Individual Diet Modification Reduces the Metabolic Syndrome in Patients Before Pharmacological Treatment
Abstract
1. Introduction
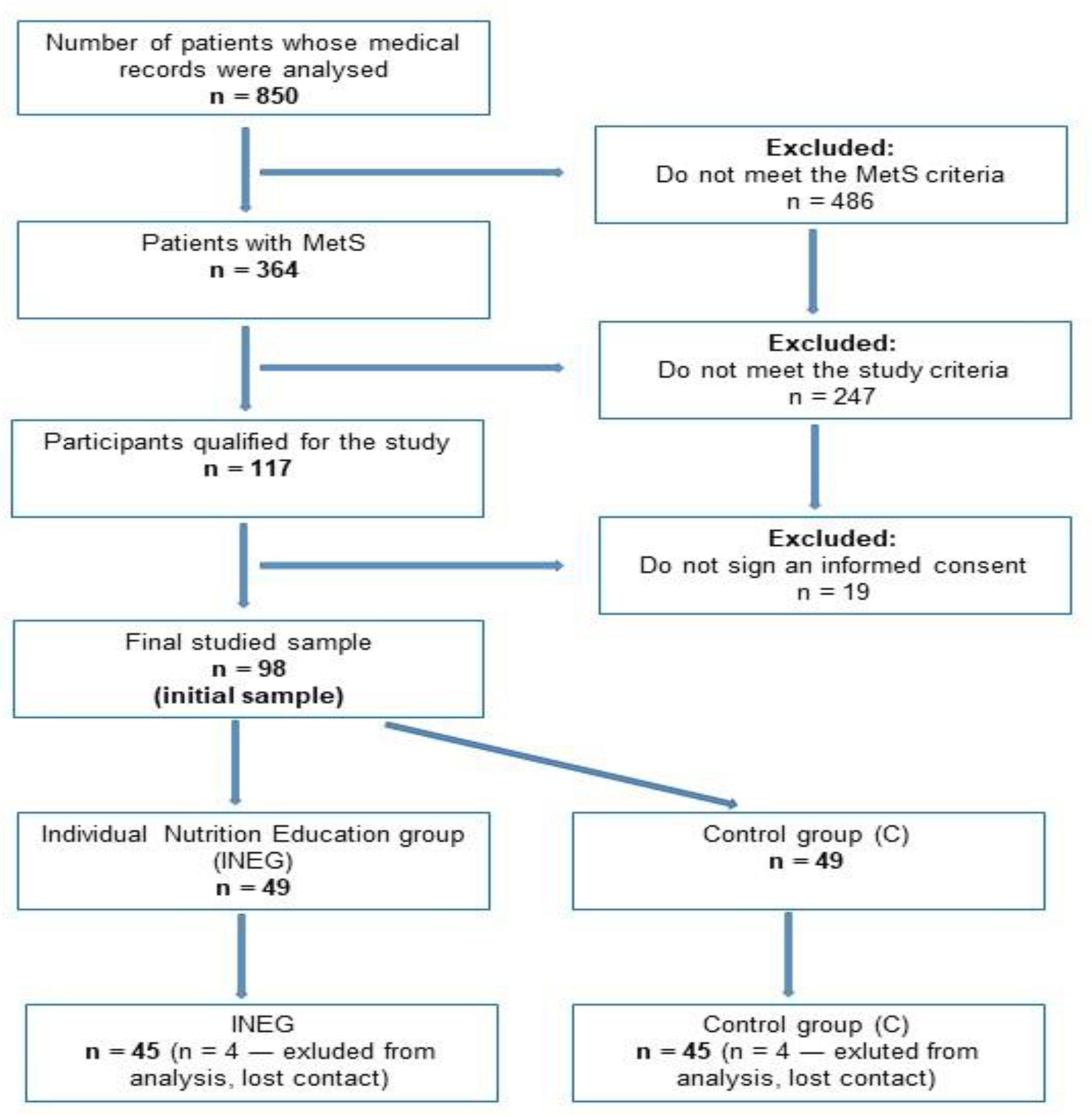
2. Materials and Methods
2.1. Ethical Approval
2.2. Subject Characteristics and Study Design
2.3. Sociodemographic and Physical Activity Information
2.4. Dietary Assessment
2.5. Clinical Measurements
2.6. Intervention
2.7. Statistical Analysis
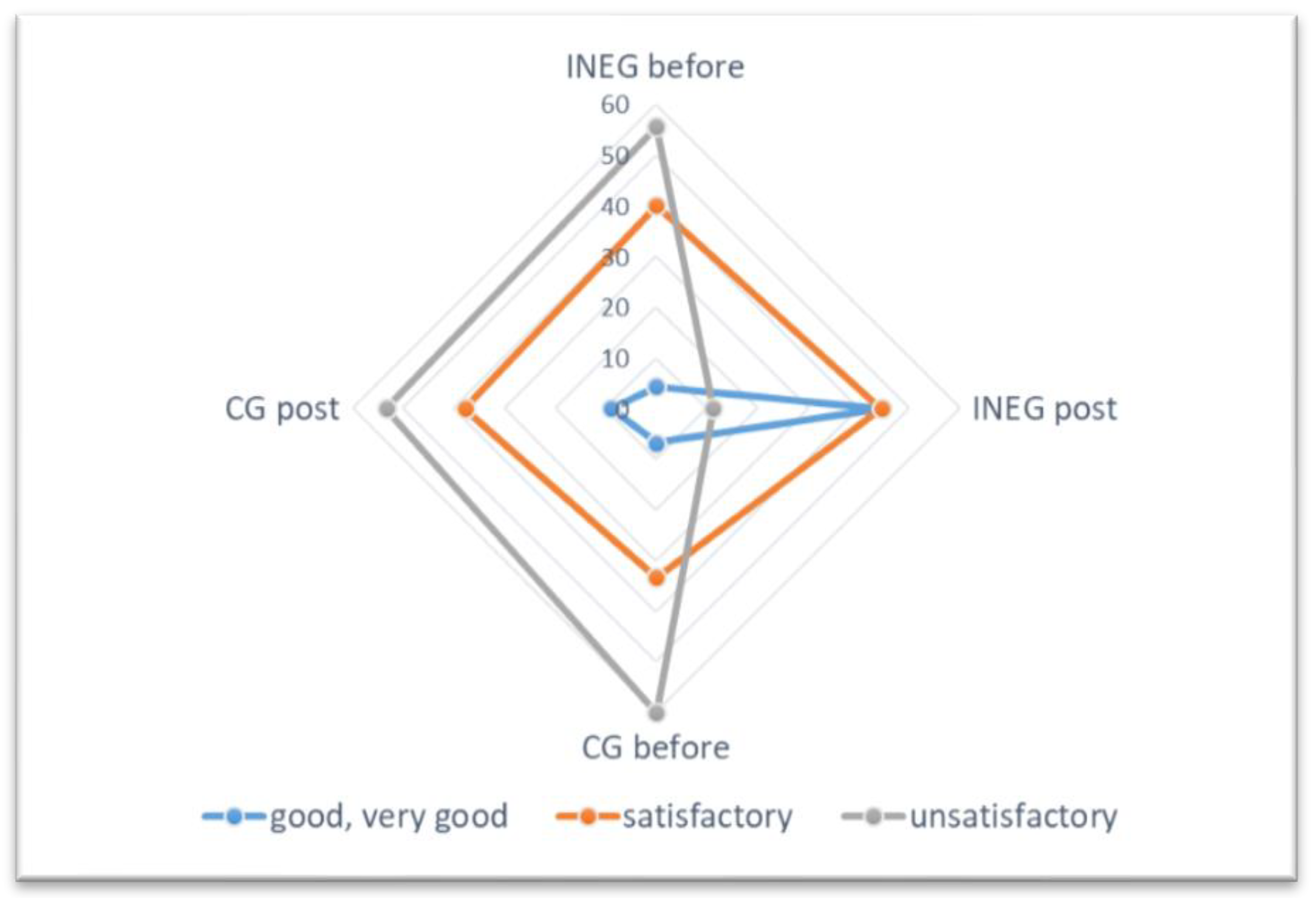
3. Results
4. Discussions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome. A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Saklayen, M.G. The global epidemic of the metabolic syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed]
- Gurka, M.J.; Filipp, S.L.; DeBoer, M.D. Geographical variation in the prevalence of obesity, metabolic syndrome, and diabetes among US adults. Nutr. Diabetes 2018, 8, 14. [Google Scholar] [CrossRef]
- Scuteri, A.; Laurent, S.; Cucca, F.; Cockcroft, J.; Cunha, P.G.; Mañas, L.R.; Mattace Raso, F.U.; Muiesan, M.L.; Ryliškytė, L.; Rietzschel, E.; et al. Metabolic Syndrome and Arteries Research (MARE) Consortium. Metabolic syndrome across Europe: Different clusters of risk factors. Eur. J. Prev. Cardiol. 2015, 22, 486–491. [Google Scholar] [CrossRef]
- Zujko, M.E.; Waśkiewicz, A.; Witkowska, A.M.; Szcześniewska, D.; Zdrojewski, T.; Kozakiewicz, K.; Drygas, W. Dietary total antioxidant capacity and dietary polyphenol intake and prevalence of metabolic syndrome in Polish adults: A nationwide study. Oxid. Med. Cell. Longev. 2018, 2018, 7487816. [Google Scholar] [CrossRef]
- Mirmiran, P.; Ziadlou, M.; Karimi, S.; Hosseini-Esfahani, F.; Azizi, F. The association of dietary patterns and adherence to WHO healthy diet with metabolic syndrome in children and adolescents: Tehran lipid and glucose study. BMC Public Health 2019, 19, 1457. [Google Scholar] [CrossRef]
- Fabiani, R.; Naldini, G.; Chiavarini, M. Dietary patterns and metabolic syndrome in adult subjects: A systematic review and meta-analysis. Nutrients 2019, 11, 2056. [Google Scholar] [CrossRef]
- Wei, Z.Y.; Liu, J.J.; Zhan, X.M.; Feng, H.M.; Zhang, Y.Y. Dietary patterns and the risk of metabolic syndrome in Chinese adults: A population-based cross-sectional study. Public Health Nutr. 2018, 21, 2409–2416. [Google Scholar] [CrossRef]
- Liu, K.; Luo, M.; Wei, S. The bioprotective effects of polyphenols on metabolic syndrome against oxidative stress: Evidences and perspectives. Oxid. Med. Cell. Longev. 2019, 2019, 6713194. [Google Scholar] [CrossRef] [PubMed]
