COVID Obesity: A One-Year Narrative Review
Abstract
1. Introduction
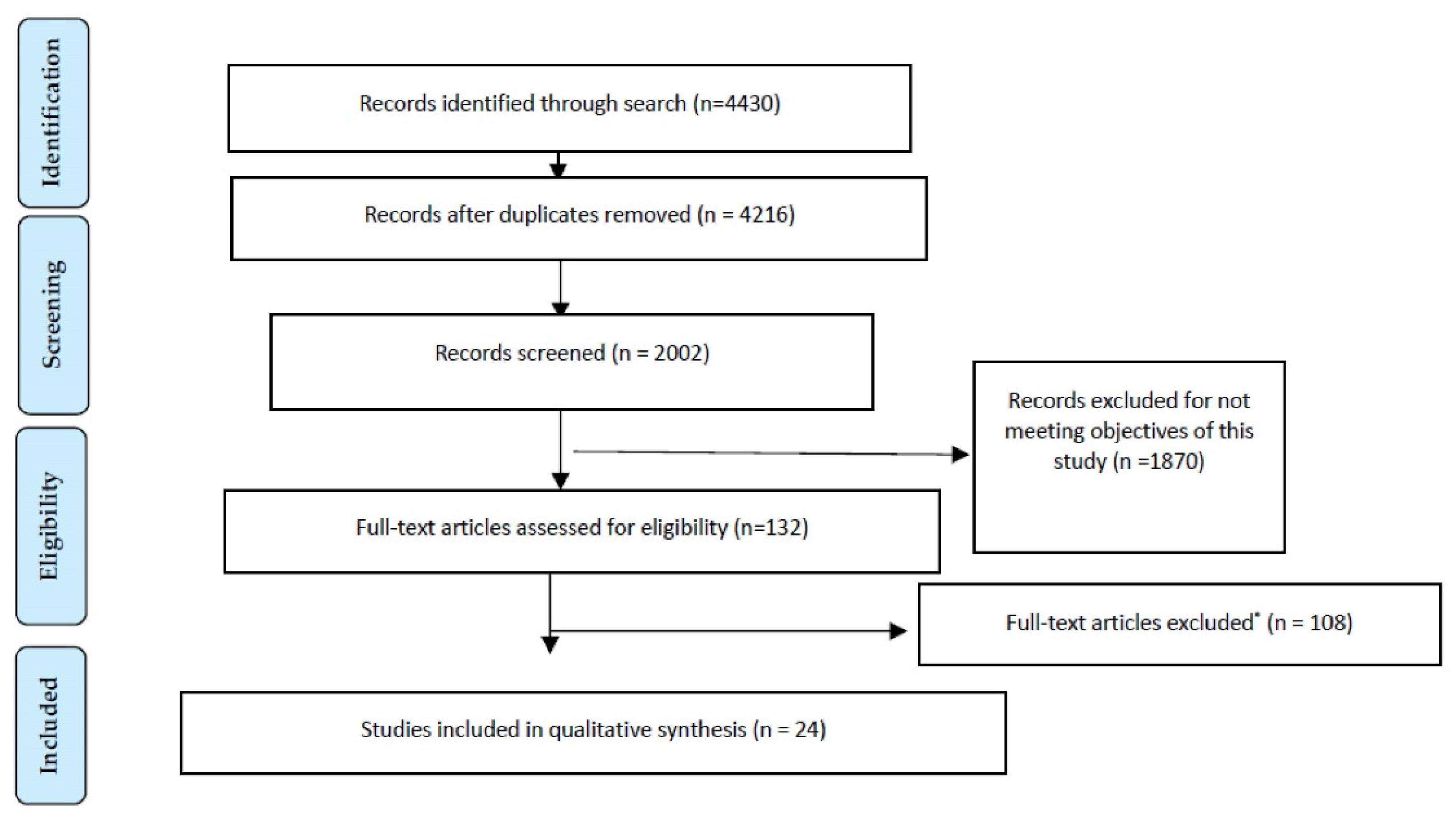
2. Materials and Methods
3. Results
3.1. China
3.2. Korea
3.3. France
3.4. USA
3.5. Spain
3.6. Italy
3.7. Mexico
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Sahin, A.R.; Erdogan, A.; Agaoglu, P.M.; Dineri, Y.; Cakirci, A.Y.; Senel, M.E.; Okyay, R.A.; Tasdogan, A.M. 2019 Novel Coronavirus (COVID-19) outbreak: A review of the current literature. EJMO 2020, 4, 1–7. [Google Scholar] [CrossRef]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Vijayanand, P.; Wilkins, M.W. Severe Acute Respiratory Syndrome (SARS): A review. Clin. Med. 2004, 4, 152–160. [Google Scholar] [CrossRef]
- Al-Tawfiq, J.A.; Gautret, P. Asymptomatic Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection: Extent and implications for infection control: A systematic review. Travel Med. Infect. Dis. 2019, 27, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Guarner, J. Three Emerging Coronaviruses in Two Decades: The Story of SARS, MERS, and Now COVID-19. Am. J. Clin. Pathol. 2020, 153, 420–421. [Google Scholar] [CrossRef] [PubMed]
- Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020, 5, 536–544. [Google Scholar] [CrossRef]
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/csr/don/17-january-2020-novel-coronavirus-japan-ex-china/en/ (accessed on 4 June 2021).
