Impact of Liver and Pancreas Diseases on Nutritional Status
Abstract
:1. Introduction
2. Consequences of Liver Disease on Nutritional Status
2.1. Impaired Dietary Intake
2.2. Altered Macro and Micronutrients Metabolism
2.2.1. Plasma Proteins
2.2.2. Vitamins and Minerals
2.3. Energy Metabolism Disturbances
2.4. Increase in Energy Expenditure
2.5. Nutrient Malabsorption
2.6. Sarcopenia and Muscle Function
2.7. Metabolic Osteopathy
2.8. Interplay between MAFLD and Diet
3. Nutritional Assessment of Patients with Chronic Liver Disease
3.1. Nutritional Screening and Risk of Malnutrition
3.2. Diagnosis of Malnutrition
3.2.1. Assessment of Reduced Intake
3.2.2. Weight Loss and Body Mass Index
3.2.3. Muscle Mass and Body Composition
3.2.4. Disease Burden/Inflammation
4. Nutritional Intervention in Liver Disease
5. Impact of Malnutrition and Its Therapy on Liver Transplantation
6. Normal Pancreatic Physiology and Mechanisms of Malnutrition
- Decreased production and secretion of pancreatic lipase due to a reduction of the pancreatic parenchyma, which occurs in chronic pancreatitis, autoimmune pancreatitis, and in pancreatic resections.
- Inaction of pancreatic lipase, which is usually due to the inactivation of lipase in excessively acidic environments, such as cystic fibrosis, where bicarbonate secretion is significantly reduced by the mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, so the intestinal lumen pH cannot properly increase; or in Zollinger–Edison syndrome, where the increased acid secretion from the stomach has a similar consequence.
- Obstruction of the pancreatic duct by pancreatic lithiasis due to chronic pancreatitis, pancreatic tumors, or ampulomas.
- Decreased lipase stimulation and production, which has been described in patients with celiac disease, Crohn’s disease, or Shwachman–Diamond syndrome (rare autosomal recessive disorder, which is the second most common cause of exocrine pancreatic insufficiency after cystic fibrosis and caused by an SBDS gene mutation on chromosome 7 that induces an abnormal functioning of ribosomes. The usual presentation is exocrine pancreatic dysfunction, skeletal abnormalities, and bone marrow dysfunction). Diabetes mellitus affects pancreatic microvascularization after years. This might facilitate fibrosis of the gland and a loss of functional tissue.
- Motility alterations, whereby partial or total gastrectomy eliminates the reservoir and the progressive arrival of chyme to the intestinal lumen, causing a decrease in stimulation through hormones and a reduction in pancreatic enzyme secretion. The prevalence of EPI after gastrectomy is as high as 40–80% [2].
7. Consequences of Exocrine Pancreatic Insufficiency for Nutritional Status
8. Assessment of Exocrine Pancreatic Function
8.1. Direct Tests
8.2. Indirect Tests
- Coefficient fat absorption (CFA), which is based on the classic Van Kamer test. It is considered the gold-standard, although it is an expensive and time-consuming method for measuring EPI. As a preliminary step, a specific diet of 100 g of fat must be administered for five days, collecting the feces of the last three days for analysis [102]. The result is the percentage of dietary fat that is absorbed, which is usually above 93% in non-EPI patients. The definition of steatorrhea is established when there is 7 g of fat in 24 h [3]. It is the only test approved by the American Food and Drug Administration (FDA) and the European Medicines Agency to assess EPI in clinical trials. However, it is not a widely used test in clinical practice. The most common criticism is that there is wide variability inside the test [3].
- Fecal elastase, which is based on the measurement of a very stable enzyme (elastase-1) that is produced in the acinar cells of the pancreas, binds bile salts in the intestine with little degradation, and can be measured in the feces. It can be measured in a single stool sample, with the requirement that these must be solid stools, because liquid stools can underestimate the presence of the enzyme and have a false positive result. A concentration of less than 200 µg/g is considered pathological. The specificity of the method is 93%, with a sensitivity for moderate and severe PID close to 100% [2]. The sensitivity decreases to 63% in cases of mild EPI. There are several measurement methods: ELISA, through the use of monoclonal antibodies or the use of polyclonal antisera. Monoclonal measurements do not interfere with enzyme replacement therapy, while polyclonal ones do [2]. Given its good results and its comfort, it has become the most widely used diagnostic test for evaluating EPI.
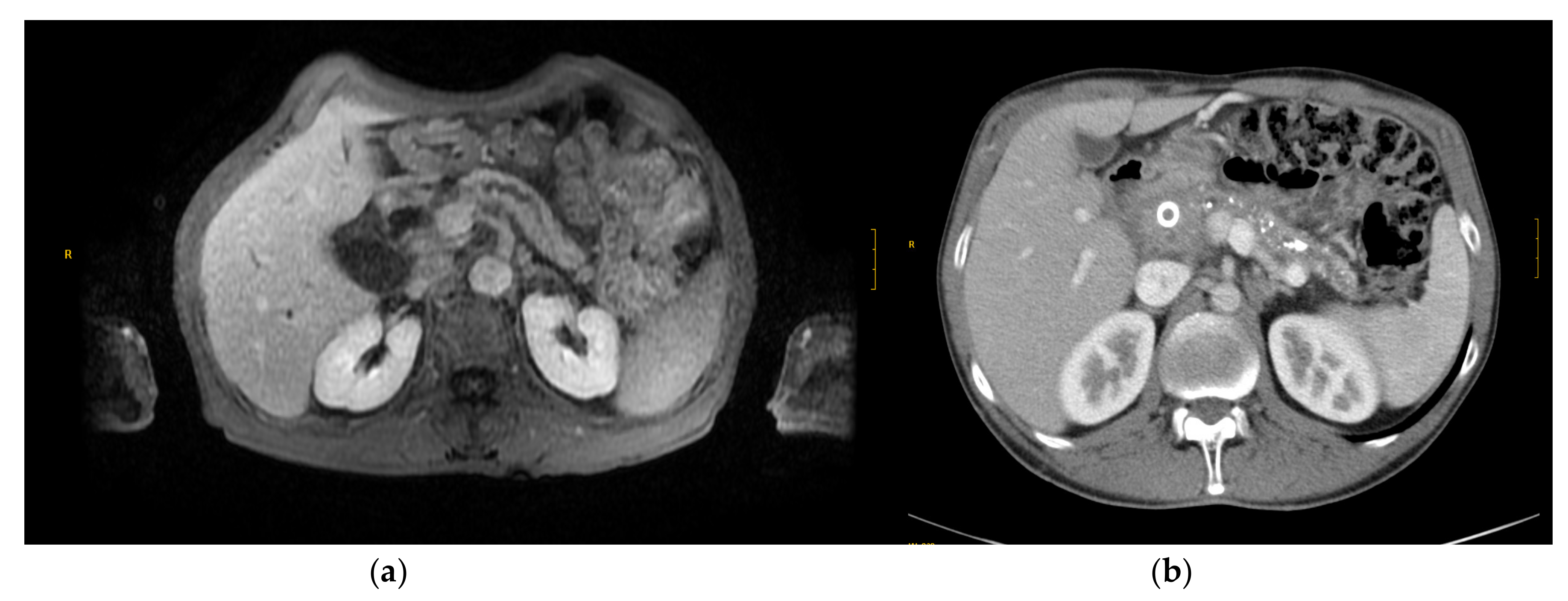
- Secretin-stimulated magnetic resonance cholangiopancreatography. Pancreatic magnetic resonance imaging has been shown to be useful for evaluating the pancreatic parenchyma, surrounding tissues, and, especially, the main pancreatic duct [113]. This allows for anatomical as well as functional assessment. Secretin stimulation enhances the enzyme secretion and visualization of the pancreatic duct. In this way, systems and scores have been developed to evaluate pancreatic function according to the increase in pancreatic juice, which can be measured by duodenal filling [2,112]. However, this diagnostic test should be standardized in a better way [110,112,114]. This method might also be useful in the assessment of the etiology of chronic pancreatitis [115].