- Bub, A.; Malpuech-Brugère, C.; Orfila, C.; Amat, J.; Arianna, A.; Blot, A.; Di Nunzio, M.; Holmes, M.; Kertész, Z.; Marshal, L.; et al. A dietary intervention of bioactive enriched foods aimed at adults at risk of metabolic syndrome: Protocol and results from PATHWAY-27 Pilot Study. Nutrients 2019, 11, 1814. [Google Scholar] [CrossRef] [PubMed]
- Del Rio, D.; Rodriguez-Mateos, A.; Spencer, J.P.E.; Tognolini, M.; Borges, G.; Crozier, A. Dietary (poly)phenolics in human health: Structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxid. Redox Signal. 2013, 18, 1818–1892. [Google Scholar] [CrossRef]
- Chiva-Blanch, G.; Urpi-Sarda, M.; Ros, E.; Valderas-Martinez, P.; Casas, R.; Arranz, S.; Guillén, M.; Lamuela-Raventós, R.M.; Llorach, R.; Andres-Lacueva, C.; et al. Effects of red wine polyphenols and alcohol on glucose metabolism and the lipid profile: A randomized clinical trial. Clin. Nutr. 2013, 32, 200–206. [Google Scholar] [CrossRef]
- Chen, S.; Zhao, X.; Ran, L.; Wan, J.; Wang, X.; Qin, Y.; Shu, F.; Gao, Y.; Yuan, L.; Zhang, Q.; et al. Resveratrol improves insulin resistance, glucose and lipid metabolism in patients with non-alcoholic fatty liver disease: A randomized controlled trial. Dig. Liver Dis. 2015, 47, 226–232. [Google Scholar] [CrossRef]
- Martínez-Maqueda, D.; Zapatera, B.; Gallego-Narbón, A.; Vaquero, M.P.; Saura-Calixto, F.; Pérez-Jiménez, J. A 6-week supplementation with grape pomace to subjects at cardiometabolic risk ameliorates insulin sensitivity, without affecting other metabolic syndrome markers. Food Funct. 2018, 9, 6010–6019. [Google Scholar] [CrossRef]
- Tynkkynen, T.; Mursu, J.; Nurmi, T.; Tuppurainen, K.; Laatikainen, R.; Soininen, P. NMR protocol for determination of oxidation susceptibility of serum lipids and application of the protocol to a chocolate study. Metabolomics 2012, 8, 386–398. [Google Scholar] [CrossRef]
- Rangel-Huerta, O.D.; Aguilera, C.M.; Martin, M.V.; Soto, M.J.; Rico, M.C.; Vallejo, F.; Tomas-Barberan, F.; Perez-de-la-Cruz, A.J.; Gil, A.; Mesa, M.D. Normal or high polyphenol concentration in orange juice affects antioxidant activity, blood pressure, and body weight in obese or overweight adults. J. Nutr. 2015, 145, 1808–1816. [Google Scholar] [CrossRef]
- Chai, S.C.; Davis, K.; Wright, R.S.; Kuczmarski, M.F.; Zhang, Z. Impact of tart cherry juice on systolic blood pressure and low-density lipoprotein cholesterol in older adults: A randomized controlled trial. Food Funct. 2018, 9, 3185–3194. [Google Scholar] [CrossRef]
- Janssens, L.H.R.; Hursel, R.; Westerterp-Plantenga, M.S. Long-term green tea extract supplementation does not affect fat absorption, resting energy expenditure, and body composition in adults. J. Nutr. 2015, 145, 864–870. [Google Scholar] [CrossRef]
