Trends and Dynamics in the First Four Years of Operation of the First Human Milk Bank in Vietnam
Abstract
:1. Introduction
2. Methods
2.1. Data Sources and Study Variables
2.2. Data Management and Analysis
2.3. Ethical Considerations
3. Results
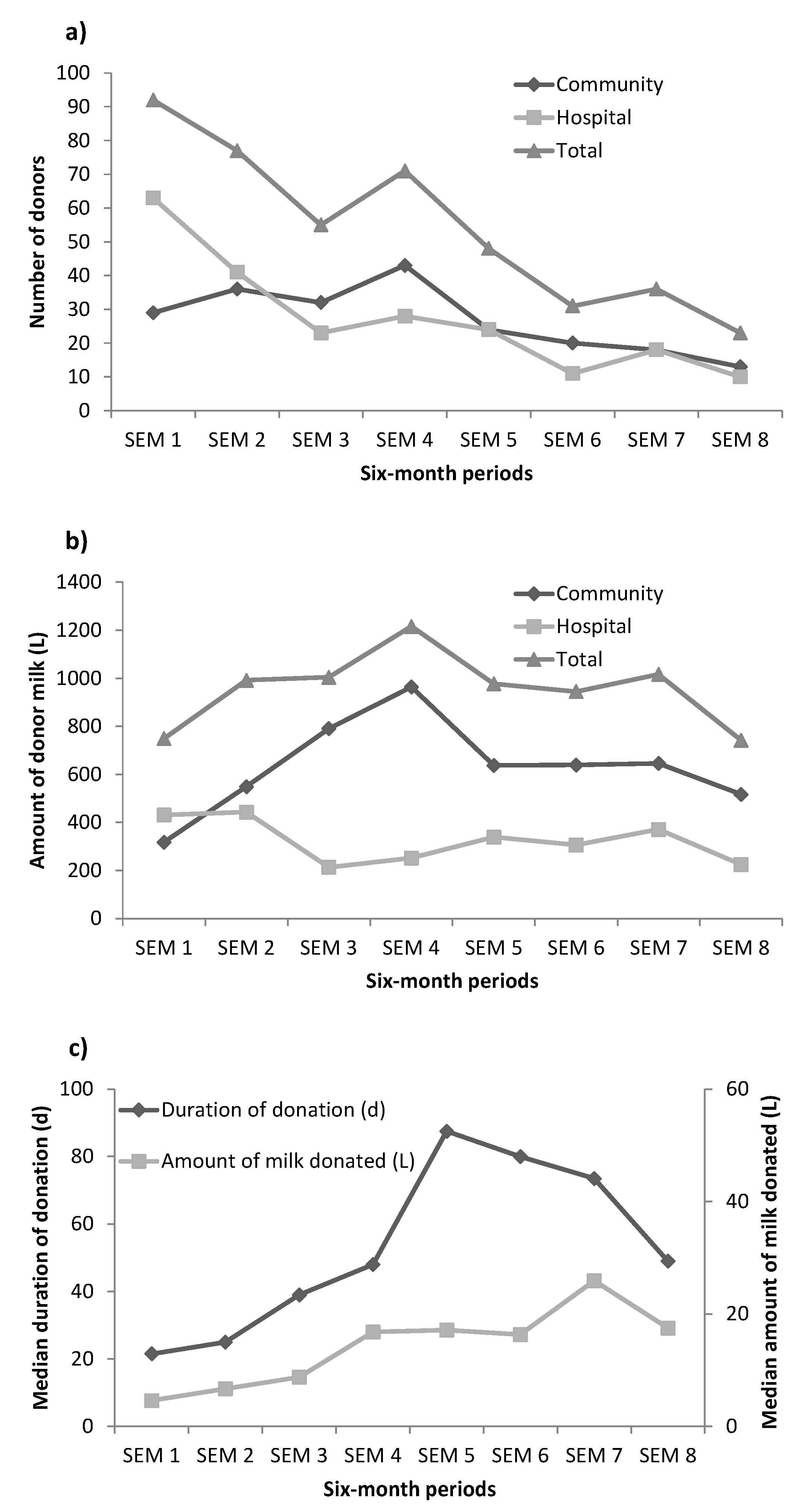
3.1. Characteristics of Human Milk Donors and Donation
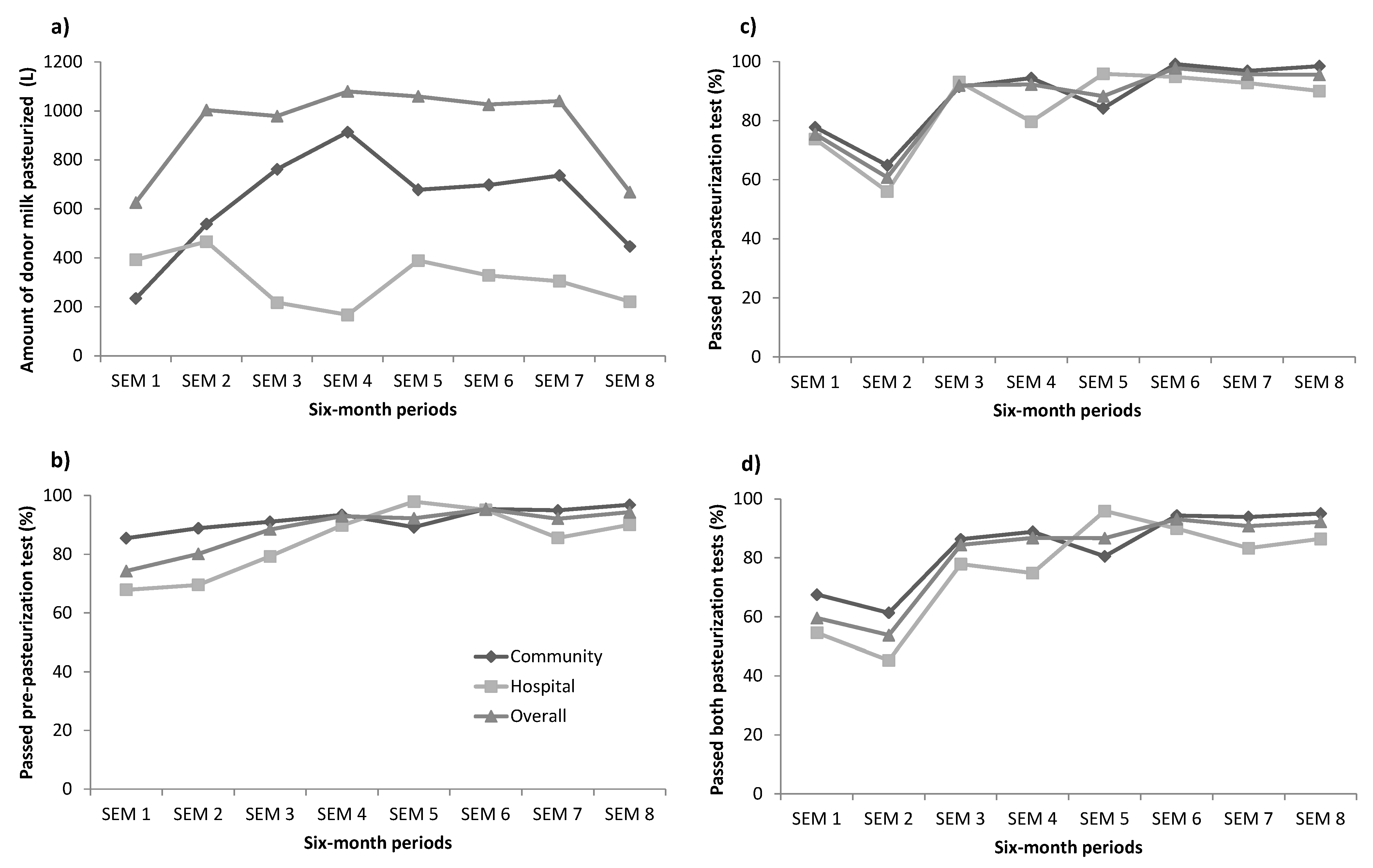
3.2. Handling and Processing of Human Donor Milk
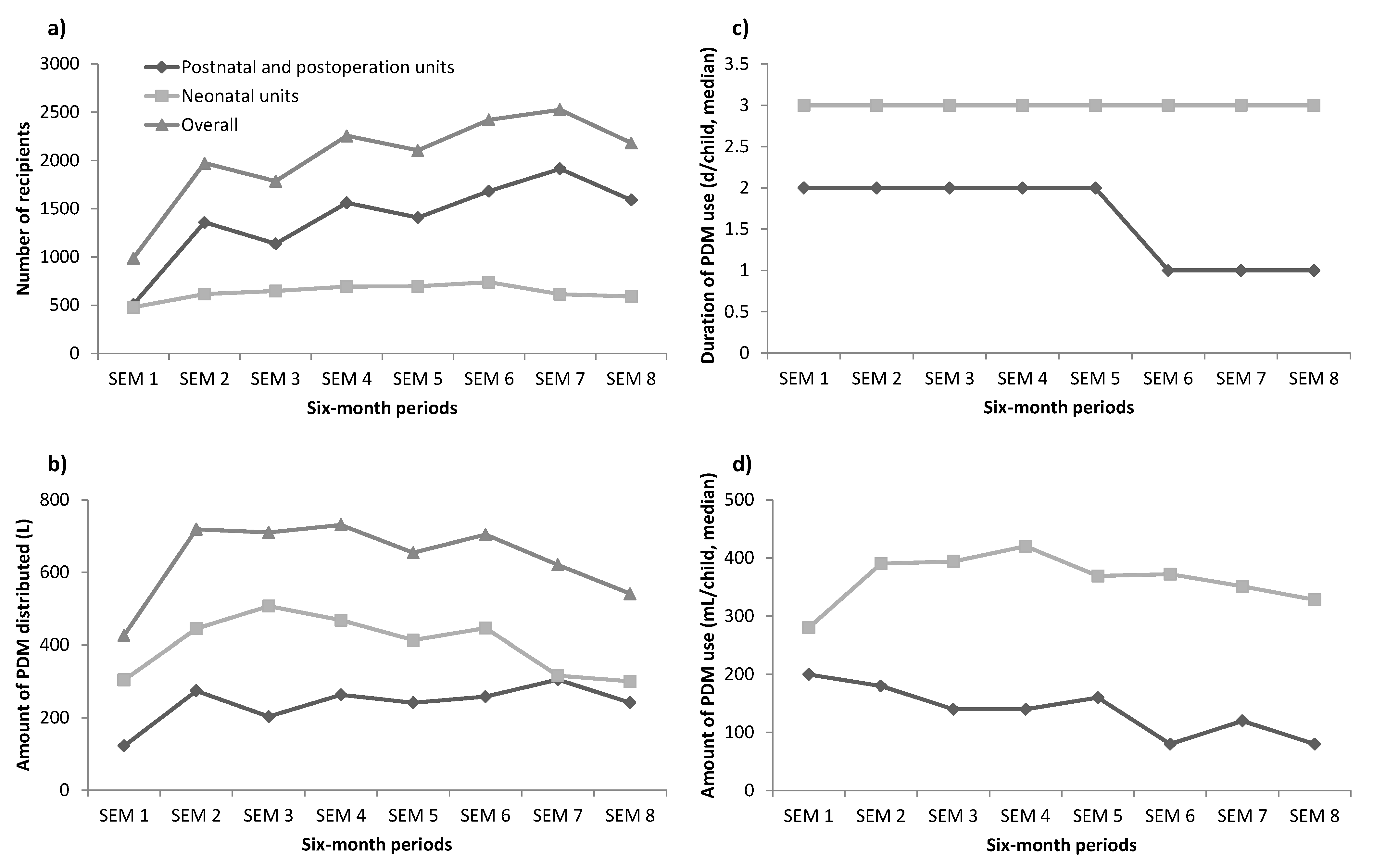
3.3. The Usage of Pasteurized Donor Milk
4. Discussions
4.1. Characteristics of Human Milk Donors
4.2. Human Donor Milk
4.3. Microbiology of Human Donor Milk
4.4. Recipients
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- United Nation Children’s Fund; World Health Organization; World Bank Group; United Nations. Levels and Trends in Child Mortality: Report 2019, Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation; United Nations Children’s Fund: New York, NY, USA, 2019. [Google Scholar]
- Tran, H.T.; Nguyen, T.T.; Mathisen, R. The use of human donor milk. BMJ 2020, 371, m4243. [Google Scholar] [CrossRef]
- WHO/UNICEF meeting on infant and young child feeding. J. Nurse Midwifery 1980, 25, 31–38. [CrossRef]
- World Health Organization. Guidelines on Optimal Feeding of Low Birth-Weight Infants in Low-and Middle-Income Countries; WHO Press: Geneva, Switzerland, 2011. [Google Scholar]
- PATH. Strengthening Human Milk Banking: A Resource Toolkit for Establishing and Integrating Human Milk Bank Programs-A Global Implementation Framework; PATH: Seattle, WA, USA, 2019. [Google Scholar]
- McCune, S.; Perrin, M.T. Donor Human Milk Use in Populations Other than the Preterm Infant: A Systematic Scoping Review. Breastfeed Med. 2021, 16, 8–20. [Google Scholar] [CrossRef]
- Quigley, M.; Embleton, N.D.; McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 2018, 6, CD002971. [Google Scholar] [CrossRef]