- Breath test with marked-13Carbon, which is carried out by administering triglycerides marked with 13C. Pancreatic lipase is capable of hydrolyzing triglycerides into fatty acids, thus releasing 13C. This can be detected by the breath test, which varies depending on the activity of the pancreatic lipase. Its disadvantage is its low specificity and sensitivity, especially in mild EPI cases. The advantage is that it is a dynamic test, because the exhalation curve can be drawn.
9. Modern Management of Exocrine Pancreatic Insufficiency
10. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Merli, M.; Berzigotti, A.; Zelber-Sagi, S.; Dasarathy, S.; Montagnese, S.; Genton, L.; Plauth, M.; Parés, A. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J. Hepatol. 2019, 70, 172–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capurso, G.; Traini, M.; Piciucchi, M.; Signoretti, M.; Arcidiacono, P.G. Exocrine pancreatic insufficiency: Prevalence, diagnosis, and management. Clin. Exp. Gastroenterol. 2019, 12, 129–139. [Google Scholar] [CrossRef] [Green Version]
- O’Brien, S.J.; Omer, E. Chronic Pancreatitis and Nutrition Therapy. Nutr. Clin. Pract. 2019, 34, S13–S26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olesen, S.S.; Büyükuslu, A.; Køhler, M.; Rasmussen, H.H.; Drewes, A.M. Sarcopenia associates with increased hospitalization rates and reduced survival in patients with chronic pancreatitis. Pancreatology 2019, 19, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Maharshi, S.; Sharma, B.C.; Srivastava, S. Malnutrition in cirrhosis increases morbidity and mortality. J. Gastroenterol. Hepatol. 2015, 30, 1507–1513. [Google Scholar] [CrossRef]
- Møller, S.; Bendtsen, F.; Christensen, E.; Henriksen, J.H. Prognostic variables in patients with cirrhosis and oesophageal varices without prior bleeding. J. Hepatol. 1994, 21, 940–946. [Google Scholar] [CrossRef]
- Periyalwar, P.; Dasarathy, S. Malnutrition in Cirrhosis: Contribution and Consequences of Sarcopenia on Metabolic and Clinical Responses. Clin. Liver Dis. 2012, 16, 95–131. [Google Scholar] [CrossRef] [Green Version]
- Bajaj, J.S.; Lauridsen, M.; Tapper, E.B.; Duarte-Rojo, A.; Rahimi, R.S.; Tandon, P.; Shawcross, D.L.; Thabut, D.; Dhiman, R.K.; Romero-Gomez, M.; et al. Important Unresolved Questions in the Management of Hepatic Encephalopathy: An ISHEN Consensus. Am. J. Gastroenterol. 2020, 115, 989–1002. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Liver transplantation. J. Hepatol. 2016, 64, 433–485. [Google Scholar] [CrossRef] [PubMed]
- Rivelsrud, M.; Paur, I.; Sygnestveit, K.; Nilsen, R.M.; Tangvik, R.J. Nutritional treatment is associated with longer survival in patients with pancreatic disease and concomitant risk of malnutrition. Clin. Nutr. 2021, 40, 2128–2137. [Google Scholar] [CrossRef] [PubMed]
- Olesen, S.S.; Frandsen, L.K.; Poulsen, J.L.; Vestergaard, P.; Rasmussen, H.H.; Drewes, A.M. The prevalence of underweight is increased in chronic pancreatitis outpatients and associates with reduced life quality. Nutrients 2017, 43–44, 1–7. [Google Scholar] [CrossRef]
- Domínguez-Muñoz, J.E.; Nieto-Garcia, L.; López-Díaz, J.; Larińo-Noia, J.; Abdulkader, I.; Iglesias-Garcia, J. Impact of the treatment of pancreatic exocrine insufficiency on survival of patients with unresectable pancreatic cancer: A retrospective analysis. BMC Cancer 2018, 18, 534. [Google Scholar] [CrossRef] [Green Version]
- Chapman, B.; Sinclair, M.; Gow, P.J.; Testro, A.G. Malnutrition in cirrhosis: More food for thought. World J. Hepatol. 2020, 12, 883–896. [Google Scholar] [CrossRef]
- Stirnimann, J.; Stirnimann, G. Nutritional Challenges in Patients with Advanced Liver Cirrhosis. J. Clin. Med. 2019, 8, 1926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamran, U.; Towey, J.; Khanna, A.; Chauhan, A.; Rajoriya, N.; Holt, A. Nutrition in alcohol-related liver disease: Physiopathology and management. World J. Gastroenterol. 2020, 26, 2916–2930. [Google Scholar] [CrossRef]
- Wu, J.; Meng, Q.-H. Current understanding of the metabolism of micronutrients in chronic alcoholic liver disease. World J. Gastroenterol. 2020, 26, 4567–4578. [Google Scholar] [CrossRef] [PubMed]
- Shergill, R.; Syed, W.; Rizvi, S.A.; Singh, I. Nutritional support in chronic liver disease and cirrhotics. World J. Hepatol. 2018, 10, 685–694. [Google Scholar] [CrossRef]
- Cheung, K.; Lee, S.S.; Raman, M. Prevalence and Mechanisms of Malnutrition in Patients with Advanced Liver Disease, and Nutrition Management Strategies. Clin. Gastroenterol. Hepatol. 2012, 10, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Kalaitzakis, E.; Bosaeus, I.; Öhman, L.; Björnsson, E. Altered postprandial glucose, insulin, leptin, and ghrelin in liver cirrhosis: Correlations with energy intake and resting energy expenditure. Am. J. Clin. Nutr. 2007, 85, 808–815. [Google Scholar] [CrossRef]
- Meyer, F.; Bannert, K.; Wiese, M.; Esau, S.; Sautter, L.F.; Ehlers, L.; Aghdassi, A.A.; Metges, C.C.; Garbe, L.-A.; Jaster, R.; et al. Molecular Mechanism Contributing to Malnutrition and Sarcopenia in Patients with Liver Cirrhosis. Int. J. Mol. Sci. 2020, 21, 5357. [Google Scholar] [CrossRef] [PubMed]
- Zaccherini, G.; Bernardi, M. The role and indications of albumin in advanced liver disease. Acta Gastroenterol. Belg. 2019, 82, 301–308. [Google Scholar]
