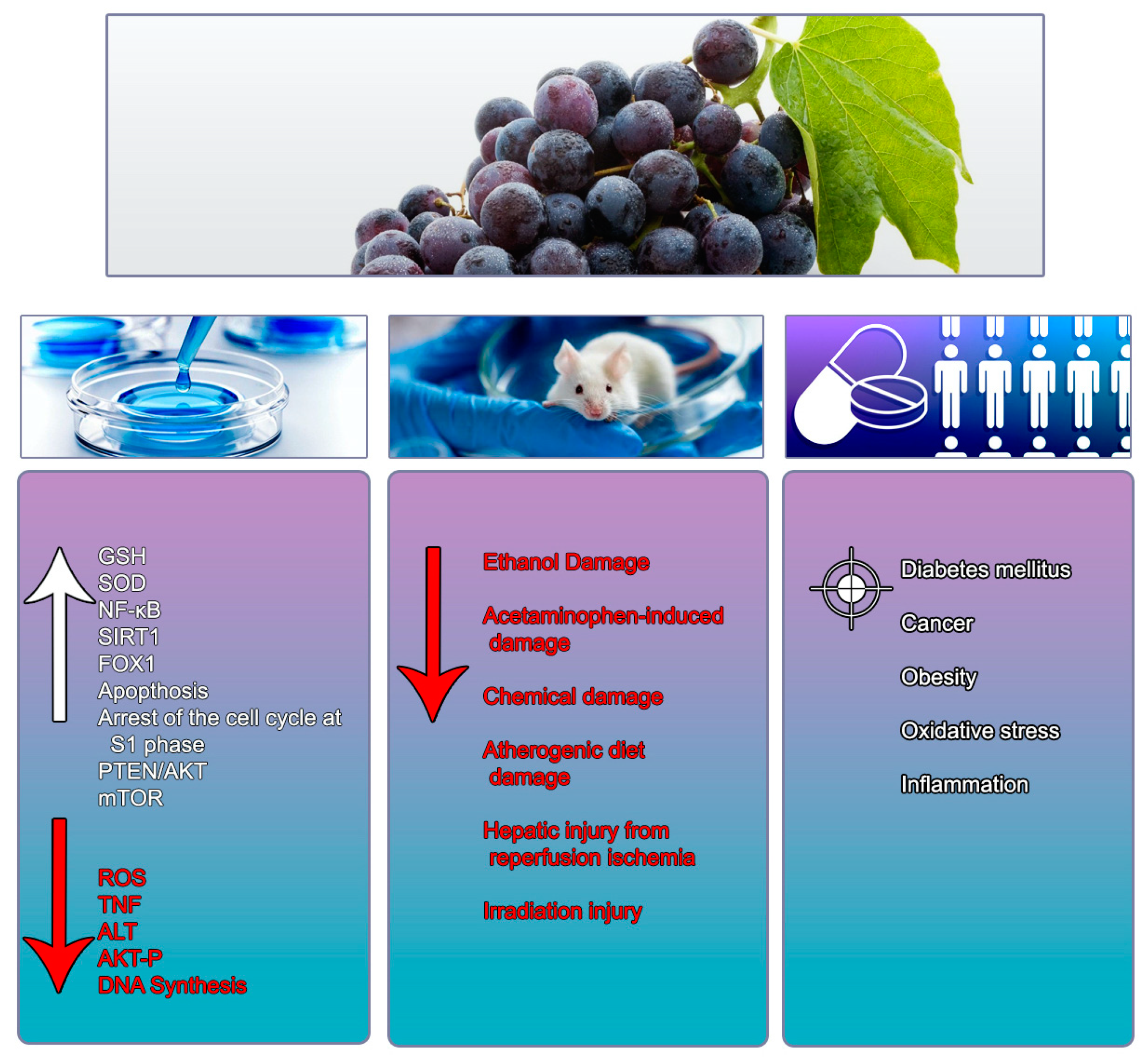
The Role of Resveratrol in Liver Disease: A Comprehensive Review from In Vitro to Clinical Trials
Abstract
1. Introduction
2. Resveratrol and Liver Disease: Molecular Mechanisms
2.1. Steatosis
2.2. Oxidative Stress and Inflammation
2.3. Liver Fibrosis
2.4. Cholestatic Liver Damage
2.5. Hepatocellular Carcinoma and Metastasis
2.6. Hepatic Glucose Metabolism and Diabetes
2.7. Chemical Liver Injury
2.8. Resveratrol and Liver Viruses
3. Resveratrol and Liver Disease: Scientific Evidence in Animal Models
3.1. Paracetamol and Resveratrol
3.2. Ethanol and Resveratrol
3.3. Resveratrol in Chemical-Induced Hepatotoxicity
3.4. Resveratrol in Liver Damage Induced by Atherogenic Diet
3.5. Resveratrol in Liver Ischemia-Reperfusion and Surgical Transplant
3.6. Resveratrol in the Irradiation-Induced Liver Injury Model
4. Liver Disease and Resveratrol: Clinical Trials
4.1. Resveratrol and Non-Alcoholic Fatty Liver Disease
4.2. Effect of Resveratrol on Diabetes Mellitus
4.3. Cancer and Resveratrol
4.4. Obesity and Resveratrol
4.5. Effect of Resveratrol on Other Health Conditions Associated with Oxidative Stress and Inflammation
5. Conclusions, Future Perspectives and Limitations
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- BedÊ, T.P.; Jesuz, V.A.; Souza, V.R.; Elias, M.B.; Oliveira, F.L.; Dias, J.F.; Teodoro, A.J.; Azeredo, V.B. Effects of Grape Juice, Red Wine and Resveratrol on Liver Parameters of Rat Submitted High-fat Diet. An. Acad. Bras. Cienc. 2020, 92, e20191230. [Google Scholar] [CrossRef]
- Baur, J.A.; Sinclair, D.A. Therapeutic Potential of Resveratrol: The in vivo Evidence. Nat. Rev. Drug Discov. 2006, 5, 493–506. [Google Scholar] [CrossRef]
- Shankar, S.; Singh, G.; Srivastava, R.K. Chemoprevention by Resveratrol: Molecular Mechanisms and Therapeutic Potential. Front. Biosci. 2007, 12, 4839–4854. [Google Scholar] [CrossRef]
- Saiko, P.; Szakmary, A.; Jaeger, W.; Szekeres, T. Resveratrol and Its Analogs: Defense against Cancer, Coronary Disease and Neurodegenerative Maladies or Just a Fad? Mutat. Res. 2008, 658, 68–94. [Google Scholar] [CrossRef] [PubMed]
- Shakibaei, M.; Harikumar, K.B.; Aggarwal, B.B. Resveratrol Addiction: To Die or not to Die. Mol. Nutr. Food Res. 2009, 53, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Kawada, N.; Seki, S.; Inoue, M.; Kuroki, T. Effect of Antioxidants, Resveratrol, Quercetin, and N-acetylcysteine, on the Functions of Cultured Rat Hepatic Stellate Cells and Kupffer Cells. Hepatology 1998, 27, 1265–1274. [Google Scholar] [CrossRef] [PubMed]
- Bechmann, L.P.; Zahn, D.; Gieseler, R.K.; Fingas, C.D.; Marquitan, G.; Jochum, C.; Gerken, G.; Friedman, S.L.; Canbay, A. Resveratrol Amplifies Profibrogenic Effects of Free Fatty Acids on Human Hepatic Stellate Cells. Hepatol. Res. 2009, 39, 601–608. [Google Scholar] [CrossRef]
- Berman, A.Y.; Motechin, R.A.; Wiesenfeld, M.Y.; Holz, M.K. The Therapeutic Potential of Resveratrol: A Review of Clinical Trials. NPJ Precis. Oncol. 2017, 1. [Google Scholar] [CrossRef]
- Schmatz, R.; Perreira, L.B.; Stefanello, N.; Mazzanti, C.; Spanevello, R.; Gutierres, J.; Bagatini, M.; Martins, C.C.; Abdalla, F.H.; Daci da Silva Serres, J.; et al. Effects of Resveratrol on Biomarkers of Oxidative Stress and on the Activity of Delta Aminolevulinic Acid Dehydratase in Liver and Kidney of Streptozotocin-induced Diabetic Rats. Biochimie 2012, 94, 374–383. [Google Scholar] [CrossRef]
- Polyzos, S.A.; Kountouras, J.; Mantzoros, C.S. Obesity and Nonalcoholic Fatty Liver Disease: From Pathophysiology to Therapeutics. Metabolism 2019, 92, 82–97. [Google Scholar] [CrossRef]
- Poulsen, M.M.; Larsen, J.; Hamilton-Dutoit, S.; Clasen, B.F.; Jessen, N.; Paulsen, S.K.; Kjær, T.N.; Richelsen, B.; Pedersen, S.B. Resveratrol Up-regulates Hepatic Uncoupling Protein 2 and Prevents Development of Nonalcoholic Fatty Liver Disease in Rats Fed a High-fat Diet. Nutr. Res. 2012, 32, 701–708. [Google Scholar] [CrossRef]
- Liu, C.; Liao, J.Z.; Li, P.Y. Traditional Chinese Herbal Extracts Inducing Autophagy as a Novel Approach in Therapy of Nonalcoholic Fatty Liver Disease. World J. Gastroenterol. 2017, 23, 1964–1973. [Google Scholar] [CrossRef]
- Eseberri, I.; Lasa, A.; Miranda, J.; Gracia, A.; Portillo, M.P. Potential miRNA Involvement in the Anti-adipogenic Effect of Resveratrol and Its Metabolites. PLoS ONE 2017, 12, e0184875. [Google Scholar] [CrossRef] [PubMed]
- Trepiana, J.; Krisa, S.; Renouf, E.; Portillo, M.P. Resveratrol Metabolites Are Able to Reduce Steatosis in Cultured Hepatocytes. Pharmaceuticals 2020, 13, 285. [Google Scholar] [CrossRef] [PubMed]
- Xin, P.; Han, H.; Gao, D.; Cui, W.; Yang, X.; Ying, C.; Sun, X.; Hao, L. Alleviative Effects of Resveratrol on Nonalcoholic Fatty Liver Disease are Associated with up Regulation of Hepatic Low Density Lipoprotein Receptor and Scavenger Receptor Class B Type I Gene Expressions in Rats. Food Chem. Toxicol. 2013, 52, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Alberdi, G.; Rodríguez, V.M.; Macarulla, M.T.; Miranda, J.; Churruca, I.; Portillo, M.P. Hepatic Lipid Metabolic Pathways Modified by Resveratrol in Rats Fed an Obesogenic Diet. Nutrition 2013, 29, 562–567. [Google Scholar] [CrossRef]
- Ding, S.; Jiang, J.; Zhang, G.; Bu, Y.; Zhao, X. Resveratrol and Caloric Restriction Prevent Hepatic Steatosis by Regulating SIRT1-autophagy Pathway and Alleviating Endoplasmic Reticulum Stress in High-fat Diet-fed Rats. PLoS ONE 2017, 12, e0183541. [Google Scholar] [CrossRef]
- Trepiana, J.; Milton-Laskibar, I.; Gómez-Zorita, S.; Eseberri, I.; González, M.; Fernández-Quintela, A.; Portillo, M.P. Involvement of 5’-Activated Protein Kinase (AMPK) in the Effects of Resveratrol on Liver Steatosis. Int. J. Mol. Sci. 2018, 19, 3473. [Google Scholar] [CrossRef] [PubMed]
- Che, Y.; Shi, X.; Zhong, X.; Zhang, Y.; Si, R.; Li, Y.; Shi, Y. Resveratrol Prevents Liver Damage in MCD-induced Steatohepatitis Mice by Promoting SIGIRR Gene Transcription. J. Nutr. Biochem. 2020, 82, 108400. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Yi, L.; Ye, X.; Zeng, X.; Liu, K.; Qin, Y.; Zhang, Q.; Mi, M. Resveratrol Ameliorates Lipid Droplet Accumulation in Liver Through a SIRT1/ATF6-Dependent Mechanism. Cell. Physiol. Biochem. 2018, 51, 2397–2420. [Google Scholar] [CrossRef]
- Khaleel, E.F.; Abdel-Aleem, G.A.; Mostafa, D.G. Resveratrol Improves High-fat Diet Induced Fatty Liver and Insulin Resistance by Concomitantly Inhibiting Proteolytic Cleavage of Sterol Regulatory Element-binding Proteins, Free Fatty Acid Oxidation, and Intestinal Triglyceride Absorption. Can. J. Physiol. Pharmacol. 2018, 96, 145–157. [Google Scholar] [CrossRef]
- Cho, S.J.; Jung, U.J.; Choi, M.S. Differential Effects of Low-dose Resveratrol on Adiposity and Hepatic Steatosis in Diet-induced Obese Mice. Br. J. Nutr. 2012, 108, 2166–2175. [Google Scholar] [CrossRef]
- Bujanda, L.; Hijona, E.; Larzabal, M.; Beraza, M.; Aldazabal, P.; García-Urkia, N.; Sarasqueta, C.; Cosme, A.; Irastorza, B.; González, A.; et al. Resveratrol Inhibits Nonalcoholic Fatty Liver Disease in Rats. BMC Gastroenterol. 2008, 8, 40. [Google Scholar] [CrossRef]
- Gracia, A.; Fernández-Quintela, A.; Miranda, J.; Eseberri, I.; González, M.; Portillo, M.P. Are miRNA-103, miRNA-107 and miRNA-122 Involved in the Prevention of Liver Steatosis Induced by Resveratrol? Nutrients 2017, 9, 360. [Google Scholar] [CrossRef]
