The Impact of COVID-19 Lockdown on Patients with Obesity after Intensive Cognitive Behavioral Therapy—A Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
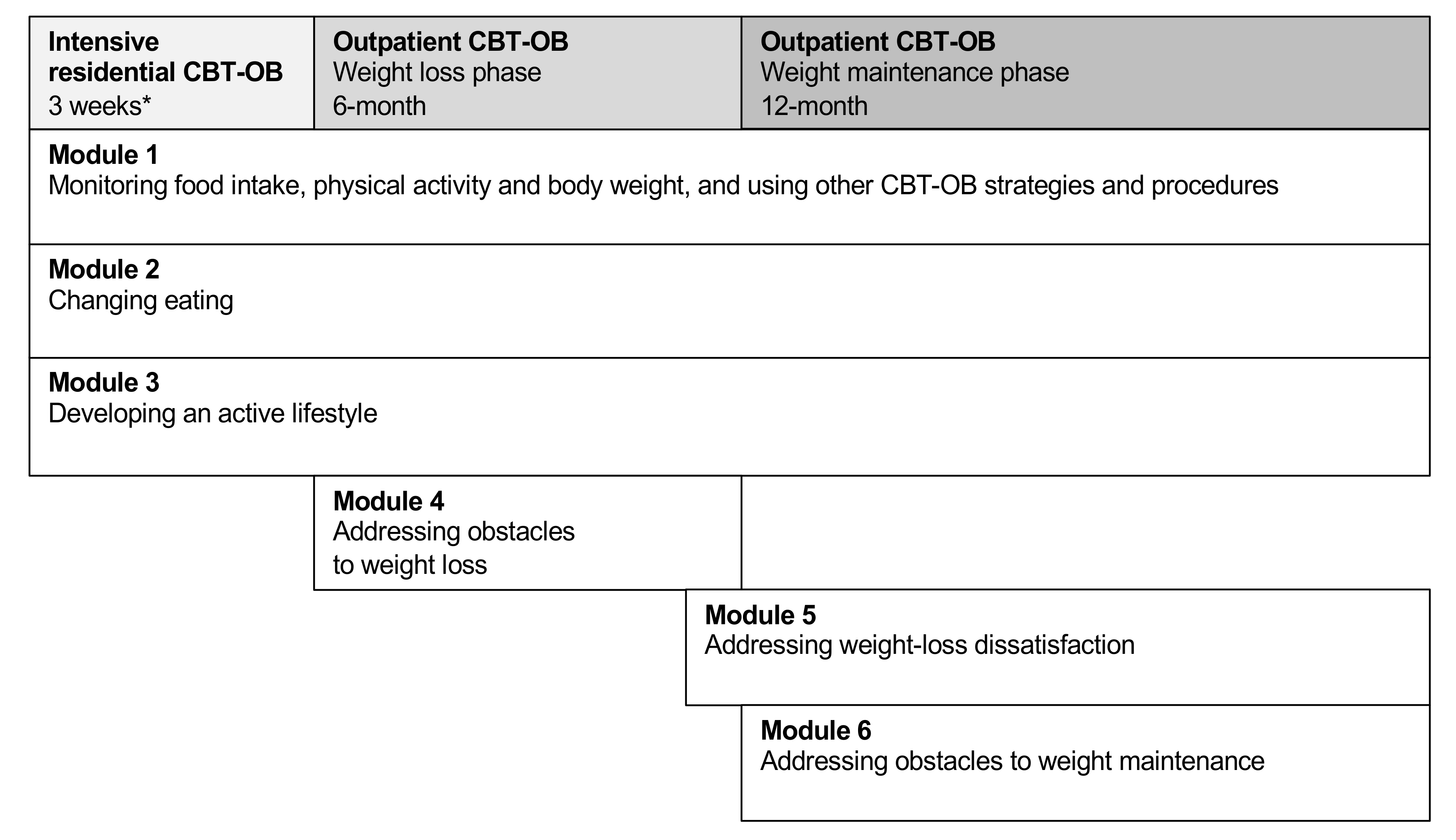
2.1. Intensive Residential CBT-OB
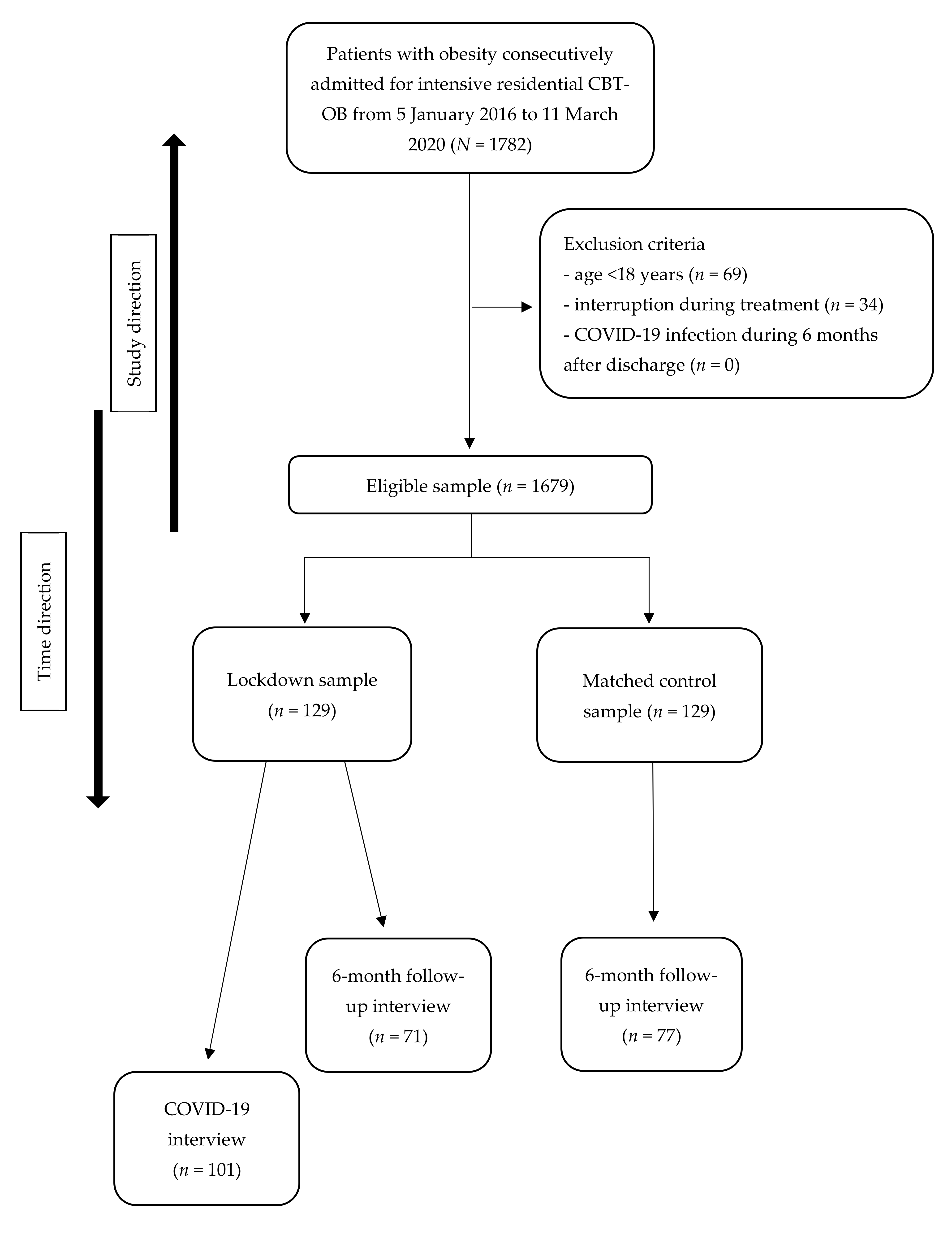
2.2. Study Design and Participants
2.3. Assessment
2.3.1. Case Report Form
2.3.2. Bodyweight and Height