- Petta, S.; Cammà, C.; Scazzone, C.; Tripodo, C.; Di Marco, V.; Bono, A.; Cabibi, D.; Licata, G.; Porcasi, R.; Marchesini, G.; et al. Low vitamin D serum level is related to severe fibrosis and low responsiveness to interferon-based therapy in genotype 1 chronic hepatitis C. Hepatology 2009, 51, 1158–1167. [Google Scholar] [CrossRef]
- Chetri, K.; Choudhuri, G. Role of trace elements in hepatic encephalopathy: Zinc and manganese. Int. J. Gastroenterol. 2003, 22, 28–30. [Google Scholar]
- Hanai, T.; Shiraki, M.; Imai, K.; Suetugu, A.; Takai, K.; Shimizu, M. Usefulness of Carnitine Supplementation for the Complications of Liver Cirrhosis. Nutrients 2020, 12, 1915. [Google Scholar] [CrossRef]
- Schneeweiss, B.; Graninger, W.; Ferenci, P.; Eichinger, S.; Grimm, G.; Schneider, B.; Laggner, A.N.; Lenz, K.; Kleinberger, G. Energy metabolism in patients with acute and chronic liver disease. Hepatology 1990, 11, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Westerterp, K.R. Physical activity and physical activity induced energy expenditure in humans: Measurement, determinants, and effects. Front. Physiol. 2013, 4, 90. [Google Scholar] [CrossRef] [Green Version]
- Peng, S.; Plank, L.D.; McCall, J.L.; Gillanders, L.K.; McIlroy, K.; Gane, E.J. Body composition, muscle function, and energy expenditure in patients with liver cirrhosis: A comprehensive study. Am. J. Clin. Nutr. 2007, 85, 1257–1266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Augustyn, M.; Grys, I.; Kukla, M. Small intestinal bacterial overgrowth and nonalcoholic fatty liver disease. Clin. Exp. Hepatol. 2019, 5, 1–10. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Khoruts, A. Microbiota changes and intestinal microbiota transplantation in liver diseases and cirrhosis. J. Hepatol. 2020, 72, 1003–1027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koo, B.K.; Kim, D.; Joo, S.K.; Kim, J.H.; Chang, M.S.; Kim, B.G.; Lee, K.L.; Kim, W. Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis. J. Hepatol. 2017, 66, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Ali, R.; Nagalli, S. Hyperammonemia; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2021. [Google Scholar]
- Dasarathy, S.; Hatzoglou, M. Hyperammonemia and proteostasis in cirrhosis. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 30–36. [Google Scholar] [CrossRef]
- Guañabens, N.; Parés, A. Osteoporosis in chronic liver disease. Liver Int. 2018, 38, 776–785. [Google Scholar] [CrossRef] [Green Version]
- Ii, D.Y.; Pan, K.; Shendge, V.B.; Liu, J.; Ebraheim, N.A. Linkage of microbiota and osteoporosis: A mini literature review. World J. Orthop. 2019, 10, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-H.; Kim, S.U.; Song, K.; Park, J.Y.; Kim, D.Y.; Ahn, S.H.; Lee, B.-W.; Kang, E.S.; Cha, B.-S.; Han, K.-H. Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: Nationwide surveys (KNHANES 2008–2011). Hepatology 2016, 63, 776–786. [Google Scholar] [CrossRef] [Green Version]
- Meroni, M.; Longo, M.; Rustichelli, A.; Dongiovanni, P. Nutrition and Genetics in NAFLD: The Perfect Binomium. Int. J. Mol. Sci. 2020, 21, 2986. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longo, M.; Meroni, M.; Paolini, E.; Macchi, C.; Dongiovanni, P. Mitochondrial dynamics and nonalcoholic fatty liver disease (NAFLD): New perspectives for a fairy-tale ending? Metabolism 2021, 117, 154708. [Google Scholar] [CrossRef] [PubMed]
- Longo, M.; Paolini, E.; Meroni, M.; Dongiovanni, P. Remodeling of Mitochondrial Plasticity: The Key Switch from NAFLD/NASH to HCC. Int. J. Mol. Sci. 2021, 22, 4173. [Google Scholar] [CrossRef]
- Loong, T.-W. Understanding sensitivity and specificity with the right side of the brain. BMJ 2003, 327, 716–719. [Google Scholar] [CrossRef]
- Shaw, C.; Fleuret, C.; Pickard, J.M.; Mohammed, K.; Black, G.; Wedlake, L. Comparison of a novel, simple nutrition screening tool for adult oncology inpatients and the Malnutrition Screening Tool (MST) against the Patient-Generated Subjective Global Assessment (PG-SGA). Support Care Cancer 2014, 23, 47–54. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, M.; Hammond, C.; Roper, T.; Mukarati, J.; Ford, R.; Burrell, J.; Gordon, V.; Burch, N. Comparing assessment tools for detecting undernutrition in patients with liver cirrhosis. Clin. Nutr. ESPEN 2018, 23, 156–161. [Google Scholar] [CrossRef]
- Yasutake, K.; Koga, S.; Hokko, Y.; Ikemoto, M.; Yaguchi, Y.; Sakai, H.; Murata, Y.; Ohe, K.; Kohjima, M.; Nakamuta, M.; et al. Relevance of the Mini Nutritional Assessment in cirrhotic liver disease patients. Asia Pac. J. Clin. Nutr. 2018, 27, 300–305. [Google Scholar]
- Boulhosa, R.S.S.B.; Lourenço, R.P.; Côrtes, D.M.; Oliveira, L.P.M.; Lyra, A.C.; De Jesus, R.P. Comparison between criteria for diagnosing malnutrition in patients with advanced chronic liver disease: GLIM group proposal versus different nutritional screening tools. J. Hum. Nutr. Diet. 2020, 33, 862–868. [Google Scholar] [CrossRef] [PubMed]
- Harimoto, N.; Yoshizumi, T.; Inokuchi, S.; Itoh, S.; Adachi, E.; Ikeda, Y.; Uchiyama, H.; Utsunomiya, T.; Kajiyama, K.; Kimura, K.; et al. Prognostic Significance of Preoperative Controlling Nutritional Status (CONUT) Score in Patients Undergoing Hepatic Resection for Hepatocellular Carcinoma: A Multi-institutional Study. Ann. Surg. Oncol. 2018, 25, 3316–3323. [Google Scholar] [CrossRef]
- Wang, T.; Shen, J. Usefulness of Simplified Nutritional Appetite Questionnaire (SNAQ) in Appetite Assessment in Elder Patients with Liver Cirrhosis. J. Nutr. Health Aging 2018, 22, 911–915. [Google Scholar] [CrossRef] [PubMed]
