Using Exercise and Nutrition to Alter Fat and Lean Mass in Men with Prostate Cancer Receiving Androgen Deprivation Therapy: A Narrative Review
Abstract
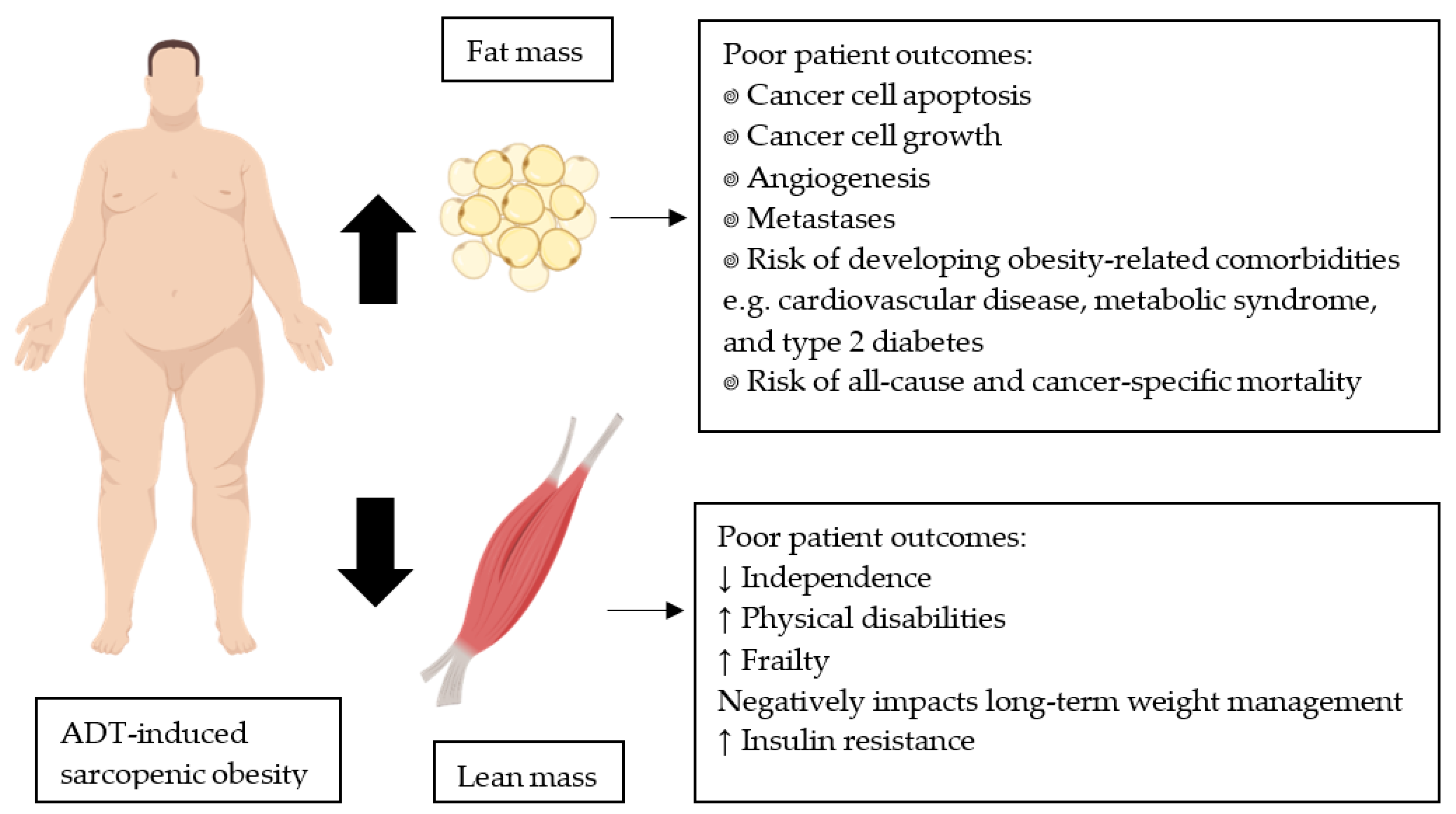
1. Introduction
2. Using Exercise to Decrease Fat Mass and Preserve or Gain Lean Mass
2.1. Aerobic Exercise
2.2. Resistance Exercise
2.3. Multi-Modal Interventions
3. Using Nutrition to Decrease Fat Mass and Preserve or Gain Lean Mass
3.1. Healthy Eating Guidelines and/or Energy Deficit
3.2. Protein Intake
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rhee, H.; Gunter, J.H.; Heathcote, P.; Ho, K.; Stricker, P.; Corcoran, N.M.; Nelson, C.C. Adverse effects of androgen-deprivation therapy in prostate cancer and their management. BJU Int. 2014, 115, 3–13. [Google Scholar] [CrossRef]
- Labrie, F.; Dupont, A.; Bélanger, A.; St-Arnaud, R.; Giguère, M.; Lacourcière, Y.; Emond, J.; Monfette, G. Treatment of prostate cancer with gonadotropin-releasing hormone agonists. Endocr. Rev. 1986, 7, 67–74. [Google Scholar] [CrossRef]
- Herbst, K.L.; Bhasin, S. Testosterone action on skeletal muscle. Curr. Opin. Clin. Nutr. Metab. Care 2004, 7, 271–277. [Google Scholar] [CrossRef]
- Saad, F.; Aversa, A.; Isidori, A.M.; Gooren, L.J. Testosterone as potential effective therapy in treatment of obesity in men with testosterone deficiency: A review. Curr. Diabetes Rev. 2012, 8, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Galvão, D.A.; Spry, N.A.; Taaffe, D.R.; Newton, R.U.; Stanley, J.; A Shannon, T.; Rowling, C.; Prince, R.L. Changes in muscle, fat and bone mass after 36 weeks of maximal androgen blockade for prostate cancer. BJU Int. 2008, 102, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Galvao, D.; Taaffe, D.; Spry, N.; Joseph, D.; Turner, D.; Newton, R. Reduced muscle strength and functional performance in men with prostate cancer undergoing androgen suppression: A comprehensive cross-sectional investigation. Prostate Cancer Prostatic Dis. 2008, 12, 198–203. [Google Scholar] [CrossRef]
- Keating, N.L.; O’Malley, A.J.; Freedland, S.J.; Smith, M.R. Diabetes and cardiovascular disease during androgen deprivation therapy: Observational study of veterans with prostate cancer. J. Natl. Cancer Inst. 2009, 102, 39–46. [Google Scholar] [CrossRef]
- Cao, Y.; Ma, J. Body Mass Index, Prostate Cancer–Specific Mortality, and Biochemical Recurrence: A Systematic Review and Meta-analysis. Cancer Prev. Res. 2011, 4, 486–501. [Google Scholar] [CrossRef]
- Joshu, C.E.; Mondul, A.M.; Menke, A.; Meinhold, C.; Han, M.; Humphreys, E.B.; Freedland, S.J.; Walsh, P.C.; Platz, E.A. Weight gain is associated with an increased risk of prostate cancer recurrence after prostatectomy in the psa era. Cancer Prev. Res. 2011, 4, 544–551. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund. American Institute for Cancer Research. Continuous Update Project Expert Report 2018. Diet, Nutrition, Physical Activity and Prostate Cancer. Available online: https://www.wcrf.org/dietandcancer/prostate-cancer (accessed on 20 May 2020).