- Nishiura, H.; Jung, S.M.; Linton, N.M.; Kinoshita, R.; Yang, Y.; Hayashi, K.; Kobayash, T.; Yuan, B.; Akhmetzhanov, A.R. The extent of transmission of novel coronavirus in Wuhan, China, 2020. J. Clin. Med. 2020, 9, 330. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 4 June 2021).
- Van den Brand, J.M.; Smits, S.L.; Haagmans, B.L. Pathogenesis of Middle East respiratory syndrome coronavirus. J. Pathol. 2015, 235, 175–184. [Google Scholar] [CrossRef]
- Louie, J.K.; Acosta, M.; Samuel, M.C.; Schechter, R.; Vugia, D.J.; Harriman, K.; Matyas, B.T. A novel risk factor for a novel virus: Obesity and 2009 pandemic influenza A (H1N1). Clin. Infect. Dis. 2011, 52, 301–312. [Google Scholar] [CrossRef]
- Wang, X.F.; Shi, G.C.; Wan, H.Y.; Hang, S.G.; Chen, H.; Chen, W.; Qu, H.P.; Han, B.H.; Zhou, M. Clinical features of three avian influenza H7N 9 virus-infected patients in Shanghai. Clin. Respir. J. 2014, 8, 410–416. [Google Scholar] [CrossRef]
- Phung, D.T.; Wang, Z.; Rutherford, S.; Huang, C.; Chu, C. Body mass index and risk of pneumonia: A systematic review and meta-analysis. Obes. Rev. 2013, 14, 839–857. [Google Scholar] [CrossRef]
- Nie, W.; Zhang, Y.; Jee, S.H.; Jung, K.J.; Li, B.; Xiu, Q. Obesity survival paradox in pneumonia: A meta-analysis. BMC Med. 2014, 12, 61. [Google Scholar] [CrossRef]
- Kahlon, S.; Eurich, D.T.; Padwal, R.S.; Malhotra, A.; Minhas-Sandhu, J.K.; Marrie, T.J.; Majumdar, S.R. Obesity and outcomes in patients hospitalized with pneumonia. Clin. Microbiol. Infect. 2013, 19, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Singanayagam, A.; Singanayagam, A.; Chalmers, J.D. Obesity is associated with improved survival in community-acquired pneumonia. Eur. Respir. J. 2013, 42, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, 65–94. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; WHO Western Pacific Region: Geneva, Switzerland, 1998. [Google Scholar]
- World Health Organization Western Pacific Region; International Association for the Study of Obesity; International Obesity Task Force. The Asian-Pacific Perspective: Redefining Obesity and Its Treatment; WHO Western Pacific Region: Geneva, Switzerland, 2000. [Google Scholar]
- Seo, M.H.; Lee, W.Y.; Kim, S.S.; Kang, J.H.; Kang, J.H.; Kim, K.K.; Kim, B.Y.; Kim, Y.H.; Kim, W.J.; Kim, E.M.; et al. 2018 Korean society for the study of obesity guideline for the management of obesity in Korea. J. Obes. Metab. Syndr. 2019, 28, 40–45. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung and Blood Institute. Quality Assessment Tool for Case Series Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 4 June 2021).