- Fang, C.; Kim, H.; Barnes, R.C.; Talcott, S.T.; Mertens-Talcott, S.U. Obesity-associated diseases biomarkers are differently modulated in lean and obese individuals and inversely correlated to plasma polyphenolic metabolites after 6 weeks of mango (mangifera indica L.) consumption. Mol. Nutr. Food Res. 2018, 62, 1800129. [Google Scholar] [CrossRef]
- Rienks, J.; Barbaresko, J.; Oluwagbemigun, K.; Schmid, M.; Nöthlings, U. Polyphenol exposure and risk of type 2 diabetes: Dose-response meta-analyses and systematic review of prospective cohort studies. Am. J. Clin. Nutr. 2018, 108, 49–61. [Google Scholar] [CrossRef]
- Del Bo’, C.; Bernardi, S.; Marino, M.; Porrini, M.; Tucci, M.; Guglielmetti, S.; Cherubini, A.; Carrieri, B.; Kirkup, B.; Kroon, P.; et al. Systematic review on polyphenol intake and health outcomes: Is there sufficient evidence to define a health-promoting polyphenol-rich dietary pattern? Nutrients 2019, 11, 1355. [Google Scholar]
- WHO. Healthy Diet. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 3 March 2020).
- Biernat, E.; Stupnicki, R.; Gajewski, A.K. Międzynarodowy Kwestionariusz Aktywności Fizycznej (IPAQ)—Wersja Polska [International Physical Activity Questionnaire (IPAQ)—Polish Version]. Wychow. Fiz. Sport [Phys. Educ. Sport] 2007, 51, 47–54. (In Polish) [Google Scholar]
- Szponar, L.; Wolnicka, K.; Rychlik, E. Album Fotografii Produktów i Potraw [Album of Photographs of Food Products and Dishes]; Wydawnictwo Instytut Żywności i Żywienia [National Food and Nutrition Institute Press]: Warsaw, Poland, 2000. (In Polish) [Google Scholar]
- Gawęcki, J. (Ed.) Kwestionariusz do Badania Poglądów i Zwyczajów Żywieniowych oraz Procedura Opracowania Danych [Beliefs and Eating Habits Questionnaire and Data Processing Procedure]. Available online: http://www.medprew.cm-uj.krakow.pl/doku/kwestionariusz_kompan2016.pdf (accessed on 16 September 2020). (In Polish).
- Witkowska, A.M.; Waśkiewicz, A.; Zujko, M.E.; Szcześniewska, D.; Pająk, A.; Stepaniak, U.; Drygas, W. Dietary polyphenol intake, but not the dietary total antioxidant capacity, is inversely related to cardiovascular disease in postmenopausal Polish women: Results of WOBASZ and WOBASZ II Studies. Oxid. Med. Cell. Longev. 2017, 2017, 5982809. [Google Scholar] [CrossRef] [PubMed]
- Neveu, V.; Perez-Jiménez, J.; Vos, F. Phenol-Explorer: An online comprehensive database on polyphenol contents in foods. J. Biol. Databases Curation 2010, 2010, bap024. Available online: http://www.phenol-explorer.eu (accessed on 12 June 2021). [CrossRef] [PubMed]
- WHO. Body Mass Index—BMI. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 11 September 2020).