- Rhee, H.; Vela, I.; Chung, E. Metabolic syndrome and prostate cancer: A review of complex interplay amongst various endocrine factors in the pathophysiology and progression of prostate cancer. Horm. Cancer 2015, 7, 75–83. [Google Scholar] [CrossRef]
- Deng, T.; Lyon, C.J.; Bergin, S.; Caligiuri, M.A.; Hsueh, W.A. Obesity, inflammation, and cancer. Annu. Rev. Pathol. Mech. Dis. 2016, 11, 421–449. [Google Scholar] [CrossRef] [PubMed]
- Troeschel, A.N.; Hartman, T.J.; Jacobs, E.J.; Stevens, V.L.; Gansler, T.; Flanders, W.D.; McCullough, L.E.; Wang, Y. Postdiagnosis body mass index, weight change, and mortality from prostate cancer, cardiovascular disease, and all causes among survivors of nonmetastatic prostate cancer. J. Clin. Oncol. 2020, 38, 2018–2027. [Google Scholar] [CrossRef]
- Newton, R.U.; Jeffery, E.; Galvão, D.A.; Peddle-McIntyre, C.J.; Spry, N.; Joseph, D.; Denham, J.W.; Taaffe, D.R.; Denham, J. Body composition, fatigue and exercise in patients with prostate cancer undergoing androgen-deprivation therapy. BJU Int. 2018, 122, 986–993. [Google Scholar] [CrossRef]
- Galvão, D.A.; Taaffe, D.R.; Spry, N.; Joseph, D.; Newton, R.U. Acute versus chronic exposure to androgen suppression for prostate cancer: Impact on the exercise response. J. Urol. 2011, 186, 1291–1297. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, R.N. Body composition in healthy aging. Ann. N. Y. Acad. Sci. 2006, 904, 437–448. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European working group on sarcopenia in older people. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Hills, A.P.; Emokhtar, N.; Byrne, N.M. Assessment of physical activity and energy expenditure: An overview of objective measures. Front. Nutr. 2014, 1, 5. [Google Scholar] [CrossRef]
- Dieli-Conwright, C.M.; Courneya, K.S.; Demark-Wahnefried, W.; Sami, N.; Lee, K.; Buchanan, T.A.; Spicer, D.V.; Tripathy, D.; Bernstein, L.; Mortimer, J.E. Effects of aerobic and resistance exercise on metabolic syndrome, sarcopenic obesity, and circulating biomarkers in overweight or obese survivors of breast cancer: A randomized controlled trial. J. Clin. Oncol. 2018, 36, 875–883. [Google Scholar] [CrossRef]
- Barnard, R.J.; Ngo, T.H.; Leung, P.-S.; Aronson, W.J.; Golding, L.A. A low-fat diet and/or strenuous exercise alters the IGF axis in vivo and reduces prostate tumor cell growth in vitro. Prostate 2003, 56, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, T.; Paulsen, S.K.; Bruun, J.M.; Pedersen, S.B.; Richelsen, B. Exercise training versus diet-induced weight-loss on metabolic risk factors and inflammatory markers in obese subjects: A 12-week randomized intervention study. Am. J. Physiol. Metab. 2010, 298, E824–E831. [Google Scholar] [CrossRef]
- Bourke, L.; Smith, D.; Steed, L.; Hooper, R.; Carter, A.; Catto, J.; Albertsen, P.C.; Tombal, B.; Payne, H.A.; Rosario, D.J. Exercise for men with prostate cancer: A systematic review and meta-analysis. Eur. Urol. 2016, 69, 693–703. [Google Scholar] [CrossRef]
- Tsang, D.S.; Alibhai, S.M.H. Bone health care for patients with prostate cancer receiving androgen deprivation therapy. Hosp. Pract. 2014, 42, 89–102. [Google Scholar] [CrossRef]
- Hackshaw-McGeagh, L.E.; Perry, R.E.; Leach, V.A.; Qandil, S.; Jeffreys, M.; Martin, R.M.; Lane, J.A. A systematic review of dietary, nutritional, and physical activity interventions for the prevention of prostate cancer progression and mortality. Cancer Causes Control. 2015, 26, 1521–1550. [Google Scholar] [CrossRef]
- Barnes, K.A.; Ball, L.E.; Galvao, D.A.; Newton, R.U.; Chambers, S.K. Nutrition care guidelines for men with prostate cancer undergoing androgen deprivation therapy: Do we have enough evidence? Prostate Cancer Prostatic Dis. 2019, 22, 221–234. [Google Scholar] [CrossRef]
- Falcone, P.H.; Tai, C.-Y.; Carson, L.R.; Joy, J.M.; Mosman, M.M.; McCann, T.R.; Crona, K.P.; Kim, M.P.; Moon, J.R. Caloric expenditure of aerobic, resistance, or combined high-intensity interval training using a hydraulic resistance system in healthy men. J. Strength Cond. Res. 2015, 29, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Collins, K.H.; Herzog, W.; Macdonald, G.Z.; Reimer, R.A.; Rios, J.L.; Smith, I.C.; Zernicke, R.F.; Hart, D.A. Obesity, metabolic syndrome, and musculoskeletal disease: Common inflammatory pathways suggest a central role for loss of muscle integrity. Front. Physiol. 2018, 9, 112. [Google Scholar] [CrossRef]