- Wang, L.F.; Wang, X.N.; Huang, C.C.; Hu, L.; Xiao, Y.F.; Guan, X.H.; Qian, Y.S.; Deng, K.Y.; Xin, H.B. Inhibition of NAMPT Aggravates High Fat Diet-induced Hepatic Steatosis in Mice Through Regulating Sirt1/AMPKα/SREBP1 Signaling Pathway. Lipids Health Dis. 2017, 16, 82. [Google Scholar] [CrossRef]
- Izdebska, M.; Piątkowska-Chmiel, I.; Korolczuk, A.; Herbet, M.; Gawrońska-Grzywacz, M.; Gieroba, R.; Sysa, M.; Czajkowska-Bania, K.; Cygal, M.; Korga, A.; et al. The Beneficial Effects of Resveratrol on Steatosis and Mitochondrial Oxidative Stress in HepG2 Cells. Can. J. Physiol. Pharmacol. 2017, 95, 1442–1453. [Google Scholar] [CrossRef]
- Hosseini, H.; Teimouri, M.; Shabani, M.; Koushki, M.; Babaei Khorzoughi, R.; Namvarjah, F.; Izadi, P.; Meshkani, R. Resveratrol Alleviates Non-alcoholic Fatty Liver Disease Through Epigenetic Modification of the Nrf2 Signaling Pathway. Int. J. Biochem. Cell. Biol. 2020, 119, 105667. [Google Scholar] [CrossRef]
- Ajmo, J.M.; Liang, X.; Rogers, C.Q.; Pennock, B.; You, M. Resveratrol Alleviates Alcoholic Fatty Liver in Mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2008, 295, G833–G842. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Zhang, H.; Zheng, Y.; Zhou, J.; Yuan, J.; Yu, Y.; Wang, J. Resveratrol Exerts Antioxidant Effects by Activating SIRT2 To Deacetylate Prx1. Biochemistry 2017, 56, 6325–6328. [Google Scholar] [CrossRef]
- Yun, H.; Park, S.; Kim, M.J.; Yang, W.K.; Im, D.U.; Yang, K.R.; Hong, J.; Choe, W.; Kang, I.; Kim, S.S.; et al. AMP-activated Protein Kinase Mediates the Antioxidant Effects of Resveratrol Through Regulation of the Transcription Factor FoxO1. FEBS J. 2014, 281, 4421–4438. [Google Scholar] [CrossRef]
- Yilmaz Demirtas, C.; Bircan, F.S.; Pasaoglu, O.T.; Turkozkan, N. The Effects of Resveratrol on Hepatic Oxidative Stress in Metabolic Syndrome Model Induced by High Fructose Diet. Bratisl. Lek. Listy 2018, 119, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Carrizzo, A.; Izzo, C.; Forte, M.; Sommella, E.; Di Pietro, P.; Venturini, E.; Ciccarelli, M.; Galasso, G.; Rubattu, S.; Campiglia, P.; et al. A Novel Promising Frontier for Human Health: The Beneficial Effects of Nutraceuticals in Cardiovascular Diseases. Int. J. Mol. Sci. 2020, 21, 8706. [Google Scholar] [CrossRef]
- Ferramosca, A.; Di Giacomo, M.; Zara, V. Antioxidant Dietary Approach in Treatment of Fatty Liver: New Insights and Updates. World J. Gastroenterol. 2017, 23, 4146–4157. [Google Scholar] [CrossRef] [PubMed]
- Carrizzo, A.; Forte, M.; Damato, A.; Trimarco, V.; Salzano, F.; Bartolo, M.; Maciag, A.; Puca, A.A.; Vecchione, C. Antioxidant Effects of Resveratrol in Cardiovascular, Cerebral and Metabolic Diseases. Food Chem. Toxicol. 2013, 61, 215–226. [Google Scholar] [CrossRef]
- de Oliveira, M.R.; Chenet, A.L.; Duarte, A.R.; Scaini, G.; Quevedo, J. Molecular Mechanisms Underlying the Anti-depressant Effects of Resveratrol: A Review. Mol. Neurobiol. 2018, 55, 4543–4559. [Google Scholar] [CrossRef]
- Meng, X.; Zhou, J.; Zhao, C.N.; Gan, R.Y.; Li, H.B. Health Benefits and Molecular Mechanisms of Resveratrol: A Narrative Review. Foods 2020, 9, 340. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.S.; Cantó, C. The Molecular Targets of Resveratrol. Biochim. Biophys. Acta 2015, 1852, 1114–1123. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.C.; Ji, J.A.; Jiang, Z.Y.; You, Q.D. The Keap1-Nrf2-ARE Pathway as a Potential Preventive and Therapeutic Target: An Update. Med. Res. Rev. 2016, 36, 924–963. [Google Scholar] [CrossRef]
- Ahmed, S.M.; Luo, L.; Namani, A.; Wang, X.J.; Tang, X. Nrf2 Signaling Pathway: Pivotal Roles in Inflammation. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 585–597. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Li, Y.; Du, Y.; Li, G.; Wang, L.; Zhou, F. Resveratrol Ameliorated Vascular Calcification by Regulating Sirt-1 and Nrf2. Transplant. Proc. 2016, 48, 3378–3386. [Google Scholar] [CrossRef]
- Bellezza, I.; Giambanco, I.; Minelli, A.; Donato, R. Nrf2-Keap1 Signaling in Oxidative and Reductive Stress. Biochim. Biophys. Acta Mol. Cell Res. 2018, 1865, 721–733. [Google Scholar] [CrossRef]
- Shaw, P.; Chattopadhyay, A. Nrf2-ARE Signaling in Cellular Protection: Mechanism of Action and the Regulatory Mechanisms. J. Cell. Physiol. 2020, 235, 3119–3130. [Google Scholar] [CrossRef] [PubMed]
- Harikumar, K.B.; Aggarwal, B.B. Resveratrol: A Multitargeted Agent for Age-associated Chronic Diseases. Cell Cycle 2008, 7, 1020–1035. [Google Scholar] [CrossRef] [PubMed]
- McCubrey, J.A.; Lertpiriyapong, K.; Steelman, L.S.; Abrams, S.L.; Cocco, L.; Ratti, S.; Martelli, A.M.; Candido, S.; Libra, M.; Montalto, G.; et al. Regulation of GSK-3 Activity by Curcumin, Berberine and Resveratrol: Potential Effects on Multiple Diseases. Adv. Biol. Regul. 2017, 65, 77–88. [Google Scholar] [CrossRef]
- Bae, M.; Park, Y.K.; Lee, J.Y. Food Components with Antifibrotic Activity and Implications in Prevention of Liver Disease. J. Nutr. Biochem. 2018, 55, 1–11. [Google Scholar] [CrossRef]
- Hessin, A.F.; Hegazy, R.R.; Hassan, A.A.; Yassin, N.Z.; Kenawy, S.A. Resveratrol Prevents Liver Fibrosis via Two Possible Pathways: Modulation of Alpha Fetoprotein Transcriptional Levels and Normalization of Protein Kinase C Responses. Indian J. Pharmacol. 2017, 49, 282–289. [Google Scholar] [CrossRef]
- Di Pascoli, M.; Diví, M.; Rodríguez-Vilarrupla, A.; Rosado, E.; Gracia-Sancho, J.; Vilaseca, M.; Bosch, J.; García-Pagán, J.C. Resveratrol Improves Intrahepatic Endothelial Dysfunction and Reduces Hepatic Fibrosis and Portal Pressure in Cirrhotic Rats. J. Hepatol. 2013, 58, 904–910. [Google Scholar] [CrossRef]
- Xu, M.; Xue, W.; Ma, Z.; Bai, J.; Wu, S. Resveratrol Reduces the Incidence of Portal Vein System Thrombosis after Splenectomy in a Rat Fibrosis Model. Oxid. Med. Cell. Longev. 2016, 2016, 7453849. [Google Scholar] [CrossRef]
- de Oliveira, C.M.; Martins, L.A.M.; de Sousa, A.C.; Moraes, K.D.S.; Costa, B.P.; Vieira, M.Q.; Coelho, B.P.; Borojevic, R.; de Oliveira, J.R.; Guma, F.C.R. Resveratrol Increases the Activation Markers and Changes the Release of Inflammatory Cytokines of Hepatic Stellate Cells. Mol. Cell. Biochem. 2020. [Google Scholar] [CrossRef]
- Zhang, D.Q.; Sun, P.; Jin, Q.; Li, X.; Zhang, Y.; Zhang, Y.J.; Wu, Y.L.; Nan, J.X.; Lian, L.H. Resveratrol Regulates Activated Hepatic Stellate Cells by Modulating NF-κB and the PI3K/Akt Signaling Pathway. J. Food Sci. 2016, 81, H240–H245. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Mou, Q.; Wang, Y.; Zhu, Z.; Cheng, M. Resveratrol Contributes to the Inhibition of Liver Fibrosis by Inducing Autophagy via the microRNA-20a-mediated Activation of the PTEN/PI3K/AKT Signaling Pathway. Int. J. Mol. Med. 2020, 46, 2035–2046. [Google Scholar] [CrossRef]
- Abdu, S.B.; Al-Bogami, F.M. Influence of Resveratrol on Liver Fibrosis Induced by Dimethylnitrosamine in Male Rats. Saudi J. Biol. Sci. 2019, 26, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.S.; Shin, M.O.; Yoon, S.; Moon, J.O. Resveratrol Inhibits Dimethylnitrosamine-induced Hepatic Fibrosis in Rats. Arch. Pharm. Res. 2010, 33, 925–932. [Google Scholar] [CrossRef]
- Hong, S.W.; Jung, K.H.; Zheng, H.M.; Lee, H.S.; Suh, J.K.; Park, I.S.; Lee, D.H.; Hong, S.S. The Protective Effect of Resveratrol on Dimethylnitrosamine-induced Liver Fibrosis in Rats. Arch. Pharm. Res. 2010, 33, 601–609. [Google Scholar] [CrossRef]
