Association between Chinese Dietary Guidelines Compliance Index for Pregnant Women and Risks of Pregnancy Complications in the Tongji Maternal and Child Health Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Development of CDGCI-PW
2.1.1. Components of CDGCI-PW
2.1.2. Scoring Criteria for CDGCI-PW
2.2. Study Population
2.3. Processes of Data Acquisition
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Food Intakes according to CDGCI-PW Scores
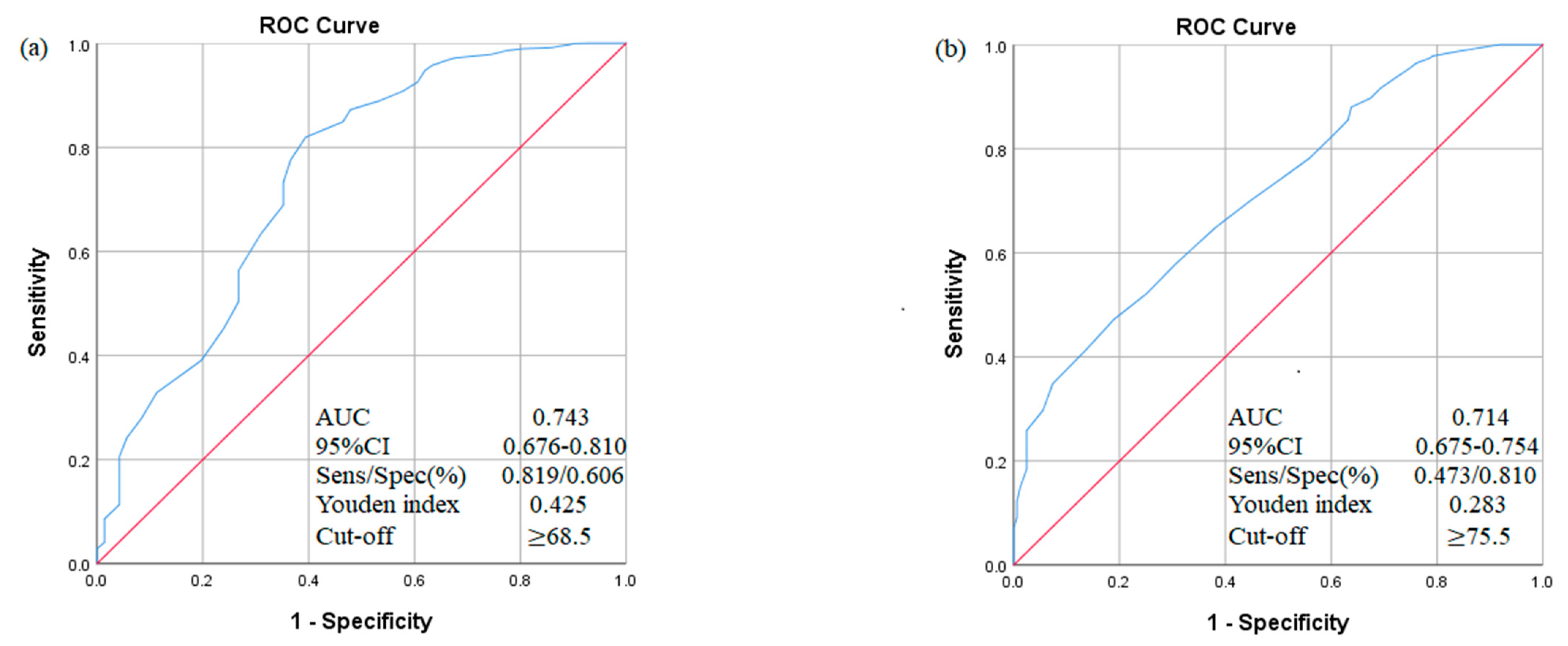
3.3. Associations between CDGCI-PW Scores and Risks of Pregnancy Complications
3.4. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chinese Nutrition Society. Chinese Dietary Guidelines; People’s Medical Publishing House Press: Beijing, China, 2016. [Google Scholar]
- Blumfield, M.L.; Hure, A.J.; MacDonald-Wicks, L.K.; Smith, R.; Simpson, S.J.; Giles, W.B.; Raubenheimer, D.; Collins, C.E. Dietary balance during pregnancy is associated with fetal adiposity and fat distribution. Am. J. Clin. Nutr. 2012, 96, 1032–1041. [Google Scholar] [CrossRef]
- Sharma, S. Development and use of FFQ among adults in diverse settings across the globe. Proc. Nutr. Soc. 2011, 70, 232–251. [Google Scholar] [CrossRef]
- Willett, W.C. Nutritional Epidemiology, 3rd ed.; Oxford University Press: New York, NY, USA, 2012. [Google Scholar]
- National Bureau of Statistics of China. Projected Data from the Annual Population Sample Survey. Available online: http://data.stats.gov.cn/easyquery.htm?cn=C01 (accessed on 31 December 2019).