2.3.3. Appropriateness of Residential Treatment
2.3.4. Eating Disorder Psychopathology and Behaviors
2.3.5. General Psychiatric Features
2.3.6. 6-Month Follow-Up Interview
2.3.7. COVID-19 Interview
2.4. Statistical Analysis
3. Results
3.1. Follow-Up Completion
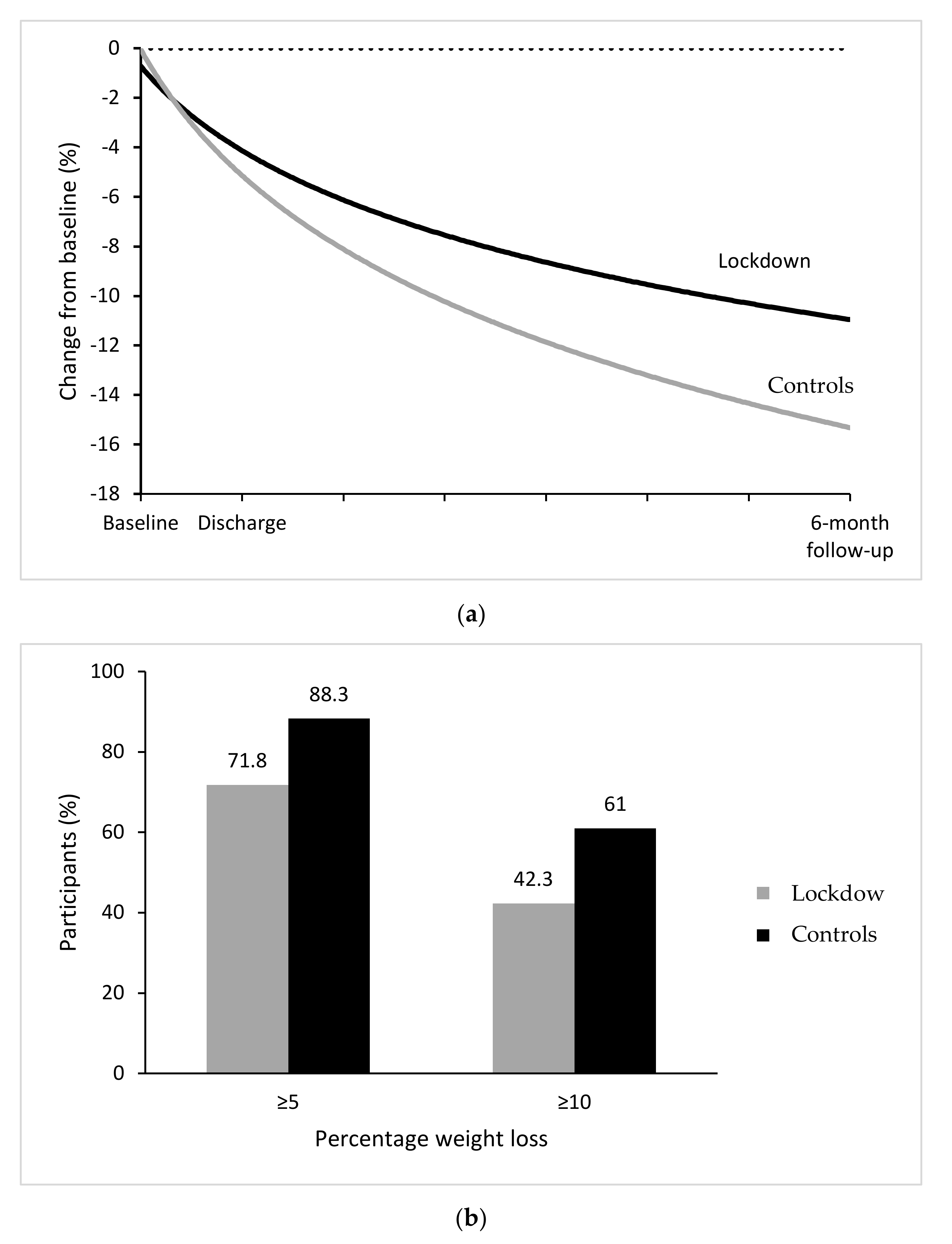
3.2. Response to Treatment
3.3. COVID-19 Interview for Lockdown Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- 001
- Patient Number (ID)
- 003
- Interview Date
- 004
- Interviewer’s Name
- 005
- Interview Outcome (1 = tracked down; 2 = refuses telephone contact; 3 = not found/unreliable data)
- 006
- Have you ever been diagnosed with COVID-19? (0 no, 1 yes)If yes, end the call by thankingIf no, continue the call
- 007
- During the COVID-19 lockdown, were you shielding?