- Chan, C.C.; Cheng, L.Y.; Lin, C.L.; Huang, Y.H.; Lin, H.C.; Lee, F.Y. The Protective Role of Natural Phytoalexin Resveratrol on Inflammation, Fibrosis and Regeneration in Cholestatic Liver Injury. Mol. Nutr. Food Res. 2011, 55, 1841–1849. [Google Scholar] [CrossRef]
- Ding, L.; Zhang, B.; Li, J.; Yang, L.; Wang, Z. Beneficial Effect of Resveratrol on α-naphthyl Isothiocyanate-induced Cholestasis via Regulation of the FXR Pathway. Mol. Med. Rep. 2018, 17, 1863–1872. [Google Scholar] [CrossRef] [PubMed]
- Chambers, K.F.; Day, P.E.; Aboufarrag, H.T.; Kroon, P.A. Polyphenol Effects on Cholesterol Metabolism via Bile Acid Biosynthesis, CYP7A1: A Review. Nutrients 2019, 11, 2588. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Zhou, Z.X.; Sun, L.X.; Li, X.; Xu, Z.M.; Chen, M.; Zhao, G.L.; Jiang, Z.Z.; Zhang, L.Y. Resveratrol Effectively Attenuates α-naphthyl-isothiocyanate-induced Acute Cholestasis and Liver Injury Through Choleretic and Anti-inflammatory Mechanisms. Acta Pharmacol. Sin. 2014, 35, 1527–1536. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Adhami, V.M.; Afaq, F.; Feyes, D.K.; Mukhtar, H. Resveratrol Causes WAF-1/p21-mediated G(1)-phase Arrest of Cell Cycle and Induction of Apoptosis in Human Epidermoid Carcinoma A431 Cells. Clin. Cancer Res. 2001, 7, 1466–1473. [Google Scholar]
- Dörrie, J.; Gerauer, H.; Wachter, Y.; Zunino, S.J. Resveratrol Induces Extensive Apoptosis by Depolarizing Mitochondrial Membranes and Activating Caspase-9 in Acute Lymphoblastic Leukemia Cells. Cancer Res. 2001, 61, 4731–4739. [Google Scholar]
- Tinhofer, I.; Bernhard, D.; Senfter, M.; Anether, G.; Loeffler, M.; Kroemer, G.; Kofler, R.; Csordas, A.; Greil, R. Resveratrol, a Tumor-suppressive Compound from Grapes, Induces Apoptosis via a Novel Mitochondrial Pathway Controlled by Bcl-2. FASEB J. 2001, 15, 1613–1615. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.H.; Sethi, G.; Um, J.Y.; Shanmugam, M.K.; Arfuso, F.; Kumar, A.P.; Bishayee, A.; Ahn, K.S. The Role of Resveratrol in Cancer Therapy. Int. J. Mol. Sci. 2017, 18, 2589. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Zhang, J.; Zeng, J.; Li, Z.; Zuo, H.; Huang, C.; Zhao, X. Nano-Gold Loaded with Resveratrol Enhance the Anti-Hepatoma Effect of Resveratrol. J. Biomed. Nanotechnol. 2019, 15, 288–300. [Google Scholar] [CrossRef] [PubMed]
- Karabekir, S.C.; Özgörgülü, A. Possible Protective Effects of Resveratrol in Hepatocellular Carcinoma. Iran J. Basic. Med. Sci. 2020, 23, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Okada, H.; Mak, T.W. Pathways of Apoptotic and Non-apoptotic Death in Tumour Cells. Nat. Rev. Cancer 2004, 4, 592–603. [Google Scholar] [CrossRef] [PubMed]
- Zirbes, T.; Novotny, G.E. Quantification of Thymic Innervation in Juvenile and Aged Rats. Acta Anat. 1992, 145, 283–288. [Google Scholar] [CrossRef]
- Ashkenazi, A.; Dixit, V.M. Apoptosis Control by Death and Decoy Receptors. Curr. Opin. Cell Biol. 1999, 11, 255–260. [Google Scholar] [CrossRef]
- van Loo, G.; Saelens, X.; van Gurp, M.; MacFarlane, M.; Martin, S.J.; Vandenabeele, P. The Role of Mitochondrial Factors in Apoptosis: A Russian Roulette with More than One Bullet. Cell Death Differ. 2002, 9, 1031–1042. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Fang, M.; Li, Y.; Li, L.; Wang, X. Smac, a Mitochondrial Protein that Promotes Cytochrome C-dependent Caspase Activation by Eliminating IAP Inhibition. Cell 2000, 102, 33–42. [Google Scholar] [CrossRef]
- Clément, M.V.; Hirpara, J.L.; Chawdhury, S.H.; Pervaiz, S. Chemopreventive Agent Resveratrol, a Natural Product Derived from Grapes, Triggers CD95 Signaling-dependent Apoptosis in Human Tumor Cells. Blood 1998, 92, 996–1002. [Google Scholar] [CrossRef]
- Delmas, D.; Rébé, C.; Lacour, S.; Filomenko, R.; Athias, A.; Gambert, P.; Cherkaoui-Malki, M.; Jannin, B.; Dubrez-Daloz, L.; Latruffe, N.; et al. Resveratrol-induced Apoptosis is Associated with Fas Redistribution in the Rafts and the Formation of a Death-inducing Signaling Complex in Colon Cancer Cells. J. Biol. Chem. 2003, 278, 41482–41490. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Mao, Q.Q.; Qin, J.; Zheng, X.Y.; Wang, Y.B.; Yang, K.; Shen, H.F.; Xie, L.P. Resveratrol Induces Apoptosis and Cell Cycle Arrest of Human T24 Bladder Cancer Cells in vitro and Inhibits Tumor Growth in vivo. Cancer Sci. 2010, 101, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.H.; Nihal, M.; Fu, V.X.; Jarrard, D.F.; Ahmad, N. Resveratrol-caused Apoptosis of Human Prostate Carcinoma LNCaP Cells is Mediated via Modulation of Phosphatidylinositol 3’-kinase/Akt Pathway and Bcl-2 Family Proteins. Mol. Cancer Ther. 2006, 5, 1335–1341. [Google Scholar] [CrossRef] [PubMed]
- Faber, A.C.; Dufort, F.J.; Blair, D.; Wagner, D.; Roberts, M.F.; Chiles, T.C. Inhibition of Phosphatidylinositol 3-kinase-mediated Glucose Metabolism Coincides with Resveratrol-induced Cell Cycle Arrest in Human Diffuse Large B-cell Lymphomas. Biochem. Pharmacol. 2006, 72, 1246–1256. [Google Scholar] [CrossRef]
- Banerjee Mustafi, S.; Chakraborty, P.K.; Raha, S. Modulation of Akt and ERK1/2 Pathways by Resveratrol in Chronic Myelogenous Leukemia (CML) Cells Results in the Downregulation of Hsp70. PLoS ONE 2010, 5, e8719. [Google Scholar] [CrossRef]
- Parekh, P.; Motiwale, L.; Naik, N.; Rao, K.V. Downregulation of Cyclin D1 is Associated with Decreased Levels of p38 MAP Kinases, Akt/PKB and Pak1 during Chemopreventive Effects of Resveratrol in Liver Cancer Cells. Exp. Toxicol. Pathol. 2011, 63, 167–173. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Wang, Y.; Zhu, J.; Orloff, M.; Eng, C. Resveratrol Enhances the Anti-tumor Activity of the mTOR Inhibitor Rapamycin in Multiple Breast Cancer Cell Lines Mainly by Suppressing Rapamycin-induced AKT Signaling. Cancer Lett. 2011, 301, 168–176. [Google Scholar] [CrossRef]
- Colin, D.; Limagne, E.; Jeanningros, S.; Jacquel, A.; Lizard, G.; Athias, A.; Gambert, P.; Hichami, A.; Latruffe, N.; Solary, E.; et al. Endocytosis of Resveratrol via Lipid Rafts and Activation of Downstream Signaling Pathways in Cancer Cells. Cancer Prev. Res. 2011, 4, 1095–1106. [Google Scholar] [CrossRef]
- Pozo-Guisado, E.; Merino, J.M.; Mulero-Navarro, S.; Lorenzo-Benayas, M.J.; Centeno, F.; Alvarez-Barrientos, A.; Fernandez-Salguero, P.M.; Salguero, P.M. Resveratrol-induced Apoptosis in MCF-7 Human Breast Cancer Cells Involves a Caspase-independent Mechanism with Downregulation of Bcl-2 and NF-kappaB. Int. J. Cancer 2005, 115, 74–84. [Google Scholar] [CrossRef]
- Benitez, D.A.; Hermoso, M.A.; Pozo-Guisado, E.; Fernández-Salguero, P.M.; Castellón, E.A. Regulation of Cell Survival by Resveratrol Involves Inhibition of NF Kappa B-regulated Gene Expression in Prostate Cancer Cells. Prostate 2009, 69, 1045–1054. [Google Scholar] [CrossRef]
- Bhardwaj, A.; Sethi, G.; Vadhan-Raj, S.; Bueso-Ramos, C.; Takada, Y.; Gaur, U.; Nair, A.S.; Shishodia, S.; Aggarwal, B.B. Resveratrol Inhibits Proliferation, Induces Apoptosis, and Overcomes Chemoresistance through Down-regulation of STAT3 and Nuclear Factor-kappaB-regulated Antiapoptotic and Cell Survival Gene Products in Human Multiple Myeloma Cells. Blood 2007, 109, 2293–2302. [Google Scholar] [CrossRef] [PubMed]
- Siveen, K.S.; Sikka, S.; Surana, R.; Dai, X.; Zhang, J.; Kumar, A.P.; Tan, B.K.; Sethi, G.; Bishayee, A. Targeting the STAT3 Signaling Pathway in Cancer: Role of Synthetic and Natural Inhibitors. Biochim. Biophys. Acta 2014, 1845, 136–154. [Google Scholar] [CrossRef]