- Skolarus, T.A.; Wolf, A.M.; Erb, N.L.; Brooks, D.D.; Rivers, B.M.; Underwood, W.; Salner, A.L.; Zelefsky, M.J.; Aragon-Ching, J.B.; Slovin, S.F.; et al. American Cancer Society prostate cancer survivorship care guidelines. CA Cancer J. Clin. 2014, 64, 225–249. [Google Scholar] [CrossRef]
- Hvid, T.; Winding, K.; Rinnov, A.; Dejgaard, T.; Thomsen, C.; Iversen, P.; Brasso, K.; Mikines, K.J.; Van Hall, G.; Lindegaard, B.; et al. Endurance training improves insulin sensitivity and body composition in prostate cancer patients treated with androgen deprivation therapy. Endocr. Relat. Cancer 2013, 20, 621–632. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.S.; Hoermann, R.; Dupuis, P.; Joon, D.L.; Zajac, J.D.; Grossmann, M. Relationships between insulin resistance and frailty with body composition and testosterone in men undergoing androgen deprivation therapy for prostate cancer. Eur. J. Endocrinol. 2016, 175, 229–237. [Google Scholar] [CrossRef]
- Chang, D.; Joseph, D.J.; Ebert, M.A.; Galvão, D.A.; Taaffe, D.R.; Denham, J.W.; Newton, R.U.; Spry, N.A. Effect of androgen deprivation therapy on muscle attenuation in men with prostate cancer. J. Med. Imaging Radiat. Oncol. 2013, 58, 223–228. [Google Scholar] [CrossRef]
- Alberga, A.S.; Segal, R.J.; Reid, R.D.; Scott, C.G.; Sigal, R.J.; Khandwala, F.; Jaffey, J.; Wells, G.A.; Kenny, G.P. Age and androgen-deprivation therapy on exercise outcomes in men with prostate cancer. Support. Care Cancer 2012, 20, 971–981. [Google Scholar] [CrossRef] [PubMed]
- Mina, D.S.; Alibhai, S.M.; Matthew, A.G.; Guglietti, C.L.; Pirbaglou, M.; Trachtenberg, J.; Ritvo, P.; Alibhai, S.M. A randomized trial of aerobic versus resistance exercise in prostate cancer survivors. J. Aging Phys. Act. 2013, 21, 455–478. [Google Scholar] [CrossRef] [PubMed]
- Mina, D.S.; Connor, M.K.; Alibhai, S.M.; Toren, P.; Guglietti, C.; Matthew, A.G.; Trachtenberg, J.; Ritvo, P. Exercise effects on adipokines and the IGF axis in men with prostate cancer treated with androgen deprivation: A randomized study. Can. Urol. Assoc. J. 2013, 7, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Uth, J.; Hornstrup, T.; Schmidt, J.F.; Christensen, J.F.; Frandsen, C.; Christensen, K.B.; Helge, E.W.; Brasso, K.; Rørth, M.; Midtgaard, J.; et al. Football training improves lean body mass in men with prostate cancer undergoing androgen deprivation therapy. Scand. J. Med. Sci. Sports 2014, 24 (Suppl. S1), 105–112. [Google Scholar] [CrossRef]
- Newton, R.U.; Galvão, D.A.; Spry, N.; Joseph, D.; Chambers, S.K.; Gardiner, R.A.; Wall, B.A.; Bolam, K.A.; Taaffe, D.R. Exercise mode specificity for preserving spine and hip BMD in prostate cancer patients. Med. Sci. Sports Exerc. 2018, 51, 607–614. [Google Scholar] [CrossRef]
- Galvão, D.A.; Nosaka, K.; Taaffe, D.R.; Spry, N.; Kristjanson, L.J.; Mcguigan, M.R.; Suzuki, K.; Yamaya, K.; Newton, R.U. Resistance training and reduction of treatment side effects in prostate cancer patients. Med. Sci. Sports Exerc. 2006, 38, 2045–2052. [Google Scholar] [CrossRef]
- Hanson, E.D.; Sheaff, A.K.; Sood, S.; Ma, L.; Francis, J.D.; Goldberg, A.P.; Hurley, B.F. Strength training induces muscle hypertrophy and functional gains in black prostate cancer patients despite androgen deprivation therapy. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2012, 68, 490–498. [Google Scholar] [CrossRef]
- Nilsen, T.S.; Raastad, T.; Skovlund, E.; Courneya, K.S.; Langberg, C.W.; Lilleby, W.; Fosså, S.D.; Thorsen, L. Effects of strength training on body composition, physical functioning, and quality of life in prostate cancer patients during androgen deprivation therapy. Acta Oncol. 2015, 54, 1805–1813. [Google Scholar] [CrossRef]
- Galvão, D.A.; Taaffe, D.R.; Spry, N.; Joseph, D.; Newton, R.U. Combined resistance and aerobic exercise program reverses muscle loss in men undergoing androgen suppression therapy for prostate cancer without bone metastases: A randomized controlled trial. J. Clin. Oncol. 2010, 28, 340–347. [Google Scholar] [CrossRef]
- Cormie, P.; Galvão, D.A.; Spry, N.; Joseph, D.; Chee, R.; Taaffe, D.R.; Chambers, S.K.; Newton, R.U. Can supervised exercise prevent treatment toxicity in patients with prostate cancer initiating androgen-deprivation therapy: A randomised controlled trial. BJU Int. 2015, 115, 256–266. [Google Scholar] [CrossRef]