- Evert, A.B.; Dennison, M.; Gardner, C.D.; Garvey, W.T.; Lau, K.H.K.; MacLeod, J.; Mitri, J.; Pereira, R.F.; Rawlings, K.; Robinsonet, S.; et al. Nutrition therapy for adults with diabetes or prediabetes: A consensus report. Diabetes Care 2019, 42, 731–754. [Google Scholar] [CrossRef]
- Horn, L.V.; Carson, J.A.S.; Appel, L.J.; Burke, L.E.; Economos, C.; Karmally, W.; Lancaster, K.; Lichtenstein, A.H.; Johnson, R.K.; Thomas, R.J.; et al. Recommended dietary pattern to achieve adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: A scientific statement from the American Heart Association. Circulation 2016, 134, e505–e529. [Google Scholar] [CrossRef]
- Piramida Zdrowego Żywienia i Aktywności Fizycznej [Pyramid of Healthy Eating and Physical Activity for the Polish Population]; Instytut Żywności i Żywienia [National Institute of Food and Nutrition]: Warsaw, Poland 2016. Available online: http://www.izz.waw.pl/zasady-prawidowego-ywienia (accessed on 15 February 2021). (In Polish).
- Jarosz, M.; Rychlik, E.; Stoś, K.; Charzewska, J. (Eds.) Normy Żywienia dla Populacji Polski i ich Zastosowanie [Nutrition Standards for the Polish Population and Their Application]; Narodowy Instytut Zdrowia Publicznego-Państwowy Zakład Higieny [National Institute of Public Health-State Department of Hygiene]: Warsaw, Poland, 2020. Available online: https://www.pzh.gov.pl/wp-content/uploads/2020/12/Normy_zywienia_2020web-1.pdf (accessed on 5 March 2021). (In Polish)
- Zujko, M.E.; Witkowska, A.M. Antioxidant potential and polyphenol content of selected food. Int. J. Food Prop. 2011, 14, 300–308. [Google Scholar] [CrossRef]
- Zujko, M.E.; Witkowska, A.M. Antioxidant potential and polyphenol content of beverages, chocolates, nuts, and seeds. Int. J. Food Prop. 2014, 17, 86–92. [Google Scholar] [CrossRef]
- Alzaben, A.S.; Alnashwan, N.I.; Alatr, A.A.; Alneghamshi, N.A.; Alhashem, A.M. Effectiveness of a nutrition education and intervention programme on nutrition knowledge and dietary practice among Princess Nourah Bint Abdulrahman University’s population. Public Health Nutr. 2021, 24, 1854–1860. [Google Scholar] [CrossRef]
- Sunuwar, D.R.; Sangroula, R.K.; Shakya, N.S.; Yadav, R.; Chaudhary, N.K.; Pradhan, P.M.S. Effect of nutrition education on hemoglobin level in pregnant women: A quasi-experimental study. PLoS ONE 2019, 14, e0213982. [Google Scholar] [CrossRef]
- Franz, M.J.; Boucher, J.L.; Evert, A.B. Evidence-based diabetes nutrition therapy recommendations are effective: The key is individualization. Diabetes Metab. Syndr. Obes. 2014, 7, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Visioli, F.; Poli, A. Fatty acids and cardiovascular risk. Evidence, lack of evidence, and diligence. Nutrients 2020, 12, 3782. [Google Scholar] [CrossRef]
- De Oliveira Otto, M.C.; Mozaffarian, D.; Kromhout, D.; Bertoni, A.G.; Sibley, C.T.; Jacobs, D.R., Jr.; Nettleton, J.A. Dietary intake of saturated fat by food source and incident cardiovascular disease: The Multi-Ethnic Study of Atherosclerosis. Am. J. Clin. Nutr. 2012, 96, 397–404. [Google Scholar] [CrossRef]
- Soliman, G.A. Dietary cholesterol and the lack of evidence in cardiovascular disease. Nutrients 2018, 10, 780. [Google Scholar] [CrossRef]
- Akhlaghi, M. Dietary Approaches to Stop Hypertension (DASH): Potential mechanisms of action against risk factors of the metabolic syndrome. Nutr. Res. Rev. 2020, 33, 1–18. [Google Scholar] [CrossRef]
- Castro-Barquero, S.; Ruiz-León, A.M.; Sierra-Pérez, M.; Estruch, R.; Casas, R. Dietary strategies for metabolic syndrome: A comprehensive review. Nutrients 2020, 12, 2983. [Google Scholar] [CrossRef]