- Georgiou, A.; Papatheodoridis, G.V.; Alexopoulou, A.; Deutsch, M.; Vlachogiannakos, I.; Ioannidou, P.; Papageorgiou, M.-V.; Papadopoulos, N.; Tsibouris, P.; Prapa, A.; et al. Evaluation of the effectiveness of eight screening tools in detecting risk of malnutrition in cirrhotic patients: The KIRRHOS study. Br. J. Nutr. 2019, 122, 1368–1376. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deza, D.C.; Msc, M.E.B.G.; Sanz-París, A.; Msc, M.L.B.; Bonilla, E.M.F.; Monterde, V.B.; Mainar, J.M.A.; Olmo, J.F. Mini Nutritional Assessment—Short Form Is a Useful Malnutrition Screening Tool in Patients with Liver Cirrhosis, Using the Global Leadership Initiative for Malnutrition Criteria as the Gold Standard. Nutr. Clin. Pract. 2021. [Google Scholar] [CrossRef]
- Jager-Wittenaar, H.; Ottery, F.D. Assessing nutritional status in cancer. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 322–329. [Google Scholar] [CrossRef] [Green Version]
- Guerra, R.S.; Fonseca, I.; Sousa, A.S.; Jesus, A.; Pichel, F.; Amaral, T.F. ESPEN diagnostic criteria for malnutrition—A validation study in hospitalized patients. Clin. Nutr. 2017, 36, 1326–1332. [Google Scholar] [CrossRef]
- Cichoż-Lach, H.; Michalak, A. A Comprehensive Review of Bioelectrical Impedance Analysis and Other Methods in the Assessment of Nutritional Status in Patients with Liver Cirrhosis. Gastroenterol. Res. Pract. 2017, 2017, 1–10. [Google Scholar] [CrossRef]
- Sinclair, M.; Hoermann, R.; Peterson, A.; Testro, A.; Angus, P.W.; Hey, P.; Chapman, B.; Gow, P.J. Use of Dual X-ray Absorptiometry in men with advanced cirrhosis to predict sarcopenia-associated mortality risk. Liver Int. 2019, 39, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Buchard, B.; Boirie, Y.; Cassagnes, L.; Lamblin, G.; Coilly, A.; Abergel, A. Assessment of Malnutrition, Sarcopenia and Frailty in Patients with Cirrhosis: Which Tools Should We Use in Clinical Practice? Nutrients 2020, 12, 186. [Google Scholar] [CrossRef] [Green Version]
- Belarmino, G.; Torrinhas, R.S.; Heymsfield, S.B.; Waitzberg, D.L. Sarcopenia in liver cirrhosis: The role of computed to-mography scan in the assessment of muscle mass compared with dual-energy X-ray absorptiometry and anthropometry. Int. Eur. J. Gastroenterol. Hepatol. 2015, 27, 1228. [Google Scholar] [CrossRef]
- Bunchorntavakul, C.; Reddy, K.R. Review article: Malnutrition/sarcopenia and frailty in patients with cirrhosis. Aliment. Pharmacol. Ther. 2019, 51, 64–77. [Google Scholar] [CrossRef] [Green Version]
- Iwasa, M.; Iwata, K.; Hara, N.; Hattori, A.; Ishidome, M.; Sekoguchi-Fujikawa, N.; Mifuji-Moroka, R.; Sugimoto, R.; Fujita, N.; Kobayashi, Y.; et al. Nutrition therapy using a multidisciplinary team improves survival rates in patients with liver cirrhosis. Nutrients 2013, 29, 1418–1421. [Google Scholar] [CrossRef]
- Bischoff, S.C.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Plauth, M. ESPEN practical guideline: Clinical nutrition in liver disease. Clin. Nutr. 2020, 39, 3533–3562. [Google Scholar] [CrossRef] [PubMed]
- Tsien, C.D.; McCullough, A.J.; Dasarathy, S. Late evening snack: Exploiting a period of anabolic opportunity in cirrhosis. J. Gastroenterol. Hepatol. 2012, 27, 430–441. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Wang, L.; Kuo, H.; Fang, Y.; Lee, H. Significant effects of late evening snack on liver functions in patients with liver cirrhosis: A meta-analysis of randomized controlled trials. J. Gastroenterol. Hepatol. 2019, 34, 1143–1152. [Google Scholar] [CrossRef] [PubMed]
- Marchesini, G.; Bianchi, G.; Merli, M.; Amodio, P.; Panella, C.; Loguercio, C.; Fanelli, F.R.; Abbiati, R. Nutritional supplementation with branched-chain amino acids in advanced cirrhosis: A double-blind, randomized trial. Gastroenterology 2003, 124, 1792–1801. [Google Scholar] [CrossRef]
- Muto, Y.; Sato, S.; Watanabe, A.; Moriwaki, H.; Suzuki, K.; Kato, A.; Kato, M.; Nakamura, T.; Higuchi, K.; Nishiguchi, S.; et al. Effects of Oral Branched-Chain Amino Acid Granules on Event-Free Survival in Patients with Liver Cirrhosis. Clin. Gastroenterol. Hepatol. 2005, 3, 705–713. [Google Scholar] [CrossRef]
- Les, I.; Doval, E.; García-Martínez, R.; Planas, M.; Cárdenas, G.; Gómez, P.; Flavià, M.; Jacas, C.; Mínguez, B.; Vergara, M.; et al. Effects of Branched-Chain Amino Acids Supplementation in Patients with Cirrhosis and a Previous Episode of Hepatic Encephalopathy: A Randomized Study. Am. J. Gastroenterol. 2011, 106, 1081–1088. [Google Scholar] [CrossRef]
- Fialla, A.D.; Israelsen, M.; Hamberg, O.; Krag, A.; Gluud, L.L. Nutritional therapy in cirrhosis or alcoholic hepatitis: A systematic review and meta-analysis. Liver Int. 2015, 35, 2072–2078. [Google Scholar] [CrossRef]
- Koretz, R.L.; Avenell, A.; Lipman, T.O. Nutritional support for liver disease. Cochrane Database Syst. Rev. 2012, CD008344. [Google Scholar] [CrossRef]
- Gluud, L.L.; Dam, G.; Les, I.; Marchesini, G.; Borre, M.; Aagaard, N.K.; Vilstrup, H. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst. Rev. 2017, 5, CD001939. [Google Scholar] [CrossRef] [PubMed]
- Zenith, L.; Meena, N.; Ramadi, A.; Yavari, M.; Harvey, A.; Carbonneau, M.; Ma, M.; Abraldes, J.G.; Paterson, I.; Haykowsky, M.J.; et al. Eight Weeks of Exercise Training Increases Aerobic Capacity and Muscle Mass and Reduces Fatigue in Patients with Cirrhosis. Clin. Gastroenterol. Hepatol. 2014, 12, 1920–1926.e2. [Google Scholar] [CrossRef]