- Salehi, S.; Abedi, A.; Balakrishnan, S.; Gholamrezanezhad, A. Coronavirus disease 2019 (COVID-19): A systematic review of imaging findings in 919 patients. Am. J. Roentgenol. 2020, 215, 1–7. [Google Scholar] [CrossRef]
- Lim, J.; Jeon, S.; Shin, H.Y.; Kim, M.J.; Seong, Y.M.; Lee, W.J.; Choe, K.W.; Kang, Y.M.; Lee, B.; Park, S.J. Case of the index patient who caused tertiary transmission of Coronavirus disease 2019 in Korea: The application of lopinavir/ritonavir for the treatment of COVID-19 pneumonia monitored by quantitative RT-PCR. J. Korean Med. Sci. 2020, 35, e79. [Google Scholar] [CrossRef]
- Kim, J.Y.; Choe, P.G.; Oh, Y.; Oh, K.J.; Kim, J.; Park, S.J.; Park, J.H.; Na, H.K.; Oh, M.D. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: Implication for infection prevention and control measures. J. Korean Med. Sci. 2020, 35, e61. [Google Scholar] [CrossRef]
- Li, Q.; Cheng, Q.; Zhao, Z.; Zeng, L.; Zhu, L.; Guo, W.; Li, C.; Wang, J.; Li, S.; Shen, N.; et al. Novel Coronavirus infection and acute kidney injury in two renal transplant recipients: Case report. J. Int. Med. Res. 2020, 48, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; He, P.; Liu, H.G.; Wang, X.J.; Li, F.J.; Chen, S.; Lin, J.; Chen, P.; Liu, J.H.; Li, C.H. Clinical characteristics of 30 medical workers infected with new coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 2020, 43, 209–214. [Google Scholar] [PubMed]
- Liu, J.; Ouyang, L.; Guo, P.; Wu, H.S.; Fu, P.; Chen, Y.L.; Yang, D.; Han, X.Y.; Cao, Y.K. Epidemiological, clinical characteristics and outcome of medical staff infected with COVID-19 in Wuhan, China: A retrospective case series analysis. MedRxiv 2020. [Google Scholar] [CrossRef]
- Yang, W.; Cao, Q.; Qin, L.; Wang, X.; Cheng, Z.; Pan, A.; Dai, J.; Sun, Q.; Zhao, F.; Qu, J.; et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): A multi-center study in Wenzhou city, Zhejiang, China. J. Infect. 2020, 80, 388–393. [Google Scholar] [CrossRef]
- Peng, Y.D.; Meng, K.; Guan, H.Q.; Leng, L.; Zhu, R.R.; Wang, B.Y.; He, M.A.; Cheng, L.X.; Huang, K.; Zeng, Q.T. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Jie He He Hu Xi Za Zhi 2020, 48, e4. [Google Scholar]
- Cai, Q.; Huang, D.; Ou, P.; Yu, H.; Zhu, Z.; Xia, Z.; Su, Y.; Ma, Z.G.; Zhang, Y.; Li, Z.; et al. COVID-19 in a designated infectious diseases Hospital outside Hubei Province, China. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/all.14309 (accessed on 4 June 2021).
- Huang, M.; Yang, Y.; Futai, S.; Yishan, Z.; Wenjing, Z.; Liang, L.; Liang, L.; Xudong, H.; Aihua, L.; Hongsheng, Z.; et al. Early and critical care in severe patients with COVID-19 in Jiangsu Province, China: A descriptive study. Lancet 2020. Available online: https://ssrn.com/abstract=3546056 (accessed on 4 June 2021). [CrossRef]
- Xu, Y.; Xu, Z.; Liu, X.; Cai, L.; Zheng, H.; Huang, Y.; Zhou, L.; Huang, L.; Lin, Y.; Deng, L. Clinical findings in critical ill patients infected with SARS-Cov-2 in Guangdong Province, China: A multi-center, retrospective, observational study. MedRxiv 2020. [Google Scholar] [CrossRef]
- Ji, D.; Zhang, D.; Chen, Z.; Xu, Z.; Zhao, P.; Zhang, M.; Zhang, L.; Cheng, G.; Wang, Y.; Yang, G. Clinical characteristics predicting progression of COVID-19. Lancet 2020. Available online: https://ssrn.com/abstract=3539674 (accessed on 4 June 2021). [CrossRef]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A.; Labreuche, J.; Mathieu, D.; Pattou, F.; Jourdain, M.; et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity 2020, 28, 1195–1199. [Google Scholar] [CrossRef]
- Palaiodimos, L.; Kokkinidis, G.; Weijia, L.; Karamanis, D.; Ognibene, J.; Arora, S.; Southern, W.N.; Mantzoros, C.S. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism 2020, 108, 154262. [Google Scholar] [CrossRef]
- Lighter, J.; Phillips, M.; Hochman, S.; Sterling, S.; Johnson, D.; Francois, F.; Stachel, A. Obesity in patients younger than 60 years is a risk factor for covid-19 hospital admission. Clin. Infect. Dis. 2020, 15, 896–897. [Google Scholar] [CrossRef]
- Nilles, E.J.; Siddiqui, S.M.; Fischinger, S.; Bartsch, Y.C.; de Saint Aubin, M.; Zhou, G.; Gluck, M.; Berger, S.; Rhee, J.; Petersen, E.; et al. Epidemiological and immunological features of obesity and SARS-CoV-2. MedRxiv 2020. [Google Scholar] [CrossRef]