- Thuita, A.W.; Kiage, B.N.; Onyango, A.N.; Makokha, A.O. Effect of a nutrition education programme on the metabolic syndrome in type 2 diabetes mellitus patients at a level 5 Hospital in Kenya: “a randomized controlled trial”. BMC Nutr. 2020, 6, 30. [Google Scholar] [CrossRef]
- Kim, J.; Bea, W.; Lee, K.; Han, J.; Kim, S.; Kim, M.; Na, W.; Sohn, C. Effect of the telephone-delivered nutrition education on dietary intake and biochemical parameters in subjects with metabolic syndrome. Clin. Nutr. Res. 2013, 2, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Castro-Barquero, S.; Tresserra-Rimbau, A.; Vitelli-Storelli, F.; Doménech, M.; Salas-Salvadó, J.; Martín-Sánchez, V.; Rubín-García, M.; Buil-Cosiales, P.; Corella, D.; Fitó, M. Dietary polyphenol intake is associated with HDL-cholesterol and a better profile of other components of the metabolic syndrome: A PREDIMED-Plus Sub-Study. Nutrients 2020, 12, 689. [Google Scholar] [CrossRef]
- Grosso, G.; Stepaniak, U.; Micek, A.; Kozela, M.; Stefler, D.; Bobak, M.; Pająk, A. Dietary polyphenol intake and risk of type 2 diabetes in the Polish arm of the Health, Alcohol and Psychosocial factors in Eastern Europe (HAPIEE) study. Br. J. Nutr. 2017, 118, 60–68. [Google Scholar] [CrossRef]
- Chiva-Blanch, G.; Badimon, L. Effects of polyphenol intake on metabolic syndrome: Current evidences from human trials. Oxid. Med. Cell. Longev. 2017, 2017, 5812401. [Google Scholar] [CrossRef]
- Chen, J.P.; Chen, G.C.; Wang, X.P.; Qin, L.; Bai, Y. Dietary fiber and metabolic syndrome: A meta-analysis and review of related mechanisms. Nutrients 2018, 10, 24. [Google Scholar] [CrossRef]
- Zibaeenezhad, M.J.; Ghavipisheh, M.; Attar, A.; Aslani, A. Comparison of the effect of omega-3 supplements and fresh fish on lipid profile: A randomized, open-labeled trial. Nutr. Diabetes 2017, 7, 1. [Google Scholar] [CrossRef]
- Kunduraci, Y.E.; Ozbek, H. Does the energy restriction intermittent fasting diet alleviate metabolic syndrome biomarkers? A randomized controlled trial. Nutrients 2020, 12, 3213. [Google Scholar] [CrossRef]
- Sorić, T.; Mavar, M.; Rumbak, I. The effects of the dietary approaches to stop hypertension (DASH) diet on metabolic syndrome in hospitalized schizophrenic patients: A randomized controlled trial. Nutrients 2019, 11, 2950. [Google Scholar] [CrossRef]
- Tovar, J.; Johansson, M.; Björck, I. A multifunctional diet improves cardiometabolic-related biomarkers independently of weight changes: An 8-week randomized controlled intervention in healthy overweight and obese subjects. Eur. J. Nutr. 2016, 55, 2295–2306. [Google Scholar] [CrossRef]

| Dietary Components | Recommended Intake |
|---|---|
| Energy 1 | 1500–2500 kcal |
| Protein | 20–25% of total energy |
| Fat | 25–35% of total energy |
| Carbohydrates | 45–50% of total energy |
| SFA | <7% of total energy |
| MUFA | 15–20% of total energy |
| PUFA | 6–10% of total energy |
| Cholesterol | <200 mg/day |
| Sodium | 1500 mg/day |
| Fiber | ≥25 g/day |
| Fruits and vegetables (without potatoes) | ≥5 servings (500 g/day; 1/4 fruits, 3/4 vegetables) |
| Fish | ≥2 servings/week (1 serving—150 g prepared for consumption) |
| Legumes | ≥2 servings/week (1 serving—40–60 g dry) |
| Unsalted nuts and seeds | ≥3–4 servings/week (1 serving—30–50 g) |
| Low-glycemic-index foods | GI < 55 |
| Wholegrain cereal products | 5 servings/day (1 serving—30 g bread or 30 g groats or pasta before cooking) |
| Meat | 3 servings/week (1 serving—100–120 g prepared for consumption, preference for poultry > red meats) |
| Low-fat dairy products | 3 servings/day (1 serving—200 mL of milk, 150 g yogurt or kefir, 35 g cottage cheese) |
| Oil (olive oils, linseed oil, rapeseed oil) | ≥4 servings/ day (1 serving—1 tablespoon) |