- Berzigotti, A.; Albillos, A.; Villanueva, C.; Genescá, J.; Ardevol, A.; Augustín, S.; Calleja, J.L.; Bañares, R.; García-Pagán, J.C.; Mesonero, F.; et al. Effects of an intensive lifestyle intervention program on portal hypertension in patients with cirrhosis and obesity: The SportDiet study. Hepatology 2017, 65, 1293–1305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tandon, P.; Ismond, K.P.; Riess, K.; Duarte-Rojo, A.; Al-Judaibi, B.; Dunn, M.A.; Holman, J.; Howes, N.; Haykowsky, M.J.F.; Josbeno, D.A.; et al. Exercise in cirrhosis: Translating evidence and experience to practice. J. Hepatol. 2018, 69, 1164–1177. [Google Scholar] [CrossRef] [Green Version]
- Everhart, J.E.; Lok, A.S.; Kim, H.; Morgan, T.R.; Lindsay, K.L.; Chung, R.T.; Bonkovsky, H.L.; Ghany, M.G. Weight-Related Effects on Disease Progression in the Hepatitis C Antiviral Long-Term Treatment Against Cirrhosis Trial. Gastroenterology 2009, 137, 549–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ericksen, R.E.; Lim, S.L.; McDonnell, E.; Shuen, W.H.; Vadiveloo, M.; White, P.J.; Ding, Z.; Kwok, R.; Lee, P.; Radda, G.K.; et al. Loss of BCAA Catabolism during Carcinogenesis Enhances mTORC1 Activity and Promotes Tumor Development and Progression. Cell Metab. 2019, 29, 1151–1165.e6. [Google Scholar] [CrossRef] [Green Version]
- Katagiri, R.; Song, M.; Zhang, X.; Lee, D.H.; Tabung, F.K.; Fuchs, C.S.; Meyerhardt, J.A.; Nishihara, R.; Chan, A.T.; Joshi, A.D.; et al. Dietary Intake of Branched-Chain Amino Acids and Risk of Colorectal Cancer. Cancer Prev. Res. 2019, 13, 65–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cabré, E.; Rodríguez-Iglesias, P.; Caballería, J.; Quer, J.C.; Sánchez-Lombraña, J.L.; Parés, A.; Papo, M.; Planas, R.; Gassull, M.A. Spanish Group for the Study of Alcoholic Hepatitis Short- and long-term outcome of severe alcohol-induced hepatitis treated with steroids or enteral nutrition: A multicenter randomized trial. Hepatology 2000, 32, 36–42. [Google Scholar] [CrossRef]
- Moreno, C.; Deltenre, P.; Senterre, C.; Louvet, A.; Gustot, T.; Bastens, B.; Hittelet, A.; Piquet, M.-A.; Laleman, W.; Orlent, H.; et al. Intensive Enteral Nutrition Is Ineffective for Patients with Severe Alcoholic Hepatitis Treated with Corticosteroids. Gastroenterology 2016, 150, 903–910.e8. [Google Scholar] [CrossRef] [Green Version]
- Stokes, C.S.; Volmer, D.A.; Grünhage, F.; Lammert, F. Vitamin D in chronic liver disease. Liver Int. 2013, 33, 338–352. [Google Scholar] [CrossRef]
- Grüngreiff, K.; Reinhold, D.; Wedemeyer, H. The role of zinc in liver cirrhosis. Ann. Hepatol. 2016, 15, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Takuma, Y.; Nouso, K.; Makino, Y.; Hayashi, M.; Takahashi, H. Clinical trial: Oral zinc in hepatic encephalopathy. Aliment. Pharmacol. Ther. 2010, 32, 1080–1090. [Google Scholar] [CrossRef]
- Sinclair, M.; Grossmann, M.; Hoermann, R.; Angus, P.W.; Gow, P.J. Testosterone therapy increases muscle mass in men with cirrhosis and low testosterone: A randomised controlled trial. J. Hepatol. 2016, 65, 906–913. [Google Scholar] [CrossRef] [PubMed]
- Tsien, C.; Shah, S.N.; McCullough, A.J.; Dasarathy, S. Reversal of sarcopenia predicts survival after a transjugular intrahepatic portosystemic stent. Eur. J. Gastroenterol. Hepatol. 2013, 25, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Wiesner, R.; Edwards, E.; Freeman, R.; Harper, A.; Kim, R.; Kamath, P.; Kremers, W.; Lake, J.; Howard, T.; Merion, R.M.; et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 2003, 124, 91–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montano-Loza, A.J.; Duarte-Rojo, A.; Meza-Junco, J.; Baracos, V.E.; Sawyer, M.B.; Pang, J.X.Q.; Beaumont, C.; Esfandiari, N.; Myers, R.P. Inclusion of Sarcopenia within MELD (MELD-Sarcopenia) and the Prediction of Mortality in Patients with Cirrhosis. Clin. Transl. Gastroenterol. 2015, 6, e102. [Google Scholar] [CrossRef] [PubMed]
- Van Vugt, J.L.A.; Alferink, L.J.M.; Buettner, S.; Gaspersz, M.P.; Bot, D.; Murad, S.D.; Feshtali, S.; van Ooijen, P.M.A.; Polak, W.G.; Porte, R.J.; et al. A model including sarcopenia surpasses the MELD score in predicting waiting list mortality in cirrhotic liver transplant candidates: A competing risk analysis in a national cohort. J. Hepatol. 2018, 68, 707–714. [Google Scholar] [CrossRef]
- Nutritional Status in Cirrhosis. Italian Multicentre Cooperative Project on Nutrition in Liver Cirrhosis. J. Hepatol. 1994, 21, 317–325. [Google Scholar]
- Bhanji, R.A.; Takahashi, N.; Moynagh, M.R.; Narayanan, P.; Angirekula, M.; Mara, K.C.; Dierkhising, R.A.; Watt, K.D. The evolution and impact of sarcopenia pre- and post-liver transplantation. Aliment. Pharmacol. Ther. 2019, 49, 807–813. [Google Scholar] [CrossRef]
- Ferreira, L.G.; Anastácio, L.R.; Correia, M.I. The impact of nutrition on cirrhotic patients awaiting liver transplantation. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 554–561. [Google Scholar] [CrossRef]
- Cabré, E.; Gassull, M.A. Nutrition in liver disease. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 545–551. [Google Scholar] [CrossRef]
- Stephenson, G.R.; Moretti, E.W.; El-Moalem, H.; Clavien, P.A.; Tuttle-Newhall, J.E. Malnutrition in liver transplant patients. Transplantation 2001, 72, 666–670. [Google Scholar] [CrossRef] [PubMed]
- DiMartini, A.; Cruz, R.J.; Dew, M.A.; Myaskovsky, L.; Goodpaster, B.; Fox, K.; Kim, K.H.; Fontes, P. Muscle mass predicts outcomes following liver transplantation. Liver Transplant. 2013, 19, 1172–1180. [Google Scholar] [CrossRef] [Green Version]