- Yu, H.; Pardoll, D.; Jove, R. STATs in Cancer Inflammation and Immunity: A Leading Role for STAT3. Nat. Rev. Cancer 2009, 9, 798–809. [Google Scholar] [CrossRef] [PubMed]
- Rajasekaran, D.; Elavarasan, J.; Sivalingam, M.; Ganapathy, E.; Kumar, A.; Kalpana, K.; Sakthisekaran, D. Resveratrol Interferes with N-nitrosodiethylamine-induced Hepatocellular Carcinoma at Early and Advanced Stages in Male Wistar Rats. Mol. Med. Rep. 2011, 4, 1211–1217. [Google Scholar] [CrossRef]
- Bishayee, A.; Dhir, N. Resveratrol-mediated Chemoprevention of Diethylnitrosamine-initiated Hepatocarcinogenesis: Inhibition of Cell Proliferation and Induction of Apoptosis. Chem. Biol. Interact. 2009, 179, 131–144. [Google Scholar] [CrossRef]
- Wu, X.; Li, C.; Xing, G.; Qi, X.; Ren, J. Resveratrol Downregulates Cyp2e1 and Attenuates Chemically Induced Hepatocarcinogenesis in SD Rats. J. Toxicol. Pathol. 2013, 26, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Teng, Y.C.; Shen, Z.Q.; Kao, C.H.; Tsai, T.F. Hepatocellular Carcinoma Mouse Models: Hepatitis B Virus-associated Hepatocarcinogenesis and Haploinsufficient Tumor Suppressor Genes. World J. Gastroenterol. 2016, 22, 300–325. [Google Scholar] [CrossRef]
- Mbimba, T.; Awale, P.; Bhatia, D.; Geldenhuys, W.J.; Darvesh, A.S.; Carroll, R.T.; Bishayee, A. Alteration of Hepatic Proinflammatory Cytokines is Involved in the Resveratrol-mediated Chemoprevention of Chemically-induced Hepatocarcinogenesis. Curr. Pharm. Biotechnol. 2012, 13, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Talib, W.H.; Alsayed, A.R.; Farhan, F.; Al Kury, L.T. Resveratrol and Tumor Microenvironment: Mechanistic Basis and Therapeutic Targets. Molecules 2020, 25, 4282. [Google Scholar] [CrossRef]
- Yu, L.; Sun, Z.J.; Wu, S.L.; Pan, C.E. Effect of Resveratrol on Cell Cycle Proteins in Murine Transplantable Liver Cancer. World J. Gastroenterol. 2003, 9, 2341–2343. [Google Scholar] [CrossRef]
- Miura, D.; Miura, Y.; Yagasaki, K. Restoration by Prostaglandins E(2) and F (2) (alpha) of Resveratrol-Induced Suppression of Hepatoma Cell Invasion in Culture. Cytotechnology 2003, 43, 155–159. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Notas, G.; Nifli, A.P.; Kampa, M.; Vercauteren, J.; Kouroumalis, E.; Castanas, E. Resveratrol Exerts Its Antiproliferative Effect on HepG2 Hepatocellular Carcinoma Cells, by Inducing Cell Cycle Arrest, and NOS Activation. Biochim. Biophys. Acta 2006, 1760, 1657–1666. [Google Scholar] [CrossRef]
- Yonamine, C.Y.; Pinheiro-Machado, E.; Michalani, M.L.; Alves-Wagner, A.B.; Esteves, J.V.; Freitas, H.S.; Machado, U.F. Resveratrol Improves Glycemic Control in Type 2 Diabetic Obese Mice by Regulating Glucose Transporter Expression in Skeletal Muscle and Liver. Molecules 2017, 22, 1180. [Google Scholar] [CrossRef] [PubMed]
- Szkudelska, K.; Deniziak, M.; Hertig, I.; Wojciechowicz, T.; Tyczewska, M.; Jaroszewska, M.; Szkudelski, T. Effects of Resveratrol in Goto-Kakizaki Rat, a Model of Type 2 Diabetes. Nutrients 2019, 11, 2488. [Google Scholar] [CrossRef] [PubMed]
- Luo, G.; Huang, B.; Qiu, X.; Xiao, L.; Wang, N.; Gao, Q.; Yang, W.; Hao, L. Resveratrol Attenuates Excessive Ethanol Exposure Induced Insulin Resistance in Rats via Improving NAD. Mol. Nutr. Food Res. 2017, 61. [Google Scholar] [CrossRef]
- Rehman, K.; Saeed, K.; Munawar, S.M.; Akash, M.S.H. Resveratrol Regulates Hyperglycemia-induced Modulations in Experimental Diabetic Animal Model. Biomed. Pharmacother. 2018, 102, 140–146. [Google Scholar] [CrossRef]
- Sebai, H.; Sani, M.; Yacoubi, M.T.; Aouani, E.; Ghanem-Boughanmi, N.; Ben-Attia, M. Resveratrol, a Red Wine Polyphenol, Attenuates Lipopolysaccharide-induced Oxidative Stress in Rat Liver. Ecotoxicol. Environ. Saf. 2010, 73, 1078–1083. [Google Scholar] [CrossRef] [PubMed]
- Rocha, K.K.; Souza, G.A.; Ebaid, G.X.; Seiva, F.R.; Cataneo, A.C.; Novelli, E.L. Resveratrol Toxicity: Effects on Risk Factors for Atherosclerosis and Hepatic Oxidative Stress in Standard and High-fat Diets. Food Chem. Toxicol. 2009, 47, 1362–1367. [Google Scholar] [CrossRef]
- Palsamy, P.; Subramanian, S. Resveratrol, a Natural Phytoalexin, Normalizes Hyperglycemia in Streptozotocin-nicotinamide Induced Experimental Diabetic Rats. Biomed. Pharmacother. 2008, 62, 598–605. [Google Scholar] [CrossRef] [PubMed]
- Rai, R.C.; Bagul, P.K.; Banerjee, S.K. NLRP3 Inflammasome Drives Inflammation in High Fructose Fed Diabetic Rat Liver: Effect of Resveratrol and Metformin. Life Sci. 2020, 253, 117727. [Google Scholar] [CrossRef]
- Oyenihi, O.R.; Oyenihi, A.B.; Adeyanju, A.A.; Oguntibeju, O.O. Antidiabetic Effects of Resveratrol: The Way Forward in Its Clinical Utility. J. Diabetes Res. 2016, 2016, 9737483. [Google Scholar] [CrossRef]
- Rivera, H.; Shibayama, M.; Tsutsumi, V.; Perez-Alvarez, V.; Muriel, P. Resveratrol and trimethylated resveratrol protect from acute liver damage induced by CCl4 in the rat. J. Appl. Toxicol. 2008, 28, 147–155. [Google Scholar] [CrossRef]
- Mohseni, R.; Arab Sadeghabadi, Z.; Goodarzi, M.T.; Karimi, J. Co-administration of Resveratrol and Beta-aminopropionitrile Attenuates Liver Fibrosis Development via Targeting Lysyl Oxidase in CCl. Immunopharmacol. Immunotoxicol. 2019, 41, 644–651. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Qin, S.Y.; Hu, B.L.; Qin, Q.Y.; Jiang, H.X.; Luo, W. Resveratrol Improves CCL4-induced Liver Fibrosis in Mouse by Upregulating Endogenous IL-10 to Reprogramme Macrophages Phenotype from M(LPS) to M(IL-4). Biomed. Pharmacother. 2019, 117, 109110. [Google Scholar] [CrossRef] [PubMed]
- Faghihzadeh, F.; Hekmatdoost, A.; Adibi, P. Resveratrol and Liver: A Systematic Review. J. Res. Med. Sci. 2015, 20, 797–810. [Google Scholar] [CrossRef]
- Vairappan, B.; Sundhar, M.; Srinivas, B.H. Resveratrol Restores Neuronal Tight Junction Proteins Through Correction of Ammonia and Inflammation in CCl. Mol. Neurobiol. 2019, 56, 4718–4729. [Google Scholar] [CrossRef]
- Cheng, K.; Yan, E.; Song, Z.; Li, S.; Zhang, H.; Zhang, L.; Wang, C.; Wang, T. Protective Effect of Resveratrol Against Hepatic Damage Induced by Heat Stress in a Rat Model is Associated with the Regulation of Oxidative Stress and Inflammation. J. Therm. Biol. 2019, 82, 70–75. [Google Scholar] [CrossRef]
- Filardo, S.; Di Pietro, M.; Mastromarino, P.; Sessa, R. Therapeutic Potential of Resveratrol Against Emerging Respiratory Viral Infections. Pharmacol. Ther. 2020, 214, 107613. [Google Scholar] [CrossRef] [PubMed]
- Date, A.A.; Destache, C.J. Natural Polyphenols: Potential in the Prevention of Sexually Transmitted Viral Infections. Drug Discov. Today 2016, 21, 333–341. [Google Scholar] [CrossRef]
- Yang, T.; Li, S.; Zhang, X.; Pang, X.; Lin, Q.; Cao, J. Resveratrol, Sirtuins, and Viruses. Rev. Med. Virol. 2015, 25, 431–445. [Google Scholar] [CrossRef]
- Annunziata, G.; Maisto, M.; Schisano, C.; Ciampaglia, R.; Narciso, V.; Tenore, G.C.; Novellino, E. Resveratrol as a Novel Anti-Herpes Simplex Virus Nutraceutical Agent: An Overview. Viruses 2018, 10, 473. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Saito, H.; Ikeda, M.; Hokari, R.; Kato, N.; Hibi, T.; Miura, S. An Antioxidant Resveratrol Significantly Enhanced Replication of Hepatitis C Virus. World J. Gastroenterol. 2010, 16, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Gu, Y.; Ye, J.; Liu, F.; Zhao, Y.; Wang, C.; Xu, Y.; Cao, X.; Zhang, L.; Dong, W.; et al. Resveratrol Prevents Hepatic Steatosis Induced by Hepatitis C Virus Core Protein. Biotechnol. Lett. 2012, 34, 2205–2212. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.J.; Kong, K.E.; Gao, W.W.; Tang, H.V.; Chaudhary, V.; Cheng, Y.; Zhou, J.; Chan, C.P.; Wong, D.K.; Yuen, M.F.; et al. Interplay between SIRT1 and Hepatitis B Virus X Protein in the Activation of Viral Transcription. Biochim. Biophys. Acta Gene. Regul. Mech. 2017, 1860, 491–501. [Google Scholar] [CrossRef]