| Eggs | 4–5/week |
| Water | 1.5–2 L/day |
| Polyphenol-rich foods | walnuts, sunflower seeds, raspberries, cranberries, blueberries, strawberries, beetroot, red cabbage |
| Sweet, cakes | not recommended |
| Average caloric distribution of meals | breakfast—25–30%, morning snack—5–10%, lunch—35–40%, afternoon snack—5–10%,dinner—15–20% |
| Frequency of eating meals | every 3–4 h |
| Variable | INEG | CG | p-Value |
|---|---|---|---|
| Age (years), mean ± SD | 45.5 ± 7.5 | 46.8 ± 10.7 | 0.415 |
| Gender, N (%) | |||
| women | 25 (55.0) | 24 (53.0) | 0.865 |
| men | 20 (45.0) | 21 (47.0) | |
| Education level, N (%) | |||
| high | 16 (35.6) | 18 (40.0) | 0.564 |
| middle | 23 (51.1) | 22 (48.9) | |
| under middle | 6 (13.3) | 5 (11.1) | |
| Working status, N (%) | |||
| currently working | 35 (77.8) | 33 (73.3) | 0.486 |
| Marital status, N (%) | |||
| married | 38 (84.4) | 34 (75.6) | 0.263 |
| single | 7 (15.6) | 11 (24.4) | |
| Physical activity, N (%) | |||
| high | 0 (0.0) | 0 (0.0) | 0.543 |
| moderate | 17 (37.8) | 15 (33.3) | |
| low | 28 (62.2) | 30 (66.7) | |
| Smoking status, N (%) | |||
| currently smoking | 10 (22.2) | 9 (20.0) | 0.496 |
| Nutritional knowledge, N (%) | |||
| Good, very good | 2 (4.4) | 3 (6.7) | 0.658 |
| satisfactory | 18 (40.0) | 15 (33.3) | |
| unsatisfactory | 25 (55.6) | 27 (60.0) | |
| Parameter | Before Intervention | Post Intervention | P 3 | P 4 | ||||
|---|---|---|---|---|---|---|---|---|
| INEG | CG | P 1 | INEG | CG | P 2 | |||
| Energy (kcal) | 2612.2 ± 345.8 | 2767.5 ± 376.3 | 0.564 | 2341.4 ± 437.3 | 2565 ± 374.9 | 0.256 | 0.324 | 0.385 |
| Protein (% energy) | 22.8 ± 7.4 | 20.6 ± 6.2 | 0.365 | 18.8 ± 8.7 | 20.3 ± 7.3 | 0.244 | 0.312 | 0.454 |
| Fat (% energy) | 34.5 ± 8.6 | 32.8 ± 9.5 | 0.465 | 31.2 ± 7.4 | 33.5 ± 6.9 | 0.157 | 0.487 | 0.515 |
| SFA (% energy) | 21.1 ± 12.5 | 19.2 ± 14.2 | 0.287 | 7.5 ± 5.4 | 16.7 ± 8.9 | 0.001 | 0.001 | 0.211 |
| MUFA (% energy) | 7.5 ± 4.6 | 8.1 ± 5.9 | 0.322 | 15.6 ± 7.1 | 8.5 ± 6.8 | 0.009 | 0.001 | 0.458 |
| PUFA (% energy) | 8.6 ± 5.9 | 7.7 ± 5.3 | 0.255 | 10.5 ± 5.9 | 8.1 ± 4.3 | 0.025 | 0.035 | 0.288 |
| PUFA n-6:n-3 | 15:1 | 13:1 | 0.432 | 3:1 | 12:1 | 0.001 | 0.001 | 0.545 |
| Cholesterol (mg) | 444.1 ± 164.5 | 428.7 ± 148.7 | 0.195 | 256.4 ± 95.8 | 412.9 ± 126.4 | 0.001 | 0.009 | 0.234 |
| Fiber (g) | 15.6 ± 9.1 | 12.8 ± 10.4 | 0.255 | 27.4 ± 9.4 | 14.8 ± 10.7 | 0.001 | 0.008 | 0.195 |
| Sodium (mg) | 3150.4 ± 483.1 | 2923.5 ± 594.7 | 0.452 | 1785.2 ± 246.4 | 3150.4 ± 483.1 | 0.001 | 0.001 | 0.654 |
| Magnesium (mg) | 265.1 ± 115.4 | 286 ± 145.7 | 0.544 | 405.1 ± 215.4 | 304.2 ± 162.4 | 0.012 | 0.009 | 0.216 |
| Calcium (mg) | 822.4 ± 255.3 | 857.5 ± 247.2 | 0.456 | 951.3 ± 295.6 | 874.2 ± 264.4 | 0.065 | 0.086 | 0.451 |
| Vitamin C (mg) | 47.2 ± 25.4 | 41.9 ± 36.5 | 0.623 | 96.3 ± 36.5 | 52.4 ± 26.8 | 0.011 | 0.008 | 0.112 |
| Vitamin A (µg) | 825.8 ± 395.6 | 860.5 ± 412.3 | 0.235 | 850.6 ± 435.9 | 920.2 ± 571.6 | 0.134 | 0.312 | 0.298 |
| Vitamin E (mg) | 8.4 ± 3.2 | 7.2 ± 4.5 | 0.185 | 10.8 ± 4.8 | 8.5 ± 5.3 | 0.095 | 0.213 | 0.317 |
| Vitamin B6 (mg) | 1.5 ± 0.8 | 1.7 ± 0.5 | 0.115 | 1.8 ± 0.9 | 1.6 ± 0.6 | 0.115 | 0.244 | 0.367 |
| Vitamin B12 (µg) | 1.8 ± 1.1 | 2.0 ± 1.5 | 0.145 | 2.4 ± 1.8 | 2.1 ± 1.6 | 0.075 | 0.185 | 0.412 |
| Folate (µg) | 287.4 ± 144.5 | 311.5 ± 133.6 | 0.365 | 335.7 ± 214.5 | 295.2 ± 186.4 | 0.088 | 0.117 | 0.311 |
| Polyphenols (mg) | 1531.2 ± 481.5 | 1618.8 ± 511.6 | 0.186 | 2089.6 ± 764.5 | 1654.3 ± 543.2 | 0.001 | 0.001 | 0.468 |
| Flavonoids | 801.5 ± 387.3 | 780.2 ± 432.9 | 0.468 | 1125.8 ± 236.4 | 802.3 ± 452.1 | 0.008 | 0.011 | 0.345 |
| flavanols | 551.3 ± 295.9 | 531.6 ± 323.4 | 0.385 | 725.7 ± 195.8 | 553.6 ± 330.8 | 0.015 | 0.009 | 0.435 |