- Winters-Stone, K.M.; Dieckmann, N.F.; Maddalozzo, G.F.; Bennett, J.A.; Ryan, C.W.; Beer, T.M. Resistance exercise reduces body fat and insulin during androgen-deprivation therapy for prostate cancer. Oncol. Nurs. Forum 2015, 42, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Wall, B.; Galvao, D.; Fatehee, N.; Taaffe, D.; Spry, N.; Joseph, D.; Hebert, J.; Newton, R. Exercise improves VO2max and body composition in ADT-treated prostate cancer patients. Med. Sci. Sports Exerc. 2017, 49, 333–334. [Google Scholar] [CrossRef]
- Ndjavera, W.; Orange, S.T.; O’Doherty, A.F.; Leicht, A.S.; Rochester, M.; Mills, R.; Saxton, J.M. Exercise-induced attenuation of treatment side-effects in patients with newly diagnosed prostate cancer beginning androgen-deprivation therapy: A randomised controlled trial. BJU Int. 2020, 125, 28–37. [Google Scholar] [CrossRef]
- Allott, E.H.; Masko, E.M.; Freedland, S.J. Obesity and prostate cancer: Weighing the evidence. Eur. Urol. 2013, 63, 800–809. [Google Scholar] [CrossRef]
- Weinheimer, E.M.; Sands, L.P.; Campbell, W.W. A systematic review of the separate and combined effects of energy restriction and exercise on fat-free mass in middle-aged and older adults: Implications for sarcopenic obesity. Nutr. Rev. 2010, 68, 375–388. [Google Scholar] [CrossRef]
- Batsis, J.A.; Gill, L.E.; Bs, R.K.M.; Adachi-Mejia, A.M.; Blunt, H.B.; Bagley, P.J.; Lopez-Jimenez, F.; Bartels, S.J. Weight loss interventions in older adults with obesity: A systematic review of randomized controlled trials since 2005. J. Am. Geriatr. Soc. 2017, 65, 257–268. [Google Scholar] [CrossRef]
- Lam, T.; Birzniece, V.; McLean, M.; Gurney, H.; Hayden, A.; Cheema, B.S. The adverse effects of androgen deprivation therapy in prostate cancer and the benefits and potential anti-oncogenic mechanisms of progressive resistance training. Sports Med. Open 2020, 6, 13–14. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.M.; Marin, P.J.; Rhea, M.R.; Wilson, S.M.; Loenneke, J.P.; Anderson, J.C. Concurrent training. J. Strength Cond. Res. 2012, 26, 2293–2307. [Google Scholar] [CrossRef]
- National Health Medical Research Council. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013.
- Gibson, A.L.; Wagner, D.; Heyward, V. Advanced Fitness Assessment and Exercise Prescription, 8th ed.; Human Kinetics: Champaign, IL, USA, 2018. [Google Scholar]
- Gilbert, S.E.; Tew, G.A.; Fairhurst, C.; Bourke, L.; Saxton, J.M.; Winter, E.M.; Rosario, D.J. Effects of a lifestyle intervention on endothelial function in men on long-term androgen deprivation therapy for prostate cancer. Br. J. Cancer 2016, 114, 401–408. [Google Scholar] [CrossRef]
- Focht, B.C.; Lucas, A.R.; Grainger, E.; Simpson, C.; Fairman, C.M.; Thomas-Ahner, J.M.; Buell, J.; Monk, J.P.; Mortazavi, A.; Clinton, S.K. Effects of a group-mediated exercise and dietary intervention in the treatment of prostate cancer patients undergoing androgen deprivation therapy: Results from the IDEA-P trial. Ann. Behav. Med. 2018, 52, 412–428. [Google Scholar] [CrossRef]
- O’Neill, R.F.; Haseen, F.; Murray, L.J.; O’Sullivan, J.M.; Cantwell, M.M. A randomised controlled trial to evaluate the efficacy of a 6-month dietary and physical activity intervention for patients receiving androgen deprivation therapy for prostate cancer. J. Cancer Surviv. 2015, 9, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Freedland, S.J.; Howard, L.; Allen, J.; Smith, J.; Stout, J.; Aronson, W.; Inman, B.A.; Armstrong, A.J.; George, D.; Westman, E.; et al. A lifestyle intervention of weight loss via a low-carbohydrate diet plus walking to reduce metabolic disturbances caused by androgen deprivation therapy among prostate cancer patients: Carbohydrate and prostate study 1 (CAPS1) randomized controlled trial. Prostate Cancer Prostatic Dis. 2019, 22, 428–437. [Google Scholar] [CrossRef] [PubMed]
- Baguley, B.J.; Skinner, T.L.; Jenkins, D.G.; Wright, O.R. Mediterranean-style dietary pattern improves cancer-related fatigue and quality of life in men with prostate cancer treated with androgen deprivation therapy: A pilot randomised control trial. Clin. Nutr. 2021, 40, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.L.; Newton, R.U.; Taaffe, D.R.; Hart, N.H.; Lyons-Wall, P.; Galvão, D.A. Weight loss for obese prostate cancer patients on androgen deprivation therapy. Med. Sci. Sports Exerc. 2020, 53, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.K.; Dorff, T.B.; Schroeder, E.T.; Lane, C.J.; Gross, M.E.; Dieli-Conwright, C.M. Impact of resistance training on body composition and metabolic syndrome variables during androgen deprivation therapy for prostate cancer: A pilot randomized controlled trial. BMC Cancer 2018, 18, 368. [Google Scholar] [CrossRef] [PubMed]
