Infant and Young Child Feeding Practices among Adolescent Mothers and Associated Factors in India
Abstract
:1. Introduction
2. Methods
2.1. Data Sources and Study Design
2.2. Outcome and Confounding Factors
- Exclusive breastfeeding under 6 months: the proportion of infants 0–5 months of age who received breast milk during the previous day;
- Predominant breastfeeding under 6 months: the proportion of infants 0–5 months of age who received breast milk as the predominant source of nourishment during the previous day;
- Early initiation of breastfeeding: the proportion of children born in the last 24 months who started breastfeeding within one hour of birth;
- Bottle feeding: the proportion of Children 0–23 months of age who were fed with a bottle during the previous day;
- Introduction to solid, semisolid or soft foods: the proportion of infants 6–8 months of age who received solid, semisolid or soft foods during the previous day;
- Minimum dietary diversity: the proportion of Children 6–23 months of age who received foods from ≥4 food groups during the previous day. The seven food groups considered were (1) grains, roots, and tubers; (2) legumes and nuts; (3) dairy products (milk, yogurt, and cheese); (4) flesh foods (meat, fish, and poultry); (5) eggs; (6) vitamin A-rich fruits and vegetables; and (7) other fruits and vegetables;
- Minimum meal frequency: the proportion of breastfed children 6–23 months of age who received solid, semisolid, or soft foods the minimum number of times or more during the previous day, and the proportion of non-breastfed children 6–23 months of age who received solid, semisolid, or soft foods or milk feeds the minimum number of times or more during the previous day;
- Minimum acceptable diet: the proportion of breastfed children 6–23 months of age who had at least the minimum dietary diversity and the minimum meal frequency during the previous day and the proportion of non-breastfed children 6–23 months of age who received at least two milk feedings and had at least the minimum dietary diversity, not including milk feeds and the minimum meal frequency during the previous day.
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
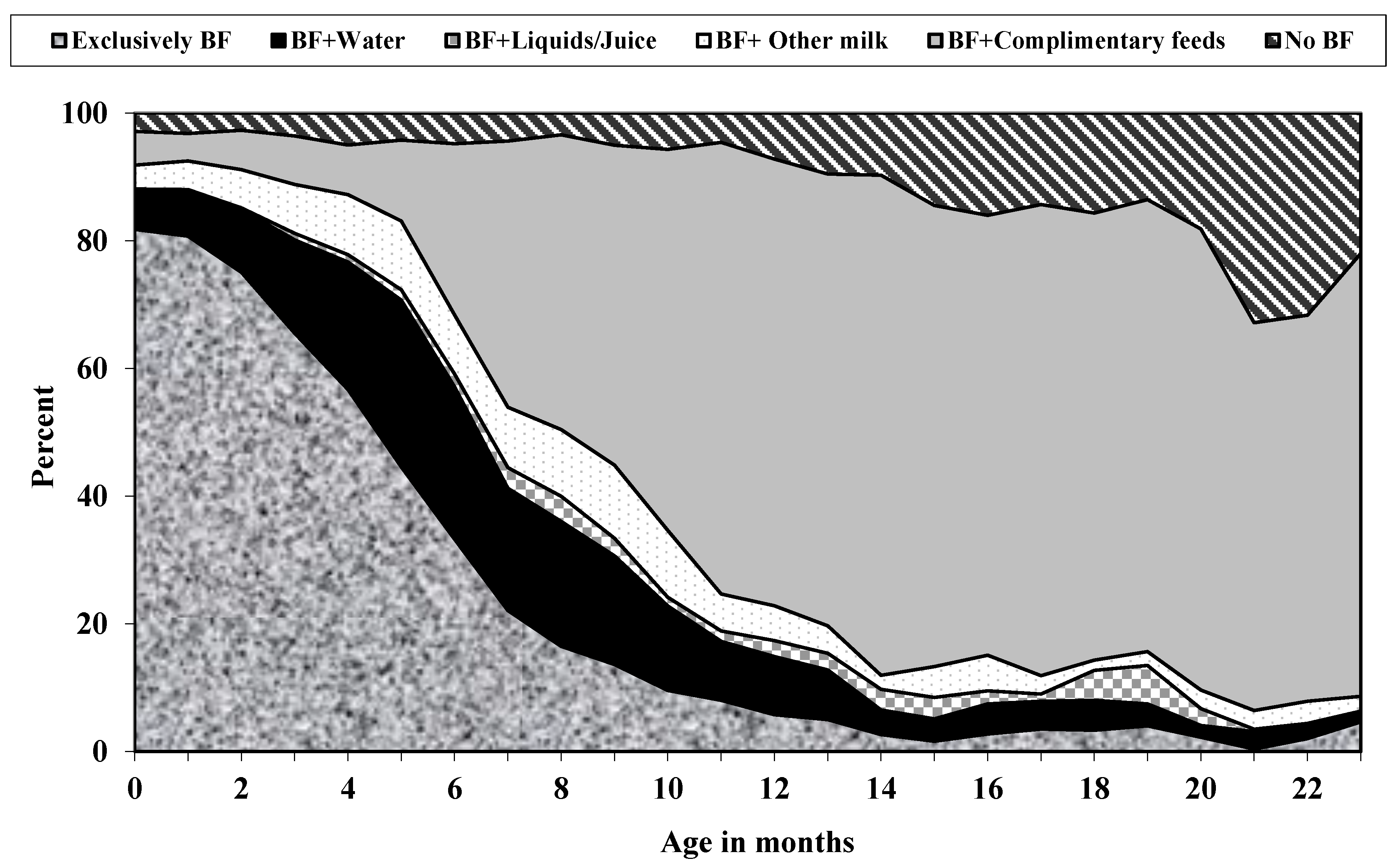
3.2. Breastfeeding and Infant Feeding Indicators
3.3. Factors Associated with Breastfeeding Indicators
3.4. Early Initiation of Breastfeeding
3.5. Exclusive Breastfeeding
3.6. Bottle-Feeding
3.7. Predominant Breastfeeding
3.8. Factors Associated with Complementary Feeding Indicators
3.9. Introduction to Solid, Semisolid, or Soft Foods
3.10. Minimum Dietary Diversity
3.11. Minimum Acceptable Diet
4. Discussion
4.1. Breastfeeding Indicators
4.2. Complementary Feeding Indicators
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- The United Nations Children’s Fund (UNICEF). Programming Guide Infant and Young Child Feeding; UNICEF, Infant and Young Child Feeding Unit NS, Programmes: New York, NY, USA, 2011. [Google Scholar]
- World Health Organization. Global Strategy for Infant and Young Child Feeding; World Health Organization UNICEF: Geneva, Switzerland, 2003. [Google Scholar]
- World Health Organisation. Children: Reducing Mortality: WHO. Available online: http://www.who.int/mediacentre/factsheets/fs178/en/ (accessed on 31 March 2021).
- Jones, G.; Steketee, R.W.; Black, R.E.; Bhutta, Z.A.; Morris, S.S. How many child deaths can we prevent this year? Lancet 2003, 362, 65–71. [Google Scholar] [CrossRef]
- Senarath, U.; Dibley, M.; Agho, K. Breastfeeding practices and associated factors among children under 24 months of age in Timor-Leste. Eur. J. Clin. Nutr. 2007, 61, 387–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogbo, F.A.; Agho, K.E.; Page, A. Determinants of suboptimal breastfeeding practices in Nigeria: Evidence from the 2008 demographic and health survey. BMC Public Health 2015, 15, 259. [Google Scholar] [CrossRef] [Green Version]
- Shifraw, T.; Worku, A.; Berhane, Y. Factors associated exclusive breastfeeding practices of urban women in Addis Ababa public health centers, Ethiopia: A cross sectional study. Int. Breastfeed. J. 2015, 10, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agho, K.E.; Dibley, M.J.; Odiase, J.I.; Ogbonmwan, S.M. Determinants of exclusive breastfeeding in Nigeria. BMC Pregnancy Childbirth 2011, 11, 2. [Google Scholar] [CrossRef] [Green Version]
- Aidam, B.A.; Perez-Escamilla, R.; Lartey, A.; Aidam, J. Factors associated with exclusive breastfeeding in Accra, Ghana. Eur. J. Clin. Nutr. 2005, 59, 789–796. [Google Scholar] [CrossRef] [Green Version]
- Veeranki, S.P.; Nishimura, H.; Krupp, K.; Gowda, S.; Arun, A.; Madhivanan, P. Suboptimal breastfeeding practices among women in rural and low-resource settings: A study of women in rural Mysore, India. Ann. Glob. Health 2017, 83, 577–583. [Google Scholar] [CrossRef]
- Amin, T.; Hablas, H.; Al Qader, A.A. Determinants of initiation and exclusivity of breastfeeding in Al Hassa, Saudi Arabia. Breastfeed. Med. 2011, 6, 59–68. [Google Scholar] [CrossRef]
- Hromi-Fiedler, A.J.; Pérez-Escamilla, R. Unintended pregnancies are associated with less likelihood of prolonged breast-feeding: An analysis of 18 Demographic and Health Surveys. Public Health Nutr. 2006, 9, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Finlay, J.E.; Özaltin, E.; Canning, D. The association of maternal age with infant mortality, child anthropometric failure, diarrhoea and anaemia for first births: Evidence from 55 low-and middle-income countries. BMJ Open 2011, 1, e000226. [Google Scholar] [CrossRef]
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C.; et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef] [Green Version]
- Azzopardi, P.S.; Hearps, S.J.; Francis, K.L.; Kennedy, E.C.; Mokdad, A.H.; Kassebaum, N.J.; Lim, S.; Irvine, C.M.; Vos, T.; Brown, A.D.; et al. Progress in adolescent health and wellbeing: Tracking 12 headline indicators for 195 countries and territories, 1990–2016. Lancet 2019, 393, 1101–1118. [Google Scholar] [CrossRef] [Green Version]
- Sipsma, H.L.; Magriples, U.; Divney, A.; Gordon, D.; Gabzdyl, E.; Kershaw, T. Breastfeeding behavior among adolescents: Initiation, duration, and exclusivity. J. Adolesc. Health 2013, 53, 394–400. [Google Scholar] [CrossRef] [Green Version]
- Senarath, U.; Dibley, M.J. Complementary feeding practices in South Asia: Analyses of recent national survey data by the South Asia Infant Feeding Research Network. Matern. Child Nutr. 2012, 8, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Inayati, D.A.; Scherbaum, V.; Purwestri, R.C.; Hormann, E.; Wirawan, N.N.; Suryantan, J.; Hartono, S.; Bloem, M.A.; Pangaribuan, R.V.; Biesalski, H.K.; et al. Infant feeding practices among mildly wasted children: A retrospective study on Nias Island, Indonesia. Int. Breastfeed. J. 2012, 7, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, D.; Goel, N.; Mittal, P.C.; Misra, P. Influence of infant-feeding practices on nutritional status of under-five children. Indian J. Pediatrics 2006, 73, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Rytter, M.J.H.; Kolte, L.; Briend, A.; Friis, H.; Christensen, V.B. The immune system in children with malnutrition—A systematic review. PLoS ONE. 2014, 9, e105017. [Google Scholar] [CrossRef] [Green Version]
- Hackett, K.M.; Mukta, U.S.; Jalal, C.S.; Sellen, D.W. Knowledge, attitudes and perceptions on infant and young child nutrition and feeding among adolescent girls and young mothers in rural Bangladesh. Matern. Child Nutr. 2015, 11, 173–189. [Google Scholar] [CrossRef]
- World Health Organisation. Indicators for Assessing Infant and Young Child Feeding Practices—Part 1—Definitions. Available online: http://apps.who.int/iris/bitstream/handle/10665/43895/9789241596664_eng.pdf?sequence=1&isAllowed=y (accessed on 30 June 2021).