- Gao, Y.; Zhou, H.; Singh, N.S.; Powell-Jackson, T.; Nash, S.; Yang, M.; Guo, S.; Fang, H.; Alvarez, M.M. Progress and challenges in maternal health in western China: A Countdown to 2015 national case study. Lancet Glob. Health 2017, 5, e523–e536. [Google Scholar] [CrossRef]
- Na, R.; Li, D.; Mi, L.; Liang, H. Prevalence rate of gestational diabetes mellitus in China: A meta-analysis. Chinese. J. Evid. Based Med. 2018, 18, 280–285. [Google Scholar]
- Li, L.; Fu, Q. Prevalence rate of gestational hypertension in China: A meta-analysis. Matern. Child Health Care China 2019, 34, 3378–3381. [Google Scholar]
- Chen, Y.; Yin, Z.; Xie, Q. Suggestions to ameliorate the inequity in urban/rural allocation of healthcare resources in China. Int. J. Equity Health 2014, 13, 34. [Google Scholar] [CrossRef]
- Yang, L.; Hong, M.; Wang, H. Primary health care among rural pregnant women in China: Achievements and challenges in maternal mortality ratio. Prim. Health Care Res. Dev. 2019, 20, e97. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.; Xi, J.; Luo, R.; Mu, T.; Xiang, M.; Wand, C.; Pan, X. The situation of human resources in the county level maternal and children health care institutes. Chin. J. Women Child. Health 2010, 11, 130–133. [Google Scholar]
- Cheng, X.; Yang, G.; Fang, C.; Gong, C. Analysis on the current situation of pregnancy nutrition clinic in Maternal and child health care institutions in Hunan province. Chin. J. Women Child. Health 2020, 11, 47–50, 55. [Google Scholar]
- Wu, T.; Liang, J.; Wu, J.; Liu, W.; Zhao, Y. A Descriptive systematic review of the development of community nutrition education in China. Health Ed. Health Prom. 2020, 15, 127–132. [Google Scholar]
- Guenther, P.M.; Casavale, K.O.; Reedy, J.; Kirkpatrick, S.I.; Hiza, H.A.; Kuczynski, K.J.; Kahle, L.L.; Krebs-Smith, S.M. Update of the Healthy Eating Index: HEI-2010. J. Acad. Nutr. Diet 2013, 113, 569–580. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- Haines, P.S.; Siega-Riz, A.M.; Popkin, B.M. The Diet Quality Index Revised. J. Am. Diet. Assoc. 1999, 99, 697–704. [Google Scholar] [CrossRef]
- Kennedy, E.T.; Ohls, J.; Carlson, S.; Fleming, K. The Healthy Eating Index: Design and applications. J. Am. Diet. Assoc. 1995, 95, 1103–1108. [Google Scholar] [CrossRef]
- Schap, T.; Kuczynski, K.; Hiza, H. Healthy Eating Index-Beyond the Score. J. Acad. Nutr. Diet 2017, 117, 519–521. [Google Scholar] [CrossRef]
- Guenther, P.M.; Reedy, J.; Krebs-Smith, S.M. Development of the Healthy Eating Index-2005. J. Am. Diet. Assoc. 2008, 108, 1896–1901. [Google Scholar] [CrossRef] [PubMed]
- Patterson, R.E.; Haines, P.S.; Popkin, B.M. Diet quality index: Capturing a multidimensional behavior. J. Am. Diet. Assoc. 1994, 94, 57–64. [Google Scholar] [CrossRef]
- Zhang, R.; Wang, Z.; Fei, Y.; Zhou, B.; Zheng, S.; Wang, L.; Huang, L.; Jiang, S.; Liu, Z.; Jiang, J.; et al. The Difference in nutrient intakes between Chinese and Mediterranean, Japanese and American Diets. Nutrients 2015, 7, 4661–4688. [Google Scholar] [CrossRef]
- Colon-Ramos, U.; Racette, S.B.; Ganiban, J.; Nguyen, T.G.; Kocak, M.; Carroll, K.N.; Volgyi, E.; Tylavsky, F.A. Association between dietary patterns during pregnancy and birth size measures in a diverse population in southern US. Nutrients 2015, 7, 1318–1332. [Google Scholar] [CrossRef]