- Patel, A.L.; Johnson, T.J.; Engstrom, J.L.; Fogg, L.F.; Jegier, B.J.; Bigger, H.R.; Meier, P.P. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2013, 33, 514–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villamor-Martinez, E.; Pierro, M.; Cavallaro, G.; Mosca, F.; Kramer, B.W.; Villamor, E. Donor Human Milk Protects against Bronchopulmonary Dysplasia: A Systematic Review and Meta-Analysis. Nutrients 2018, 10. [Google Scholar] [CrossRef] [Green Version]
- Mansen, K.; Nguyen, T.T.; Nguyen, N.Q.; Do, C.T.; Tran, H.T.; Nguyen, N.T.; Mathisen, R.; Nguyen, V.D.; Ngo, Y.T.K.; Israel-Ballard, K. Strengthening Newborn Nutrition Through Establishment of the First Human Milk Bank in Vietnam. J. Hum. Lact. 2020. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.T.; Doyle, L.W.; Lee, K.J.; Dang, N.M.; Graham, S.M. Morbidity and mortality in hospitalised neonates in central Vietnam. Acta Paediatrica 2015, 104, e200–e205. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Chang, F.Y.; Cheng, S.W.; Wu, T.Z.; Fang, L.J. Characteristics of the first human milk bank in Taiwan. Pediatr. Neonatol. 2013, 54, 28–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Chen, H.; Sun, J.; Xiao, M.; Wu, J. The Operation and Data of the First Human Milk Bank in Mainland China. EC Nutr. 2015, 1, 67–71. [Google Scholar]
- Liu, X.H.; Han, S.P.; Wei, Q.F.; Zheng, F.Y.; Zhang, T.; Chen, H.M.; Mao, M. The data and characteristics of the human milk banks in mainland China. World J. Pediatr. 2019, 15, 190–197. [Google Scholar] [CrossRef] [Green Version]
- Katke, R.D.; Saraogi, M. Socio-Economic Factors Influencing Milk Donation in Milk Banks in India: An Institutional Study. Int. J. Reprod. Contracept. Obstet. Gynecol. 2014, 389–393. [Google Scholar] [CrossRef]
- Nangia, S.; Ramaswamy, V.V.; Bhasin, M. The Profile of Donors to a Human Milk Bank in a Developing Nation. Breastfeed. Med. 2020, 15, 135–139. [Google Scholar] [CrossRef]
- Candelaria, L.M.; Spatz, D.L.; Giordano, N. Experiences of Women Who Donated Human Milk. J. Obstet. Gynecol. Neonatal Nurs. 2018, 47, 556–563. [Google Scholar] [CrossRef]