- Anderson, M.R.; Geleris, J.; Anderson, D.R.; Zucker, J.; Nobel, Y.R.; Freedberg, D.; Small-Saunders, J.; Rajagopalan, K.N.; Greendyk, R.; Chae, S.R.; et al. Body mass index and risk for intubation or death in SARS-CoV-2 infection: A retrospective cohort study. Ann. Intern. Med. 2020, 173, 782–790. [Google Scholar] [CrossRef]
- Cai, Q.; Chen, F.; Wang, T.; Luo, F.; Liu, X.; Wu, Q.; He, Q.; Wang, Z.; Liu, Y.; Liu, L.; et al. Obesity and COVID-19 severity in a designated hospital in Shenzhen, China. Diabetes Care 2020, 43, 1392–1398. [Google Scholar] [CrossRef] [PubMed]
- Shao Hang, C.; Liao, W.; Shu Wei, C.; Li Li, L.; Si Yao, L.; Zhi Dan, Z. Association between obesity and clinical prognosis in patients infected with SARSCoV-2. Infect. Dis. Poverty 2020, 9, 80. [Google Scholar]
- Fernandez Garcia, L.; Puentes Gutierrez, A.B.; Garci Bascones, M. Relación entre obesidad, diabetes e ingreso en UCI en pacientes COVID-19. Med. Clin. 2020, 155, 313–317. [Google Scholar] [CrossRef]
- Ferrando, C.; Mellado Artigas, R.; Gea, A.; Arruti, E.; Aldecoa, C.; Bordell, A.; Adalia, R.; Zattera, L.; Ramasco, F.; Monedero, P.; et al. Características, evolución clínica y factores asociados, la mortalidad en UCI de los pacientes críticos infectados por SARS-CoV-2 en España: Estudio prospectivo, de cohorte t multicéntrico. Rev. Esp. Anestesiol. Reanim. 2020, 67, 425–437. [Google Scholar] [CrossRef]
- Casas-Rojo, J.M.; Santos, J.M.; Millán-Núñez-Cortés, J.; Lumbreras-Bermejo, C.; Ramos-Rincón, J.M.; Roy-Vallejo, E.; Artero-Mora, A.; Arnalich-Fernández, F.; García-Bruñén, J.M.; Vargas-Núñez, J.A.; et al. Clinical characteristics of patients hospitalized with COVID-19 in Spain: Results from the SEMI-COVID-19 Registry. Rev. Clin. Esp. 2020, 220, 480–494. [Google Scholar] [CrossRef]
- Rosales Castillo, A.; García de los Rios, C.; Mediavilla García, C. Persistencia de manifestaciones clínicas tras la infección COVID-19: Importancia del seguimiento. Med. Clin. 2020, 156, 35–36. [Google Scholar] [CrossRef]
- Halasz, G.; Leoni, L.M.; Quinto Villani, G.; Nolli, M.; Villani, M. Obesity, overweight and survival in critically ill patients with SARS-CoV-2 pneumonia: Is there an obesity paradox? Preliminary results from Italy. Eur. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef]
- Herrera García, J.C.; Arellano Montellano, E.I.; Juárez González, L.I.; Contreras Andrade, R.I. Persistencia de síntomas en pacientes después de la enfermedad por coronavirus (COVID-19) en un hospital de tercer nivel de Puebla, México. Med. Int. Méx. 2020, 6, 789–793. [Google Scholar]
- Huang, R.; Zhu, L.; Xue, L.; Liu, L.; Yan, X.; Wang, J.; Zhang, B.; Xu, T.; Ji, F.; Zhao, Y.; et al. Clinical findings of patients with coronavirus disease 2019 in Jiangsu Province, China: A retrospective, multi-center study. PLoS Negl. Trop. Dis. 2020, 14, e0008280. [Google Scholar] [CrossRef] [PubMed]
- McMichael, T.M.; Clark, S.; Pogosjans, S.; Kay, M.; Lewis, J.; Baer, A.; Kawakami, V.; Lukoff, M.D.; Ferro, J.; Brostrom-Smith, C.; et al. COVID-19 in a Long-Term Care Facility—King County, Washington, February 27–March 9, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 339–342. [Google Scholar] [CrossRef] [PubMed]
- Deng, S.Q.; Peng, H.J. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J. Clin. Med. 2020, 2, 575. [Google Scholar] [CrossRef]
- Liao, J.; Fan, S.; Chen, J.; Wu, J.; Xu, S.; Guo, Y.; Li, C.; Zhang, X.; Wu, C.; Mou, H.; et al. Epidemiological and clinical characteristics of COVID-19 in adolescents and young adults. Innovation 2020, 1, 1–13. [Google Scholar]
- Larrea Villacis, M.J.; Vallejo Romero, V.E. Neumonía por Covid-19 en paciente femenina con obesidad mórbida. Recimundo 2020, 4, 168–172. [Google Scholar] [CrossRef]
- Spiteri, G.; Fielding, J.; Diercke, M.; Campese, C.; Enouf, V.; Gaymard, A.; Bella, A.; Sognamiglio, P.; Sierra Moros, M.J.; Nicolau Riutort, A.; et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill. 2020, 25, 2000178. [Google Scholar] [CrossRef]
- World Health Organization. Surface Sampling of Coronavirus Disease (COVID-19): A Practical “How to” Protocol for Health Care and Public Health Professionals. Available online: https://apps.who.int/iris/handle/10665/331058 (accessed on 4 June 2021).
