The Effectiveness of Supportive Psychotherapy in Weight Loss in a Group of Young Overweight and Obese Women
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
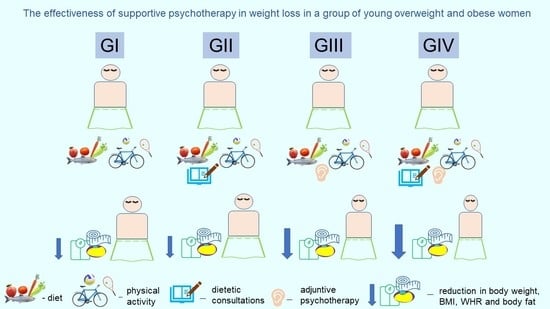
2.2. Study Procedure
2.3. Psychotherapeutic Procedure
2.4. Anthropometric Measurements
2.5. Statistics
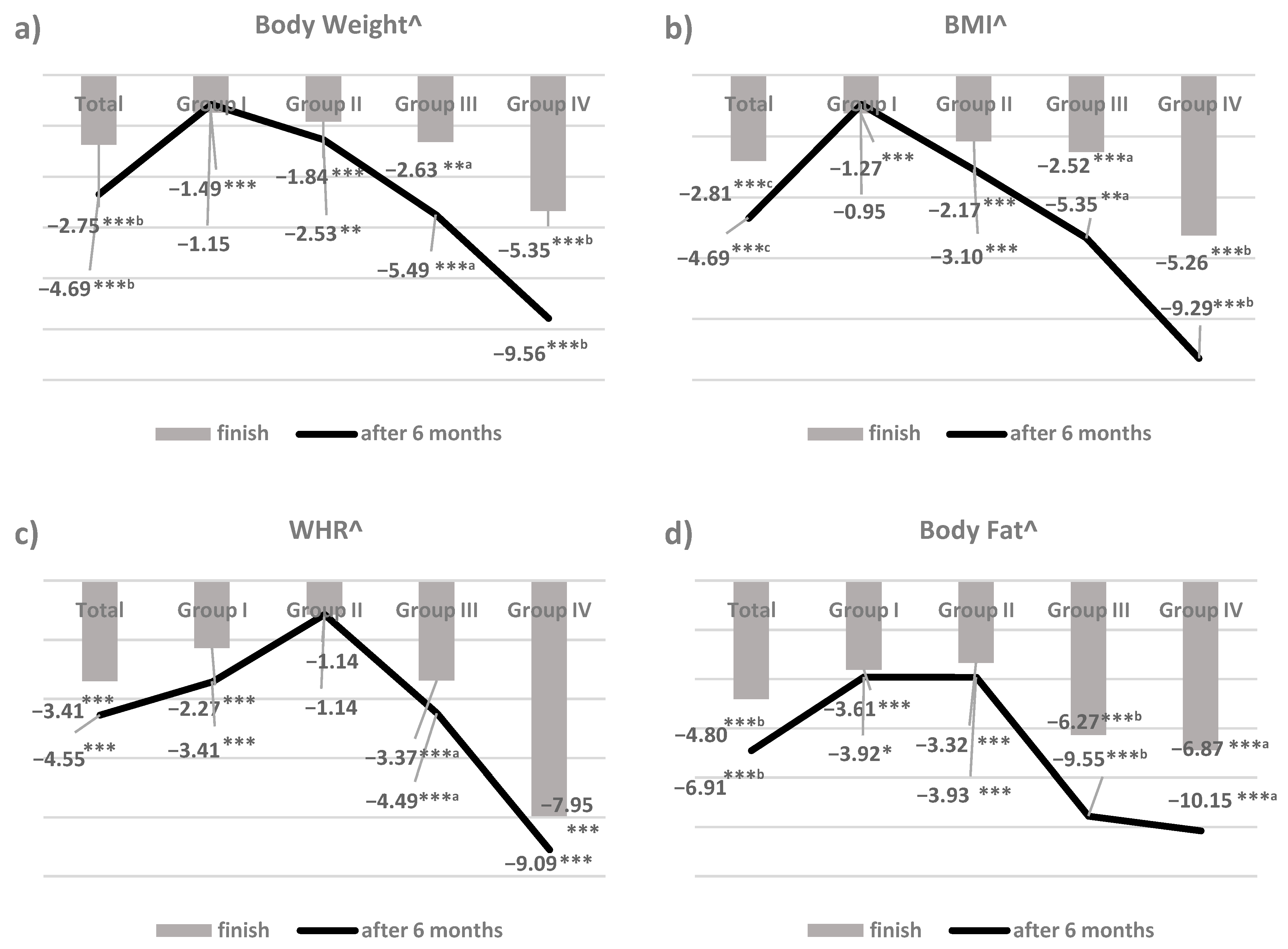
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Castelnuovo, G.; Pietrabissa, G.; Manzoni, G.M.; Corti, S.; Ceccarini, M.; Borrello, M.; Giusti, E.M.; Novelli, M.; Cattivelli, R.; Middleton, N.A.; et al. Chronic care management of globesity: Promoting healthier lifestyles in traditional and mHealth based settings. Front. Psychol. 2015, 6, 1557. [Google Scholar] [CrossRef]
- Poobalan, A.; Aucott, L. Obesity among young adults in developing countries: A systematic overview. Curr. Obes. Rep. 2016, 5, 2–13. [Google Scholar] [CrossRef]
- Dietz, W.H. Obesity and excessive weight gain in young adults. New targets for prevention. JAMA 2017, 318, 241–242. [Google Scholar] [CrossRef] [PubMed]
- Basen-Engquist, K.; Chang, M. Obesity and cancer risk: Recent review and evidence. Curr. Oncol. Rep. 2011, 13, 71–76. [Google Scholar] [CrossRef]
- Hruby, A.; Manson, J.E.; Qi, L.; Malik, V.S.; Rimm, E.B.; Sun, Q.; Willett, W.C.; Hu, F.B. Determinants and Consequences of Obesity. Am. J. Public Health 2016, 106, 1656–1662. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Burke, L.E.; Bray, G.A.; Blair, S.; Allison, D.B.; Pi-Sunyer, X.; Hong, Y.; Eckel, R.H.; American Heart Association Council on Nutrition, Physical Activity, and Metabolism. Clinical implications of obesity with special focus on cardiovascular disease: A statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: Endorsed by the American College of Cardiology Foundation. Circulation 2004, 110, 2952–2967. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.D.; Basu, A. Estimating the medical care costs of obesity in the United States: Systematic review, meta-analysis, and empirical analysis. Value Health 2016, 19, 602–613. [Google Scholar] [CrossRef]
- Russel-Mayhew, S.; McVey, G.; Bardick, A.; Ireland, A. Mental health, wellness, and childhood overweight/obesity. J. Obes. 2012, 2012, 281801. [Google Scholar] [CrossRef]
- Puhl, R.M.; Heuer, C.A. Obesity stigma: Important considerations for public health. Am. J. Public Health 2010, 100, 1019–1028. [Google Scholar] [CrossRef]