- Vietnam National Assembly. Labor code, 2012. In Law on Health Insurance 25/2008/QH12; Vietnam National Assembly: Ha Noi, Vietnam, 2012. [Google Scholar]
- Pimenteira Thomaz, C.A.; Maia Loureiro, L.V.; da Silva Oliveira, T.; de Mendonça Furtado Montenegro, N.C.; Dantas Almeida Júnior, E.; Fernando Rodrigues Soriano, C.; Calado Cavalcante, J. The human milk donation experience: Motives, influencing factors, and regular donation. J. Hum. Lact. 2008, 24, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.T.; Mannava, P.; Murray, J.; Nguyen, P.T.; Tuyen, L.T.M.; Tuan, H.A.; Nga, P.T.Q.; Vinh, N.D.; Sobel, H.L. Early essential newborn care is associated with reduced adverse neonatal outcomes in a tertiary hospital in Da Nang, Viet Nam: A pre- post- intervention study. EClinicalMedicine 2018, 6, 51–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, C.; Li, Y.; Soowon, L.; Xu, Y.; Zhu, Q.; Zhao, H. Lactating Women’s Knowledge and Attitudes About Donor Human Milk in China. J. Hum. Lact. 2020. [Google Scholar] [CrossRef] [PubMed]
- Gidrewicz, D.A.; Fenton, T.R. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatr. 2014, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lamb, R.L.; Haszard, J.J.; Little, H.M.J.; Franks, A.F.; Meeks, M.G. Macronutrient Composition of Donated Human Milk in a New Zealand Population. J. Hum. Lact. 2020. [Google Scholar] [CrossRef]
- Gila-Diaz, A.; Arribas, S.M.; Algara, A.; Martín-Cabrejas, M.A.; López de Pablo, Á.L.; Sáenz de Pipaón, M.; Ramiro-Cortijo, D. A Review of Bioactive Factors in Human Breastmilk: A Focus on Prematurity. Nutrients 2019, 11, 1307. [Google Scholar] [CrossRef] [Green Version]
- Underwood, M.A. Human milk for the premature infant. Pediatr. Clin. North Am. 2013, 60, 189–207. [Google Scholar] [CrossRef] [Green Version]
- Lindemann, P.C.; Foshaugen, I.; Lindemann, R. Characteristics of breast milk and serology of women donating breast milk to a milk bank. Arch. Dis. Child. Fetal Neonatal Ed. 2004, 89, F440–F441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarmoc, G.; Bar-Yam, N.; Hagadorn, J.I.; Tosi, L.; Brownell, E.A. Demographics and Geographic Distribution of Mothers Donating to a Nonprofit Milk Bank. Breastfeed. Med. 2021, 16, 54–58. [Google Scholar] [CrossRef]