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef] [PubMed]
- Bilben, B.; Grandal, L.; Søvik, S. National Early Warning Score (NEWS) as an emergency department predictor of disease severity and 90-day survival in the acutely dyspneic patient–a prospective observational study. Scand. J. Trauma. Resusc. Emerg. Med. 2016, 24, 80. [Google Scholar] [CrossRef] [PubMed]
- Canpolat, G.; Ozgultekin, A.; Turan, G.; Iskender, A.; Adiyeke, E.; Ekinci, O. Does average volume-assured pressure support make any difference compared with BIPAP? Crit. Care 2014, 18, P265. [Google Scholar] [CrossRef]
- Heymann, D.L.; Shindo, N. COVID-19: What is next for public health? Lancet 2020, 395, 542–545. [Google Scholar] [CrossRef]
- Chen, W.H.; Lu, C.Y.; Shao, P.L.; Lee, P.I.; Kao, C.L.; Chung, M.Y.; Chang, L.Y.; Huang, L.M. Risk factors of severe novel influenza A (H1N1) infections in hospitalized children. J. Formos. Med. Assoc. 2012, 111, 421–426. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Plessa, E.; Diakakis, P.; Gardelis, J.; Thirios, A.; Koletsi, P.; Falagas, M.E. Clinical features, risk factors, and complications among pediatric patients with pandemic influenza A (H1N1). Clin. Pediatr. 2010, 49, 777–781. [Google Scholar] [CrossRef]
- Moser, J.S.; Galindo-Fraga, A.; Ortiz-Hernández, A.A.; Gu, W.; Hunsberger, S.; Galán-Herrera, J.F.; Guerrero, M.L.; Ruiz-Palacios, G.M.; Beigel, J.H.; La Red ILI 002 Study Group. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir. Viruses 2019, 13, 3–9. [Google Scholar] [CrossRef]
- Milner, J.J.; Rebeles, J.; Dhungana, S.; Stewart, D.A.; Sumner, S.C.; Meyers, M.H.; Mancuso, P.; Beck, M.A. Obesity increases mortality and modulates the lung metabolome during Pandemic H1N1 Influenza virus infection in mice. J. Immunol. 2015, 194, 4846–4859. [Google Scholar] [CrossRef]
- Maier, H.E.; Lopez, R.; Sanchez, N.; Ng, S.; Gresh, L.; Ojeda, S.; Burger-Calderon, R.; Kuan, G.; Harris, E.; Balmaseda, A. Obesity increases the duration of Influenza A virus shedding in adults. J. Infect. Dis. 2018, 218, 1378–1382. [Google Scholar] [CrossRef]
- Dietz, W.; Santos-Burgoa, C. Obesity and its implications for COVID-19 mortality. Obesity 2020, 28, 1005. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Pang, B.; Zhang, J.; Liu, Q.; Yang, Z.; Feng, J.; Liu, X.; Zhang, L.; Wang, B.; Huang, Y.; et al. Core outcome set for clinical trials on Coronavirus Disease 2019 (COS-COVID). Engineering 2020, 6, 1147–1152. [Google Scholar] [CrossRef]
- Arnold, F.W.; Burns, M.V.; Mahmood, K.; Aden, D.; Furmanek, S.P.; Tella, M.A.; Glick, C.; Raghuram, A.; Beavin, L.; Cavallazzi, R.; et al. Endemic human coronaviruses in hospitalized adults with community-acquired pneumonia: Results from the Louisville Pneumonia Study. Univ. Louisville J. Respir. Infect. 2020, 4, 1–11. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Novel, C.P.E.R.E. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 41, 145–151. [Google Scholar]
- Liu, Y.; Yan, L.M.; Wan, L.; Xiang, T.X.; Le, A.; Liu, J.M.; Peiris, M.; Poon, L.L.M.; Zhang, W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect. Dis. 2020, 20, 656–657. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. New Coronavirus Pneumonia Diagnosis and Treatment Program (Trial Version 5, Revised Version). Available online: http://www.nhc.gov.cn/yzygj/s7652m/202002/41c3142b38b84ec4a748e60773cf9d4f.shtml (accessed on 4 June 2021).