- Merli, M.; Giusto, M.; Gentili, F.; Novelli, G.; Ferretti, G.; Riggio, O.; Corradini, S.G.; Siciliano, M.; Farcomeni, A.; Attili, A.F.; et al. Nutritional status: Its influence on the outcome of patients undergoing liver transplantation. Liver Int. 2010, 30, 208–214. [Google Scholar] [CrossRef]
- Van Vugt, J.L.A.; Levolger, S.; De Bruin, R.W.F.; Van Rosmalen, J.; Metselaar, H.J.; Ijzermans, J.N.M. Systematic Review and Meta-Analysis of the Impact of Computed Tomography-Assessed Skeletal Muscle Mass on Outcome in Patients Awaiting or Undergoing Liver Transplantation. Arab. Archaeol. Epigr. 2016, 16, 2277–2292. [Google Scholar] [CrossRef] [PubMed]
- Giusto, M.; Lattanzi, B.; Di Gregorio, V.; Giannelli, V.; Lucidi, C.; Merli, M. Changes in nutritional status after liver transplantation. World J. Gastroenterol. 2014, 20, 10682–10690. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.; Verma, S.; Thuluvath, P.J. Obesity and its effect on survival in patients undergoing orthotopic liver transplantation in the United States. Hepatology 2002, 35, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Martin, P.; DiMartini, A.; Feng, S.; Brown, R.; Fallon, M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology 2014, 59, 1144–1165. [Google Scholar] [CrossRef] [PubMed]
- Merli, M.; Nicolini, G.; Angeloni, S.; Riggio, O. Malnutrition is a risk factor in cirrhotic patients undergoing surgery. Nutrients 2002, 18, 978–986. [Google Scholar] [CrossRef]
- Parekh, J.; Corley, D.A.; Feng, S. Diabetes, Hypertension and Hyperlipidemia: Prevalence over Time and Impact on Long-Term Survival After Liver Transplantation. Arab. Archaeol. Epigr. 2012, 12, 2181–2187. [Google Scholar] [CrossRef] [PubMed]
- Anastácio, L.R. Nutrition therapy: Integral part of liver transplant care. World J. Gastroenterol. 2016, 22, 1513–1522. [Google Scholar] [CrossRef] [PubMed]
- Le Cornu, K.A.; McKiernan, F.J.; Kapadia, S.A.; Neuberger, J.M. A Prospective randomized study of preoperative nutritional supplementation in patients awaiting elective orthotopic liver transplantation. Transplantation 2000, 69, 1364–1369. [Google Scholar] [CrossRef]
- Zhu, X.-H.; Wu, Y.-F.; Qiu, Y.-D.; Jiang, C.-P.; Ding, Y.-T. Liver-protecting effects of omega-3 fish oil lipid emulsion in liver transplantation. World J. Gastroenterol. 2012, 18, 6141–6147. [Google Scholar] [CrossRef]
- Lei, Q.; Wang, X.; Zheng, H.; Bi, J.; Tan, S.; Li, N. Peri-operative immunonutrition in patients undergoing liver trans-plantation: A meta-analysis of randomized controlled trials. Asia Pac. J. Clin. Nutr. 2015, 24, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Doi, J.; Moro, A.; Fujiki, M.; Eghtesad, B.; Quintini, C.; Menon, K.V.N.; Hashimoto, K.; Sasaki, K. Nutrition Support in Liver Transplantation and Postoperative Recovery: The Effects of Vitamin D Level and Vitamin D Supplementation in Liver Transplantation. Nutrients 2020, 12, 3677. [Google Scholar] [CrossRef] [PubMed]
- Mazurak, V.C.; Tandon, P.; Montano-Loza, A.J. Nutrition and the transplant candidate. Liver Transplant. 2017, 23, 1451–1464. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.J.; McNally, S.; Wigmore, S.J. Enhanced recovery following liver surgery: A systematic review and meta-analysis. HPB 2014, 16, 699–706. [Google Scholar] [CrossRef] [Green Version]
- Alkaade, S.; Vareedayah, A.A. A primer on exocrine pancreatic insufficiency, fat malabsorption, and fatty acid abnormalities. Am. J. Manag. Care 2017, 23, 203. [Google Scholar]
- Domínguez-Muñoz, J.E.; Phillips, M. Nutritional Therapy in Chronic Pancreatitis. Gastroenterol. Clin. N. Am. 2018, 47, 95–106. [Google Scholar] [CrossRef]
- Bartels, R.H.; Brink, D.A.V.D.; Bandsma, R.H.; van Hensbroek, M.B.; Tabbers, M.M.; Voskuijl, W.P. The Relation between Malnutrition and the Exocrine Pancreas: A Systematic Review. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 193–203. [Google Scholar] [CrossRef]
- Struyvenberg, M.R.; Martin, C.R.; Freedman, S.D. Practical guide to exocrine pancreatic insufficiency—Breaking the myths. BMC Med. 2017, 15, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lévy, P.; Barthet, M.; Mollard, B.R.; Amouretti, M.; Marion-Audibert, A.-M.; Dyard, F. Estimation of the prevalence and incidence of chronic pancreatitis and its complications. Gastroentérolog. Clinique Biol. 2006, 30, 838–844. [Google Scholar] [CrossRef]
- Lévy, P.; Domínguez-Muñoz, E.; Imrie, C.; Löhr, M.; Maisonneuve, P. Epidemiology of chronic pancreatitis: Burden of the disease and consequences. United Eur. Gastroenterol. J. 2014, 2, 345–354. [Google Scholar] [CrossRef] [Green Version]
- Del Portillo, R.C.; MiIla, S.P.; Váquez, N.G.; López, B.P.; López, L.B.; Serván, P.R.; García-Luna, P.P.; Gómez-Candela, C. Assessment of nutritional status in the healthcare setting in Spain. Nutr. Hosp. 2015, 31, 196–208. [Google Scholar]
- Min, M.; Patel, B.; Han, S.; Bocelli, L.; Kheder, J.; Vaze, A.; Wassef, W. Exocrine Pancreatic Insufficiency and Malnutrition in Chronic Pancreatitis. Pancreas 2018, 47, 1015–1018. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Munoz, J.E.; Drewes, A.M.; Lindkvist, B.; Ewald, N.; Czakó, L.; Rosendahl, J.; Löhr, J.M.; Löhr, M.; Besselink, M.; Mayerle, J.; et al. Recommendations from the United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis. Pancreatology 2018, 18, 847–854. [Google Scholar] [CrossRef]