- Shenker, N.; Staff, M.; Vickers, A.; Aprigio, J.; Tiwari, S.; Nangia, S.; Sachdeva, R.C.; Clifford, V.; Coutsoudis, A.; Reimers, P.; et al. Maintaining human milk bank services throughout the COVID-19 pandemic: A global response. Matern. Child. Nutr. 2021. [Google Scholar] [CrossRef]
- Jang, H.L.; Cho, J.Y.; Kim, M.J.; Kim, E.J.; Park, E.Y.; Park, S.A.; Kim, I.Y.; Choi, Y.S.; Bae, C.W.; Chung, S.H. The Experience of Human Milk Banking for 8 Years: Korean Perspective. J. Korean Med. Sci. 2016, 31, 1775–1783. [Google Scholar] [CrossRef]
- Mullie, C.; Obin, O.; Outurquin, G.; Grognet, S.; Leke, A.; Adjide, C. Breastmilk donations: Bacteriological assessment, analysis of causes of non-compliance and suggestions for improvement. Archives Pédiatrie. 2018, 25, 263–268. [Google Scholar] [CrossRef]
- Simpson, J. Who gets donated human milk in Glasgow. In Proceedings of the EMBA International Milk Banking Congress, Glasgow, UK, 5–6 October 2017. [Google Scholar]
- Belfort, M.B.; Drouin, K.; Riley, J.F.; Gregory, K.E.; Philipp, B.L.; Parker, M.G.; Sen, S. Prevalence and Trends in Donor Milk Use in the Well-Baby Nursery: A Survey of Northeast United States Birth Hospitals. Breastfeed. Med. 2018, 13, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.; Nair, H.; Simpson, J.; Embleton, N. Use of Donor Human Milk and Maternal Breastfeeding Rates: A Systematic Review. J. Hum. Lact. 2016, 32, 212–220. [Google Scholar] [CrossRef]
- Stevens, E.E.; Patrick, T.E.; Pickler, R. A history of infant feeding. J. Perinat. Educ. 2009, 18, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Rowe-Murray, H.J.; Fisher, J.R. Baby friendly hospital practices: Cesarean section is a persistent barrier to early initiation of breastfeeding. Birth 2002, 29, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Banapurmath, C.R.; Ramachandrappa, S.; Guruprasad, G.; Biradar, S.B. Is cesarean section a barrier to early initiation of breastfeeding? Indian Pediatr. 2013, 50, 1062–1063. [Google Scholar]