- Ministry of Health and Family Welfare. National Family Health Survey (NFHS-4), 2015–2016; International Institute for Population Sciences (IIPS), ICF: Mumbai, India, 2017. [Google Scholar]
- Daelmans, B.; Dewey, K.; Arimond, M. New and updated indicators for assessing infant and young child feeding. Food Nutr. Bull. 2009, 30, 256. [Google Scholar] [CrossRef] [Green Version]
- Dhami, M.V.; Ogbo, F.A.; Diallo, T.M.; Agho, K.E. Regional analysis of associations between infant and young child feeding practices and Diarrhoea in Indian children. Int. J. Environ. Res. Public Health 2020, 17, 4740. [Google Scholar] [CrossRef]
- Archana, P.; Yamini, P.; Neetu, B.; Jitesh, B.; Kingsley, E.A.; Michael, J.D. Determinants of inappropriate complementary feeding practices in young children in India: Secondary analysis of National Family Health Survey 2005–2006. Matern. Child Nutr. 2010, 8, 28–44. [Google Scholar]
- Senarath, U.; Godakandage, S.S.P.; Jayawickrama, H.; Siriwardena, I.; Dibley, M.J. Determinants of inappropriate complementary feeding practices in young children in Sri Lanka: Secondary data analysis of Demographic and Health Survey 2006–2007. Matern. Child Nutr. 2012, 8, 60–77. [Google Scholar] [CrossRef] [PubMed]
- Na, M.; Aguayo, V.M.; Arimond, M.; Stewart, C.P. Risk factors of poor complementary feeding practices in Pakistani children aged 6–23 months: A multilevel analysis of the Demographic and Health Survey 2012–2013. Matern. Child Nutr. 2017, 13, e12463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hazir, T.; Akram, D.S.; Nisar, Y.B.; Kazmi, N.; Agho, K.E.; Abbasi, S.; Khan, A.M.; Dibley, M.J. Determinants of suboptimal breast-feeding practices in Pakistan. Public Health Nutr. 2013, 16, 659–672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filmer, D.; Pritchett, L.H. Estimating wealth effects without expenditure data—Or tears: An application to educational enrollments in states of India. Demography 2001, 38, 115–132. [Google Scholar]
- Ogbo, F.A.; Dhami, M.V.; Awosemo, A.O.; Olusanya, B.O.; Olusanya, J.; Osuagwu, U.L.; Ghimire, P.R.; Page, A.; Agho, K.E. Regional prevalence and determinants of exclusive breastfeeding in India. Int. Breastfeed. J. 2019, 14, 20. [Google Scholar] [CrossRef] [PubMed]
- Agho, K.E.; Ezeh, O.K.; Ogbo, F.A.; Enoma, A.I.; Raynes-Greenow, C. Factors associated with inadequate receipt of components and use of antenatal care services in Nigeria: A population-based study. Int. Health 2018, 10, 172–181. [Google Scholar] [CrossRef]
- Agho, K.E.; Osuagwu, U.L.; Ezeh, O.K.; Ghimire, P.R.; Chitekwe, S.; Ogbo, F.A. Gender differences in factors associated with prehypertension and hypertension in Nepal: A nationwide survey. PLoS ONE 2018, 13, e0203278. [Google Scholar] [CrossRef]
- Agho, K.E.; Ahmed, T.; Fleming, C.; Dhami, M.V.; Miner, C.A.; Torome, R.; Ogbo, F.A. Breastfeeding practices among adolescent mothers and associated factors in Bangladesh (2004–2014). Nutrients 2021, 13, 557. [Google Scholar] [CrossRef]
- Benova, L.; Siddiqi, M.; Abejirinde, I.-O.O.; Badejo, O. Time trends and determinants of breastfeeding practices among adolescents and young women in Nigeria, 2003–2018. BMJ Glob. Health 2020, 5, e002516. [Google Scholar] [CrossRef]
- Karim, F.; Khan, A.N.S.; Tasnim, F.; Chowdhury, M.A.K.; Billah, S.M.; Karim, T.; Arifeen, S.E. Prevalence and determinants of initiation of breastfeeding within one hour of birth: An analysis of the Bangladesh Demographic and Health Survey, 2014. PLoS ONE. 2019, 14, e0220224. [Google Scholar] [CrossRef]
- Senanayake, P.; O’Connor, E.; Ogbo, F.A. National and rural-urban prevalence and determinants of early initiation of breastfeeding in India. BMC Public Health 2019, 19, 896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sahu, M. Exclusive breastfeeding-mothers absolute affection. Acta Sci. Med Sci. 2018, 2, 1–2. [Google Scholar]
- Banke-Thomas, O.; Banke-Thomas, A.; Ameh, C.A. Utilisation of maternal health services by adolescent mothers in Kenya: Analysis of the demographic health survey 2008–2009. Int. J. Adolesc. Med. Health 2018, 30. [Google Scholar] [CrossRef] [PubMed]
- Jama, N.A.; Wilford, A.; Haskins, L.; Coutsoudis, A.; Spies, L.; Horwood, C. Autonomy and infant feeding decision-making among teenage mothers in a rural and urban setting in KwaZulu-Natal, South Africa. BMC Pregnancy Childbirth 2018, 18, 52. [Google Scholar] [CrossRef] [Green Version]
- Lamberti, L.M.; Walker, C.L.F.; Noiman, A.; Victora, C.; Black, R.E. Breastfeeding and the risk for diarrhea morbidity and mortality. BMC Public Health 2011, 11, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Mihrshahi, S.; Ichikawa, N.; Shuaib, M.; Oddy, W.; Ampon, R.; Dibley, M.J.; Kabir, A.I.; Peat, J.K. Prevalence of exclusive breastfeeding in Bangladesh and its association with diarrhoea and acute respiratory infection: Results of the multiple indicator cluster survey 2003. J. Health Popul. Nutr. 2007, 25, 195. [Google Scholar]
- Black, R.E.; Brown, K.H.; Becker, S.; Alim, A.A.; Merson, M.H. Contamination of weaning foods and transmission of enterotoxigenic Escherichia coli diarrhoea in children in rural Bangladesh. Trans. R. Soc. Trop. Med. Hyg. 1982, 76, 259–264. [Google Scholar] [CrossRef]
- Nasrul, N.; Hafid, F.; Ramadhan, K.; Suza, D.E.; Efendi, F. Factors associated with bottle feeding in children aged 0–23 months in Indonesia. Child. Youth Serv. Rev. 2020, 116, 105251. [Google Scholar] [CrossRef]
- Berde, A.S. Factors associated with bottle feeding in Namibia: Findings from Namibia 2013 demographic and health survey. J. Trop. Pediatrics 2018, 64, 460–467. [Google Scholar] [CrossRef]
- Naik, S.N.; Verma, A.; Dhumal, G.G. Knowledge, attitudes and practices regarding breastfeeding in postpartum mothers at a tertiary care institute during a public health awareness campaign. Breastfeed. Rev. 2017, 25, 7. [Google Scholar]
- Seid, S.S.; Muluneh, E.; Sinbirro, I.A.; Moga, T.T.; Haso, T.K.; Ibro, S.A. Utilization of bottle feeding practices and associated factors among mothers who have infant less than 12 months of age in Agaro Twon, Jimma Zone South West Ethiopia, 2018. Health Sci. J. 2019, 13, 1–10. [Google Scholar] [CrossRef]
- Issaka, A.I.; Agho, K.E.; Page, A.N.; Burns, P.L.; Stevens, G.J.; Dibley, M.J. Determinants of suboptimal complementary feeding practices among children aged 6–23 months in four anglophone W est A frican countries. Matern. Child Nutr. 2015, 11, 14–30. [Google Scholar] [CrossRef]