- Lindkvist, B.; Domínguez-Muñoz, J.E.; Luaces-Regueira, M.; Castiñeiras-Alvariño, M.; Nieto-Garcia, L.; Iglesias-Garcia, J. Serum nutritional markers for prediction of pancreatic exocrine insufficiency in chronic pancreatitis. Pancreatology 2012, 12, 305–310. [Google Scholar] [CrossRef]
- Abu-El-Haija, M.; Conwell, D.L. Pancreatic Insufficiency. Gastrointest. Endosc. Clin. N. Am. 2018, 28, 521–528. [Google Scholar] [CrossRef]
- Tirkes, T.; Yadav, D.; Conwell, D.L.; Territo, P.R.; Zhao, X.; Venkatesh, S.K.; Kolipaka, A.; Li, L.; Pisegna, J.R.; Pandol, S.J.; et al. Magnetic resonance imaging as a non-invasive method for the assessment of pancreatic fibrosis (MINIMAP): A comprehensive study design from the consortium for the study of chronic pancreatitis, diabetes, and pancreatic cancer. Abdom. Radiol. 2019, 44, 2809–2821. [Google Scholar] [CrossRef] [PubMed]
- Keller, J.; Aghdassi, A.A.; Lerch, M.M.; Mayerle, J.V.; Layer, P. Tests of pancreatic exocrine function—Clinical significance in pancreatic and non-pancreatic disorders. Best Pract. Res. Clin. Gastroenterol. 2009, 23, 425–439. [Google Scholar] [CrossRef] [PubMed]
- Engjom, T.; Tjora, E.; Erchinger, F.; Madzak, A.; Dimcevski, G.; Frøkjær, J.B.; Haldorsen, I.S. Secretin-Stimulated Magnetic Resonance Imaging Reveals Variable Diagnostic Accuracy According to Etiology in Pancreatic Disease. Pancreas 2020, 49, 361–367. [Google Scholar] [CrossRef] [PubMed]
- De La Iglesia-García, D.; Huang, W.; Szatmary, P.; Baston-Rey, I.; Gonzalez-Lopez, J.; Prada-Ramallal, G.; Mukherjee, R.; Nunes, Q.M.; Domínguez-Muñoz, J.E.; Sutton, R.; et al. Efficacy of pancreatic enzyme replacement therapy in chronic pancreatitis: Systematic review and meta-analysis. Gut 2017, 66, 1354–1355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, J.R.; Gardner, T.B.; Waljee, A.K.; DiMagno, M.J.; Schoenfeld, P.S. Systematic review: Efficacy and safety of pancreatic enzyme supplements for exocrine pancreatic insufficiency. Aliment. Pharmacol. Ther. 2010, 31, 57–72. [Google Scholar] [CrossRef] [PubMed]
- Vecht, J.; Symersky, T.; Lamers, C.B.H.W.; Masclee, A.A.M. Efficacy of Lower than Standard Doses of Pancreatic Enzyme Supplementation Therapy during Acid Inhibition in Patients with Pancreatic Exocrine Insufficiency. J. Clin. Gastroenterol. 2006, 40, 721–725. [Google Scholar] [CrossRef] [PubMed]
- Bruno, M.J.; Rauws, E.A.J.; Hoek, F.J.; Tytgat, G.N.J. Comparative effects of adjuvant cimetidine and omeprazole during pancreatic enzyme replacement therapy. Dig. Dis. Sci. 1994, 39, 988–992. [Google Scholar] [CrossRef]

| Nutritional Consequence [Ref.] | Mechanisms in Chronic Liver Disease |
|---|---|
| 1. Impaired dietary intake [19,20] | Anorexia, dysgeusia, abdominal pain, bloating, early satiety secondary to ascites, prescription of restrictive diets, alcohol consumption |
| 2. Altered macro and micronutrient metabolism [13,14,15,16,21,22,23,24] | Lack of glycogen and vitamin storage, breakdown of fat and proteins as the principal energy source, decrease of vitamin and mineral levels |
| 3. Energy metabolism disturbances [25] | Hypermetabolic state, impaired glucose and lipid metabolism, sedentary lifestyle |
| 4. Increase in energy expenditure [26,27] | Increased catecholamines, malnutrition, immune compromise |
| 5. Nutrient malabsorption [28,29] | Decreased bile production, cholestasis, portosystemic shunting, portal hypertension gastropathy and enteropathy, small intestinal bacterial overgrowth, drug-related diarrhea |
| 6. Sarcopenia and muscle function [30,31,32] | Proteolysis as the energy source, inhibition of muscle growth, muscle autophagy, proinflammatory state |
| 7. Metabolic osteopathy [33] | Decrease in bone formation, increased bone resorption, dysbiosis, vitamin K and D deficiencies |
| Vitamin [Ref.] | Liver Role | Deficiency and Liver Disease | |
|---|---|---|---|
| Fat-soluble vitamins | |||
| A (retinol) [14,15,16] | Production of RBP4 (transporter) Main storage in HSc (80%) | Lost in vitamin A storage through the transformation of HSc into myofibroblasts. Deficiency is associated with nyctalopia (night blindness) and with hepatic encephalopathy | |
| D [14,15,16,22] | 25-hydroxylation site Production of binding proteins | Deficiency is associated with fibrosis, liver dysfunction, and mortality | |
| K [14,15,16] | Absorption of vitamin K trough bile acids | Deficiency is associated with coagulopathy and bone disease through an inadequate carboxylation of bone matrix proteins | |
| E [14,15,16] | Absorption of vitamin E trough bile acids | Deficiency is associated with hemolytic anemia, creatinuria, and neuronal degeneration | |
| Water-soluble vitamins | |||
| B [14,15,16] | B1 (thiamine) | Normal thiamine function | Lost in activation and transport. Deficiency is associated with neurologic dysfunction (Wernicke encephalopathy) and high-output heart failure (wet beriberi) |
| B2 (riboflavin) | Storage of riboflavin | Inadequate intake, increased utilization, and deficient storage. Deficiency is associated with inflammation of the gums and sores | |
| B6 (pyridoxine) | Storage of pyridoxine | Deficiency is associated with anemia and neutropenia | |
| B9 (folate) | Storage of folate | Deficiency is associated with anemia and macrocytosis | |
| B12 (cobalamin) | Storage of cobalamin | Deficiency is associated with anemia and neutropenia | |
| C [14,15,16] | Storage of vitamin C | Deficiency is common in MAFLD. Deficiency is associated with bleeding, joint pain, and an increase of free radicals | |
| Minerals | |||