- 008
- During the COVID-19 lockdown, did you stop working or lose your job? (0 no, 1 yes, I was not working before the lockdown)
- During the COVID-19 lockdown, did you continue to go to work outside your home? (0 no, 1 yes)
- During the COVID-19 lockdown, did you continue to work remotely from home (smart working)? (0 no, 1 yes)
- 009
- During the COVID-19 lockdown, did you worry about not having enough food available? (0 no, 1 yes)
- 0010
- During the COVID-19 lockdown, did you accumulate more food than you normally would? (0 no, 1 yes)
- 0011
- During the COVID-19 lockdown, how often did you follow the “regular eating” procedure (3 planned meals + 2 snacks and not eating between)? (0 = never; 1 = rarely; 2 = sometimes; 3 = often; 4 = always)
- 0012
- During the COVID-19 lockdown, how often did you stick to your calorie goals set at Villa Garda? (0 = never; 1= rarely; 2= sometimes; 3= often; 4= always)
- 0013
- During the COVID-19 lockdown, how often did you exercise? (0= never; 1= rarely; 2= sometimes; 3= often; 4= always)
References
- Kassir, R. Risk of COVID-19 for patients with obesity. Obes. Rev. 2020, 21. [Google Scholar] [CrossRef]
- Dietz, W.; Santos-Burgoa, C. Obesity and its Implications for COVID-19 Mortality. Obesity 2020, 28, 1005. [Google Scholar] [CrossRef] [PubMed]
- Muscogiuri, G.; Pugliese, G.; Barrea, L.; Savastano, S.; Colao, A. Commentary: Obesity: The “Achilles heel” for COVID-19? Metabolism 2020, 108, 154251. [Google Scholar] [CrossRef] [PubMed]
- Caussy, C.; Wallet, F.; Laville, M.; Disse, E. Obesity is Associated with Severe Forms of COVID-19. Obesity 2020, 28, 1175. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Hu, J.; Zhu, C. Obesity aggravates COVID-19: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Ryan, D.H.; Ravussin, E.; Heymsfield, S. COVID 19 and the Patient with Obesity—The Editors Speak Out. Obesity 2020, 28, 847. [Google Scholar] [CrossRef]
- Clemmensen, C.; Petersen, M.B.; Sørensen, T.I.A. Will the COVID-19 pandemic worsen the obesity epidemic? Nat. Rev. Endocrinol. 2020, 16, 469–470. [Google Scholar] [CrossRef] [PubMed]
- Chua, M.W.J.; Zheng, S. Obesity and COVID-19: The clash of two pandemics. Obes. Res. Clin. Pract. 2020, 14, 380–382. [Google Scholar] [CrossRef]
- Maffetone, P.B.; Laursen, P.B. The Perfect Storm: Coronavirus (Covid-19) Pandemic Meets Overfat Pandemic. Front. Public Health 2020, 8, 135. [Google Scholar] [CrossRef]
- Parekh, N.; Deierlein, A.L. Health behaviours during the coronavirus disease 2019 pandemic: Implications for obesity. Public Health Nutr. 2020, 23, 3121–3125. [Google Scholar] [CrossRef]
- Ghanemi, A.; Yoshioka, M.; St-Amand, J. Will an obesity pandemic replace the coronavirus disease-2019 (COVID-19) pandemic? Med. Hypotheses 2020, 144, 110042. [Google Scholar] [CrossRef]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The Impact of COVID-19 Stay-At-Home Orders on Health Behaviors in Adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef]