- Patel, A.; Badhoniya, N.; Khadse, S.; Senarath, U.; Agho, K.E.; Dibley, M.J. Infant and young child feeding indicators and determinants of poor feeding practices in India: Secondary data analysis of National Family Health Survey 2005–2006. Food Nutr. Bull. 2010, 31, 314–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mihrshahi, S.; Kabir, I.; Roy, S.K.; Agho, K.E.; Senarath, U.; Dibley, M.J.; South Asia Infant Feeding Research Network (SAIFRN). Determinants of infant and young child feeding practices in Bangladesh: Secondary data analysis of Demographic and Health Survey 2004. Food Nutr. Bull. 2010, 31, 295–313. [Google Scholar] [CrossRef] [Green Version]
- Munuswamy, S.; Nakamura, K.; Seino, K.; Kizuki, M. Inequalities in use of antenatal care and its service components in India. J. Rural. Med. 2013, 9, 2877. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mumbare, S.S.; Rege, R. Ante natal care services utilization, delivery practices and factors affecting them in tribal area of North Maharashtra. Indian J. Community Med. 2011, 36, 287. [Google Scholar] [CrossRef]
- Ram, F.; Singh, A. Is antenatal care effective in improving maternal health in rural Uttar Pradesh? Evidence from a district level household survey. J. Biosoc. Sci. 2006, 38, 433. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Das, J.K.; Rizvi, A.; Gaffey, M.F.; Walker, N.; Horton, S.; Webb, P.; Lartey, A.; Black, R.E.; Group, T.L.N.I.R.; et al. Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet 2013, 382, 452–477. [Google Scholar] [CrossRef]
- Chowdhury, M.R.K.; Rahman, M.S.; Khan, M.M.H. Levels and determinants of complementary feeding based on meal frequency among children of 6 to 23 months in Bangladesh. BMC Public Health 2016, 16, 944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nkoka, O.; Mhone, T.G.; Ntenda, P.A. Factors associated with complementary feeding practices among children aged 6–23 mo in Malawi: An analysis of the demographic and health survey 2015–2016. Int. Health 2018, 10, 466–479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mekonnen, T.C.; Workie, S.B.; Yimer, T.M.; Mersha, W.F. Meal frequency and dietary diversity feeding practices among children 6–23 months of age in Wolaita Sodo town, Southern Ethiopia. J. Health Popul. Nutr. 2017, 36, 18. [Google Scholar] [CrossRef] [PubMed]
- Abadura, S.A.; Lerebo, W.T.; Kulkarni, U.; Mekonnen, Z.A. Individual and community level determinants of childhood full immunization in Ethiopia: A multilevel analysis. BMC Public Health 2015, 15, 972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agize, A.; Jara, D.; Dejenu, G. Level of knowledge and practice of mothers on minimum dietary diversity practices and associated factors for 6–23-month-old children in Adea Woreda, Oromia, Ethiopia. BioMed Res. Int. 2017, 2017, 7204562. [Google Scholar] [CrossRef] [Green Version]
- Sekartaji, R.; Suza, D.E.; Fauziningtyas, R.; Almutairi, W.M.; Susanti, I.A.; Astutik, E.; Efendi, F. Dietary diversity and associated factors among children aged 6–23 months in Indonesia. J. Pediatric Nurs. 2021, 56, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Edris, M.; Atnafu, N.; Abota, T. Determinants of dietary diversity score among children age between 6–23 months in Bench Maji Zone, Southwest Ethiopia. Ped. Health Res. 2018, 3, 10. [Google Scholar]
- Organization WHO. Indicators for Assessing Infant and Young Child Feeding Practices: Definitions and Measurement Methods. Available online: https://www.who.int/publications/i/item/9789240018389 (accessed on 1 June 2021).
- Heidkamp, R.A.; Kang, Y.; Chimanya, K.; Garg, A.; Matji, J.; Nyawo, M.; Craig, H.; Arimond, M.; Lyman, A.L.T. Implications of updating the minimum dietary diversity for children indicator for tracking progress in the eastern and southern Africa region. Curr. Dev. Nutr. 2020, 4, nzaa141. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | n | % |
|---|---|---|
| Individual-level factors | ||
| Mother’s religion (n = 5147) | ||
| Hindu | 3997 | 77.7 |
| Muslim | 913 | 17.7 |
| Christian and others | 237 | 4.6 |
| Mother’s working status | ||
| Nonworking | 5071 | 98.5 |
| Working (past 12 months) | 76 | 1.5 |
| Mother’s education | ||
| No education | 936 | 18.2 |
| Primary | 631 | 12.3 |
| Secondary and above | 3581 | 69.6 |
| Father’s occupation | ||
| Nonagricultural | 527 | 10.2 |
| Agricultural | 311 | 6.0 |
| Not working | 4310 | 83.7 |
| Total Maternal BMI (Kg/m2, n = 5083) | ||
| <18.5 | 1408 | 27.7 |
| 18.5–24.9 | 3382 | 66.5 |
| 25+ | 293 | 5.8 |
| Mother’s age (years) | ||
| 15–17 | 668 | 13.0 |
| 18 | 1650 | 32.1 |
| 19 | 2830 | 55.0 |
| Marital status (n = 5135) | ||
| Currently married | 5091 | 99.1 |
| Formerly married # | 44 | 0.9 |
| Combined Mode and Place of delivery | ||
| Non-caesarean and home | 759 | 14.8 |
| Non-caesarean and health facility | 3517 | 68.3 |
| Caesarean and health facility | 871 | 16.9 |
| Type of delivery assistance | ||
| Health professional | 3704 | 72.4 |
| Traditional birth attendant | 450 | 8.8 |
| Others & | 966 | 18.9 |
| Number of antenatal clinic visits (n = 4885) | ||
| 8+ | 761 | 15.6 |
| 4–7 | 1806 | 37.0 |
| 1–3 | 1532 | 31.4 |
| None | 786 | 16.1 |
| Timely postnatal check | ||
| 0–2 days | 122 | 2.4 |
| After 2 days | 239 | 4.7 |
| No postnatal check | 4787 | 93.0 |
| Mothers reading newspapers | ||
| Not at all | 3659 | 71.1 |
| Yes/some ^ | 1489 | 28.9 |
| Mothers listening to radio | ||
| Not at all | 4562 | 88.6 |
| Yes/some ^ | 586 | 11.4 |
| Mothers watching television | ||
| Not at all | 1479 | 28.7 |
| Yes/some ^ | 3669 | 71.3 |
| Power over household decision making | ||
| Husband | 4480 | 87.0 |
| Woman alone | 667 | 13.0 |
| Power over earning | ||
| Husband | 4658 | 90.5 |
| Woman alone | 490 | 9.5 |
| Birth order | ||
| 1st born | 4437 | 86.2 |
| 2nd–4th | 711 | 13.8 |
| Preceding birth interval | ||
| No previous birth | 4471 | 86.9 |
| Yes | 677 | 13.2 |
| Sex of baby | ||
| Male | 2621 | 50.9 |
| Female | 2527 | 49.1 |
| Age of child (months) | ||
| 0–5 | 1862 | 36.2 |
| 6–11 | 1544 | 30.0 |
| 12–17 | 1088 | 21.1 |
| 18–23 | 654 | 12.7 |
| Low birth weight (<2500 g, n = 4464) | ||
| No | 3554 | 79.6 |
| Yes | 910 | 20.4 |
| Size of the baby (n = 5090) | ||
| Small | 735 | 14.4 |
| Average | 3192 | 62.7 |
| Large | 1164 | 22.9 |
| Children who had diarrhea recently | ||
| No | 4452 | 86.5 |
| Yes | 696 | 13.5 |
| Children with acute respiratory infection treatment | ||