- He, Y.; Zhai, F.; Yang, X.; Ge, K. The Chinese diet balance index revised. Acta Nutr. Sin. 2009, 31, 532–536. [Google Scholar]
- He, Y.; Zhai, F.; Ge, K. Approaching Chinese diet balance index. J. Hyg. Res. 2005, 34, 208–211. [Google Scholar]
- Wang, Y.; Li, R.; Liu, D.; Dai, Z.; Liu, J.; Zhang, J.; Zhou, R.; Zeng, G. Evaluation of the dietary quality by Diet Balance Index for pregnancy among pregnant women. J. Hyg. Res. 2016, 45, 211–216. [Google Scholar]
- Li, S.; Lei, F.; Zhang, R.; Liu, D.; Qu, P.; Cheng, Y.; Liu, X.; Chen, F.; Dang, S.; Yan, H. Socioeconomic disparity in the diet quality of pregnant women in Northwest China. Asia Pac. J. Clin. Nutr. 2019, 28, 330–340. [Google Scholar]
- Shao, Y.; Bai, Y.; Lin, R.; He, W.; Fu, W. Dietary patterns among pregnant woman in Lanzhou. Chin. J. Women Child. Health 2020, 11, 56–60+64. [Google Scholar]
- Yang, Y.; Wang, G.; Pan, X. China Food Composition Tables; Peking University Medical Press: Beijing, China, 2019. [Google Scholar]
- Zhou, X.; Chen, R.; Zhong, C.; Wu, J.; Li, X.; Li, Q.; Cui, W.; Yi, N.; Xiao, M.; Yin, H.; et al. Maternal dietary pattern characterised by high protein and low carbohydrate intake in pregnancy is associated with a higher risk of gestational diabetes mellitus in Chinese women: A prospective cohort study. Br. J. Nutr. 2018, 120, 1045–1055. [Google Scholar] [CrossRef]
- Zhang, H.; Qiu, X.; Zhong, C.; Zhang, K.; Xiao, M.; Yi, N.; Xiong, G.; Wang, J.; Yao, J.; Hao, L.; et al. Reproducibility and relative validity of a semi-quantitative food frequency questionnaire for Chinese pregnant women. Nutr. J. 2015, 14, 56. [Google Scholar] [CrossRef]
- Ding, Y.; Yang, Y.; Li, F.; Shao, Y.; Sun, Z.; Zhong, C.; Fan, P.; Li, Z.; Zhang, M.; Li, X.; et al. Development and validation of a photographic atlas of food portions for accurate quantification of dietary intakes in China. J. Hum. Nutr. Diet. 2021. (Online ahead of print). [Google Scholar] [CrossRef] [PubMed]
- Cunningham, F.G.; Leveno, K.J.; Bloom, S.L.; Hauth, J.C.; Rouse, D.J.; Spong, C.Y. Pregnancy hypertension. In Williams Obstetrics, 23rd ed.; McGraw Hill: New York, NY, USA, 2009. [Google Scholar]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1988, 240, 1285–1293. [Google Scholar] [CrossRef]
- Wu, W.; Wang, Y.; Zhang, L. Analysis of dietary intake in 333 pregnant women of the second trimester in Xigu of LanZhou. Mod. Prev. Med. 2010, 37, 1438–1440. [Google Scholar]
- Han, Y.; Li, L.; Shu, L.; Yu, T.; Bo, Q.; Hu, A. Evaluation on the dietary quality of pregnant women with an adjusted dietary balance index. J. Hyg. Res. 2011, 40, 454–456. [Google Scholar]
- Schoenaker, D.A.; Soedamah-Muthu, S.S.; Mishra, G.D. The association between dietary factors and gestational hypertension and pre-eclampsia: A systematic review and meta-analysis of observational studies. BMC Med 2014, 12, 157. [Google Scholar] [CrossRef] [PubMed]
- Timmermans, S.; Steegers-Theunissen, R.P.; Vujkovic, M.; Bakker, R.; den Breeijen, H.; Raat, H.; Russcher, H.; Lindemans, J.; Hofman, A.; Jaddoe, V.W.; et al. Major dietary patterns and blood pressure patterns during pregnancy: The Generation R Study. Am. J. Obs. Gynecol. 2011, 205, e1–e12. [Google Scholar] [CrossRef] [PubMed]