- Hanson, E.D.; Nelson, A.R.; West, D.W.D.; Violet, J.A.; O’Keefe, L.; Phillips, S.M.; Hayes, A. Attenuation of resting but not load-mediated protein synthesis in prostate cancer patients on androgen deprivation. J. Clin. Endocrinol. Metab. 2017, 102, 1076–1083. [Google Scholar] [CrossRef]
- Smith, J.C.; Bennett, S.; Evans, L.M.; Kynaston, H.G.; Parmar, M.; Mason, M.D.; Cockcroft, J.R.; Scanlon, M.F.; Davies, J.S. The effects of induced hypogonadism on arterial stiffness, body composition, and metabolic parameters in males with prostate cancer. J. Clin. Endocrinol. Metab. 2001, 86, 4261–4267. [Google Scholar] [CrossRef]
- Mohamad, H.; McNeill, G.; Haseen, F.; N’Dow, J.; Craig, L.C.A.; Heys, S.D. The effect of dietary and exercise interventions on body weight in prostate cancer patients: A systematic review. Nutr. Cancer 2015, 67, 43–60. [Google Scholar] [CrossRef]
- Golombos, D.M.; Ayangbesan, A.; O’Malley, P.; Lewicki, P.; Barlow, L.; Barbieri, C.E.; Chan, C.; DuLong, C.; Abu-Ali, G.; Huttenhower, C.; et al. The role of gut microbiome in the pathogenesis of prostate cancer: A prospective, pilot study. Urology 2018, 111, 122–128. [Google Scholar] [CrossRef]
- Verheggen, R.J.H.M.; Maessen, M.F.H.; Green, D.J.; Hermus, A.R.M.M.; Hopman, M.T.E.; Thijssen, D.H.T. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: Distinct effects on body weight and visceral adipose tissue. Obes. Rev. 2016, 17, 664–690. [Google Scholar] [CrossRef]
- Alamuddin, N.; Bakizada, Z.; Wadden, T.A. Management of obesity. J. Clin. Oncol. 2016, 34, 4295–4305. [Google Scholar] [CrossRef] [PubMed]
- Ferro, M.; Terracciano, D.; Buonerba, C.; Lucarelli, G.; Bottero, D.; Perdonà, S.; Autorino, R.; Serino, A.; Cantiello, F.; Damiano, R.; et al. The emerging role of obesity, diet and lipid metabolism in prostate cancer. Futur. Oncol. 2017, 13, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Foulkes, S.J.; Daly, R.M.; Fraser, S.F. The clinical importance of quantifying body fat distribution during androgen deprivation therapy for prostate cancer. Endocr. Relat. Cancer 2017, 24, R35–R48. [Google Scholar] [CrossRef]
- Henning, S.M.; Galet, C.; Gollapudi, K.; Byrd, J.B.; Liang, P.; Li, Z.; Grogan, T.; Elashoff, D.; Magyar, C.E.; Said, J.; et al. Phase II prospective randomized trial of weight loss prior to radical prostatectomy. Prostate Cancer Prostatic Dis. 2017, 21, 212–220. [Google Scholar] [CrossRef] [PubMed]
| Current Exercise and Nutrition Guidelines | Current Weight Loss Guidelines | |
|---|---|---|
 Aerobic training | 150 min/week of moderate intensity exercise or 75 min/week of vigorous intensity exercise | 300 min/week of moderate intensity exercise or 150 min/week of vigorous intensity exercise |
 Resistance training | Minimum two strength training sessions/week | |
 Nutritional intake | Healthy balanced diet with high fruit and vegetables, low saturated fats, and adequate calcium (<1200 mg/d) and vitamin D (>600 IU) | 2100–4200 kJ daily energy deficit |
| Study | Study Design | Primary Outcome | Intervention | Body Composition Assessment | Groups (N) | Outcome Variable | Mean Pre-Intervention Values (kg) | Mean Post-Intervention Values (kg) |
|---|---|---|---|---|---|---|---|---|
| Aerobic-based interventions | ||||||||
| Alberga et al. [32] | RCT | Body composition and fitness | 24 weeks 3 ×/week Supervised aerobic exercise at 50–75% HRmax or Supervised resistance exercise at 60–70% 1 RM | DXA | Aerobic (N = 40) | |||
| ADT | BF% | 31.2% | 33.3% * | |||||
| Lean mass | 65.0 | 63.0 * | ||||||
| No ADT | BF% | 29.9% | 30.5% | |||||
| Lean mass | 66.2 | 65.7 | ||||||
| Resistance (N = 40) | ||||||||
| ADT | BF% | 32.6% | 33.0% §UC | |||||
| Lean mass | 63.7 | 63.4 §UC | ||||||
| No ADT | BF% | 29.7% | 29.2% | |||||
| Lean mass | 66.7 | 67.3 | ||||||
| Usual care (N = 41) | ||||||||
| ADT | BF% | 32.0% | 35.2% §R * | |||||
| Lean mass | 64.2 | 61.1 §R * | ||||||
| No ADT | BF% | 31.2 | 30.6 | |||||
| Lean mass | 65.0 | 65.6 | ||||||
| Hvid et al. [29] | Prospective cohort | Insulin sensitivity and body composition | 12 weeks 3 ×/week 135 min/week Aerobic interval exercise 50–100% VO2max | DXA and MRI | Prostate cancer exercise (N = 9) | Fat mass | 24.4 | 23.1 # |