| No | 4860 | 94.4 |
| Yes | 288 | 5.6 |
| Children who had fever in last 2 weeks | ||
| No | 4322 | 84.0 |
| Yes | 826 | 16.1 |
| Household-level factors | ||
| Wealth Index | ||
| Poor | 2941 | 57.1 |
| Middle | 1236 | 24.0 |
| Rich | 971 | 18.9 |
| Number of living children | ||
| 1 | 4525 | 87.9 |
| 2 to 3 | 623 | 12.1 |
| Source of drinking water | ||
| Improved | 3970 | 77.1 |
| Unimproved | 1178 | 22.9 |
| Type of toilet facility | ||
| Improved | 1887 | 36.7 |
| Unimproved | 3261 | 63.3 |
| Community-level factors | ||
| Residence | ||
| Urban | 995 | 19.3 |
| Rural | 4153 | 80.7 |
| Geographical region | ||
| North | 389 | 7.6 |
| South | 910 | 17.7 |
| East | 2066 | 40.1 |
| West | 707 | 13.7 |
| Central | 799 | 15.5 |
| Northeast | 276 | 5.4 |
| Type of caste or tribe | ||
| Schedule caste | 1211 | 23.5 |
| Schedule tribe | 699 | 13.6 |
| Other backward caste | 1990 | 38.7 |
| Other * | 1248 | 24.3 |
| Indicator | Size of Subsample (Weighted) | n (Weighted) | Rate (%) | 95% CI | |
|---|---|---|---|---|---|
| Early initiation of breastfeeding a | |||||
| Yes | 5148 | 2256 | 43.8 | 41.8 | 45.9 |
| Ever breastfed rate b | |||||
| Yes | 5148 | 5049 | 98.1 | 97.5 | 98.5 |
| Bottle feeding rate b | |||||
| Yes | 5148 | 854.1 | 16.6 | 15.1 | 18.3 |
| Exclusive breastfeeding rate c | |||||
| Yes | 1862 | 1154 | 62.0 | 58.7 | 65.2 |
| Predominant breastfeeding rate c | |||||
| Yes | 1862 | 331.4 | 17.8 | 15.5 | 20.4 |
| Continued breastfeeding rate (1 year) d | |||||
| Yes | 766.3 | 676.3 | 88.3 | 85.0 | 90.9 |
| Continued breastfeeding rate (2 years) e | |||||
| Yes | 408.5 | 291.4 | 71.3 | 62.0 | 79.1 |
| Early introduction of complementary feeding rate f | |||||
| Yes | 857 | 370.9 | 43.3 | 38.0 | 48.7 |
| Minimum dietary diversity g | |||||
| Yes | 3286 | 545.6 | 16.6 | 14.8 | 18.7 |
| Minimum meal frequency g | |||||
| Yes | 3286 | 898.8 | 27.4 | 25.1 | 29.8 |
| Minimum acceptable diet g | |||||
| Yes | 3286 | 222.1 | 6.8 | 5.5 | 8.2 |
| Median duration of any breastfeeding * (months) | 4.6 | ||||
| Median duration of exclusive breastfeeding * (months) | 23.0 | ||||
| Early Initiation of Breastfeeding | Exclusive Breastfeeding | |||||||
|---|---|---|---|---|---|---|---|---|
| uOR (95% CI) | p | OR (95% CI) | p | uOR (95% CI) | p | OR (95% CI) | p | |
| Individual-level factors | ||||||||
| Mother’s religion | ||||||||
| Hindu | 1.00 | 1.00 | ||||||
| Muslim | 0.97 (0.78, 1.20) | 0.766 | 0.96 (0.68, 1.37) | 0.829 | ||||
| Christian | 1.13 (0.73, 1.74) | 0.592 | 1.06 (0.46, 2.45) | 0.886 | ||||
| Mother’s working status | ||||||||
| Nonworking | 1.00 | 1.00 | ||||||
| Working (past 12 months) | 0.81 (0.41, 1.58) | 0.533 | 6.49 (0.85, 49.81) | 0.072 | ||||
| Mother’s education | ||||||||
| No education | 1.00 | 1.00 | 1.00 | |||||
| Primary | 0.99 (0.74, 1.32) | 0.929 | 0.53 (0.33, 0.86) | 0.011 | 0.55 (0.34, 0.88) | 0.013 | ||
| Secondary and above | 1.16 (0.95, 1.43) | 0.150 | 0.65 (0.46, 0.94) | 0.022 | 0.60 (0.41, 0.89) | 0.010 | ||
| Total Maternal BMI (Kg/m2) | ||||||||
| <18.5 | 1.00 | 1.00 | ||||||
| 18.5–24.9 | 1.02 (0.85, 1.21) | 0.849 | 1.27 (0.92, 1.74) | 0.144 | ||||
| 25+ | 0.93 (0.59, 1.45) | 0.737 | 0.84 (0.41, 1.70) | 0.620 | ||||
| Mother’s age (years) | ||||||||
| 15–17 | 1.00 | 1.00 | ||||||
| 18 | 0.77 (0.57, 1.02) | 0.070 | 1.24 (0.81, 1.89) | 0.326 | ||||
| 19 | 0.81 (0.62, 1.06) | 0.131 | 0.86 (0.58, 1.28) | 0.459 | ||||
| Marital status | ||||||||
| Currently married | 1.00 | 1.00 | ||||||
| Formerly married # | 5.64 (2.69, 11.85) | <0.001 | 0.27 (0.06, 1.16) | 0.079 | ||||
| Combined mode and place of delivery | ||||||||
| Non-caesarean and Home | 1.00 | 1.00 | 1.00 | |||||
| Non-caesarean and health facility | 1.48 (1.18, 1.86) | 0.001 | 1.36 (1.06, 1.73) | 0.013 | 0.86 (0.60, 1.25) | 0.444 | ||
| Caesarean and health facility | 0.56 (0.41, 0.76) | <0.001 | 0.43 (0.30, 0.62) | <0.001 | 0.72 (0.45, 1.18) | 0.195 | ||
| Type of delivery assistance | ||||||||
| Health professional | 1.00 | 1.00 | ||||||
| Traditional birth attendant | 0.69 (0.52, 0.92) | 0.010 | 0.90 (0.59, 1.38) | 0.641 | ||||
| Others & | 0.68 (0.55, 0.85) | <0.001 | 0.74 (0.53, 1.05) | 0.096 | ||||
| Number of antenatal clinic visits | ||||||||
| 8+ | 1.00 | 1.00 | 1.00 | |||||
| 4–7 | 0.75 (0.56, 1.01) | 0.056 | 0.82 (0.60, 1.11) | 0.209 | 1.33 (0.81, 2.18) | 0.265 | ||
| 1–3 | 0.64 (0.48, 0.85) | 0.002 | 0.75 (0.55, 1.01) | 0.066 | 0.98 (0.61, 1.58) | 0.938 | ||
| None | 0.52 (0.37, 0.72) | <0.001 | 0.58 (0.41, 0.83) | 0.003 | 1.06 (0.62, 1.81) | 0.836 | ||
| Timely postnatal check | ||||||||
| 0–2 days | 1.00 | 1.00 | 1.00 | |||||
| After 2 days | 0.64 (0.35, 1.17) | 0.147 | 3.60 (1.25, 10.36) | 0.017 | 3.47 (1.19, 10.08) | 0.022 | ||
| No postnatal check | 0.66 (0.42, 1.05) | 0.078 | 2.89 (1.35, 6.18) | 0.006 | 3.06 (1.44, 6.49) | 0.003 | ||
| Mothers reading newspapers | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.01 (0.84, 1.21) | 0.894 | 0.89 (0.66, 1.18) | 0.411 | ||||
| Mothers listening to radio | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 0.96 (0.75, 1.23) | 0.746 | 0.75 (0.51, 1.12) | 0.162 | ||||
| Mothers watching television | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.17 (0.99, 1.38) | 0.068 | 1.07 (0.81, 1.41) | 0.623 | ||||
| Power over household decision making | ||||||||
| Husband | 1.00 | 1.00 | ||||||
| Woman alone | 0.98 (0.76, 1.27) | 0.896 | 1.16 (0.73, 1.84) | 0.527 | ||||
| Power over earning | ||||||||
| Husband | 1.00 | 1.00 | ||||||
| Woman alone | 1.05 (0.78, 1.41) | 0.754 | 1.35 (0.83, 2.18) | 0.221 | ||||
| Father’s occupation | ||||||||
| Nonagricultural | 1.00 | 1.00 | ||||||
| Agricultural | 1.28 (0.84, 1.96) | 0.256 | 1.19 (0.53, 2.65) | 0.677 | ||||
| Not working | 1.19 (0.89, 1.60) | 0.238 | 0.84 (0.48, 1.47) | 0.552 | ||||
| Birth order | ||||||||
| 1st born | 1.00 | 1.00 | 1.00 | |||||
| 2nd–4th | 1.41 (1.12, 1.77) | 0.003 | 0.49 (0.34, 0.71) | <0.001 | 0.46 (0.31, 0.66) | <0.001 | ||
| Preceding birth interval | ||||||||
| No previous birth | 1.00 | 1.00 | ||||||
| Yes | 1.36 (1.08, 1.71) | 0.008 | 0.5 (0.35, 0.71) | <0.001 | ||||
| Sex of baby | ||||||||
| Male | 1.00 | 1.00 | ||||||
| Female | 1.15 (0.97, 1.36) | 0.097 | 0.88 (0.67, 1.16) | 0.375 | ||||
| Child’s age (in <6 months) | 0.64 (0.59, 0.71) | <0.001 | ||||||
| Child’s age in category | ||||||||
| 0–5 | 1.00 | |||||||
| 6–11 | 1.01 (0.82, 1.24) | 0.943 | ||||||