- Grannell, A.; Le Roux, C.W.; McGillicuddy, D. “I am terrified of something happening to me” The lived experience of people with obesity during the COVID-19 pandemic. Clin. Obes. 2020, 10, e12406. [Google Scholar] [CrossRef] [PubMed]
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Gazda, C.; Ofori, A.; Kukreja, S.; Messiah, S.E. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin. Obes. 2020, 10, e12386. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, M.; Ponzo, V.; Rosato, R.; Scumaci, E.; Goitre, I.; Benso, A.; Belcastro, S.; Crespi, C.; De Michieli, F.; Ghigo, E.; et al. Changes in Weight and Nutritional Habits in Adults with Obesity during the “Lockdown” Period Caused by the COVID-19 Virus Emergency. Nutrients 2020, 12, 2016. [Google Scholar] [CrossRef]
- Dalle Grave, R.; Sartirana, M.; El Ghoch, M.; Calugi, S. Treating Obesity with Personalized Cognitive Behavioral Therapy; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Dalle Grave, R.; Sartirana, M.; Calugi, S. Personalized cognitive-behavioural therapy for obesity (CBT-OB): Theory, strategies and procedures. Biopsychosoc. Med. 2020, 14, 5. [Google Scholar] [CrossRef] [PubMed]
- Dalle Grave, R. Perdere e Mantenere il Peso Con il Programma di Villa Garda; Positive Press: Verona, Italy, 2017. [Google Scholar]
- Donini, L.M.; Dalle Grave, R.; Di Flaviano, E.; Gentile, M.G.; Mezzani, B.; Pandolfo Mayme, M.; Brunani, A.; Rovera, G.; Santini, F.; Lenzi, A.; et al. Assessing the appropriateness of the level of care for morbidly obese subjects: Validation of the CASCO-R scale. Ann. Ig. 2014, 26, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Cooper, Z.; O’Connor, M. Eating Disorder Examination Questionnaire (EDE-Q 6.0). In Cognitive Behavior Therapy and Eating Disorders; Fairburn, C.G., Ed.; Guilford Press: New York, NY, USA, 2008; pp. 309–313. [Google Scholar]
- Calugi, S.; Sartirana, M.; Milanese, C.; El Ghoch, M.; Riolfi, F.; Dalle Grave, R. The clinical impairment assessment questionnaire: Validation in Italian patients with eating disorders. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2018, 23, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Calugi, S.; Ricca, V.; Castellini, G.; Lo Sauro, C.; Ruocco, A.; Chignola, E.; El Ghoch, M.; Dalle Grave, R. The Eating Disorder Examination: Reliability and validity of the Italian version. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2015, 20, 505–511. [Google Scholar] [CrossRef]
- Derogatis, L.R. SCL-90-R: Administration, Scoring and Procedures Manual; National Computer Systems: Minneapolis, MN, USA, 1994. [Google Scholar]
- Sarno, I.; Preti, E.; Prunas, A.; Madeddu, F. SCL-90-R: Symptom Check List 90 R. Versione Italiana Validata e Standardizzata; Giunti OS: Firenze, Italy, 2011. [Google Scholar]