| Trunk fat | 14.5 | 13.4 # | ||||||
| Lean mass | 52.3 | 52.3 | ||||||
| BF% | 31.1% | 29.8% # | ||||||
| Visceral a | −8.4% # | |||||||
| Subcutaneous a | −4.9% # | |||||||
| Intermuscular a | 0% § # | |||||||
| Non-cancer exercise (N = 10) | Fat mass | 20.5 | 19.6 # | |||||
| Trunk fat | 12.4 | 11.8 # | ||||||
| Lean mass | 56.3 | 56.2 | ||||||
| BF% | 25.7% | 25.0% # | ||||||
| Visceral a | −5.8% # | |||||||
| Subcutaneous a | −2.5% # | |||||||
| Intermuscular a | −8.5% # | |||||||
| Santa Mina et al. [33] | RCT | Quality of life | 6 months 3–5 ×/week 90–300 min/week Home-based resistance band/ball/body weight exercise 12–15 RPE Or Home-based aerobic exercise at 60–80% HRmax | Skinfolds | Aerobic (N = 22) | Chest skinfold | 35.6 mm | 33.5 mm *3 |
| BF% | 28.5% | 27.3% *3 | ||||||
| Resistance (N = 34) | Chest skinfold | 35.3 mm | 33.7 mm | |||||
| BF% | 28.0% | 27.3% | ||||||
| Santa Mina et al. [34] | RCT | Blood biomarkers | See Santa Mina et al. [33] | Skinfolds | Aerobic (N = 13) | BF% | 28.4% | 26.4% |
| Resistance (N = 13) | BF% | 26.5% | 25.3% | |||||
| Uth et al. [35] | RCT | Lean mass | 12 weeks 2 ×/week (1–8 weeks) 3 ×/week (9–12 weeks) 90–180 min/week Supervised football training | DXA | Football (N= 29) | Fat mass | 27.6 | 26.3 |
| Lean mass | 53.1 | 54.0 § * | ||||||
| BF% | 32.6% | 31.7% | ||||||
| Usual care (N = 28) | Fat mass | 30.0 | 29.7 | |||||
| Lean mass | 56.7 | 56.8 | ||||||
| BF% | 32.9% | 32.9% | ||||||
| Newton et al. [36] | RCT | Bone mineral density | 12 months 2 ×/week Supervised impact exercise at ground reaction force of 3–5 × body weight Resistance exercise 6–12 RM, 2–4 sets 2 ×/week Home-based impact exercise Or 6 months 2 ×/week 150 min/week Supervised aerobic at 65–85% HRmax Resistance exercise 6–12 RM, 2–4 sets Home-based aerobic exercise 6 months Home-based aerobic Resistance (body weight/band) exercise Or 6 months waiting period 6 months 2 ×/week 80 min/week Aerobic exercise at 70% HRmax | DXA | Resistance/impact (N = 57) | Fat mass | 24.0 | 25.1 |
| Lean mass | 57.9 | 59.3 | ||||||
| ASM | 25.0 | 25.9 §6DEL | ||||||
| Aerobic/resistance (N = 50) | Fat mass | 22.8 | 23.7 | |||||
| Lean mass | 58.1 | 58.7 | ||||||
| ASM | 25.2 | 25.6 | ||||||
| Delay/aerobic (N = 47) | Fat mass | 27.1 | 28.3 | |||||
| Lean mass | 59.3 | 60.4 | ||||||
| ASM | 25.3 | 25.9 | ||||||
| Resistance-based interventions | ||||||||
| Galvão et al. [37] | Prospective cohort | Muscle function | 20 weeks 2 ×/week 120 min/week Supervised resistance exercise 6–12 RM, 2–4 sets | DXA | Resistance (N = 10) | Fat mass | 25.7 | 24.9 |
| Lean mass | 52.2 | 52.0 | ||||||
| BF% | 30.7% | 30.6% | ||||||
| Quadriceps thickness | 2.15 cm | 2.46 cm * | ||||||
| Hamstring thickness | 4.52 cm | 1.53 cm | ||||||
| Biceps thickness | 2.69 cm | 2.91 cm | ||||||
| Triceps thickness | 1.94 cm | 2.33 cm | ||||||
| Alberga et al. [32] | Details in aerobic section | |||||||
| Santa Mina et al. [33] | Details in aerobic section | |||||||
| Santa Mina et al. [34] | Details in aerobic section | |||||||
| Hanson et al. [38] | Prospective cohort | Muscle size and function | 12 weeks 3 ×/week 180 min/week Supervised high-intensity resistance exercise 15 repetitions, first 5 at 5 RM | DXA and CT | Resistance (N = 17) | Fat mass | 31.2 | 31.1 |
| Subcutaneous | 118 cm2 | 118 cm2 | ||||||
| Intermuscular | 7.9 cm2 | 7.6 cm2 | ||||||
| Lean mass | 62.4 | 64.1 * | ||||||
| BF% | 31.4% | 30.7% * | ||||||
| Nilsen et al. [39] | RCT | Lean mass | 16 weeks 3 ×/week Supervised resistance exercise 6–10 RM, 1–3 sets | DXA | Resistance (N = 28) | Fat mass | 26.5 | 26.4 |
| Trunk fat | 14.7 | 14.6 | ||||||
| Lean mass | 59.8 | 60.3 | ||||||
| ASM | 25.2 | 25.7 § | ||||||
| BF% | 29.5% | 29.3% | ||||||
| Control (N = 30) | Fat mass | 26.4 | 26.7 | |||||
| Trunk fat | 14.6 | 14.7 | ||||||
| Lean mass | 57.9 | 57.9 | ||||||
| ASM | 24.8 | 24.7 | ||||||
| BF% | 30.0% | 30.2% | ||||||
| Multi-modal interventions | ||||||||
| Galvão et al. [40] | RCT | Lean mass | 12 weeks 2 ×/week Supervised aerobic at 65–80% HRmax Resistance exercise 6–12 RM, 2–4 sets | DXA | Exercise (N = 29) | Fat mass | 22.5 | 22.3 |
| Trunk fat | 12.2 | 11.9 | ||||||
| Lean mass | 56.1 | 56.8 § | ||||||
| ASM | 23.5 | 24.0 § | ||||||
| BF% | 27.5% | 27.2% | ||||||
| Usual care (N = 28) | Fat mass | 23.2 | 23.5 | |||||
