–164. [Google Scholar] [CrossRef]
- Park, S.J.; Choi, J.H.; Lee, J.Y.; Lee, C.; Lee, H.J. Association between nutrient intakes and prevalence of depressive disorder in Korean adults: 2014 Korean National Health and Nutrition Examination Survey. J. Nutr. Health 2018, 51, 414–422. [Google Scholar] [CrossRef]
- Choi, E.; Ha, K.; Shin, J.; Ham, D.; Joung, H. Association of dietary intake of polyunsaturated fatty acids with depression in Korean adults (P14-009-19). Curr. Dev. Nutr. 2019, 3. [Google Scholar] [CrossRef] [Green Version]
- Ju, S.-Y.; Park, Y.K. Low fruit and vegetable intake is associated with depression among Korean adults in data from the 2014 Korea National Health and Nutrition Examination Survey. J. Health Popul. Nutr. 2019, 38, 39. [Google Scholar] [CrossRef] [PubMed]
- Ljungberg, T.; Bondza, E.; Lethin, C. Evidence of the importance of dietary habits regarding depressive symptoms and depression. Int. J. Environ. Res. Public Health 2020, 17, 1616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verger, E.O.; Le Port, A.; Borderon, A.; Bourbon, G.; Moursi, M.; Savy, M.; Mariotti, F.; Martin-Prevel, Y. Dietary diversity indicators and their associations with dietary adequacy and health outcomes: A systematic scoping review. Adv. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ko, G.T.; Chan, J.C.; Tong, S.D.; Chan, A.W.; Wong, P.T.; Hui, S.S.; Kwok, R.; Chan, C.L. Associations between dietary habits and risk factors for cardiovascular diseases in a Hong Kong Chinese working population—The “Better Health for Better Hong Kong” (BHBHK) health promotion campaign. Asia Pac. J. Clin. Nutr. 2007, 16, 757–765. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).