| Zinc (Zn) [14,15,16] | Absorption of Zn | Inadequate dietary intake, impaired absorption, and an increase in urinary loss. Deficiency is associated with hepatic encephalopathy and alterations in taste and smell | |
| Magnesium (Mg) [14,15,16] | Transport of Mg | Impaired transport and decrease intake. Deficiency is associated with dysgeusia, decreased appetite, muscle cramps, and weakness | |
| Manganese (Mn) [23] | Absorption trough bile acid production | Elevated if there is a decrease in biliary excretion Deficiency is associated with brain accumulation and parkinsonism | |
| Carnitine [24] | Metabolism of carnitine | Poor intake. Deficiency is associated with muscle cramps | |
| Selenium (Se) [14,15,16] | Metabolism of Se | Deficiency related to severity liver disease Deficiency is associated with insulin resistance | |
| Iron (Fe) [14,15,16] | Metabolism of Fe | Overload in alcoholic liver disease. Deficiency is associated with hepatic overload, fibrosis, and dysfunction | |
| Screening Tool [Ref.] | Target Population | Variables | Strengths and Weaknesses | Usefulness in Patients with Liver Cirrhosis |
|---|---|---|---|---|
| MST [40] | Hospitalized patients | 1—Weight loss 2—Food intake 3—Appetite | Quick and easy No calculations No training Self-administered | May be inaccurate due to fluid overload. Low sensitivity in patients with liver cirrhosis. |
| MUST [41] | Hospitalized patients and outpatients | 1—BMI 2—Weight loss 3—Acute illness and impact on dietary | Quick and easy Adds acute illness Offers advice | May be inaccurate due to fluid overload. Low sensitivity in patients with liver cirrhosis. |
| MNA-SF [42] | Elderly patients | 1—Weight loss 2—Appetite 3—Mobility 4—Neuropsycho problems 5—BMI 6—Acute illness | Full evaluation, not only nutritional aspects BMI can be replaced by calf diameter | Good performance in liver cirrhosis. High sensitivity and good specificity. |
| NRS-2002 [43] | Hospitalized patients | 1—BMI 2—Weight loss 3—Food intake 4—Illness severity | Adds illness severity and age | May be inaccurate due to fluid overload. Low sensitivity in liver cirrhosis. High specificity |
| CONUT [44] | Informatic tool Hospitalized patients and outpatients | 1—Albumin 2—Cholesterol 3—Lymphocytes 4—Age 5—Illness severity 6—Length of illness 7—Treatment | Automated screening of large populations Blood test required Low specificity | Predictor of survival and complications after liver resection. Predictor of survival in end-stage liver disease. |
| SNAQ [45] | Hospitalized patients and outpatients | 1—Weight loss 2—Appetite 3—Nutritional supplements 4—BMI 5—Albumin 6—Lymphocytes | Simple and quick Provides a recommendation Blood test required | Limited data on the population with liver cirrhosis, but correlation with the Child–Pugh stage. |
| RFH-NPT [46] | Patients with liver cirrhosis | 1—Transplant 2—Fluid overload 3—Weight loss 4—Food intake 5—BMI (in absence of fluid overload) 6—Acute illness | Adds transplantation Reduces the impact of fluid retention Adds acute illness | Superior results compared to other tests in liver cirrhosis. High sensitivity and specificity. |
| LDUST [45] | Patients with liver cirrhosis | 1—Food intake, 2—Weight loss 3—Body fat loss 4—Muscle mass loss 5—Fluid overload 6—Functional capability | Reduces the impact of fluid retention Adds functional capacity Includes subjective variables | Limited data in clinical practice. High sensitivity and specificity. |
| Normal Pancreatic Physiology Phases | Beginning | Secretion | Function | Neurotransmission and Hormones Involved | |
|---|---|---|---|---|---|
| Digestive secretion | 1. Cephalic phase | Before the food reaches the stomach | Acinar secretion | Pancreatic enzyme synthesis and moderate secretion | ACh (vagal nerve) VIP GRP |
| 2. Gastric phase | Gastric distension | Acinar secretion | Low pancreatic enzymes secretion with small amounts of water and bicarbonate. | Gastropancreatic vagovagal reflex | |
| 3. Intestinal phase | When the chyme enters the intestinal lumen and pH < 4.5 | Ductal secretion | Secretion of large amounts of fluid and bicarbonate and pancreatic enzymes. | Secretin (S intestinal cells) → bicarbonate Cholecystokinin (I intestinal cells) → enzymes | |
| Interdigestive secretion | Between meals cyclically | Ductal secretion | Cleansing of excretion system | Ach, peptide motilin and pancreatic polypeptide | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cañamares-Orbis, P.; Bernal-Monterde, V.; Sierra-Gabarda, O.; Casas-Deza, D.; Garcia-Rayado, G.; Cortes, L.; Lué, A. Impact of Liver and Pancreas Diseases on Nutritional Status. Nutrients 2021, 13, 1650. https://doi.org/10.3390/nu13051650
Cañamares-Orbis P, Bernal-Monterde V, Sierra-Gabarda O, Casas-Deza D, Garcia-Rayado G, Cortes L, Lué A. Impact of Liver and Pancreas Diseases on Nutritional Status. Nutrients. 2021; 13(5):1650. https://doi.org/10.3390/nu13051650
Chicago/Turabian StyleCañamares-Orbis, Pablo, Vanesa Bernal-Monterde, Olivia Sierra-Gabarda, Diego Casas-Deza, Guillermo Garcia-Rayado, Luis Cortes, and Alberto Lué. 2021. "Impact of Liver and Pancreas Diseases on Nutritional Status" Nutrients 13, no. 5: 1650. https://doi.org/10.3390/nu13051650
APA StyleCañamares-Orbis, P., Bernal-Monterde, V., Sierra-Gabarda, O., Casas-Deza, D., Garcia-Rayado, G., Cortes, L., & Lué, A. (2021). Impact of Liver and Pancreas Diseases on Nutritional Status. Nutrients, 13(5), 1650. https://doi.org/10.3390/nu13051650