- Guan, W.J.; Liang, W.H.; Zhao, Y.; Liang, H.R.; Chen, Z.S.; Li, Y.M.; Liu, X.Q.; Chen, R.C.; Tang, C.L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef]
- Johnson, H.C.; Gossner, C.M.; Colzani, E.; Kinsman, J.; Alexakis, L.; Beauté, J.; Würz, A.; Tsolova, S.; Bundle, N.; Ekdahl, K. Potential scenarios for the progression of a COVID-19 epidemic in the European Union and the European Economic Area, March 2020. Euro Surveill. 2020, 25, 2000202. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità. Characteristics of COVID-19 Patients Dying in Italy Report Based on Available Data on March 20th. 2020. Available online: https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_20_marzo_eng.pdf (accessed on 4 June 2021).
- Addo, L. Of the COVID-19 in Ghana—Preparedness, Demographics and Comorbidity (March 27, 2020). Available online: https://ssrn.com/abstract=3562720 (accessed on 4 June 2021).
- Comité Internacional para la Elaboración de Consensos y Estandarización en Nutriología (CIENUT). Posición de Expertos Sobre el Manejo Nutricional del Coronavirus COVID-19. Available online: https://www.cienut.org/comite_internacional/declaraciones/pdf/declaracion2.pdf (accessed on 4 June 2021).
- Shi, Q.; Zhang, X.; Jiang, F.; Tao, J.; Zhang, X.; Hu, N.; Feng, J.; Bimu, J.; Yan, S.; Guan, Y.; et al. Diabetic Patients with COVID-19, Characteristics and Outcome: A Two-Centre, Retrospective, Case Control Study. SSRN. Available online: https://awesomecapital.blogspot.com/2020/03/diabetic-patients-with-covid-19.html (accessed on 4 June 2021).
- Wang, T.; Du, Z.; Zhu, F.; Cao, Z.; An, Y.; Gao, Y.; Jiang, B. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet 2020, 395, e52. [Google Scholar] [CrossRef]
- Luzi, L.; Radaelli, M.G. Influenza and obesity: Its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020, 57, 759–764. [Google Scholar] [CrossRef]
- Li, Y.; Jiang, H.; Xu, H.; Li, N.; Zhang, Y.; Wang, G.; Xu, Z. Impact of a higher body mass index on prolonged intubation in patients undergoing surgery for acute thoracic aortic dissection. Heart Lung Circ. 2020, 29, 1725–1732. [Google Scholar] [CrossRef]
- Xu, K.; Cai, H.; Shen, Y.; Ni, Q.; Chen, Y.; Hu, S.; Li, J.; Wang, H.; Yu, L.; Huang, H.; et al. Management of corona virus disease-19 (COVID-19): The Zhejiang experience. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020, 49, 147–157. [Google Scholar]
- Li, L.; Li, S.; Xu, M.; Zheng, S.; Duan, Z.; Chen, Y.; Li, J. The level of plasma C-reactive protein is closely related to the liver injury in patients with COVID-19. MedRxiv 2020. [Google Scholar] [CrossRef]
- Baos, V. A Medical Account from My Own Experience. 2020. Available online: https://www.vozpopuli.com/altavoz/next/Covid-19-relato-medico-propia-experiencia_0_1341767497.html (accessed on 4 June 2021).