- Bowers, K.; Tobias, D.K.; Yeung, E.; Hu, F.B.; Zhang, C. A prospective study of prepregnancy dietary fat intake and risk of gestational diabetes. Am. J. Clin. Nutr. 2012, 95, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Alwan, N.A.; West, J.; Brown, S.; McKinlay, C.J.; Farrar, D.; Crowther, C.A. Lifestyle interventions for the treatment of women with gestational diabetes. Cochrane Database Syst. Rev. 2017, 5, CD011970. [Google Scholar] [CrossRef]
- Tieu, J.; Shepherd, E.; Middleton, P.; Crowther, C.A. Dietary advice interventions in pregnancy for preventing gestational diabetes mellitus. Cochrane Database Syst. Rev. 2017, 1, CD006674. [Google Scholar] [CrossRef]
- Mijatovic-Vukas, J.; Capling, L.; Cheng, S.; Stamatakis, E.; Louie, J.; Cheung, N.W.; Markovic, T.; Ross, G.; Senior, A.; Brand-Miller, J.C.; et al. Associations of diet and physical activity with risk for gestational diabetes mellitus: A systematic review and meta-analysis. Nutrients 2018, 10, 698. [Google Scholar] [CrossRef]
- Paknahad, Z.; Fallah, A.; Moravejolahkami, A.R. Maternal dietary patterns and their association with pregnancy outcomes. Clin. Nutr. Res. 2019, 8, 64–73. [Google Scholar] [CrossRef]
- Kazemian, E.; Dorosty-Motlagh, A.R.; Sotoudeh, G.; Eshraghian, M.R.; Ansary, S.; Omidian, M. Nutritional status of women with gestational hypertension compared with normal pregnant women. Hypertens Pregnancy 2013, 32, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Yee, L.M.; Silver, R.M.; Haas, D.M.; Parry, S.; Mercer, B.M.; Iams, J.; Wing, D.; Parker, C.B.; Reddy, U.M.; Wapner, R.J.; et al. Quality of periconceptional dietary intake and maternal and neonatal outcomes. Am. J. Obs. Gynecol. 2020, 223, 121.e1–121.e8. [Google Scholar] [CrossRef]
- Timmermans, S.; Steegers-Theunissen, R.P.; Vujkovic, M.; den Breeijen, H.; Russcher, H.; Lindemans, J.; Mackenbach, J.; Hofman, A.; Lesaffre, E.E.; Jaddoe, V.V.; et al. The Mediterranean diet and fetal size parameters: The Generation R Study. Br. J. Nutr. 2012, 108, 1399–1409. [Google Scholar] [CrossRef]
- Hillesund, E.R.; Bere, E.; Haugen, M.; Overby, N.C. Development of a New Nordic Diet score and its association with gestational weight gain and fetal growth—A study performed in the Norwegian Mother and Child Cohort Study (MoBa). Public Health Nutr. 2014, 17, 1909–1918. [Google Scholar] [CrossRef]
- Okubo, H.; Miyake, Y.; Sasaki, S.; Tanaka, K.; Murakami, K.; Hirota, Y.; Osaka, M.; Child Health Study, G.; Kanzaki, H.; Kitada, M.; et al. Maternal dietary patterns in pregnancy and fetal growth in Japan: The Osaka Maternal and Child Health Study. Br. J. Nutr. 2012, 107, 1526–1533. [Google Scholar] [CrossRef]

| Key Recommendation | Components of CDGCI-PW |
|---|---|
| (1) Eat a variety of foods, mainly cereals and their products (a balanced diet includes 11 categories of foods per week and 12 kinds of foods per day. Whole grains and beans other than soybeans should form no less than one-third of the total intake of staple food). | 1. How many categories of food do you eat per week on average? |
| 2. How many kinds of foods do you eat per day on average? | |
| 3. Can whole grains and beans other than soybeans account for more than one-third of your staple food intake? | |
| (2) Eat a balanced diet with no less than 130 g of carbohydrates per day. | 4. Does your daily intake of staple food reach 200 g on average? |