- Goisser, S.; Kiesswetter, E.; Schoene, D.; Torbahn, G.; Bauer, J.M. Dietary weight-loss interventions for the management of obesity in older adults. Rev. Endocr. Metab. Disord. 2020, 21, 355–368. [Google Scholar] [CrossRef]
- Gibbs, B.B.; Tudorascu, D.; Bryce, C.L.; Comer, D.; Fischer, G.S.; Hess, R.; Huber, K.A.; McTigue, K.M.; Simkin-Silverman, L.R.; Conroy, M.B. Diet and physical activity behaviors in primary care patients with recent intentional weight loss. Transl. J. Am. Coll. Sports Med. 2017, 2, 114–121. [Google Scholar] [PubMed]
- Golbidi, S.; Daiber, A.; Korac, B.; Li, H.; Faadiel Essop, M.; Laher, I. Health benefits of fasting and caloric restriction. Curr. Diab. Rep. 2017, 17, 123. [Google Scholar] [CrossRef]
- Bruci, A.; Tuccinardi, D.; Tozzi, R.; Balena, A.; Santucci, S.; Frontani, R.; Mariani, S.; Basciani, S.; Spera, G.; Gnessi, L.; et al. Very low-calorie ketogenic diet: A safe and effective tool for weight loss in patients with obesity and mild kidney failure. Nutrients 2020, 12, 333. [Google Scholar] [CrossRef]
- Johnstone, A. Fasting for weight loss: An effective strategy or latest dieting trend? Int. J. Obes. 2015, 39, 727–733. [Google Scholar] [CrossRef]
- Paul, L.; van der Heiden, C.; Hoek, H.W. Cognitive behavioral therapy and predictors of weight loss in bariatric surgery patients. Curr. Opin. Psychiatry 2017, 30, 474–479. [Google Scholar] [CrossRef]
- Habib, S.; Samamé, J.; Galvani, C.A. Treatment of morbid obesity. Surgery Curr. Res. 2013, 3, 135. [Google Scholar] [CrossRef]
- Schigt, A.; Gerdes, V.E.A.; Cense, H.A.; Berends, F.J.; van Dielen, F.M.H.; Janssen, I.; van der Laar, A.; van Wagensveld, B.A.; Romijn, J.A.; Serlie, M.J. Bariatric surgery is an effective treatment for morbid obesity. Neth. J. Med. 2013, 71, 4–9. [Google Scholar] [PubMed]
- Van Dorsten, B.; Lindley, E.M. Cognitive and behavioral approaches in the treatment of obesity. Med. Clin. N. Am. 2011, 95, 971–988. [Google Scholar] [CrossRef]
- Davis, C.; Curtis, C.; Levitan, R.D.; Carter, J.C.; Kaplan, A.S.; Kennedy, J.L. Evidence that food addiction is a valid phenotype of obesity. Appetite 2011, 57, 711–717. [Google Scholar] [CrossRef]
- Stroebe, W.; Papies, E.K.; Aarts, H. From homeostatic to hedonic theories of eating: Self-regulatory failure in food-rich environments. Appl. Psychol. 2008, 57, 172–193. [Google Scholar] [CrossRef]
- Schwartz, D.C.; Nickow, M.S.; Arseneau, R.; Gisslow, M.T. A substance called food: Long-term psychodynamic group treatment for compulsive overeating. Int. J. Group Psychother. 2015, 65, 387–409. [Google Scholar] [CrossRef] [PubMed]