- Barazzoni, R.; Bischoff, S.C.; Krznaric, Z.; Pirlich, M.; Singer, P. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin. Nutr. 2020, 39, 1631–1638. [Google Scholar] [CrossRef]
- Schneider, S.M.; Albert, V.; Barbier, N.; Barnoud, D.; Bouteloup, C.; Chambrier, C.; Fayemendy, P.; Flori, N.; Goulet, O.; Guimber, D. Adaptations de la prise en charge des patients en Nutrition Artificielle à Domicile au cours de l’épidémie virale COVID-19 en France: Avis du Comité de Nutrition à Domicile de la Société Francophone de Nutrition Clinique et Métabolisme (SFNCM). Nutr. Clin. Métab. 2020, 34, 105–107. [Google Scholar] [CrossRef]
- Monteleone, G.; Ardizzone, S. Are patients with inflammatory bowel disease at increased risk for Covid-19 infection? J. Crohns Colitis 2020, 14, 1334–1336. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Moore, L.W. Impact of nutrition and diet on COVID-19 infection and implications for kidney health and kidney disease management. J. Ren. Nutr. 2020, 30, 179–181. [Google Scholar] [CrossRef] [PubMed]
| Anthropometric Parameters | International Adults | Asian Criteria-Based Adults | Korean Criteria-Based Adults | |||
|---|---|---|---|---|---|---|
| BMI (kg/m2) | Risk of Co-Morbidities | BMI (kg/m2) | Risk of Co-Morbidities | BMI (kg/m2) | Risk of Co-Morbidities | |
| Underweight | <18.5 | Lower (other health risk) | <18.5 | Lower (other health risk) | <18.5 | Low a/average b |
| Normal weight | 18.5–24.9 | Average | 18.5–22.9 | Average | 18.5–22.9 | Average a/increased b |
| Overweight (pre-obesity) | 25.0–29.9 | Increased | 23.0–24.9 | Increased | 23.0–24.9 | Increased a/moderate b |
| Obesity class I | 30.0–34.9 | Moderate | 25.0–29.9 | Moderate | 25.0–29.9 | High a/severe b |
| Obesity class II | 35.0–39.9 | Severe | ≥30.0 | Severe | 30.0–34.9 | Moderate a/very severe b |
| Obesity class III | ≥40.0 | Very severe | n.a. | n.a. | ≥35 | Severea/very severe b |
| Reference/Item a | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Quality Rating b |
|---|---|---|---|---|---|---|---|---|---|---|
| [24] | + | + | ? | ? | + | + | + | ? | + | 6 |
| [25] | + | + | ? | ? | + | + | + | ? | + | 6 |
| [26] | + | + | ? | ? | + | + | + | ? | + | 6 |
| [27] | + | + | ? | ? | + | + | + | + | + | 6 |
| [28] | + | + | ? | ? | + | + | + | + | + | 6 |
| [29] | + | + | ? | ? | ? | + | ? | + | + | 5 |
| [30] | + | + | ? | ? | ? | + | ? | ? | + | 4 |
| [31] | + | + | ? | ? | ? | + | ? | ? | + | 4 |
| [32] | + | + | ? | ? | ? | + | ? | ? | + | 5 |
| [33] | + | + | ? | ? | ? | + | ? | - | + | 4 |
| [34] | + | + | ? | ? | ? | + | ? | ? | + | 4 |
| [35] | + | + | ? | ? | + | + | + | + | + | 7 |
| [36] | + | + | ? | ? | ? | + | ? | + | + | 5 |
| [37] | + | + | ? | ? | ? | + | + | + | + | 6 |
| [38] | + | + | ? | ? | ? | + | + | + | + | 6 |
| [39] | + | + | ? | ? | + | + | + | + | + | 7 |
| [40] | + | + | ? | ? | + | + | + | + | + | 7 |
| [41] | + | + | ? | ? | + | + | ? | + | + | 6 |
| [42] | + | + | ? | ? | ? | + | ? | ? | + | 4 |
| [43] | + | + | ? | ? | + | + | + | + | + | 7 |
| [44] | + | + | ? | ? | + | + | + | ? | + | 6 |
| [45] | + | + | ? | ? | ? | + | ? | ? | + | 4 |
| [46] | + | + | ? | ? | ? | + | + | ? | + | 5 |
| [47] | + | + | ? | ? | + | + | + | ? | + | 6 |
| No. of Patients | Age | Sex | Country | BMI (kg/m2)/Anthropometric Parameters [18,19,20] | References |
|---|---|---|---|---|---|
| 1 | 54 | Male (M) | Korea | 25.7/Obesity class I | [24] |
| 1 | 35 | Female (F) | Korea | 33.4/Obesity class II | [25] |
| 1 | 59 | M | China | 26.6/Obesity class I | [26] |
| 30 | 21–59 | F (66.7%)/M (33.3%) | China | 22.0 ± 1.3/Normal weight a 27.0 ± 2.5/Obesity class I b | [27] |