| flavonols | 91.4 ± 78.9 | 85.4 ± 85.3 | 0.411 | 108.7 ± 59.5 | 92.7 ± 75.8 | 0.114 | 0.098 | 0.105 |
| flavanones | 83.3 ± 72.7 | 79.8 ± 69.9 | 0.454 | 96.9 ± 55.2 | 82.9 ± 65.4 | 0.232 | 0.118 | 0.411 |
| flavones | 16.8 ± 11.8 | 15.7 ± 12.2 | 0.623 | 18.4 ± 8.5 | 16.6 ± 10.5 | 0.375 | 0.285 | 0.387 |
| anthocyanins | 31.8 ± 56.7 | 29.6 ± 42.4 | 0.585 | 105.7 ± 35.8 | 26.8 ± 54.2 | 0.001 | 0.001 | 0.395 |
| isoflavones | 2.1 ± 0.5 | 1.8 ± 0.7 | 0.314 | 2.9 ± 0.6 | 2.2 ± 0.9 | 0.354 | 0.323 | 0.423 |
| Phenolic acids | 695.5 ± 322.6 | 798.4 ± 345.2 | 0.285 | 896,7 ± 216.4 | 810.7 ± 314.8 | 0.087 | 0.045 | 0.564 |
| hydroxybenzoic | 85.2 ± 78.4 | 89.5 ± 80.8 | 0.456 | 95.7 ± 63.9 | 91.4 ± 82.1 | 0.245 | 0.115 | 0.476 |
| hydroxycinnamic | 602.4 ± 356.3 | 684.9 ± 423.7 | 0.325 | 784.6 ± 276.5 | 704.9 ± 388.5 | 0.312 | 0.095 | 0.392 |
| Stilbenes | 0.2 ± 0.8 | 0.2 ± 1.1 | 0.786 | 0.3 ± 0.5 | 0.2 ± 0.9 | 0.236 | 0.163 | 0.485 |
| Lignans | 0.5 ± 9.5 | 0.5 ± 10.2 | 0.644 | 0.6 ± 7.4 | 0.5 ± 9.7 | 0.354 | 0.322 | 0.678 |
| Parameter | Before Intervention | Post Intervention | P 3 | P 4 | ||||
|---|---|---|---|---|---|---|---|---|
| INEG | CG | P1 | INEG | CG | P2 | |||
| Weight (kg) | 97.6 ± 34.3 | 91.2 ± 29.2 | 0.155 | 82.5 ± 21.3 | 93.4 ± 31.7 | 0.011 | 0.025 | 0.356 |
| BMI (kg/m2) | 32.6 ± 12.2 | 30.2 ± 11.5 | 0.245 | 27.5 ± 5.4 | 29.4 ± 9.5 | 0.021 | 0.009 | 0.411 |
| WC (cm) | 105.3 ± 18.6 | 108.5 ± 15.8 | 0.432 | 91.1 ± 14.4 | 108.3 ± 18.6 | 0.009 | 0.015 | 0.455 |
| MM (kg) | 35.2 ± 7.2 | 34.1 ± 8.8 | 0.156 | 33.9 ± 9.5 | 32.7 ± 7.9 | 0.234 | 0.242 | 0.328 |
| FM (kg) | 36.4 ± 15.2 | 37.8 ± 13.5 | 0.387 | 28.4 ± 12.5 | 35.7 ± 18.7 | 0.034 | 0.012 | 0.265 |
| FG (mg/dL) | 107.6 ± 16.8 | 110.4 ± 19.4 | 0.432 | 89.5 ± 13.1 | 105.2 ± 17.2 | 0.011 | 0.009 | 0.324 |
| TC (mg/dL) | 232.3 ± 35.3 | 251.4 ± 29.8 | 0.115 | 185.5 ± 22.4 | 244.1 ± 27.6 | 0.009 | 0.012 | 0.565 |
| LDL-C (mg/dL) | 143.4 ± 25.3 | 148.4 ± 21.5 | 0.355 | 115.9 ± 16.5 | 142.8 ± 18.7 | 0.001 | 0.008 | 0.487 |
| HDL-C (mg/dL) | 54.6 ± 9.1 | 50.23 ± 11.3 | 0.231 | 65.8 ± 12.4 | 52.2 ± 9.5 | 0.025 | 0.018 | 0.314 |
| TG (mg/dL) | 169.8 ± 29.1 | 166.4 ± 25.2 | 0.554 | 148.2 ± 18.9 | 159.6 ± 21.5 | 0.085 | 0.068 | 0.249 |
| SBP (mm Hg) | 141.6 ± 13.4 | 138.8 ± 10.6 | 0.387 | 135.2 ± 11.8 | 145.1 ± 9.5 | 0.115 | 0.217 | 0.363 |
| DBP (mm Hg) | 89.4 ± 7.9 | 87.2 ± 10.5 | 0.425 | 84.6 ± 8.4 | 86.5 ± 9.8 | 0.225 | 0.378 | 0.512 |
| Parameter | Before Intervention | Post Intervention | P 3 | P 4 | ||||
|---|---|---|---|---|---|---|---|---|
| INEG | CG | P 1 | INEG | CG | P 2 | |||
| Elevated WC | 35 (77.8) | 38 (84.4) | 0.556 | 27 (60.0) | 39 (86.7) | 0.008 | 0.011 | 0.432 |
| Elevated FG | 30 (66.7) | 27 (60.0) | 0.452 | 17 (37.8) | 28 (62.2) | 0.001 | 0.009 | 0.395 |
| Elevated TG | 15 (33.3) | 18 (40.0) | 0.397 | 13 (28.9) | 15 (33.3) | 0.422 | 0.565 | 0.483 |
| Reduced HDL-C | 13 (28.9) | 15 (33.3) | 0.622 | 8 (17.8) | 14 (31.1) | 0.012 | 0.007 | 0.388 |
| Elevated BP | 26 (57.8) | 28 (62.2) | 0.458 | 27 (60.0) | 29 (64.4) | 0.452 | 0.354 | 0.411 |
| MetS risk factors | ||||||||
| 1–2 | 0 (0.0) | 0 (0.0) | - | 28 (62.2) | 2 (4.4) | 0.001 | 0.001 | 0.254 |
| 3 | 30 (66.7) | 34 (75.6) | 0.233 | 15 (33.3) | 31 (68.9) | 0.001 | 0.001 | 0.315 |
| 4–5 | 15 (33.3) | 11 (24.4) | 0.185 | 2 (4.4) | 12 (26.7) | 0.001 | 0.001 | 0.455 |
| Nutrients in Diet | WC | FG | HDL-C |
|---|---|---|---|
| SFA (% energy) | 0.08 | 0.07 | −0.35 * |
| MUFA (% energy) | −0.16 | −0.12 | −0.14 |
| PUFA (% energy) | −0.09 | −0.11 | 0.31 * |
| PUFA n-6:n-3 | −0.11 | −0.19 | −0.41 * |
| Cholesterol (mg) | 0.13 | 0.09 | −0.15 |
| Fiber (g) | −0.45 * | −0.48 * | 0.38 * |