| 12–17 | 1.12 (0.90, 1.38) | 0.320 | ||||||
| 18–23 | 1.13 (0.85, 1.49) | 0.412 | ||||||
| Low Birth Weight (<2500 g) | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 0.98 (0.79, 1.23) | 0.881 | 1.28 (0.89, 1.82) | 0.178 | ||||
| Size of the baby | ||||||||
| Small | 1.00 | 1.00 | ||||||
| Average | 0.94 (0.74, 1.19) | 0.598 | 0.92 (0.63, 1.36) | 0.688 | ||||
| Large | 0.85 (0.64, 1.13) | 0.259 | 0.84 (0.52, 1.35) | 0.469 | ||||
| Children who had diarrhea recently | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 0.68 (0.54, 0.86) | 0.001 | 0.75 (0.57, 0.97) | 0.030 | 0.58 (0.38, 0.88) | 0.012 | 0.62 (0.40, 0.95) | 0.031 |
| Children with acute respiratory infection treatment | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 0.74 (0.51, 1.06) | 0.102 | 0.42 (0.19, 0.95) | 0.037 | ||||
| Children who had fever in last 2 weeks | ||||||||
| No | 1.00 | 1.00 | 1.00 | |||||
| Yes | 0.72 (0.57, 0.91) | 0.006 | 0.77 (0.61, 0.98) | 0.037 | 0.84 (0.57, 1.24) | 0.390 | ||
| Household-level factors | ||||||||
| Wealth index | ||||||||
| Poor | 1.00 | 1.00 | ||||||
| Middle | 0.90 (0.74, 1.11) | 0.332 | 0.94 (0.67, 1.32) | 0.724 | ||||
| Rich | 0.89 (0.71, 1.12) | 0.309 | 0.86 (0.60, 1.25) | 0.435 | ||||
| Number of living children | ||||||||
| 1 | 1.00 | |||||||
| 2 to 3 | 1.51 (1.19, 1.93) | 0.001 | 0.44 (0.30, 0.64) | <0.001 | ||||
| Source of drinking water | ||||||||
| Improved | 1.00 | 1.00 | ||||||
| Unimproved | 0.96 (0.79, 1.16) | 0.687 | 1.36 (0.99, 1.86) | 0.055 | ||||
| Type of toilet facility | ||||||||
| Improved | 1.00 | 1.00 | ||||||
| Unimproved | 1.00 (0.84, 1.20) | 0.944 | 1.3 (0.97, 1.74) | 0.085 | ||||
| Community-level factors | ||||||||
| Residence | ||||||||
| Urban | 1.00 | 1.00 | ||||||
| Rural | 0.87 (0.68, 1.11) | 0.264 | 0.98 (0.67, 1.45) | 0.952 | ||||
| Geographical region | ||||||||
| North | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| South | 1.84 (1.37, 2.49) | <0.001 | 2.19 (1.56, 3.06) | <0.001 | 1.15 (0.70, 1.88) | 0.575 | 1.28 (0.77, 2.11) | 0.326 |
| East | 1.54 (1.20, 1.99) | 0.001 | 1.69 (1.31, 2.18) | <0.001 | 0.86 (0.56, 1.31) | 0.500 | 0.82 (0.54, 1.24) | 0.360 |
| West | 2.55 (1.80, 3.61) | <0.001 | 2.66 (1.88, 3.75) | <0.001 | 0.90 (0.50, 1.59) | 0.720 | 0.89 (0.51, 1.57) | 0.704 |
| Central | 0.90 (0.69, 1.16) | 0.430 | 0.99 (0.76, 1.30) | 0.992 | 0.63 (0.42, 0.96) | 0.034 | 0.63 (0.42, 0.95) | 0.031 |
| Northeast | 3.92 (2.94, 5.23) | <0.001 | 4.26 (3.15, 5.75) | <0.001 | 1.40 (0.85, 2.31) | 0.174 | 1.33 (0.78, 2.25) | 0.288 |
| Type of caste or tribe | ||||||||
| Schedule caste | 1.00 | 1.00 | 1.00 | |||||
| Schedule tribe | 0.95 (0.73, 1.23) | 0.684 | 1.98 (1.26, 3.09) | 0.003 | 2.00 (1.27, 3.16) | 0.003 | ||
| Other backward caste | 0.87 (0.70, 1.07) | 0.183 | 1.05 (0.73, 1.49) | 0.781 | 1.02 (0.71, 1.45) | 0.900 | ||
| Other * | 1.11 (0.85, 1.44) | 0.444 | 1.11 (0.72, 1.70) | 0.621 | 1.08 (0.69, 1.67) | 0.727 | ||
| Bottle Feeding | Predominant Breastfeeding | |||||||
|---|---|---|---|---|---|---|---|---|
| uOR (95% CI) | p | OR (95% CI) | p | uOR (95% CI) | p | OR (95% CI) | p | |
| Individual-level factors | ||||||||
| Mother’s religion | ||||||||
| Hindu | 1.00 | 1.00 | ||||||
| Muslim | 1.10 (0.82, 1.47) | 0.522 | 0.56 (0.35, 0.90) | 0.016 | ||||
| Christian | 0.93 (0.53, 1.63) | 0.796 | 1.25 (0.42, 3.75) | 0.685 | ||||
| Mother’s working status | ||||||||
| Nonworking | 1.00 | 1.00 | ||||||
| Working (past 12 months) | 0.78 (0.36, 1.69) | 0. 583 | 0.42 (0.05, 3.77) | 0.434 | ||||
| Mother’s education | ||||||||
| No education | 1.00 | 1.00 | 1.00 | |||||
| Primary | 1.40 (0.93, 2.13) | 0.110 | 1.81 (1.06, 3.09) | 0.028 | 1.90 (1.06, 3.39) | 0.029 | ||
| Secondary and above | 1.54 (1.15, 2.07) | 0.004 | 1.18 (0.77, 1.80) | 0.445 | 1.41 (0.88, 2.26) | 0.142 | ||
| Total maternal BMI (Kg/m2) | ||||||||
| <18.5 | 1.00 | 1.00 | ||||||
| 18.5–24.9 | 1.04 (0.81, 1.33) | 0.748 | 0.82 (0.57, 1.17) | 0.276 | ||||
| 25+ | 2.14 (1.18, 3.86) | 0.012 | 0.54 (0.23, 1.29) | 0.165 | ||||
| Mother’s age (years) | ||||||||
| 15–17 | 1.00 | 1.00 | ||||||
| 18 | 1.06 (0.69, 1.63) | 0.797 | 1.31 (0.81, 2.14) | 0.276 | ||||
| 19 | 1.24 (0.84, 1.83) | 0.286 | 1.50 (0.94, 2.41) | 0.092 | ||||
| Marital status | ||||||||
| Currently married | 1.00 | 1.00 | ||||||
| Formerly married # | 0.94 (0.41, 2.19) | 0.895 | 1.91(0.33, 11.10) | 0.472 | ||||
| Combined mode and place of delivery | ||||||||
| Non-caesarean and home | 1.00 | 1.00 | 1.00 | |||||
| Non-caesarean and health facility | 1.72 (1.22, 2.43) | 0.002 | 1.58 (1.10, 2.26) | 0.011 | 1.29 (0.83, 2) | 0.259 | ||
| Caesarean and health facility | 2.98 (1.94, 4.59) | <0.001 | 2.45 (1.58, 3.81) | <0.001 | 1.02 (0.56, 1.86) | 0.947 | ||
| Type of delivery assistance | ||||||||
| Health professional | 1.00 | 1.00 | 1.00 | |||||
| Traditional birth attendant | 0.76 (0.52, 1.1) | 0.142 | 1.46 (0.90, 2.36) | 0.122 | 1.60 (0.94, 2.73) | 0.081 | ||
| Others & | 0.84 (0.6, 1.18) | 0.321 | 1.74 (1.13, 2.69) | 0.011 | 1.60 (1.04, 2.47) | 0.031 | ||
| Number of antenatal clinic visits | ||||||||
| 8+ | 1.00 | 1.00 | ||||||
| 4–7 | 0.92 (0.64, 1.33) | 0.676 | 0.73 (0.39, 1.36) | 0.318 | ||||
| 1–3 | 0.92 (0.65, 1.31) | 0.655 | 1.16 (0.64, 2.10) | 0.635 | ||||
| None | 0.94 (0.59, 1.51) | 0.799 | 0.96 (0.50, 1.86) | 0.907 | ||||
| Timely postnatal check | ||||||||
| 0–2 days | 1.00 | 1.00 | ||||||
| After 2 days | 0.99 (0.44, 2.20) | 0.977 | 0.79 (0.20, 3.20) | 0.742 | ||||
| No postnatal check | 0.84 (0.45, 1.58) | 0.596 | 1.97 (0.64, 6.07) | 0.238 | ||||
| Mothers reading newspapers | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.03 (0.81, 1.32) | 0.809 | 1.33 (0.93, 1.90) | 0.119 | ||||
| Mothers listening to radio | ||||||||
| Not at all | 1.00 | 1.00 | 1.00 | |||||
| Yes/some ^ | 1.49 (1.07, 2.08) | 0.018 | 1.51 (1.07, 2.11) | 0.016 | 0.79 (0.48, 1.30) | 0.352 | ||
| Mothers watching television | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.53 (1.20, 1.95) | 0.001 | 0.74 (0.53, 1.03) | 0.070 | ||||
| Power over household decision making | ||||||||
| Husband | 1.00 | 1.00 | ||||||
| Woman alone | 1.31 (0.89, 1.92) | 0.170 | 1.01 (0.53, 1.91) | 0.972 | ||||
| Power over earning | ||||||||
| Husband | 1.00 | 1.00 | ||||||
| Woman alone | 1.25 (0.78, 1.99) | 0.359 | 0.99 (0.56, 1.76) | 0.980 | ||||
| Father’s occupation | ||||||||
| Nonagricultural | 1.00 | 1.00 | ||||||
| Agricultural | 0.53 (0.28, 0.98) | 0.043 | 0.97 (0.33, 2.84) | 0.958 | ||||