- Marchitelli, S.; Mazza, C.; Lenzi, A.; Ricci, E.; Gnessi, L.; Roma, P. Weight Gain in a Sample of Patients Affected by Overweight/Obesity with and without a Psychiatric Diagnosis during the Covid-19 Lockdown. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Abbas, A.M.; Kamel, M.M. Dietary habits in adults during quarantine in the context of COVID-19 pandemic. Obes. Med. 2020, 19, 100254. [Google Scholar] [CrossRef]
- Alhusseini, N.; Alqahtani, A. COVID-19 pandemic’s impact on eating habits in Saudi Arabia. J. Public Health Res. 2020, 9, 1868. [Google Scholar] [CrossRef]
- AlMughamis, N.; AlAsfour, S.; Mehmood, S. Poor eating habits and predictors of weight gain during the COVID-19 quarantine measures in Kuwait: A cross sectional study [version 1; peer review: 2 approved with reservations]. F1000Research 2020, 9, 914. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Chopra, S.; Ranjan, P.; Malhotra, A.; Sahu, A.; Dwivedi, S.N.; Baitha, U.; Goel, A.; Kumar, A. Development and validation of a questionnaire to evaluate the impact of COVID-19 on lifestyle-related behaviours: Eating habits, activity and sleep behaviour. Public Health Nutr. 2021, 24, 1275–1290. [Google Scholar] [CrossRef] [PubMed]
- Wadden, T.A.; Tronieri, J.S.; Butryn, M.L. Lifestyle modification approaches for the treatment of obesity in adults. Am. Psychol. 2020, 75, 235–251. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite 2021, 156, 104853. [Google Scholar] [CrossRef]
- Bennett, G.; Young, E.; Butler, I.; Coe, S. The Impact of Lockdown During the COVID-19 Outbreak on Dietary Habits in Various Population Groups: A Scoping Review. Front. Nutr. 2021, 8, 626432. [Google Scholar] [CrossRef] [PubMed]
- Dalle Grave, R.; Calugi, S.; Marchesini, G. The influence of cognitive factors in the treatment of obesity: Lessons from the QUOVADIS study. Behav. Res. Ther. 2014, 63, 157–161. [Google Scholar] [CrossRef]
| Lockdown Patients (n = 129) | Control Patients (n = 129) | t Test, Mann–Whitney or Chi-Squared Test | p-Value | |
|---|---|---|---|---|
| Gender, % women | 90 (69.8%) | 90 (69.8%) | -- | -- |
| Age, y | 57.0 (14.2) | 56.5 (14.0) | Z = 0.33 | 0.742 |
| Body Mass Index, kg/m2 | 41.6 (8.3) | 42.2 (8.1) | Z = 0.72 | 0.474 |
| EDE-Q global score | 2.5 (1.2) | 2.6 (1.1) | t = 0.92 | 0.354 |
| EDE-Q restraint | 1.7 (1.5) | 1.6 (1.3) | Z = 0.40 | 0.689 |
| EDE-Q eating concern | 1.7 (1.4) | 1.8 (1.3) | Z = 0.77 | 0.443 |
| EDE-Q weight concern | 3.0 (1.4) | 3.2 (1.3) | Z = 1.36 | 0.174 |
| EDE-Q shape concern | 3.5 (1.6) | 3.9 (1.6) | Z = 1.85 | 0.065 |
| EDE-Q objective binge-eating episodes, mean (SD), if present | 8.2 (8.0) | 11.5 (19.5) | χ2 = 1.45 | 0.148 |
| EDE-Q self-induced vomiting, mean (SD), if present | 5.6 (3.8) | 5.8 (4.6) | χ2 = 0.07 | 0.942 |
| EDE-Q laxative misuse, mean (SD), if present | 4.0 (2.6) | 14.0 (10.9) | χ2 = 1.52 | 0.166 |
| EDE-Q excessive exercise, mean (SD), if present | 8.2 (6.2) | 6.0 (5.6) | χ2 = 1.23 | 0.227 |
| SCL-90-R global score | 0.83 (0.54) | 0.78 (0.63) | Z = 1.18 | 0.237 |
| Completer Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|