| Sodium (mg) | 0.02 | 0.17 | 0.01 |
| Magnesium (mg) | −0.01 | −0.06 | 0.11 |
| Vitamin C (mg) | −0.08 | −0.12 | 0.14 |
| Polyphenols (mg) | −0.45 * | −0.54 * | 0.43 * |
| Flavonoids (mg) | −0.44 * | −0.65 * | 0.48 * |
| Flavanols (mg) | −0.43 * | −0.38 * | 0.42 * |
| Anthocyanins (mg) | −0.41 * | −0.51 * | 0.45 * |
| Phenolic acids (mg) | −0.21 | −0.19 | 0.22 |
| Model | Variables | WC | FG | HDL-C |
|---|---|---|---|---|
| Polyphenols (mg) | ||||
| 1 | β (95% CI) p-value | −0.392 (0.085–0.624) 0.014 | −0.535 (0.287–0.756) 0.006 | −0.388 (0.097–0.624) 0.012 |
| Model parameters | R2 = 0.11 | R2 = 0.44 | R2 = 0.10 | |
| 2 | β (95% CI) p-value | −0.355 (0.085–0.582) 0.021 | −0.498 (0.185–0.722) 0.011 | −0.374 (0.105–0.549) 0.011 |
| Model parameters | R2 = 0.10 0.025 | R2 = 0.38 0.014 | R2 = 0.09 0.044 | |
| 3 | β (95% CI) p-value | −0.402 (0.095–0.712) 0.014 | −0.482 (0.195–0.698) 0.019 | −0.397 (0.118–0.564) 0.013 |
| Model parameters | R2 = 0.06 0.225 | R2 = 0.35 0.024 | R2 = 0.09 0.112 | |
| Flavonoids (mg) | ||||
| 1 | β (95% CI) p-value | −0.422 (0.142–0.654) 0.011 | −0.652 (0.398–0.912) 0.001 | −0.476 (0.155–0.698) 0.012 |
| Model parameters | R2 = 0.15 | R2 = 0.57 | R2 = 0.14 | |
| 2 | β (95% CI) p-value | −0.414 (0.112–0.622) 0.014 | −0.632 (0.355–0.897) 0.001 | −0.442 (0.201–0.623) 0.016 |
| Model parameters | R2 = 0.13 0.021 | R2 = 0.55 0.001 | R2 = 0.11 0.034 | |
| 3 | β (95% CI) p-value | −0.387 (0.106–0.698) 0.034 | −0.597 (0.311–0.815) 0.001 | −0.398 (0.125–0.612) 0.045 |
| Model parameters | R2 = 0.09 0.095 | R2 = 0.45 0.009 | R2 = 0.08 0.114 | |
| Flavanols (mg) | ||||
| 1 | β (95% CI) p-value | −0.422 (0.112–0.654) 0.017 | −0.373 (0.085–0.545) 0.016 | −0.392 (0.154–0.523) 0.024 |
| Model parameters | R2 = 0.12 | R2 = 0.14 | R2 = 0.11 | |
| 2 | β (95% CI) p-value | −0.388 (0.089–0.565) 0.021 | −0.352 (0.115–0.512) 0.025 | −0.376 (0.117–0.526) 0.019 |
| Model parameters | R2 = 0.10 | R2 = 0.11 | R2 = 0.12 | |
| 3 | β (95% CI) p-value | −0.361 (0.079–0.584) 0.022 | −0.335 (0.086–0.554) 0.031 | −0.344 (0.115–0.545) 0.039 |
| Model parameters | R2 = 0.09 0.134 | R2 = 0.06 0.219 | R2 = 0.08 0.185 | |
| Anthocyanins (mg) | ||||
| 1 | β (95% CI) p-value | −0.394 (0.135–0.711) 0.011 | −0.498 (0.195–0.798) 0.001 | −0.435 (0.155–0.681) 0.015 |
| Model parameters | R2 = 0.13 | R2 = 0.39 | R2 = 0.14 | |
| 2 | β (95% CI) p-value | −0.351 (0.118–0.668) 0.014 | −0.477 (0.211–0.744) 0.001 | −0.415 (0.132–0.654) 0.018 |
| Model parameters | R2 = 0.11 0.019 | R2 = 0.35 0.011 | R2 = 0.16 0.034 | |
| 3 | β (95% CI) p-value | −0.335 (0.113–0.598) 0.024 | −0.455 (0.178–0.699) –0.015 | −0.382 (0.098–0.591) 0.021 |
| Model parameters | R2 = 0.08 0.119 | R2 = 0.32 0.015 | R2 = 0.09 0.135 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zujko, M.E.; Rożniata, M.; Zujko, K. Individual Diet Modification Reduces the Metabolic Syndrome in Patients Before Pharmacological Treatment. Nutrients 2021, 13, 2102. https://doi.org/10.3390/nu13062102
Zujko ME, Rożniata M, Zujko K. Individual Diet Modification Reduces the Metabolic Syndrome in Patients Before Pharmacological Treatment. Nutrients. 2021; 13(6):2102. https://doi.org/10.3390/nu13062102
Chicago/Turabian StyleZujko, Małgorzata Elżbieta, Marta Rożniata, and Kinga Zujko. 2021. "Individual Diet Modification Reduces the Metabolic Syndrome in Patients Before Pharmacological Treatment" Nutrients 13, no. 6: 2102. https://doi.org/10.3390/nu13062102
APA StyleZujko, M. E., Rożniata, M., & Zujko, K. (2021). Individual Diet Modification Reduces the Metabolic Syndrome in Patients Before Pharmacological Treatment. Nutrients, 13(6), 2102. https://doi.org/10.3390/nu13062102