- Park, S.; Lim, J.; Kim, J.R.; Cho, S. Inhibitory Effects of Resveratrol on Hepatitis B Virus X Protein-induced Hepatocellular Carcinoma. J. Vet. Sci. 2017, 18, 419–429. [Google Scholar] [CrossRef]
- Larson, A.M.; Polson, J.; Fontana, R.J.; Davern, T.J.; Lalani, E.; Hynan, L.S.; Reisch, J.S.; Schiødt, F.V.; Ostapowicz, G.; Shakil, A.O.; et al. Acetaminophen-induced Acute Liver Failure: Results of a United States Multicenter, Prospective Study. Hepatology 2005, 42, 1364–1372. [Google Scholar] [CrossRef]
- Sheen, C.L.; Dillon, J.F.; Bateman, D.N.; Simpson, K.J.; Macdonald, T.M. Paracetamol Toxicity: Epidemiology, Prevention and Costs to the Health-care System. QJM 2002, 95, 609–619. [Google Scholar] [CrossRef]
- Fontana, R.J. Acute Liver Failure Including Acetaminophen Overdose. Med. Clin. North Am. 2008, 92, 761–794. [Google Scholar] [CrossRef]
- Elbe, H.; Gul, M.; Cetin, A.; Taslidere, E.; Ozyalin, F.; Turkoz, Y.; Otlu, A. Resveratrol Reduces Light and Electron Microscopic Changes in Acetaminophen-induced Hepatotoxicity in Rats: Role of iNOS Expression. Ultrastruct. Pathol. 2018, 42, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Heard, K.J. Acetylcysteine for Acetaminophen Poisoning. N. Engl. J. Med. 2008, 359, 285–292. [Google Scholar] [CrossRef]
- Linden, C.H.; Rumack, B.H. Acetaminophen Overdose. Emerg. Med. Clin. N. Am. 1984, 2, 103–119. [Google Scholar] [CrossRef]
- Sener, G.; Toklu, H.Z.; Sehirli, A.O.; Velioğlu-Oğünç, A.; Cetinel, S.; Gedik, N. Protective Effects of Resveratrol Against Acetaminophen-induced Toxicity in Mice. Hepatol. Res. 2006, 35, 62–68. [Google Scholar] [CrossRef]
- Masubuchi, Y.; Sugiyama, S.; Horie, T. Th1/Th2 Cytokine Balance as a Determinant of Acetaminophen-induced Liver Injury. Chem. Biol. Interact. 2009, 179, 273–279. [Google Scholar] [CrossRef]
- Oliva, J.; French, B.A.; Li, J.; Bardag-Gorce, F.; Fu, P.; French, S.W. Sirt1 is Involved in Energy Metabolism: The Role of Chronic Ethanol Feeding and Resveratrol. Exp. Mol. Pathol. 2008, 85, 155–159. [Google Scholar] [CrossRef]
- Li, S.; Tan, H.Y.; Wang, N.; Zhang, Z.J.; Lao, L.; Wong, C.W.; Feng, Y. The Role of Oxidative Stress and Antioxidants in Liver Diseases. Int. J. Mol. Sci. 2015, 16, 26087–26124. [Google Scholar] [CrossRef]
- Ballardini, G.; De Raffele, E.; Groff, P.; Bioulac-Sage, P.; Grassi, A.; Ghetti, S.; Susca, M.; Strazzabosco, M.; Bellusci, R.; Iemmolo, R.M.; et al. Timing of Reinfection and Mechanisms of Hepatocellular Damage in Transplanted Hepatitis C Virus-reinfected Liver. Liver Transpl. 2002, 8, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Strazzabosco, M.; Allen, J.I.; Teisberg, E.O. Value-based Care in Hepatology. Hepatology 2017, 65, 1749–1755. [Google Scholar] [CrossRef] [PubMed]
- Lieber, C.S. Alcoholic Fatty Liver: Its Pathogenesis and Mechanism of Progression to Inflammation and Fibrosis. Alcohol 2004, 34, 9–19. [Google Scholar] [CrossRef]
- Lieber, C.S. Metabolism of Alcohol. Clin. Liver Dis. 2005, 9, 1–35. [Google Scholar] [CrossRef]
- Lieber, C.S. Pathogenesis and Treatment of Alcoholic Liver Disease: Progress over the Last 50 Years. Rocz. Akad. Med. Bialymst. 2005, 50, 7–20. [Google Scholar]
- Bujanda, L.; García-Barcina, M.; Gutiérrez-de Juan, V.; Bidaurrazaga, J.; de Luco, M.F.; Gutiérrez-Stampa, M.; Larzabal, M.; Hijona, E.; Sarasqueta, C.; Echenique-Elizondo, M.; et al. Effect of Resveratrol on Alcohol-induced Mortality and Liver Lesions in Mice. BMC Gastroenterol. 2006, 6, 35. [Google Scholar] [CrossRef] [PubMed]
- Kasdallah-Grissa, A.; Mornagui, B.; Aouani, E.; Hammami, M.; Gharbi, N.; Kamoun, A.; El-Fazaa, S. Protective Effect of Resveratrol on Ethanol-induced Lipid Peroxidation in Rats. Alcohol Alcohol. 2006, 41, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Kasdallah-Grissa, A.; Mornagui, B.; Aouani, E.; Hammami, M.; El May, M.; Gharbi, N.; Kamoun, A.; El-Fazaâ, S. Resveratrol, a Red Wine Polyphenol, Attenuates Ethanol-induced Oxidative Stress in Rat Liver. Life Sci. 2007, 80, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
- Eybl, V.; Kotyzova, D.; Koutensky, J. Comparative Study of Natural Antioxidants–Curcumin, Resveratrol and Melatonin–in Cadmium-induced Oxidative Damage in Mice. Toxicology 2006, 225, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Meng, C.Y.; Han, Y.F.; Liu, Y.L.; Gao, H.X.; Ren, Y.Y.; Qian, Q.Z.; Wang, Q.; Li, Q.Z. Resveratrol Alleviate the Injury of Mice Liver Induced by Cadmium Sulfide Nanoparticles. Kaohsiung J. Med. Sci. 2019, 35, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Sehirli, O.; Tozan, A.; Omurtag, G.Z.; Cetinel, S.; Contuk, G.; Gedik, N.; Sener, G. Protective Effect of Resveratrol against Naphthalene-induced Oxidative Stress in Mice. Ecotoxicol. Environ. Saf. 2008, 71, 301–308. [Google Scholar] [CrossRef]
- Upadhyay, G.; Singh, A.K.; Kumar, A.; Prakash, O.; Singh, M.P. Resveratrol Modulates Pyrogallol-induced Changes in Hepatic Toxicity Markers, Xenobiotic Metabolizing Enzymes and Oxidative Stress. Eur. J. Pharmacol. 2008, 596, 146–152. [Google Scholar] [CrossRef]
- Farghali, H.; Cerný, D.; Kameníková, L.; Martínek, J.; Horínek, A.; Kmonícková, E.; Zídek, Z. Resveratrol Attenuates Lipopolysaccharide-induced Hepatitis in D-galactosamine Sensitized Rats: Role of Nitric Oxide Synthase 2 and Heme Oxygenase-1. Nitric Oxide 2009, 21, 216–225. [Google Scholar] [CrossRef]
- Qian, J.; Zha, L.; Wang, B.; Zhang, C.; Hong, L.; Chen, W. Synthesis, Cytotoxicity and Liver Targeting of 3-O-β-D-Galactosylated Resveratrol. J. Pharm. Pharmacol. 2019, 71, 929–936. [Google Scholar] [CrossRef]
- Sun, S.; Zhang, M.; Yang, Q.; Shen, Z.; Chen, J.; Yu, B.; Wang, H.; Qu, J.; Pang, D.; Ren, W.; et al. Resveratrol Suppresses Lipoprotein-associated Phospholipase A. Mol. Nutr. Food Res. 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Huminiecki, L.; Atanasov, A.G.; Horbańczuk, J. Etiology of Atherosclerosis Informs Choice of Animal Models and Tissues for Initial Functional Genomic Studies of Resveratrol. Pharmacol. Res. 2020, 156, 104598. [Google Scholar] [CrossRef]
- Fernández-Quintela, A.; Milton-Laskibar, I.; González, M.; Portillo, M.P. Antiobesity Effects of Resveratrol: Which Tissues are Involved? Ann. NY Acad. Sci. 2017, 1403, 118–131. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Gao, J.; Ke, W.; Wang, J.; Li, D.; Liu, R.; Jia, Y.; Wang, X.; Chen, X.; Chen, F.; et al. Resveratrol Reduces Obesity in High-fat Diet-fed Mice via Modulating the Composition and Metabolic Function of the Gut Microbiota. Free Radic. Biol. Med. 2020, 156, 83–98. [Google Scholar] [CrossRef]
- Xu, L.; Wang, R.; Liu, H.; Wang, J.; Mang, J.; Xu, Z. Resveratrol Treatment Is Associated with Lipid Regulation and Inhibition of Lipoprotein-Associated Phospholipase A2 (Lp-PLA2) in Rabbits Fed a High-Fat Diet. Evid. Based Complement. Alternat. Med. 2020, 2020, 9641582. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.; Song, Z.; Zhang, H.; Li, S.; Wang, C.; Zhang, L.; Wang, T. The Therapeutic Effects of Resveratrol on Hepatic Steatosis in High-fat Diet-induced Obese Mice by Improving Oxidative Stress, Inflammation and Lipid-related Gene Transcriptional Expression. Med. Mol. Morphol. 2019, 52, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.; Cho, I.; Kim, S.; Kwon, D.; Ha, T. Dietary Resveratrol Alters Lipid Metabolism-related Gene Expression of Mice on an Atherogenic Diet. J. Hepatol. 2008, 49, 1019–1028. [Google Scholar] [CrossRef]