| Not working | 0.70 (0.45, 1.09) | 0.112 | 1.10 (0.50, 2.44) | 0.809 | ||||
| Birth order | ||||||||
| 1st born | 1.00 | 1.00 | ||||||
| 2nd–4th | 0.78 (0.55, 1.10) | 0.158 | 0.98 (0.62, 1.53) | 0.912 | ||||
| Preceding birth interval | ||||||||
| No previous birth | 1.00 | 1.00 | ||||||
| Yes | 0.66 (0.46, 0.95) | 0.025 | 0.89 (0.56, 1.40) | 0.611 | ||||
| Sex of baby | ||||||||
| Male | 1.00 | 1.00 | ||||||
| Female | 1.00 (0.80, 1.27) | 0.975 | 1.19 (0.85, 1.66) | 0.304 | ||||
| Child’s age (in <6 months) | 1.50 (1.34, 1.67) | <0.001 | 1.51 (1.35, 1.69) | <0.001 | ||||
| Child’s age in category | ||||||||
| 0–5 | 1.00 | 1.00 | ||||||
| 6–11 | 1.65 (1.21, 2.27) | 0.002 | 1.64 (1.20, 2.24) | 0.002 | ||||
| 12–17 | 2.01 (1.48, 2.72) | <0.001 | 2.07 (1.52, 2.80) | <0.001 | ||||
| 18–23 | 1.86 (1.28, 2.69) | 0.001 | 1.89 (1.30, 2.75) | 0.001 | ||||
| Low birth weight (<2500 g) | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 1.16 (0.88, 1.52) | 0.286 | 1.02 (0.67, 1.54) | 0.931 | ||||
| Size of the baby | ||||||||
| Small | 1.00 | 1.00 | ||||||
| Average | 0.78 (0.58, 1.04) | 0.093 | 1.27 (0.82, 1.98) | 0.283 | ||||
| Large | 1.14 (0.79, 1.64) | 0.474 | 0.96 (0.52, 1.76) | 0.901 | ||||
| Children who had diarrhea recently | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 1.19 (0.89, 1.59) | 0.233 | 1.76 (1.04, 2.96) | 0.035 | ||||
| Children with acute respiratory infection treatment | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 1.37 (0.89, 2.09) | 0.149 | 1.60 (0.54, 4.81) | 0.347 | ||||
| Children who had fever in last 2 weeks | ||||||||
| No | 1.00 | 1.00 | 1.00 | |||||
| Yes | 1.68 (1.28, 2.20) | <0.001 | 1.54 (1.17, 2.03) | 0.002 | 1.25 (0.78, 2.01) | 0.362 | ||
| Household-level factors | ||||||||
| Wealth index | ||||||||
| Poor | 1.00 | 1.00 | 1.00 | |||||
| Middle | 1.75 (1.31, 2.33) | <0.001 | 1.42 (1.08, 1.88) | 0.012 | 1.29 (0.86, 1.94) | 0.215 | ||
| Rich | 1.98 (1.49, 2.64) | <0.001 | 1.61 (1.20, 2.16) | 0.001 | 1.03 (0.64, 1.65) | 0.918 | ||
| Number of living children | ||||||||
| 1 | 1.00 | 1.00 | ||||||
| 2 to 3 | 0.76 (0.53, 1.11) | 0.160 | 1.03 (0.65, 1.65) | 0.886 | ||||
| Source of drinking water | ||||||||
| Improved | 1.00 | 1.00 | ||||||
| Unimproved | 0.85 (0.65, 1.12) | 0.245 | 0.69 (0.47, 1.01) | 0.056 | ||||
| Type of toilet facility | ||||||||
| Improved | 1.00 | 1.00 | ||||||
| Unimproved | 0.68 (0.53, 0.86) | 0.002 | 0.88 (0.61, 1.28) | 0.510 | ||||
| Community-level factors | ||||||||
| Residence | ||||||||
| Urban | 1.00 | 1.00 | ||||||
| Rural | 0.77 (0.55, 1.07) | 0.117 | 0.99 (0.60, 1.63) | 0.977 | ||||
| Geographical region | ||||||||
| North | 1.00 | 1.00 | 1.00 | |||||
| South | 1.20 (0.82, 1.74) | 0.352 | 0.61 (0.33, 1.15) | 0.129 | 0.63 (0.33, 1.21) | 0.168 | ||
| East | 1.06 (0.76, 1.46) | 0.747 | 0.69 (0.42, 1.15) | 0.164 | 0.58 (0.34, 1.00) | 0.052 | ||
| West | 0.70 (0.40, 1.23) | 0.213 | 1.37 (0.71, 2.65) | 0.345 | 1.24 (0.65, 2.35) | 0.503 | ||
| Central | 1.10 (0.80, 1.52) | 0.559 | 1.51 (0.93, 2.44) | 0.088 | 1.36 (0.82, 2.27) | 0.227 | ||
| Northeast | 0.69 (0.48, 1.00) | 0.051 | 0.39 (0.21, 0.75) | 0.005 | 0.31 (0.15, 0.63) | 0.001 | ||
| Type of caste or tribe | ||||||||
| Schedule caste | 1.00 | 1.00 | 1.00 | |||||
| Schedule tribe | 0.52 (0.35, 0.77) | 0.001 | 0.61 (0.40, 0.92) | 0.021 | 0.80 (0.47, 1.37) | 0.421 | ||
| Other backward caste | 1.12 (0.84, 1.51) | 0.419 | 1.05 (0.78, 1.42) | 0.727 | 1.03 (0.66, 1.59) | 0.906 | ||
| Other * | 1.46 (1.02, 2.09) | 0.035 | 1.37 (0.96, 1.96) | 0.081 | 0.61 (0.36, 1.05) | 0.074 | ||
| Introduction to Solid, Semisolid or Soft Foods | Minimum Dietary Diversity | |||||||
|---|---|---|---|---|---|---|---|---|
| uOR (95% CI) | p | OR (95% CI) | p | uOR (95% CI) | p | OR (95% CI) | p | |
| Individual-level factors | ||||||||
| Mother’s religion | ||||||||
| Hindu | 1.00 | 1.00 | ||||||
| Muslim | 0.81 (0.46, 1.44) | 0.477 | 1.22 (0.86, 1.73) | 0.275 | ||||
| Christian | 1.43 (0.56, 3.64) | 0.458 | 1.04 (0.56, 1.93) | 0.901 | ||||
| Mother’s working status | ||||||||
| Nonworking | 1.00 | 1.00 | ||||||
| Working (past 12 months) | 0.68 (0.15, 3.15) | 0.625 | 0.85 (0.36, 2.05) | 0.727 | ||||
| Mother’s education | ||||||||
| No education | 1.00 | 1.00 | 1.00 | |||||
| Primary | 1.61 (0.79, 3.27) | 0.187 | 1.19 (0.70, 2.01) | 0.503 | 1.20 (0.69, 2.10) | 0.504 | ||
| Secondary and above | 1.55 (0.95, 2.52) | 0.081 | 1.86 (1.28, 2.73) | 0.001 | 1.67 (1.10, 2.52) | 0.014 | ||
| Total maternal BMI (Kg/m2) | ||||||||
| <18.5 | 1.00 | 1.00 | ||||||
| 18.5–24.9 | 0.80 (0.52, 1.24) | 0.318 | 0.99 (0.73, 1.34) | 0.935 | ||||
| 25+ | 1.52 (0.46, 5.01) | 0.489 | 1.22 (0.65, 2.30) | 0.541 | ||||
| Mother’s age (years) | ||||||||
| 15–17 | 1.00 | 1.00 | ||||||
| 18 | 0.79 (0.37, 1.70) | 0.550 | 0.97 (0.59, 1.58) | 0.897 | ||||
| 19 | 0.73 (0.37, 1.44) | 0.358 | 1.08 (0.70, 1.67) | 0.730 | ||||
| Marital status | ||||||||
| Currently married | 1.00 | 1.00 | 1.00 | |||||
| Formerly married # | 1.39 (0.17, 1.52) | 0.757 | 0.20 (0.07, 0.56) | 0.002 | 0.19 (0.06, 0.60) | 0.005 | ||
| Combined mode and place of delivery | ||||||||
| Non-caesarean and Home | 1.00 | 1.00 | ||||||
| Non-caesarean and Health Facility | 0.99 (0.56, 1.73) | 0.963 | 1.34 (0.88, 2.04) | 0.171 | ||||
| Caesarean and Health Facility | 1.25 (0.57, 2.74) | 0.584 | 1.95 (1.18, 3.21) | 0.009 | ||||
| Type of delivery assistance | ||||||||
| Health professional | 1.00 | 1.00 | ||||||
| Traditional birth attendant | 0.87 (0.45, 1.70) | 0.682 | 0.58 (0.36, 0.93) | 0.025 | ||||
| Others & | 1.13 (0.62, 2.06) | 0.690 | 1.06 (0.73, 1.56) | 0.749 | ||||
| Number of antenatal clinic visits | ||||||||
| 8+ | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 4–7 | 0.76 (0.36, 1.60) | 0.479 | 0.88 (0.42, 1.86) | 0.752 | 0.60 (0.38, 0.93) | 0.024 | 0.55 (0.33, 0.90) | 0.020 |
| 1–3 | 0.36 (0.17, 0.74) | 0.006 | 0.42 (0.19, 0.91) | 0.029 | 0.47 (0.30, 0.73) | 0.001 | 0.49 (0.29, 0.82) | 0.007 |
| None | 0.46 (0.17, 1.23) | 0.123 | 0.52 (0.21, 1.30) | 0.165 | 0.41 (0.24, 0.69) | 0.001 | 0.47 (0.26, 0.84) | 0.011 |
| Timely postnatal check | ||||||||
| 0–2 days | 1.00 | 1.00 | ||||||
| After 2 days | 0.86 (0.20, 3.77) | 0.839 | 1.09 (0.44, 2.74) | 0.847 | ||||
| No postnatal check | 0.51 (0.16, 1.61) | 0.251 | 1.05 (0.52, 2.09) | 0.899 | ||||
| Mothers reading newspapers | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.30 (0.80, 2.11) | 0.296 | 1.05 (0.78, 1.43) | 0.744 | ||||