- Wallenborn, J.T.; Graves, W.C.; Masho, S.W. Breastfeeding Initiation in Mothers with Repeat Cesarean Section: The Impact of Marital Status. Breastfeed. Med. 2017, 12, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.T.; Nguyen, P.T.K.; Huynh, L.T.; Le, C.H.M.; Giang, H.T.N.; Nguyen, P.T.T.; Murray, J. Appropriate care for neonates born to mothers with COVID-19 disease. Acta Paediatrica 2020. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.T.; Huynh, L.T.; Le, C.H.M.; Nguyen, V.D.; Nguyen, P.T.T.; Hoang, D.T.; Nguyen, N.T.T.; Pham, N.T.Q.; Murray, J.C.; Park, K.; et al. Early Essential Newborn Care can still be used with mothers who have COVID-19 if effective infection control measures are applied. Acta Paediatrica 2021. [Google Scholar] [CrossRef] [PubMed]
| Proportion (%) (n = 433) | Proportion (%) (n = 433) | ||
|---|---|---|---|
| Residence Place: | Mean age (SD), y | 28.4 (4.1) | |
| Da Nang city | 69.8 | Number of Children: | |
| Other provinces | 30.2 | 1 child | 58.9 |
| Education: | 2 children | 37.0 | |
| Up to high school | 26.1 | >2 children | 4.1 |
| Diploma | 19.6 | Birthing place: | |
| College, university | 52.4 | DNHWC | 79.0 |
| Postgraduate | 1.9 | Other hospitals in Da Nang | 17.8 |
| Profession: | Hospitals from other provinces | 3.2 | |
| Worker | 6.2 | Childbirth characteristics: | |
| Farmer | 1.6 | Cesarean section | 57.0 |
| Housewife | 17.6 | Preterm birth | 43.0 |
| White collar job | 74.6 | Donors recruited in DNHWC | 50.3 |
| Community | Hospital | Overall | |
|---|---|---|---|
| Amount of donor milk collected, L | 5062 | 2580 | 7642 |
| Amount of donor milk pasteurized: | |||
| Volume, L | 5007 | 2485 | 7484 |
| Passed pre-pasteurization test (% of Volume) | 92.5 | 83.1 | 89.3 |
| Passed post-pasteurization test (% of Volume) | 90.0 | 82.5 | 87.5 |
| Passed both tests (% of Volume) | 85.5 | 73.7 | 81.7 |
| Neonatal Units (n = 5073) | Postnatal Wards (n = 11,162) | |