| Admission | Discharge | 6-Month Follow-Up | ||||||
| Lockdown Patients (n = 71) | Control Patients (n = 77) | Lockdown Patients (n = 71) | Control Patients (n = 77) | Lockdown Patients (n = 71) | Control Patients (n = 77) | Repeated-Measures ANOVA | ||
| Time | TimeXGroup | |||||||
| Bodyweight in kg, mean (SD) | 111.7 (22.9) | 117.0 (22.2) | 106.5 (21.7) | 111.8 (21.1) | 101.1 (22.0) | 101.6 (19.7) | <0.001 | 0.002 |
| Body mass index in kg/m2, mean (SD) | 40.9 (7.4) | 43.2 (6.8) | 39.1 (7.1) | 41.3 (6.6) | 37.0 (7.2) | 37.6 (6.6) | <0.001 | 0.002 |
| t-test; p-value discharge | t-test; p-value 6-month follow-up | |||||||
| Weight loss from admission in kg, mean (SD) | -- | -- | 5.2 (3.5) | 5.2 (2.8) | 10.6 (9.2) | 15.3 (9.3) | 0.16; 0.872 | 3.09; 0.002 |
| Percentage weight loss from admission, mean (SD) | -- | -- | 4.6 (3.1) | 4.3 (2.0) | 9.4 (7.5) | 13.0 (7.1) | 0.65; 0.514 | 2.94; 0.004 |
| Chi-squared test; p-value discharge | Chi-squared test; p-value 6-month follow-up | |||||||
| ≥5% weight loss from admission, n (%) | -- | -- | 20 (28.2%) | 25 (32.5%) | 51 (71.8%) | 68 (88.3%) | 0.32; 0.570 | 6.37; 0.012 |
| ≥10% weight loss from admission, n (%) | -- | -- | 1 (1.4%) | 1 (1.3%) | 30 (42.3%) | 47 (61.0%) | 0.003; 0.954 | 5.22; 0.022 |
| Intention-to-Treat Analysis | ||||||||
| Admission | Discharge | 6-Month Follow-Up | Repeated-Measures ANOVA | |||||
| Time | TimeXGroup | |||||||
| Lockdown Patients (n = 129) | Control Patients (n = 129) | Lockdown Patients (n = 129) | Control Patients (n = 129) | Lockdown Patients (n = 129) | Control Patients (n = 129) | |||
| Bodyweight in kg, mean (SD) | 112.5 (23.0) | 115.5 (24.7) | 107.4 (21.8) | 110.5 (23.4) | 101.3 (22.6) | 101.2 (22.4) | <0.001 | <0.001 |
| Body mass index in kg/m2, mean (SD) | 41.6 (8.2) | 42.2 (8.1) | 39.9 (7.9) | 40.4 (7.7) | 37.5 (8.3) | 37.1 (7.8) | <0.001 | <0.001 |
| t-test; p-value discharge | t-test; p-value 6-month follow-up | |||||||
| Weight loss from admission in kg, mean (SD) | -- | -- | 5.06 (2.9) | 5.07 (2.8) | 11.1 (10.0) | 14.4 (10.2) | 0.12; 0.908 | 8.45; <0.001 |
| Percentage weight loss from admission, mean (SD) | -- | -- | 4.5 (2.4) | 4.3 (2.1) | 9.9 (8.6) | 12.3 (8.2) | 1.88; 0.060 | 7.36; <0.001 |
| Chi-squared test; p-value discharge | Chi-squared test; p-value 6-month follow-up | |||||||
| ≥5% weight loss from admission, n (%) | -- | -- | 37 (28.7%) | 42 (32.6%) | 92 (71.3%) | 106 (82.2%) | 5.02; 0.025 | 44.6; <0.001 |
| ≥10% weight loss from admission, n (%) | -- | -- | 1 (0.8%) | 1 (0.8%) | 59 (45.8%) | 76 (58.9%) | -- | 48.6; <0.001 |
| Admission | 6-Month Follow-Up | |||||
| Lockdown Patients (n = 71) | Control Patients (n = 77) | Lockdown Patients (n = 71) | Control Patients (n = 77) | Chi-Squared Test; p-Value between Groups | Sign Test; p-Value within Groups | |