| Trunk fat | 12.4 | 12.2 | ||||||
| Lean mass | 57.8 | 57.8 | ||||||
| ASM | 24.6 | 24.4 | ||||||
| BF% | 27.3% | 27.5% | ||||||
| Galvão et al. [15] | RCT | Various ADT side effects | See Galvão et al. [40] | DXA | Acute ADT (N = 16) | Fat mass | 22.7 | 23.3 § * |
| Trunk fat | 12.2 | 12.4 | ||||||
| Lean mass | 58.5 | 59.1 | ||||||
| ASM | 24.7 | 25.2 | ||||||
| BF% | 26.8% | 27.2% § | ||||||
| Chronic ADT (N = 34) b | Fat mass | 23.4 | 23.0 * | |||||
| Trunk fat | 12.1 | 11.8 * | ||||||
| Lean mass | 56.5 | 57.4 * | ||||||
| ASM | 23.8 | 24.4 * | ||||||
| BF% | 28.1% | 27.4% * | ||||||
| Cormie et al. [41] | RCT | Lean mass | 12 weeks 2 ×/week 150 min/week Supervised aerobic at 70–85% HRmax Resistance exercise at 60–85% 1 RM Home-based exercise of choice | DXA | Exercise (N = 32) | Fat mass | 26.9 | 26.3 § |
| Trunk fat | 14.8 | 14.3 § | ||||||
| Visceral fat | 913 g | 874 g * | ||||||
| Lean mass | 56.6 | 56.0 | ||||||
| ASM | 23.7 | 23.5 § | ||||||
| BF% | 30.6% | 30.5% § | ||||||
| Usual care (N = 31) | Fat mass | 26.9 | 27.8 * | |||||
| Trunk fat | 15.2 | 15.5 | ||||||
| Visceral fat | 926 g | 922 g | ||||||
| Lean mass | 58.7 | 57.3 * | ||||||
| ASM | 24.9 | 24.3 * | ||||||
| BF% | 30.3% | 31.4% * | ||||||
| Winters-Stone et al. [42] | RCT | Body composition | 12 months 2 ×/week 165 min/week Supervised resistance at 60–80% 1 RM Impact exercise 1 ×/week Home-based exercise of choice | DXA | Exercise (N = 29) | Fat mass | 24.3 | 23.9 § |
| Trunk fat | 13.5 | 13.1 | ||||||
| Lean mass | 59.2 | 59.2 | ||||||
| BF% | 28.7% | 28.4% | ||||||
| Flexibility (N = 22) | Fat mass | 28.4 | 29.9 | |||||
| Trunk fat | 15.0 | 15.4 | ||||||
| Lean mass | 57.5 | 57.2 | ||||||
| BF% | 31.6% | 32.4% | ||||||
| Wall et al. [43] | RCT | Cardiorespiratory fitness | 6 months 2 ×/week 150 min/week Supervised aerobic at 70–90% HRmax Resistance exercise 6–12 RM, 1–4 sets 1 ×/week Home-based aerobic exercise | DXA | Exercise (N = 50) | Fat mass | 24.1 | 24.5 § |
| Trunk fat | 13.2 | 13.0 § | ||||||
| Lean mass | 59.4 | 60.1 § | ||||||
| BF% | 27.2% | 27.2% § | ||||||
| Usual care (N = 47) | Fat mass | 25.7 | 27.2 | |||||
| Trunk fat | 14.2 | 14.9 | ||||||
| Lean mass | 58.7 | 58.6 | ||||||
| BF% | 28.2% | 30.3% | ||||||
| Newton et al. [36] | Details in aerobic section | |||||||
| Ndjavera et al. [44] | RCT | Fat mass | 12 weeks 2 ×/week Supervised aerobic at 55–85% HRmax Resistance exercise 10 RM, 2–4 sets Home-based aerobic exercise | BIA | Exercise (N = 24) | Fat mass | 24.3 | 21.7 |
| Fat-free mass | 58.2 | 58.9 | ||||||
| Usual care (N = 26) | Fat mass | 23.3 | 22.7 | |||||
| Fat-free mass | 59.1 | 58.2 | ||||||
| Study | Study Design | Primary Outcome | Intervention | Body Composition Assessment | Groups (N) | Outcome Variable | Mean Pre-Intervention Values (kg) | Mean Post-Intervention Values (kg) |
|---|---|---|---|---|---|---|---|---|
| Healthy eating guidelines and/or energy deficit | ||||||||
| O’Neill et al. [54] | RCT | Fat mass | 6 months ≥5 ×/week 150 min/week Home-based brisk walking UK healthy eating guidelines + energy deficit diet if overweight. | Skinfolds | Intervention (N = 47) | Fat mass | 28.8 | 26.9 § |
| Lean mass | 58.3 | 59.8 | ||||||
| BF% | 32.6% | 30.8% § | ||||||
| Control (N = 47) | Fat mass | 29.5 | 30.1 | |||||
| Lean mass | 59.8 | 59.1 | ||||||
| BF% | 32.4% | 32.8% | ||||||
| Gilbert et al. [52] | RCT | Brachial artery flow mediated dilatation | 12 weeks 180 min/week 2 ×/week (1–6 weeks) 1 ×/week (7–12 weeks) Supervised aerobic at 55–75% HRmax + resistance exercise at 60% 1 RM 1 ×/week (1–6 weeks) 2 ×/week (7–12 weeks) Home-based exercise of choice Fortnightly healthy eating seminars | BIA | Intervention (N = 25) | Fat mass | 34.5 | 31.6 |
| Skeletal muscle mass | 31.9 | 32.9 § | ||||||
| Usual care (N = 25) | Fat mass | 30.4 | 29.6 | |||||
| Skeletal muscle mass | 31.2 | 32.3 | ||||||
| Focht et al. [53] | RCT | Mobility | 12 weeks 150 min/week 2 ×/week (1–6 weeks) 1 ×/week (7–8 weeks) Supervised aerobic 3–4 RPE (1–10 scale) + resistance 8–12 RM, 3 sets 1 ×/week (7–8 weeks) 2 ×/week (9–12 weeks) Unsupervised aerobic + resistance Home-based exercise of choice Nutrition counselling sessions—8 as a group and 2 individual phone calls + energy deficit diet if overweight. | Bod Pod | Intervention (N = 16) | Fat mass b | −1.8 § | |
| Fat-free mass b | −0.06 | |||||||
| BF% b | −1.05% § | |||||||