| 64 | 35.0 (average) | F (64.0%)/M (36.0%) | China | <24 (89.2%) and ≥ 24 (10.8%) c <24 (88.0%) and ≥ 24 (12.0%) d | [28] |
| 149 | 45.11 ± 13.35 | F (45.6%)/M (54.4%) | China | 23.7 ± 4.5/Overweight | [29] |
| 112 | 62.0 (average) | F (52.7%)/M (47.3%) | China | 22.0 (22.0–24.0)/Normal weight e 25.5 (23.0–27.5)/Obesity class I f | [30] |
| 298 | 33–61 | F (50.0%)/M (50.0%) | China | 22.9 (20.6–25.2)/Normal weight g 24.5 (22.0–27.8)/Overweight h | [31] |
| 60 | 57 (average) | F (41.7%)/M (58.3%) | China | 25.0 ± 3.3/Obesity class I | [32] |
| 45 | 56.7 ± 15.4 | F (35.6%)/M (64.4%) | China | 23.2 (21.4–25.3)/Overweight i 25.2 (22.9–26.9)/Obesity class I j | [33] |
| 49 | 43.6 ± 17.1 | F (36.7%)/M (63.3%) | China | 24.3 ± 3.6/Overweight k 26.4 ± 2.8/Obesity class I l | [34] |
| 124 | 51–70 | F (27.0%)/M (73.0%) | France | 31.1 (27.3–37.5)/Obesity class I m 27.0 (25.3–30.8)/Overweight I n | [35] |
| 200 | 64 (50–73.5) | F (51.0%)/M (49.0%) | USA | 30.0 (26–35) Obesity class I | [36] |
| 3615 | ≥0 to <60 (mention two groups) | Both | USA | 30–34 (21%) and ≥ 35 (16%) | [37] |
| 4469 | >18 | F (600)/M (3730) Not reported (139) | USA | 27.1 ± 5.4 Overweight | [38] |
| 2466 | 67 (54–78) | F (42%)/M (58%) | USA | 27.9 (24.3–32.6)/Overweight | [39] |
| 383 | 28–62 | F(52.2%)/M (47.8%) | China | <18.5 (4.2%) 18.5–23.9 (53.1%) 24.0–27.9 (32.0%) >28.0 (10.7%) | [40] |
| 96 | 17–62 | F (45.0%)/M (54.9%) | China | <24 (61.45%) and ≥24 (38.55%) | [41] |
| 49 | 60.3 ± 11.8 | F (42.8%)/M (57.1%) | Spain | 28.40 ± 3.34/Overweight 25–29.9 (59.2%) >30 (24.5%) | [42] |
| 663 | 64 (56–72) | F (33.1%)/M (66.8%) | Spain | 28.3 (25.5–32.2)/Overweight | [43] |
| 15,111 | 69.4 (18–102) | F (42.8%)/M (57.2%) | Spain | >30 (21.2%) | [44] |
| 118 | 60.16 | F (44.1%)/M (55.9%) | Spain | 29.7 ± 5.79/Overweight >30.0 (41%) >25.0–29.9 (37.3%) | [45] |
| 242 | 64 (56–71) | F (18.2%)/M (80.2%) | Italy | 27.7 (25.4–29.7)/Overweight | [46] |
| 50 | 50.5 | F (30%)/M (70%) | Mexico | 28 ± 3/Overweight | [47] |
| No of Patients | Age | Sex | Country | Anthropometric Parameters | References |
|---|---|---|---|---|---|
| 1 | 73 | F | USA | Obesity | [49] |
| 33 | 41.8 ± 14.1 | F (48.5%)/M (51.5%) | China | 9.1% obesity | [50] |
| 46 | 10–24 | F (47.3%)/M (52.7%) | China | 8.7% underweight 52.0% normal 37.0% overweight/obesity | [51] |
| 129 | 54–100 a 22–79 b 52–88 c | F (65.4%)/M (34.6%) a F (79.4%)/M (20.6%) b F (28.6%)/M (71.4%) c | USA | 33.3% obesity a 0% obesity b 3% obesity c | [52] |
| 1 | 59 | F | Ecuador | Obesity class III | [53] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ovalle, D.L.P.; Rodrigo-Cano, S.; González, A.; Soler, C.; Catalá-Gregori, A.I.; Merino-Torres, J.F.; Soriano, J.M. COVID Obesity: A One-Year Narrative Review. Nutrients 2021, 13, 2060. https://doi.org/10.3390/nu13062060
Ovalle DLP, Rodrigo-Cano S, González A, Soler C, Catalá-Gregori AI, Merino-Torres JF, Soriano JM. COVID Obesity: A One-Year Narrative Review. Nutrients. 2021; 13(6):2060. https://doi.org/10.3390/nu13062060
Chicago/Turabian StyleOvalle, Diana L. Palacios, Susana Rodrigo-Cano, Aránzazu González, Carla Soler, Ana I. Catalá-Gregori, J. Francisco Merino-Torres, and Jose M. Soriano. 2021. "COVID Obesity: A One-Year Narrative Review" Nutrients 13, no. 6: 2060. https://doi.org/10.3390/nu13062060
APA StyleOvalle, D. L. P., Rodrigo-Cano, S., González, A., Soler, C., Catalá-Gregori, A. I., Merino-Torres, J. F., & Soriano, J. M. (2021). COVID Obesity: A One-Year Narrative Review. Nutrients, 13(6), 2060. https://doi.org/10.3390/nu13062060