| Objective binge-eating episodes, n (%) No episodes Fewer than 1 episode per week 1 episode per week 2–3 episodes per week 4–7 episodes per week 8–13 episodes per week 14 or more episodes per week | 24 (33.8) 16 (22.5) 17 (23.9) 8 (11.3) 6 (8.5) 0 0 | 23 (30.3) 15 (19.7) 16 (21.1) 10 (13.2) 11 (14.5) 0 1 (1.3) | 58 (81.7) 6 (8.5) 3 (4.2) 2 (2.8) 1 (1.4) 1 (1.4) 0 | 66 (86.8) 6 (7.9) 2 (2.6) 2 (2.6) 0 0 0 | Admission: 2.61; 0.760 6-month follow-up: 2.55; 0.769 | Lockdown: 5.18; <0.001 Control: 6.72; <0.001 |
| During the COVID-19 Lockdown… | |
|---|---|
| …were you shielding | No, n = 99/101 (98%) Yes, n = 2/101 (2%) |
| …did you stop working or lose your job | I was not working before the lockdown, n = 45/101 (44.5%) No, n = 35/56 (62.5%) Yes, n = 19/56 (30.4%) |
| …did you continue to go to work outside your home | No, n = 17/35 (48.6%) Yes, n = 17/35 (48.6%) Both, n = 1/35 (2.8%) |
| …did you continue to work remotely from home (smart working) | No, n = 17/35 (48.6%) Yes, n = 17/35 (48.6%) Both, n = 1/35 (2.8%) |
| …did you worry about not having enough food available | No, n = 94/101 (93.1%) Yes, n = 7/101 (6.9%) |
| …did you accumulate more food than you normally would | No, n = 67/101 (66.3%) Yes, n = 34/35 (33.7%) |
| … how often did you follow the “regular eating” procedure (3 planned meals + 2 snacks and not eating between) | Never, n = 22/101 (21.8%) Rarely, n = 8/101 (7.9%) Sometimes, n = 21/101 (20.8%) Often, n = 22/101 (21.8%) Always, n = 28/101 (27.7%) |
| …how often did you stick to your calorie goals set at Villa Garda | Never, n = 26/101 (25.7%) Rarely, n = 9/101 (8.9%) Sometimes, n = 17/101 (16.8%) Often, n = 18/101 (17.8%) Always, n = 31/101 (30.7%) |
| … how often did you exercise | Never, n = 29/101 (28.7%) Rarely, n = 10/101 (9.9%) Sometimes, n = 13/101 (12.9%) Often, n = 26/101 (25.7%) Always, n = 23/101 (22.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calugi, S.; Andreoli, B.; Dametti, L.; Dalle Grave, A.; Morandini, N.; Dalle Grave, R. The Impact of COVID-19 Lockdown on Patients with Obesity after Intensive Cognitive Behavioral Therapy—A Case-Control Study. Nutrients 2021, 13, 2021. https://doi.org/10.3390/nu13062021
Calugi S, Andreoli B, Dametti L, Dalle Grave A, Morandini N, Dalle Grave R. The Impact of COVID-19 Lockdown on Patients with Obesity after Intensive Cognitive Behavioral Therapy—A Case-Control Study. Nutrients. 2021; 13(6):2021. https://doi.org/10.3390/nu13062021
Chicago/Turabian StyleCalugi, Simona, Beatrice Andreoli, Laura Dametti, Anna Dalle Grave, Nicole Morandini, and Riccardo Dalle Grave. 2021. "The Impact of COVID-19 Lockdown on Patients with Obesity after Intensive Cognitive Behavioral Therapy—A Case-Control Study" Nutrients 13, no. 6: 2021. https://doi.org/10.3390/nu13062021
APA StyleCalugi, S., Andreoli, B., Dametti, L., Dalle Grave, A., Morandini, N., & Dalle Grave, R. (2021). The Impact of COVID-19 Lockdown on Patients with Obesity after Intensive Cognitive Behavioral Therapy—A Case-Control Study. Nutrients, 13(6), 2021. https://doi.org/10.3390/nu13062021