|---|---|---|
| Characteristics of recipients: | ||
| Preterm (%) | 35.8 | 4.1 |
| Gestation age, week (Mean, SD) | 35.2 (3.7) | 38.3 (1.4) |
| Birthweight, g (Mean, SD) | 2355 (829) | 3141 (496) |
| Prescription reasons (%): | ||
| Newborns with a birthweight of < 1500 g | 15.1 | 0 |
| Cesarean births | 62.8 | 74.1 |
| Mother absence | 4.4 | 0.2 |
| Mother used medication contradicted to breastfeeding | 0.2 | 0.2 |
| Mothers did not have enough milk | 87.9 | 95.3 |
| Missing data | 7.5 | 4.4 |
| Consumption of PDM: | ||
| Volume of PDM distributed to newborns, L | 3199 | 1907 |
| Average days using PDM, d (median, 25th–75th) | 3 (2–4) | 2 (1–2) |
| Average amount of PDM consumed, mL (median, 25th–75th) | 370 (198–638) | 150 (80–200) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, H.T.; Nguyen, T.T.; Barnett, D.; Weaver, G.; Nguyen, O.T.X.; Van Ngo, Q.; Le, H.T.T.; Huynh, L.T.; Do, C.T.; Mathisen, R. Trends and Dynamics in the First Four Years of Operation of the First Human Milk Bank in Vietnam. Nutrients 2021, 13, 1107. https://doi.org/10.3390/nu13041107
Tran HT, Nguyen TT, Barnett D, Weaver G, Nguyen OTX, Van Ngo Q, Le HTT, Huynh LT, Do CT, Mathisen R. Trends and Dynamics in the First Four Years of Operation of the First Human Milk Bank in Vietnam. Nutrients. 2021; 13(4):1107. https://doi.org/10.3390/nu13041107
Chicago/Turabian StyleTran, Hoang Thi, Tuan Thanh Nguyen, Debbie Barnett, Gillian Weaver, Oanh Thi Xuan Nguyen, Quang Van Ngo, Huong Thi Thanh Le, Le Thi Huynh, Chung Thi Do, and Roger Mathisen. 2021. "Trends and Dynamics in the First Four Years of Operation of the First Human Milk Bank in Vietnam" Nutrients 13, no. 4: 1107. https://doi.org/10.3390/nu13041107
APA StyleTran, H. T., Nguyen, T. T., Barnett, D., Weaver, G., Nguyen, O. T. X., Van Ngo, Q., Le, H. T. T., Huynh, L. T., Do, C. T., & Mathisen, R. (2021). Trends and Dynamics in the First Four Years of Operation of the First Human Milk Bank in Vietnam. Nutrients, 13(4), 1107. https://doi.org/10.3390/nu13041107