- Meza-Torres, C.; Hernández-Camacho, J.D.; Cortés-Rodríguez, A.B.; Fang, L.; Bui Thanh, T.; Rodríguez-Bies, E.; Navas, P.; López-Lluch, G. Resveratrol Regulates the Expression of Genes Involved in CoQ Synthesis in Liver in Mice Fed with High Fat Diet. Antioxidants 2020, 9, 431. [Google Scholar] [CrossRef]
- Cho, I.J.; Ahn, J.Y.; Kim, S.; Choi, M.S.; Ha, T.Y. Resveratrol Attenuates the Expression of HMG-CoA Reductase mRNA in Hamsters. Biochem. Biophys. Res. Commun. 2008, 367, 190–194. [Google Scholar] [CrossRef]
- Rašković, A.; Ćućuz, V.; Torović, L.; Tomas, A.; Gojković-Bukarica, L.; Ćebović, T.; Milijašević, B.; Stilinović, N.; Cvejić Hogervorst, J. Resveratrol Supplementation Improves Metabolic Control in Rats with Induced Hyperlipidemia and Type 2 Diabetes. Saudi Pharm. J. 2019, 27, 1036–1043. [Google Scholar] [CrossRef] [PubMed]
- Deschênes, M.; Belle, S.H.; Krom, R.A.; Zetterman, R.K.; Lake, J.R. Early Allograft Dysfunction after Liver Transplantation: A Definition and Predictors of Outcome. National Institute of Diabetes and Digestive and Kidney Diseases Liver Transplantation Database. Transplantation 1998, 66, 302–310. [Google Scholar] [CrossRef]
- Plin, C.; Tillement, J.P.; Berdeaux, A.; Morin, D. Resveratrol Protects against Cold Ischemia-warm Reoxygenation-induced Damages to Mitochondria and Cells in Rat Liver. Eur. J. Pharmacol. 2005, 528, 162–168. [Google Scholar] [CrossRef]
- Yu, S.; Zhou, X.; Xiang, H.; Wang, S.; Cui, Z.; Zhou, J. Resveratrol Reduced Liver Damage after Liver Resection in a Rat Model by Upregulating Sirtuin 1 (SIRT1) and Inhibiting the Acetylation of High Mobility Group Box 1 (HMGB1). Med. Sci. Monit. 2019, 25, 3212–3220. [Google Scholar] [CrossRef] [PubMed]
- Gedik, E.; Girgin, S.; Ozturk, H.; Obay, B.D.; Buyukbayram, H. Resveratrol Attenuates Oxidative Stress and Histological Alterations induced by Liver Ischemia/Reperfusion in Rats. World J. Gastroenterol. 2008, 14, 7101–7106. [Google Scholar] [CrossRef]
- Hassan-Khabbar, S.; Vamy, M.; Cottart, C.H.; Wendum, D.; Vibert, F.; Savouret, J.F.; Thérond, P.; Clot, J.P.; Waligora, A.J.; Nivet-Antoine, V. Protective Effect of Post-ischemic Treatment with Trans-resveratrol on Cytokine Production and Neutrophil Recruitment by Rat Liver. Biochimie 2010, 92, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.L.; Yu, L.; Pan, C.E.; Jiao, X.Y.; Lv, Y.; Fu, J.; Meng, K.W. Apoptosis of Lymphocytes in Allograft in a Rat Liver Transplantation Model Induced by Resveratrol. Pharmacol. Res. 2006, 54, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Kirimlioglu, H.; Ecevit, A.; Yilmaz, S.; Kirimlioglu, V.; Karabulut, A.B. Effect of Resveratrol and Melatonin on Oxidative Stress Enzymes, Regeneration, and Hepatocyte Ultrastructure in Rats Subjected to 70% Partial Hepatectomy. Transplant. Proc. 2008, 40, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Velioğlu-Oğünç, A.; Sehirli, O.; Toklu, H.Z.; Ozyurt, H.; Mayadağli, A.; Ekşioğlu-Demiralp, E.; Erzik, C.; Cetinel, S.; Yeğen, B.C.; Sener, G. Resveratrol Protects against Irradiation-induced Hepatic and Ileal Damage via Its Anti-oxidative Activity. Free Radic. Res. 2009, 43, 1060–1071. [Google Scholar] [CrossRef]
- Ye, Q.; Zou, B.; Yeo, Y.H.; Li, J.; Huang, D.Q.; Wu, Y.; Yang, H.; Liu, C.; Kam, L.Y.; Tan, X.X.E.; et al. Global Prevalence, Incidence, and Outcomes of Non-obese or Lean Non-alcoholic Fatty Liver Disease: A Systematic Review and Meta-analysis. Lancet Gastroenterol. Hepatol. 2020, 5, 739–752. [Google Scholar] [CrossRef]
- Jennison, E.; Patel, J.; Scorletti, E.; Byrne, C.D. Diagnosis and Management of Non-alcoholic Fatty Liver Disease. Postgrad. Med. J. 2019, 95, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Makri, E.; Goulas, A.; Polyzos, S.A. Epidemiology, Pathogenesis, Diagnosis and Emerging Treatment of Nonalcoholic Fatty Liver Disease. Arch. Med. Res. 2020. [Google Scholar] [CrossRef]
- Wijarnpreecha, K.; Aby, E.S.; Ahmed, A.; Kim, D. Evaluation and Management of Extrahepatic Manifestations of Nonalcoholic Fatty Liver Disease. Clin. Mol. Hepatol. 2020. [Google Scholar] [CrossRef]
- Mikolasevic, I.; Filipec-Kanizaj, T.; Mijic, M.; Jakopcic, I.; Milic, S.; Hrstic, I.; Sobocan, N.; Stimac, D.; Burra, P. Nonalcoholic Fatty Liver Disease and Liver Transplantation–Where Do We Stand? World J. Gastroenterol. 2018, 24, 1491–1506. [Google Scholar] [CrossRef] [PubMed]
- Targher, G.; Byrne, C.D.; Tilg, H. NAFLD and Increased Risk of Cardiovascular Disease: Clinical Associations, Pathophysiological Mechanisms and Pharmacological Implications. Gut 2020, 69, 1691–1705. [Google Scholar] [CrossRef]
- Ismaiel, A.; Dumitraşcu, D.L. Cardiovascular Risk in Fatty Liver Disease: The Liver-Heart Axis-Literature Review. Front. Med. 2019, 6, 202. [Google Scholar] [CrossRef] [PubMed]
- Kantartzis, K.; Fritsche, L.; Bombrich, M.; Machann, J.; Schick, F.; Staiger, H.; Kunz, I.; Schoop, R.; Lehn-Stefan, A.; Heni, M.; et al. Effects of Resveratrol Supplementation on Liver Fat Content in Overweight and Insulin-resistant Subjects: A Randomized, Double-blind, Placebo-controlled Clinical Trial. Diabetes Obes. Metab. 2018, 20, 1793–1797. [Google Scholar] [CrossRef]
- Cicero, A.F.G.; Fogacci, F.; Banach, M. Botanicals and Phytochemicals Active on Cognitive Decline: The Clinical Evidence. Pharmacol. Res. 2018, 130, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.; Yu, X. Efficacy of Resveratrol Supplementation on Liver Enzymes in Patients with Non-alcoholic Fatty Liver Disease: A Systematic Review and Meta-analysis. Complement. Ther. Med. 2020, 57, 102635. [Google Scholar] [CrossRef]
- Asghari, S.; Rafraf, M.; Farzin, L.; Asghari-Jafarabadi, M.; Ghavami, S.M.; Somi, M.H. Effects of Pharmacologic Dose of Resveratrol Supplementation on Oxidative/Antioxidative Status Biomarkers in Nonalcoholic Fatty Liver Disease Patients: A Randomized, Double-Blind, Placebo-Controlled Trial. Adv. Pharm. Bull. 2018, 8, 307–317. [Google Scholar] [CrossRef]
- Rafiee, S.; Mohammadi, H.; Ghavami, A.; Sadeghi, E.; Safari, Z.; Askari, G. Efficacy of Resveratrol Supplementation in Patients with Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-analysis of Clinical Trials. Complement. Ther. Clin. Pract. 2020, 42, 101281. [Google Scholar] [CrossRef]
- Fogacci, F.; Banach, M.; Cicero, A.F.G. Resveratrol Effect on Patients with Non-alcoholic Fatty Liver Disease: A Matter of Dose and Treatment Length. Diabetes Obes. Metab. 2018, 20, 1798–1799. [Google Scholar] [CrossRef]
- Theodotou, M.; Fokianos, K.; Moniatis, D.; Kadlenic, R.; Chrysikou, A.; Aristotelous, A.; Mouzouridou, A.; Diakides, J.; Stavrou, E. Effect of Resveratrol on Non-alcoholic Fatty Liver Disease. Exp. Ther. Med. 2019, 18, 559–565. [Google Scholar] [CrossRef]
- Cuerda, C.; Luengo, L.M.; Valero, M.A.; Vidal, A.; Burgos, R.; Calvo, F.L.; Martínez, C. Antioxidants and Diabetes Mellitus: Review of the Evidence. Nutr. Hosp. 2011, 26, 68–78. [Google Scholar]