| (3) Ensure adequate intake of vegetables, milk and its products, soybeans and its products, and nuts. Among them, the intake of green leafy and colored vegetables (red and yellow) should reach 200 g per day. | 5. Do you eat more than 200 g of green leafy and colored vegetables (red and yellow) per day on average (raw weight)? |
| 6. How often do you drink milk and its products per week on average? Dairy intake is considered to be significant when servings are equivalent to 250 mL of fresh liquid milk each time. | |
| 7. How often do you eat soybeans and soybean products per week on average? The intake of soybeans products is considered to be significant when servings are the equivalent of up to 15 g of dry soybeans each time. | |
| 8. How often do you eat nuts per week on average? Nuts intake is considered to be significant when servings are the equivalent of up to 10 g of dry nuts each time. | |
| (4) Eat appropriate amounts of lean meat (livestock and poultry meat), aquatic products (fish, shrimp, and shellfish), and eggs. Eat iron-rich foods such as animal blood or liver once or twice a week. | 9. Do you eat 125 g of lean meat (livestock and poultry meat), aquatic products (fish, shrimp, and shellfish), or eggs per day on average? |
| 10. How often do you eat animal blood and liver per week on average? The intake of animal blood and liver is considered to be significant when it is reach to 20 to 50 g each time. | |
| (5) Eat iodized table salt and iodine-rich seafood. | 11. Do you eat iodized table salt every day? |
| 12. How often do you eat iodine-rich seafood per week on average? This includes kelp, nori, undaria pinnatifida, shellfish, sea fish, etc. | |
| (6) Develop healthy eating habits | 13. Do you often eat foods high in oil, salt, and sugar? |
| Components | Scoring Criterion | Range of Score |
|---|---|---|
| 1. How many categories of food do you eat per week on average? | A. Less than or equal to 6 categories | 0 points |
| B. Range from 7 to 10 categories | 5 to 20 points (5 points for each additional category) | |
| C. More than or equal to 11 categories | 25 points | |
| 2. How many types of foods do you eat per day on average? | A. Less than or equal to 4 kinds | 0 points |
| B. Range from 5 to 11 kinds | 1 to 7 points (1 point for each additional kind) | |
| C. Range from 11 to 20 kinds | 7 to 25 points (2 points for each additional kind) | |
| D. More than or equal to 20 kinds | 25 points | |
| 3. Can whole grains and beans other than soybeans account for more than one-third of your staple food intake? | A. No | 0 points |
| B. Yes | 4 points | |
| 4. Does your daily intake of staple food reach 200 g on average? | A. No | 0 points |
| B. Yes | 4 points | |
| 5. Do you eat more than 200 g of green leafy and colored vegetables (red and yellow) per day on average? (raw weight) | A. No | 0 points |
| B. Yes | 5 points | |
| 6. How often do you drink milk and its products per week on average? Dairy intake is considered to be significant when servings are equivalent to 250 mL of fresh liquid milk each time. | A. Less than or equal to once a week | 0 points |
| B. Range from 2 to 4 times per week | 1 to 3 points (1 point for each additional time per week) | |
| C. More than or equal to 5 times per week | 4 points | |
| 7. How often do you eat soybeans and soybean products per week on average? The intake of soybeans products is considered to be significant when servings are the equivalent of up to 15 g of dry soybeans each time. | A. Less than or equal to once a week | 0 points |