| Mothers listening to radio | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.19 (0.60, 2.38) | 0.619 | 1.27 (0.86, 1.88) | 0.230 | ||||
| Mothers watching television | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.49 (0.97, 2.27) | 0.066 | 1.67 (1.24, 2.25) | 0.001 | ||||
| Power over household decision making | ||||||||
| Husband | 1.00 | |||||||
| Woman alone | 2.12 (1.02, 4.38) | 0.044 | 1.04 (0.68, 1.57) | 0.864 | ||||
| Power over earning | ||||||||
| Husband | 1.00 | 1.00 | ||||||
| Woman alone | 1.90 (0.78, 4.63) | 0.158 | 1.12 (0.7, 1.80) | 0.628 | ||||
| Father’s occupation | ||||||||
| Nonagricultural | 1.00 | 1.00 | ||||||
| Agricultural | 0.61 (0.21, 1.81) | 0.370 | 0.76 (0.39, 1.50) | 0.435 | ||||
| Not working | 0.56 (0.24, 1.30) | 0.176 | 1.11 (0.69, 1.78) | 0.681 | ||||
| Birth order | ||||||||
| 1st born | 1.00 | 1.00 | ||||||
| 2nd–4th | 1.62 (0.89, 2.95) | 0.114 | 1.08 (0.73, 1.61) | 0.701 | ||||
| Preceding birth interval | ||||||||
| No previous birth | 1.00 | 1.00 | ||||||
| Yes | 1.57 (0.85, 2.90) | 0.149 | 1.13 (0.76, 1.69) | 0.535 | ||||
| Sex of baby | ||||||||
| Male | 1.00 | 1.00 | ||||||
| Female | 1.35 (0.88, 2.08) | 0.171 | 1.10 (0.83, 1.46) | 0.487 | ||||
| Child age in 6–8 months | 1.26 (0.98, 1.62) | 0.074 | ||||||
| Child age in category | 1.00 | 1.00 | ||||||
| 6–11 | 3.88 (2.59, 5.82) | <0.001 | 3.95 (2.62, 5.95) | <0.001 | ||||
| 12–17 | 4.64 (3.01, 7.15) | <0.001 | 4.79 (3.10, 7.42) | <0.001 | ||||
| 18–23 | ||||||||
| Low birth weight (<2500 g) | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 0.82 (0.47, 1.44) | 0.490 | 1.29 (0.87, 1.90) | 0.209 | ||||
| Size of the baby | ||||||||
| Small | 1 | 1 | ||||||
| Average | 0.67 (0.37, 1.23) | 0.197 | 0.75 (0.51, 1.12) | 0.156 | ||||
| Large | 0.97 (0.46, 2.02) | 0.929 | 1.05 (0.67, 1.65) | 0.841 | ||||
| Children who had diarrhea recently | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 1.62 (0.96, 2.74) | 0.070 | 1.03 (0.71, 1.49) | 0.879 | ||||
| Children with acute respiratory infection treatment | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 1.62 (0.73, 3.61) | 0.232 | 1.06 (0.62, 1.82) | 0.836 | ||||
| Children who had fever in last 2 weeks | ||||||||
| No | 1.00 | 1.00 | 1.00 | |||||
| Yes | 1.31 (0.78, 2.18) | 0.306 | 1.50 (1.05, 2.15) | 0.025 | 1.65 (1.09, 2.48) | 0.016 | ||
| Household-level factors | ||||||||
| Wealth index | ||||||||
| Poor | 1.00 | 1.00 | 1.00 | |||||
| Middle | 2.68 (1.59, 4.50) | <0.001 | 2.57 (1.50, 4.40) | 0.001 | 1.11 (0.80, 1.56) | 0.525 | ||
| Rich | 1.10 (0.62, 1.94) | 0.735 | 1.02 (0.54, 1.90) | 0.941 | 1.23 (0.83, 1.82) | 0.297 | ||
| Number of living children | ||||||||
| 1 | 1.00 | 1.00 | ||||||
| 2 to 3 | 1.78 (0.94, 3.40) | 0.079 | 1.15 (0.75, 1.77) | 0.523 | ||||
| Source of drinking water | ||||||||
| Improved | 1.00 | 1.00 | ||||||
| Unimproved | 0.91 (0.56, 1.49) | 0.710 | 0.86 (0.61, 1.23) | 0.414 | ||||
| Type of toilet facility | ||||||||
| Improved | 1.00 | 1.00 | ||||||
| Unimproved | 0.79 (0.50, 1.26) | 0.325 | 0.89 (0.67, 1.20) | 0.453 | ||||
| Community-level factors | ||||||||
| Residence | ||||||||
| Urban | 1 | 1 | ||||||
| Rural | 0.82 (0.42, 1.60) | 0.555 | 0.87 (0.58, 1.29) | 0.476 | ||||
| Geographical region | ||||||||
| North | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| South | 2.79 (1.25, 6.22) | 0.012 | 2.15 (0.89, 5.18) | 0.085 | 4.41 (2.62, 7.43) | <0.001 | 3.59 (2.02, 6.40) | <0.001 |
| East | 1.58 (0.83, 3.00) | 0.160 | 1.69 (0.85, 3.36) | 0.133 | 2.73 (1.67, 4.44) | <0.001 | 2.77 (1.68, 4.56) | <0.001 |
| West | 3.37 (1.36, 8.38) | 0.009 | 2.66 (1.04, 6.76) | 0.040 | 1.47 (0.70, 3.07) | 0.299 | 1.22 (0.55, 2.71) | 0.622 |
| Central | 2.22 (1.18, 4.17) | 0.012 | 2.71 (1.37, 5.35) | 0.004 | 1.14 (0.67, 1.93) | 0.610 | 1.29 (0.75, 2.24) | 0.346 |
| Northeast | 2.27 (1.07, 4.78) | 0.031 | 2.63 (1.18, 5.87) | 0.018 | 3.13 (1.88, 5.22) | <0.001 | 3.38 (1.91, 5.98) | <0.001 |
| Type of caste or tribe | ||||||||
| Schedule caste | 1.00 | 1.00 | 1.00 | |||||
| Schedule tribe | 1.03 (0.57, 1.89) | 0.916 | 0.57 (0.37, 0.88) | 0.012 | 0.85 (0.52, 1.39) | 0.534 | ||
| Other backward caste | 0.84 (0.50, 1.43) | 0.531 | 0.67 (0.46, 0.96) | 0.031 | 0.64 (0.42, 0.98) | 0.040 | ||
| Other * | 1.22 (0.62, 2.39) | 0.571 | 0.67 (0.43, 1.03) | 0.070 | 0.59 (0.34, 1.02) | 0.060 | ||
| Minimum Meal Frequency | Minimum Acceptable Diet | |||||||
|---|---|---|---|---|---|---|---|---|
| uOR (95% CI) | p | OR (95% CI) | p | uOR (95% CI) | p | OR (95% CI) | p | |
| Individual-level factors | ||||||||
| Mother’s religion | ||||||||
| Hindu | 1.00 | 1.00 | ||||||
| Muslim | 0.91 (0.67, 1.25) | 0.560 | 0.8 (0.42, 1.52) | 0.491 | ||||
| Christian | 1.37 (0.79, 2.40) | 0.266 | 1.11 (0.42, 2.96) | 0.837 | ||||
| Mother’s working status | ||||||||
| Nonworking | 1.00 | 1.00 | ||||||
| Working (past 12 months) | 1.08 (0.54, 2.16) | 0.825 | 0.45 (0.14, 1.41) | 0.173 | ||||
| Mother’s education | ||||||||
| No education | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Primary | 1.51 (1.00, 2.28) | 0.046 | 1.59 (1.06, 2.41) | 0.025 | 1.45 (0.63, 3.30) | 0.374 | 1.52 (0.66, 3.49) | 0.318 |
| Secondary and above | 1.25 (0.95, 1.65) | 0.105 | 1.41 (1.06, 1.87) | 0.016 | 1.83 (1.01, 3.31) | 0.045 | 1.94 (1.06, 3.53) | 0.030 |
| Total maternal BMI (Kg/m2) | ||||||||
| <18.5 | 1.00 | 1.00 | ||||||
| 18.5–24.9 | 1.06 (0.84, 1.35) | 0.613 | 0.81 (0.52, 1.29) | 0.377 | ||||
| 25+ | 1.38 (0.67, 2.85) | 0.382 | 0.61 (0.22, 1.74) | 0.355 | ||||
| Mother’s age (years) | ||||||||
| 15–17 | 1.00 | 1.00 | 1.00 | |||||
| 18 | 1.54 (0.99, 2.41) | 0.054 | 1.60 (1.02, 2.51) | 0.039 | 1.24 (0.59, 2.61) | 0.573 | ||
| 19 | 1.51 (1.00, 2.28) | 0.047 | 1.57 (1.04, 2.37) | 0.030 | 1.18 (0.59, 2.33) | 0.642 | ||
| Marital status | ||||||||
| Currently married | 1.00 | 1.00 | 1.00 | |||||
| Formerly married # | 1.98 (0.72, 5.48) | 0.187 | 0.11 (0.03, 0.38) | 0.001 | 0.12 (0.03, 0.44) | 0.001 | ||
| Combined mode and place of delivery | ||||||||
| Non-caesarean and home | 1.00 | 1.00 | ||||||
| Non-caesarean and health facility | 1.21 (0.88, 1.66) | 0.241 | 1.37 (0.66, 2.88) | 0.401 | ||||
| Caesarean and health facility | 1.39 (0.89, 2.18) | 0.152 | 1.91 (0.82, 4.47) | 0.134 | ||||
| Type of delivery assistance | ||||||||
| Health professional | 1.00 | 1.00 | ||||||
| Traditional birth attendant | 0.82 (0.57, 1.2) | 0.318 | 0.61 (0.33, 1.15) | 0.128 | ||||
| Others & | 1.30 (0.96, 1.76) | 0.092 | 1.19 (0.71, 2.01) | 0.510 | ||||