- Yılmaz, Z.; Kalaz, E.B.; Aydın, A.F.; Olgaç, V.; Doğru-Abbasoğlu, S.; Uysal, M.; Koçak-Toker, N. The Effect of Resveratrol on Glycation and Oxidation Products in Plasma and Liver of Chronic Methylglyoxal-treated Rats. Pharmacol. Rep. 2018, 70, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Bakker, G.C.; van Erk, M.J.; Pellis, L.; Wopereis, S.; Rubingh, C.M.; Cnubben, N.H.; Kooistra, T.; van Ommen, B.; Hendriks, H.F. An Antiinflammatory Dietary Mix Modulates Inflammation and Oxidative and Metabolic Stress in Overweight Men: A Nutrigenomics Approach. Am. J. Clin. Nutr. 2010, 91, 1044–1059. [Google Scholar] [CrossRef]
- Brasnyó, P.; Molnár, G.A.; Mohás, M.; Markó, L.; Laczy, B.; Cseh, J.; Mikolás, E.; Szijártó, I.A.; Mérei, A.; Halmai, R.; et al. Resveratrol Improves Insulin Sensitivity, Reduces Oxidative Stress and Activates the Akt Pathway in Type 2 Diabetic Patients. Br. J. Nutr. 2011, 106, 383–389. [Google Scholar] [CrossRef]
- Dash, S.; Xiao, C.; Morgantini, C.; Szeto, L.; Lewis, G.F. High-dose Resveratrol Treatment for 2 Weeks Inhibits Intestinal and Hepatic Lipoprotein Production in Overweight/Obese Men. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 2895–2901. [Google Scholar] [CrossRef] [PubMed]
- Timmers, S.; de Ligt, M.; Phielix, E.; van de Weijer, T.; Hansen, J.; Moonen-Kornips, E.; Schaart, G.; Kunz, I.; Hesselink, M.K.; Schrauwen-Hinderling, V.B.; et al. Resveratrol as Add-on Therapy in Subjects With Well-Controlled Type 2 Diabetes: A Randomized Controlled Trial. Diabetes Care 2016, 39, 2211–2217. [Google Scholar] [CrossRef] [PubMed]
- Knop, F.K.; Konings, E.; Timmers, S.; Schrauwen, P.; Holst, J.J.; Blaak, E.E. Thirty Days of Resveratrol Supplementation Does not Affect Postprandial Incretin Hormone Responses, but Suppresses Postprandial Glucagon in Obese Subjects. Diabet. Med. 2013, 30, 1214–1218. [Google Scholar] [CrossRef] [PubMed]
- Movahed, A.; Raj, P.; Nabipour, I.; Mahmoodi, M.; Ostovar, A.; Kalantarhormozi, M.; Netticadan, T. Efficacy and Safety of Resveratrol in Type 1 Diabetes Patients: A Two-Month Preliminary Exploratory Trial. Nutrients 2020, 12, 161. [Google Scholar] [CrossRef]
- Hosseini, H.; Koushki, M.; Khodabandehloo, H.; Fathi, M.; Panahi, G.; Teimouri, M.; Majidi, Z.; Meshkani, R. The Effect of Resveratrol Supplementation on C-reactive Protein (CRP) in Type 2 Diabetic Patients: Results from a Systematic Review and Meta-analysis of Randomized Controlled Trials. Complement. Ther. Med. 2020, 49, 102251. [Google Scholar] [CrossRef]
- Zhang, B.; Yin, X.; Sui, S. Resveratrol Inhibited the Progression of Human Hepatocellular Carcinoma by Inducing Autophagy via Regulating p53 and the Phosphoinositide 3-kinase/protein Kinase B Pathway. Oncol. Rep. 2018, 40, 2758–2765. [Google Scholar] [CrossRef]
- Grifantini, K. Understanding Pathways of Calorie Restriction: A Way to Prevent Cancer? J. Natl. Cancer. Inst. 2008, 100, 619–621. [Google Scholar] [CrossRef]
- Goldberg, D.M.; Yan, J.; Soleas, G.J. Absorption of Three Wine-related Polyphenols in Three Different Matrices by Healthy Subjects. Clin. Biochem. 2003, 36, 79–87. [Google Scholar] [CrossRef]
- Howells, L.M.; Berry, D.P.; Elliott, P.J.; Jacobson, E.W.; Hoffmann, E.; Hegarty, B.; Brown, K.; Steward, W.P.; Gescher, A.J. Phase I Randomized, Double-blind Pilot Study of Micronized Resveratrol (SRT501) in Patients with Hepatic Metastases-safety, Pharmacokinetics, and Pharmacodynamics. Cancer Prev. Res. 2011, 4, 1419–1425. [Google Scholar] [CrossRef]
- Timmers, S.; Konings, E.; Bilet, L.; Houtkooper, R.H.; van de Weijer, T.; Goossens, G.H.; Hoeks, J.; van der Krieken, S.; Ryu, D.; Kersten, S.; et al. Calorie Restriction-like Effects of 30 Days of Resveratrol Supplementation on Energy Metabolism and Metabolic Profile in Obese Humans. Cell Metab. 2011, 14, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Most, J.; Timmers, S.; Warnke, I.; Jocken, J.W.; van Boekschoten, M.; de Groot, P.; Bendik, I.; Schrauwen, P.; Goossens, G.H.; Blaak, E.E. Combined Epigallocatechin-3-gallate and Resveratrol Supplementation for 12 wk Increases Mitochondrial Capacity and Fat Oxidation, but not Insulin Sensitivity, in Obese Humans: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2016, 104, 215–227. [Google Scholar] [CrossRef]
- Akbari, M.; Tamtaji, O.R.; Lankarani, K.B.; Tabrizi, R.; Dadgostar, E.; Haghighat, N.; Kolahdooz, F.; Ghaderi, A.; Mansournia, M.A.; Asemi, Z. The Effects of Resveratrol on Lipid Profiles and Liver Enzymes in Patients with Metabolic Syndrome and Related Disorders: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Lipids Health Dis. 2020, 19, 25. [Google Scholar] [CrossRef] [PubMed]
- Gualdoni, G.A.; Kovarik, J.J.; Hofer, J.; Dose, F.; Pignitter, M.; Doberer, D.; Steinberger, P.; Somoza, V.; Wolzt, M.; Zlabinger, G.J. Resveratrol Enhances TNF-α Production in Human Monocytes upon Bacterial Stimulation. Biochim. Biophys. Acta 2014, 1840, 95–105. [Google Scholar] [CrossRef]
- Espinoza, J.L.; Trung, L.Q.; Inaoka, P.T.; Yamada, K.; An, D.T.; Mizuno, S.; Nakao, S.; Takami, A. The Repeated Administration of Resveratrol Has Measurable Effects on Circulating T-Cell Subsets in Humans. Oxid. Med. Cell. Longev. 2017, 2017, 6781872. [Google Scholar] [CrossRef] [PubMed]
- Evans, H.M.; Howe, P.R.; Wong, R.H. Effects of Resveratrol on Cognitive Performance, Mood and Cerebrovascular Function in Post-Menopausal Women; A 14-Week Randomised Placebo-Controlled Intervention Trial. Nutrients 2017, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.T.; Sun, X.Y.; Lin, A.X. Supplementation with High-dose Trans-resveratrol Improves Ultrafiltration in Peritoneal Dialysis Patients: A Prospective, Randomized, Double-blind Study. Ren. Fail. 2016, 38, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Rotches-Ribalta, M.; Andres-Lacueva, C.; Estruch, R.; Escribano, E.; Urpi-Sarda, M. Pharmacokinetics of Resveratrol Metabolic Profile in Healthy Humans after Moderate Consumption of Red Wine and Grape Extract Tablets. Pharmacol. Res. 2012, 66, 375–382. [Google Scholar] [CrossRef]
- Almeida, L.; Vaz-da-Silva, M.; Falcão, A.; Soares, E.; Costa, R.; Loureiro, A.I.; Fernandes-Lopes, C.; Rocha, J.F.; Nunes, T.; Wright, L.; et al. Pharmacokinetic and Safety Profile of Trans-resveratrol in a Rising Multiple-dose Study in Healthy Volunteers. Mol. Nutr. Food Res. 2009, 53, S7–S15. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Castro, L.A.; Schiborr, C.; David, F.; Ehrt, H.; Voggel, J.; Sus, N.; Behnam, D.; Bosy-Westphal, A.; Frank, J. The Oral Bioavailability of Trans-Resveratrol from a Grapevine-Shoot Extract in Healthy Humans is Significantly Increased by Micellar Solubilization. Mol. Nutr. Food Res. 2018, 62, e1701057. [Google Scholar] [CrossRef]
- Azachi, M.; Yatuv, R.; Katz, A.; Hagay, Y.; Danon, A. A Novel Red Grape Cells Complex: Health Effects and Bioavailability of Natural Resveratrol. Int. J. Food. Sci. Nutr. 2014, 65, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Vaz-da-Silva, M.; Loureiro, A.I.; Falcao, A.; Nunes, T.; Rocha, J.F.; Fernandes-Lopes, C.; Soares, E.; Wright, L.; Almeida, L.; Soares-da-Silva, P. Effect of Food on the Pharmacokinetic Profile of Trans-resveratrol. Int. J. Clin. Pharmacol. Ther. 2008, 46, 564–570. [Google Scholar] [CrossRef] [PubMed]
| Improvement | Model | Dosage | Mechanism | Result | Reference |
|---|---|---|---|---|---|
| Steatosis | Rats | 10 mg | Increase in SOD (superoxide dismutase), GPx (glutathione peroxidase), CAT (catalase) and a reduction in NOS (nitric oxide synthase) activity | Reduction in fatty acid deposition in liver | [23] |