| B. Range from 2 to 4 times per week | 1 to 3 points (1 point for each additional time per week) | |
| C. More than or equal to 5 times per week | 4 points | |
| 8. How often do you eat nuts per week on average? Nuts intake is considered to be significant when servings are the equivalent of up to 10 g of dry nuts each time. | A. Less than or equal to once a week | 0 points |
| B. Range from 2 to 4 times per week | 1 to 3 points (1 point for each additional time per week) | |
| C. More than or equal to 5 times per week | 4 points | |
| 9. Do you eat 125 g of lean meat (livestock and poultry meat), aquatic products (fish, shrimp, and shellfish), or eggs per day on average? | A. No | 0 points |
| B. Yes | 5 points | |
| 10. How often do you eat animal blood and liver per week on average? The intake of animal blood and liver is considered to be significant when it reaches 20 to 50 g each serving. | A. Never | 0 points |
| B. 1 time per week | 3 points | |
| C. More than or equal to 2 times per week | 5 points | |
| 11. Do you eat iodized table salt every day? | A. No | 0 points |
| B. Yes | 4 points | |
| 12. How often do you eat iodine-rich seafood per week on average? This includes kelp, nori, undaria pinnatifida, shellfish, sea fish, etc. | A. Never | 0 points |
| B. Range from 1 to 4 times per week | 1 to 4 points (1 point for each additional time per week) | |
| C. More than or equal to 5 times per week | 5 points | |
| 13. Do you often eat foods high in oil, salt and sugar? | A. Yes | 0 points |
| B. No | 6 points |
| Characteristics | Value | p-Value | |||
|---|---|---|---|---|---|
| First Quartile (n = 425) | Second Quartile (n = 331) | Third Quartile (n = 386) | Fourth Quartile (n = 347) | ||
| CDGCI-PW score 2 | 66.0 (63.0, 69.0) | 72.0 (71.0, 74.0) | 77.0 (76.0, 78.0) | 83.0 (81.0, 86.0) | |
| Age, y | 28.3 ± 3.5 | 28.2 ± 3.3 | 28.4 ± 3.6 | 28.6 ± 3.5 | 0.41 |
| Pre-pregnancy BMI, kg/m2 | 21.1 ± 2.9 | 21.1 ± 2.8 | 20.9 ± 2.8 | 20.7 ± 2.5 | 0.12 |
| Height, cm | 159.6 ± 5.1 | 159.8 ± 4.5 | 160.7 ± 4.7 | 160.9 ± 5.4 | <0.01 |
| Weight gain in the second trimester, kg | 7.9 ± 3.6 | 8.6 ± 3.5 | 8.4 ± 3.5 | 8.4 ± 3.5 | 0.07 |
| Weight gain throughout pregnancy, kg | 15.5 ± 4.4 | 16.6 ± 4.7 | 16.1 ± 4.5 | 16.2 ± 4.7 | 0.17 |
| Educational level, % | <0.01 | ||||
| ≤9 | 4.2 | 2.4 | 2.3 | 1.4 | |
| 10–12 | 14.1 | 10.6 | 8.7 | 7.8 | |
| 13–15 | 31.1 | 58.5 | 27.0 | 23.1 | |
| ≥16 | 50.6 | 28.5 | 62.0 | 67.7 | |
| Household income, % (Yuan/month, 1¥ = 0.15$) | <0.01 | ||||
| ≤1000 | 1.2 | 0 | 0.8 | 0.2 | |
| 1001–2999 | 10.4 | 6.3 | 5.2 | 5.2 | |
| 3000–4999 | 39.5 | 38.7 | 30.8 | 26.8 | |
| 5000–9999 | 36.2 | 41.7 | 47.4 | 45.0 | |
| ≥10,000 | 12.7 | 13.3 | 15.8 | 22.8 | |
| Primiparous, % | 16.5 | 13.3 | 15.5 | 13.8 | 0.59 |
| Food Categories | First Quartile (n = 425) | Second Quartile (n = 331) | Third Quartile (n = 386) | Fourth Quartile (n = 347) | Rec 5 (g/d) | p- Trend | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Below Rec 2 | Within Rec 3 | Above Rec4 | Below Rec 2 | Within Rec 3 | Above Rec 4 | Below Rec 2 | Within Rec 3 | Above Rec 4 | Below Rec 2 | Within Rec 3 | Above Rec 4 | |||
| Cereals and their products, potatoes and beans other than soybeans | 334 (78.6) | 50 (11.8) | 41 (9.6) | 236 (71.3) | 58 (17.5) | 37 (11.2) | 253 (65.5) | 62 (16.1) | 71 (18.4) | 203 (58.5) | 72 (20.7) | 72 (20.7) | 275–325 | <0.01 |