| Usual care (N = 16) | Fat mass b | 0.9 | ||||||
| Fat-free mass b | −0.5 | |||||||
| BF% b | 0.82% | |||||||
| Freedland et al. [55] | RCT | Insulin resistance | 6 months ≥5 d/week 150 min/week Home-based walking Carbohydrate intake ≤ 20 g/day | DXA | Intervention (N = 11) | Fat mass | 32.3 | 24.0 § |
| Lean mass | 61.0 | 58.9 § | ||||||
| BF% | 28.3% | 26.6% § | ||||||
| Control (N = 18) | Fat mass | 25.3 | 28.3 | |||||
| Lean mass | 55.9 | 55.4 | ||||||
| BF% | 30.5% | 32.3% | ||||||
| Baguley et al. [56] | RCT | Cancer-related fatigue and quality of life | 12 weeks Individualised consultation with dietician every 2 weeks Mediterranean-style diet | DXA | Intervention (N = 12) | Fat mass | 29.5 | 27.8 * |
| Lean mass | 53.2 | 52.0 | ||||||
| Usual care (N = 11) | Fat mass | 29.8 | 29.3 | |||||
| Lean mass | 53.4 | 53.4 | ||||||
| Wilson et al. [57] | Prospective cohort | Fat mass | 12 weeks 3 ×/week 300 min/week Supervised resistance exercise at 6–12 RM, 2–4 sets Daily home-based aerobic exercise, RPE 3–8 (1–10 scale) 3 nutrition counselling sessions Calorie deficit diet 40 g protein powder after each supervised exercise session | DXA | Intervention (N = 14) | Fat mass | 39.8 | 37.0 * |
| Trunk fat | 20.1 | 18.3 * | ||||||
| Visceral fat | 954 g | 866 g * | ||||||
| Lean mass | 55.9 | 55.9 | ||||||
| ASM | 23.3 | 23.3 | ||||||
| BF% | 40.0% | 38.3% * | ||||||
| Protein intake | ||||||||
| Dawson et al. [58] | RCT | Lean mass | 12 weeks 3 ×/week 150 min/week Supervised resistance exercise at 60–83% 1 RM 2 × 25 g protein powder per day | DXA | Exercise (N = 8) + Exercise/protein (N = 8) | Fat mass | 30.3 | 31.2 |
| Lean mass | 48.5 | 53.2 § | ||||||
| Fat-free mass | 54.6 | 56.4 § | ||||||
| ASM | 23.5 | 24.8 § | ||||||
| BF% | 36.8% | 35.9% § | ||||||
| Protein (N = 10) + Flexibility control (N = 11) a | Fat mass | 25.6 | 26.2 | |||||
| Lean mass | 51.5 | 48.6 | ||||||
| Fat-free mass | 51.4 | 51.5 | ||||||
| ASM | 21.5 | 21.6 | ||||||
| BF% | 33.9% | 34.5% | ||||||
| Unanswered Questions for Prostate Cancer Patients on ADT Aiming to Induce Fat Loss and Muscle Gain. | |
|---|---|
 Aerobic training | 1. Will a low-intensity lead-in period designed to build baseline fitness reduce injury risk and improve adherence, particularly for high-risk patients? |
| 2. Is there a minimum intensity/volume for lipolysis and muscle protein synthesis stimulation? | |
 Resistance training | 1. Will a low-intensity familiarisation period designed to build baseline strength reduce injury risk and improve adherence, particularly for high-risk patients? |
| 2. Is there a minimum intensity/volume for muscle protein synthesis stimulation? | |
 Nutritional intake | 1. Who is an energy deficit or healthy eating guideline diet most appropriate for? |
| 2. What is the optimum protein intake to enhance muscle protein synthesis leading to muscle gain? | |
| Other questions inclusive of all elements | 1. Are the benefits gained from a combined exercise and nutrition intervention influenced by length of time on ADT? |
| 2. What is a clinically significant change in fat and lean mass for prostate cancer patients on ADT? |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, R.L.; Taaffe, D.R.; Newton, R.U.; Hart, N.H.; Lyons-Wall, P.; Galvão, D.A. Using Exercise and Nutrition to Alter Fat and Lean Mass in Men with Prostate Cancer Receiving Androgen Deprivation Therapy: A Narrative Review. Nutrients 2021, 13, 1664. https://doi.org/10.3390/nu13051664
Wilson RL, Taaffe DR, Newton RU, Hart NH, Lyons-Wall P, Galvão DA. Using Exercise and Nutrition to Alter Fat and Lean Mass in Men with Prostate Cancer Receiving Androgen Deprivation Therapy: A Narrative Review. Nutrients. 2021; 13(5):1664. https://doi.org/10.3390/nu13051664
Chicago/Turabian StyleWilson, Rebekah L., Dennis R. Taaffe, Robert U. Newton, Nicolas H. Hart, Philippa Lyons-Wall, and Daniel A. Galvão. 2021. "Using Exercise and Nutrition to Alter Fat and Lean Mass in Men with Prostate Cancer Receiving Androgen Deprivation Therapy: A Narrative Review" Nutrients 13, no. 5: 1664. https://doi.org/10.3390/nu13051664
APA StyleWilson, R. L., Taaffe, D. R., Newton, R. U., Hart, N. H., Lyons-Wall, P., & Galvão, D. A. (2021). Using Exercise and Nutrition to Alter Fat and Lean Mass in Men with Prostate Cancer Receiving Androgen Deprivation Therapy: A Narrative Review. Nutrients, 13(5), 1664. https://doi.org/10.3390/nu13051664