| [16]. 30 mg/kg [17]. 200 mg/kg | Activation of the AMPK/SIRT1 (AMP activated protein kinase/sirtuin 1) axis | [16,17] | |||
| Oxidative stress and inflammation | [36]. 500 mg od for six months | AMPK/SIRT1/Nrf2, ERK/p38, MAPK and PTEN/Akt signaling pathways, inducing autophagy through an mTOR-dependent or TFEB-dependent pathway | Synthesis of antioxidant molecules and the expression of related genes involved in the biogenesis of mitochondrial energy | [36,37] | |
| [43]. 10 to 1000 µM/L | Inhibition of the Nrf2 ubiquitination; promotion of the transcriptional functions of FoxOs | Induction of the transcription of antioxidant genes (CAT, SOD) | [41,42,43] | ||
| Liver fibrosis | Rats | [47]. 10 to 20 mg/kg od [50]. 25 to 150 µM/L od | Reduction in MDA (malondialdehyde) levels and increase in GPx and SOD levels, as well as the inhibition of mRNA expression of inflammatory mediators, including inducible NO, TNF-α (tumor necrosis factor-α), and IL-1β (interleukin-1β) | Reduction in portal pressure | [47,50,51] |
| [52]. 20 mg/kg od for 3 weeks [54]. 20 mg/kg 3 days per week | Reduction in MDA levels and increase in GPx and SOD levels; inhibition of mRNA expression of inflammatory mediators (iNOS, TNF-α, IL-1β) | Reducing the liver tissue infiltration of inflammatory cells and fibrosis deposition | [52,53,54] | ||
| Cholestatic liver damage | Rat model of bile duct ligation | Reduction in TNF-α and IL-6 mRNA levels and in the number of CD68 (+) Kupffer cells recruited in the liver | Reduction in cholestatic damage | [55] | |
| Reduction in TIMP-1 and collagen Iα1 mRNA expression; increase of Ki67-positive hepatocytes | Reduction in fibrotic tissue deposition | [55] | |||
| Hepatocellular carcinoma and metastasis | [70]. Increasing doses of RSV, ranging from 4 to 32 µM/L [75]. 40 µM/L | Regulation of Fas and FasL levels; inhibition of the PI3K/Akt/mTOR pathway; inhibition of NF-κB | Induction of apoptosis | [70,71,72,77] [75,76,78] [79,80] | |
| Animal models exposed to carcinogenic chemicals (DENA) | [86]. 60 mg/kg od [88]. 50 mg/kg | Reduction in DENA-induced lipid peroxidation, iNOS; increase in protein carbonyl formation, Nrf2; reduction in the expression of hepatic TNF-α, IL-1β, and IL-6 | Restoring of cellular antioxidant defenses Direct anti-inflammatory effect | [86,87,88] | |
| 500 mg | Blocking of VEGFR expression through HIF-1a downregulation | Antiangiogenetic effect | [89] | ||
| RSV dissolved in DMSO at a concentration of 25 mM | Reduction in cyclin D1, p38 MAP kinase, Akt, and Pak1 expression | Reduction in cellular proliferation | [76] | ||
| Hepatic glucose metabolism and diabetes | [98]. 6 mg od [99]. 5 mg/kg twice weekly for 30 days [100]. 10 mg/kg od | Decreased activity of lactate dehydrogenase, glucose-6-phosphatase, glycogen phosphorylase, and reduction in phosphoenolpyruvate carboxykinase protein levels; increases in hexokinase and pyruvate kinase activity, glycogen synthase. | Increased insulin metabolism | [97,98,99,100] | |
| Chemical liver injury | Carbon tetrachloride-induced hepatotoxicity | [105]. 25/50/75/100 µM/L | Prevention of the increase in lipid peroxidation and γ-glutamyl transpeptidase activity | Antioxidant and antiapoptotic effect | [103,104,105,106] |
| Improvement | Dosage | Patients | Result | Reference |
|---|---|---|---|---|
| NAFLD | 150 mg | Overweight or obese insulin-resistant patients with NAFLD | No effect on hepatic fat content | [165] |
| 50 mg Group 1 200 mg Group 2 | 44 patients, aged 29–70 years (n = 22 per group) | Reduction in the liver fat | [171] | |
| Diabetes Mellitus | 1 g, 1.5 g, or 2 g daily for 4 weeks | 10 overweight subjects with impaired glucose tolerance | Improvement in insulin sensitivity and postprandial glucose levels | [175] |
| 150 mg/day for 30 days | 17 volunteers with T2D (type 2 diabetes) | Reduction in intrahepatic lipid content and systolic blood pressure | [176,177] | |
| 150 mg/day for 30 days | Evaluation of postprandial plasma responses of the incretin hormones and glucagon in 10 obese men | Suppression of postprandial glucagon | [178] | |
| 500 mg capsules, twice daily for 60 days | 13 patients with T1D (type 1 diabetes) | Reduction in HbA1c (glycosylated hemoglobin), FBS (fasting blood sugar) and oxidative stress markers | [179] | |
| Cancer | 0.5, 1.0, 2.5, or 5.0 g per day | 40 healthy volunteers | Anticarcinogenica and caloric restriction mimetic effect by reducing IGF-1 and IGFBP-3 | [182] |
| Micronized RSV, 5 g daily for 14 days | Patients with colorectal cancer and hepatic metastases scheduled to undergo hepatectomy | Increase in cleaved caspase-3, a marker of apoptosis | [184] | |
| Obesity | 150 mg/day for 30 days | 11 obese men in a randomized double-blind crossover study | In muscle: activation of AMPK, increased levels of SIRT1 and peroxisome activity. Increase in citrate synthase activity and decrease in lipid content within the liver, circulating glucose levels, triglycerides, alanine aminotransferase, and other inflammation markers | [185] |
| EGCG (epigallocatechin-3-gallate) + RSV (282 and 80 mg/d, respectively) or placebo for 12 wk. | randomized double-blind study, 38 overweight and obese subjects | Increase in mitochondrial capacity and stimulated fat oxidation, without leading to increased tissue-specific insulin sensitivity | [186] | |
| Health condition associated with oxidative stress and inflammation | 5 g, single dose | Plasma cytokine levels were measured over 48 h after oral administration in 10 healthy subjects | Increased production of TNF-α; enhanced NF-κB activation | [188] |
| 1000 mg/day for 28 days | Repeated doses of resveratrol on circulating immune cells in healthy individuals | Increase in circulating γδ T cells and regulatory T cells Decrease in plasma levels of the proinflammatory cytokines TNF-α and MCP-1 | [189] | |
| 150 mg or 450 mg daily | 72 patients undergoing peritoneal dialysis randomly assigned to 12 week treatment of low-dose or high-dose trans-resveratrol or a placebo | Improvement in mean net UF volume and UF rate through a reduction in VEGF, Flk-1 (fetal liver kinase-1) and Ang-2 (angiopoietin) levels | [191] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Izzo, C.; Annunziata, M.; Melara, G.; Sciorio, R.; Dallio, M.; Masarone, M.; Federico, A.; Persico, M. The Role of Resveratrol in Liver Disease: A Comprehensive Review from In Vitro to Clinical Trials. Nutrients 2021, 13, 933. https://doi.org/10.3390/nu13030933
Izzo C, Annunziata M, Melara G, Sciorio R, Dallio M, Masarone M, Federico A, Persico M. The Role of Resveratrol in Liver Disease: A Comprehensive Review from In Vitro to Clinical Trials. Nutrients. 2021; 13(3):933. https://doi.org/10.3390/nu13030933
Chicago/Turabian StyleIzzo, Carmine, Monica Annunziata, Giuseppe Melara, Roberta Sciorio, Marcello Dallio, Mario Masarone, Alessandro Federico, and Marcello Persico. 2021. "The Role of Resveratrol in Liver Disease: A Comprehensive Review from In Vitro to Clinical Trials" Nutrients 13, no. 3: 933. https://doi.org/10.3390/nu13030933
APA StyleIzzo, C., Annunziata, M., Melara, G., Sciorio, R., Dallio, M., Masarone, M., Federico, A., & Persico, M. (2021). The Role of Resveratrol in Liver Disease: A Comprehensive Review from In Vitro to Clinical Trials. Nutrients, 13(3), 933. https://doi.org/10.3390/nu13030933