| Vegetables | 231 (54.4) | 144 (33.9) | 50 (11.8) | 155 (46.8) | 107 (32.3) | 69 (20.8) | 135 (35.0) | 153 (39.6) | 98 (25.4) | 89 (25.6) | 134 (38.6) | 124 (35.7) | 300–500 | <0.01 |
| Fruits | 80 (18.8) | 183 (43.1) | 162 (38.1) | 54 (16.4) | 139 (42.0) | 136 (41.4) | 41 (10.6) | 161 (41.7) | 184 (47.7) | 29 (8.4) | 135 (38.9) | 183 (52.7) | 200–400 | <0.01 |
| Aquatic products | 357 (84.0) | 47 (11.1) | 21 (4.9) | 127 (38.4) | 9 (2.7) | 195 (58.9) | 105 (27.2) | 9 (2.3) | 272 (70.5) | 57 (16.4) | 7 (2.0) | 283 (81.6) | 50–75 | <0.01 |
| Livestock meat and poultry | 242 (56.9) | 127 (29.9) | 56 (13.2) | 159 (48.0) | 108 (32.6) | 64 (19.3) | 140 (36.3) | 127 (32.9) | 119 (30.8) | 64 (18.4) | 67 (19.3) | 216 (62.2) | 50–75 | <0.01 |
| Eggs | 302 (71.1) | 80 (18.8) | 43 (10.1) | 219 (66.2) | 71 (21.5) | 41 (12.4) | 226 (58.5) | 110 (28.5) | 50 (13.0) | 170 (49.0) | 82 (23.6) | 95 (27.4) | 50 | <0.01 |
| Milk and its products | 367 (86.4) | 43 (10.1) | 15 (3.5) | 237 (71.6) | 78 (23.6) | 16 (4.8) | 221 (57.3) | 126 (32.6) | 39 (10.1) | 133 (38.3) | 165 (47.6) | 49 (14.1) | 300–500 | <0.01 |
| Soybean and its products | 340 (80.0) | 19 (4.5) | 66 (15.1) | 243 (73.4) | 15 (4.5) | 73 (22.1) | 264 (68.4) | 9 (2.3) | 113 (29.3) | 208 (59.9) | 27 (7.8) | 112 (32.3) | 20 | <0.01 |
| Nuts | 263 (61.9) | 3 (0.7) | 159 (37.4) | 127 (38.4) | 9 (2.7) | 195 (58.9) | 105 (27.2) | 9 (2.3) | 272 (70.5) | 57 (16.4) | 7 (2.0) | 283 (81.6) | 10 | <0.01 |
| Characteristics | Value n (%) | Unadjusted Model, OR (95% CI) | Multivariable Model 2, OR (95% CI) |
|---|---|---|---|
| Gestational hypertension | 71 (4.8) | 0.26 (0.19,0.35) * | 0.30 (0.20,0.37) * |
| Gestational diabetes mellitus | 163 (10.9) | 0.37 (0.30,0.45) * | 0.38 (0.31,0.48) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ding, Y.; Xu, F.; Zhong, C.; Tong, L.; Li, F.; Li, Q.; Chen, R.; Zhou, X.; Li, X.; Cui, W.; et al. Association between Chinese Dietary Guidelines Compliance Index for Pregnant Women and Risks of Pregnancy Complications in the Tongji Maternal and Child Health Cohort. Nutrients 2021, 13, 829. https://doi.org/10.3390/nu13030829
Ding Y, Xu F, Zhong C, Tong L, Li F, Li Q, Chen R, Zhou X, Li X, Cui W, et al. Association between Chinese Dietary Guidelines Compliance Index for Pregnant Women and Risks of Pregnancy Complications in the Tongji Maternal and Child Health Cohort. Nutrients. 2021; 13(3):829. https://doi.org/10.3390/nu13030829
Chicago/Turabian StyleDing, Ye, Fangping Xu, Chunrong Zhong, Lishu Tong, Fang Li, Qian Li, Renjuan Chen, Xuezhen Zhou, Xiating Li, Wenli Cui, and et al. 2021. "Association between Chinese Dietary Guidelines Compliance Index for Pregnant Women and Risks of Pregnancy Complications in the Tongji Maternal and Child Health Cohort" Nutrients 13, no. 3: 829. https://doi.org/10.3390/nu13030829
APA StyleDing, Y., Xu, F., Zhong, C., Tong, L., Li, F., Li, Q., Chen, R., Zhou, X., Li, X., Cui, W., Zhang, Y., Huang, L., Xu, S., Liu, C., Wu, J., Chen, X., Gao, Q., Yang, N., & Wang, Z. (2021). Association between Chinese Dietary Guidelines Compliance Index for Pregnant Women and Risks of Pregnancy Complications in the Tongji Maternal and Child Health Cohort. Nutrients, 13(3), 829. https://doi.org/10.3390/nu13030829