| Number of antenatal clinic visits | ||||||||
| 8+ | 1.00 | 1.00 | ||||||
| 4–7 | 1.42 (0.96, 2.1) | 0.075 | 1.11 (0.58, 2.13) | 0.750 | ||||
| 1–3 | 0.80 (0.55, 1.18) | 0.263 | 0.55 (0.28, 1.07) | 0.078 | ||||
| None | 1.06 (0.66, 1.69) | 0.822 | 0.66 (0.3, 1.46) | 0.306 | ||||
| Timely postnatal check | ||||||||
| 0–2 days | 1.00 | 1.00 | ||||||
| After 2 days | 1.87 (0.72, 4.85) | 0.195 | 2.97 (0.6, 14.75) | 0.183 | ||||
| No postnatal check | 1.72 (0.78, 3.83) | 0.177 | 3.10 (1.02, 9.45) | 0.047 | ||||
| Mothers reading newspapers | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.17 (0.91, 1.52) | 0.220 | 0.87 (0.53, 1.43) | 0.585 | ||||
| Mothers listening to radio | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.10 (0.79, 1.54) | 0.571 | 1.13 (0.60, 2.12) | 0.698 | ||||
| Mothers watching television | ||||||||
| Not at all | 1.00 | 1.00 | ||||||
| Yes/some ^ | 1.49 (1.18, 1.88) | <0.001 | 1.47 (0.93, 2.31) | 0.099 | ||||
| Power over household decision making | ||||||||
| Husband | 1.00 | 1.00 | ||||||
| Woman alone | 1.21 (0.82, 1.78) | 0.343 | 1.42 (0.79, 2.56) | 0.247 | ||||
| Power over earning | ||||||||
| Husband | 1.00 | 1.00 | ||||||
| Woman alone | 1.18 (0.74, 1.87) | 0.485 | 0.91 (0.49, 1.69) | 0.763 | ||||
| Father’s occupation | ||||||||
| Nonagricultural | 1.00 | 1.00 | ||||||
| Agricultural | 0.57 (0.32, 1.03) | 0.061 | 0.48 (0.18, 1.24) | 0.128 | ||||
| Not working | 0.75 (0.49, 1.16) | 0.198 | 0.78 (0.40, 1.50) | 0.449 | ||||
| Birth order | ||||||||
| 1st born | 1.00 | 1.00 | ||||||
| 2nd–4th | 0.83 (0.60, 1.14) | 0.247 | 0.64 (0.31, 1.35) | 0.243 | ||||
| Preceding birth interval | ||||||||
| No previous birth | 1.00 | 1.00 | ||||||
| Yes | 0.80 (0.58, 1.12) | 0.194 | 0.67 (0.32, 1.41) | 0.292 | ||||
| Sex of baby | ||||||||
| Male | 1.00 | 1.00 | ||||||
| Female | 0.97 (0.76, 1.22) | 0.770 | 1.11 (0.73, 1.70) | 0.597 | ||||
| Age of child (months) | ||||||||
| 6–11 | 1.00 | 1.00 | ||||||
| 12–17 | 0.86 (0.63, 1.18) | 0.350 | 0.29 (0.16, 0.51) | <0.001 | ||||
| 18–23 | 0.94 (0.69, 1.28) | 0.696 | 0.69 (0.43, 1.12) | 0.134 | ||||
| Low Birth Weight (<2500 g) | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 0.62 (0.45, 0.86) | <0.001 | 1.06 (0.58, 1.93) | 0.854 | ||||
| Size of the baby | ||||||||
| Small | 1.00 | 1.00 | ||||||
| Average | 0.86 (0.63, 1.18) | 0.342 | 0.51 (0.29, 0.91) | 0.022 | ||||
| Large | 0.95 (0.64, 1.42) | 0.818 | 0.66 (0.33, 1.31) | 0.234 | ||||
| Children who had diarrhea recently | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 1.15 (0.86, 1.54) | 0.362 | 1.06 (0.58, 1.93) | 0.854 | ||||
| Children with acute respiratory infection treatment | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 0.78 (0.50, 1.23) | 0.289 | 0.70 (0.26, 1.91) | 0.489 | ||||
| Children who had fever in last 2 weeks | ||||||||
| No | 1.00 | 1.00 | ||||||
| Yes | 0.96 (0.72, 1.28) | 0.782 | 1.21 (0.72, 2.02) | 0.471 | ||||
| Household-level factors | ||||||||
| Wealth index | ||||||||
| Poor | 1.00 | 1.00 | ||||||
| Middle | 1.19 (0.88, 1.61) | 0.254 | 0.87 (0.52, 1.47) | 0.609 | ||||
| Rich | 0.92 (0.67, 1.27) | 0.610 | 0.84 (0.47, 1.52) | 0.570 | ||||
| Number of living children | ||||||||
| 1 | 1.00 | 1.00 | ||||||
| 2 to 3 | 0.80 (0.57, 1.14) | 0.220 | 0.70 (0.32, 1.55) | 0.381 | ||||
| Source of drinking water | ||||||||
| Improved | 1.00 | 1.00 | ||||||
| Unimproved | 1.20 (0.91, 1.58) | 0.195 | 0.84 (0.47, 1.52) | 0.567 | ||||
| Type of toilet facility | ||||||||
| Improved | 1.00 | 1.00 | ||||||
| Unimproved | 0.99 (0.77, 1.28) | 0.962 | 0.92 (0.60, 1.42) | 0.712 | ||||
| Community-level factors | ||||||||
| Residence | ||||||||
| Urban | 1.00 | 1.00 | ||||||
| Rural | 0.98 (0.68, 1.42) | 0.922 | 1.63 (0.89, 2.98) | 0.112 | ||||
| Geographical Region | ||||||||
| North | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| South | 1.48 (0.93, 2.34) | 0.090 | 1.45 (0.91, 2.32) | 0.111 | 3.53 (1.46, 8.56) | 0.005 | 3.14 (1.28, 7.68) | 0.012 |
| East | 1.64 (1.12, 2.40) | 0.010 | 1.69 (1.15, 2.48) | 0.007 | 3.70 (1.63, 8.37) | 0.002 | 3.56 (1.57, 8.07) | 0.002 |
| West | 1.43 (0.83, 2.46) | 0.196 | 1.39 (0.81, 2.38) | 0.223 | 1.10 (0.38, 3.23) | 0.850 | 1.02 (0.34, 3.09) | 0.962 |
| Central | 2.02 (1.38, 2.96) | <0.001 | 2.00 (1.36, 2.94) | <0.001 | 1.89 (0.80, 4.46) | 0.141 | 1.86 (0.78, 4.39) | 0.156 |
| Northeast | 1.37 (0.90, 2.10) | 0.140 | 1.39 (0.89, 2.18) | 0.145 | 3.16 (1.33, 7.52) | 0.009 | 3.18 (1.30, 7.76) | 0.011 |
| Type of caste or tribe | ||||||||
| Schedule caste | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Schedule tribe | 1.08 (0.75, 1.54) | 0.673 | 1.14 (0.79, 1.64) | 0.471 | 0.58 (0.31, 1.06) | 0.078 | 0.74 (0.40, 1.37) | 0.344 |
| Other backward caste | 0.73 (0.54, 0.98) | 0.036 | 0.73 (0.54, 0.98) | 0.037 | 0.52 (0.31, 0.88) | 0.015 | 0.53 (0.31, 0.89) | 0.017 |
| Other * | 0.73 (0.50, 1.08) | 0.118 | 0.75 (0.51, 1.10) | 0.148 | 0.54 (0.28, 1.03) | 0.062 | 0.54 (0.27, 1.07) | 0.082 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhami, M.V.; Ogbo, F.A.; Diallo, T.M.O.; Olusanya, B.O.; Goson, P.C.; Agho, K.E.; on behalf of the Global Maternal and Child Health Research Collaboration (GloMACH). Infant and Young Child Feeding Practices among Adolescent Mothers and Associated Factors in India. Nutrients 2021, 13, 2376. https://doi.org/10.3390/nu13072376
Dhami MV, Ogbo FA, Diallo TMO, Olusanya BO, Goson PC, Agho KE, on behalf of the Global Maternal and Child Health Research Collaboration (GloMACH). Infant and Young Child Feeding Practices among Adolescent Mothers and Associated Factors in India. Nutrients. 2021; 13(7):2376. https://doi.org/10.3390/nu13072376
Chicago/Turabian StyleDhami, Mansi Vijaybhai, Felix Akpojene Ogbo, Thierno M. O. Diallo, Bolajoko O. Olusanya, Piwuna Christopher Goson, Kingsley Emwinyore Agho, and on behalf of the Global Maternal and Child Health Research Collaboration (GloMACH). 2021. "Infant and Young Child Feeding Practices among Adolescent Mothers and Associated Factors in India" Nutrients 13, no. 7: 2376. https://doi.org/10.3390/nu13072376
APA StyleDhami, M. V., Ogbo, F. A., Diallo, T. M. O., Olusanya, B. O., Goson, P. C., Agho, K. E., & on behalf of the Global Maternal and Child Health Research Collaboration (GloMACH). (2021). Infant and Young Child Feeding Practices among Adolescent Mothers and Associated Factors in India. Nutrients, 13(7), 2376. https://doi.org/10.3390/nu13072376