- Kiesewetter, S.; Koepsel, A.; Koepp, W.; Kallenbach-Dermutz, B.; Pfeiffer, A.F.H.; Spranger, J.; Deter, H.-C. Psychodynamic mechanism and weight reduction in obesity group therapy—first observations with different attachment styles. Psychosoc. Med. 2010, 7. [Google Scholar] [CrossRef]
- Eichen, D.M.; Matheson, B.E.; Appleton-Knapp, S.L.; Boutelle, K.N. Neurocognitive treatments for eating disorders and obesity. Curr. Psychiatry Rep. 2017, 19, 62. [Google Scholar] [CrossRef]
- Alamuddin, N.; Wadden, T.A. Behavioral treatment of the patient with obesity. Endocrinol. Metab. Clin. N. Am. 2016, 45, 565–580. [Google Scholar] [CrossRef] [PubMed]
- Lv, N.; Azar, K.M.J.; Goldman Rosas, L.; Wulfovich, S.; Xiao, L.; Ma, J. Behavioral lifestyles interventions for moderate and severe obesity: A systematic review. Prev. Med. 2017, 100, 180–193. [Google Scholar] [CrossRef]
- Chu, D.-T.; Nguyet, N.T.M.; Nga, V.T.; Lien, N.T.V.; Vo, D.D.; Lien, N.; Ngoc, V.T.N.; Le, D.-H.; Nga, V.B.; Van Tu, P.; et al. An update on obesity: Mental consequences and psychological interventions. Diabetes Metab. Syndr. 2019, 13, 155–160. [Google Scholar] [CrossRef]
- Teufel, M.; Becker, S.; Rieber, N.; Stephan, K.; Zipfel, S. Psychotherapie und Adipositas. Strategien, Herausforderungen und Chancen. Nervenarzt 2011, 82, 1133–1139. [Google Scholar] [CrossRef]
- Ogata, K.; Koyama, K.I.; Amitani, M.; Amitani, H.; Asakawa, A.; Inui, A. The effectiveness of cognitive behavioral therapy with mindfulness and an internet intervention for obesity: A case series. Front. Nutr. 2018, 5, 56. [Google Scholar] [CrossRef]
- Mason, C.; de Dieu Tapsoba, J.; Duggan, C.; Wang, C.-Y.; Alfano, C.M.; McTiernan, A. Eating behaviors and weight loss outcomes in a 12-month randomized trial of diet and/or exercise intervention in postmenopausal women. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 113. [Google Scholar] [CrossRef]
- Iacovino, J.M.; Gredysa, D.M.; Altman, M.; Wilfley, D.E. Psychological treatments for binge eating disorder. Curr. Psychiatry Rep. 2012, 14, 432–446. [Google Scholar] [CrossRef]
- Maroda, K.J. Techniki Psychoterapii Psychodynamicznej. Praca nad Emocjami w Relacji Terapeutycznej, 1st ed.; Wydawnictwo Uniwersytetu Jagiellońskiego: Kraków, Poland, 2012; pp. 15–298. [Google Scholar]
- Gabbard, G.O. Psychiatria Psychodynamiczna w Praktyce Klinicznej, 2nd ed.; Wydawnictwo Uniwersytetu Jagiellońskiego: Kraków, Poland, 2014; pp. 17–628. [Google Scholar]
- Paans, N.P.G.; Bot, M.; Brouwer, I.A.; Visser, M.; Gili, M.; Roca, M.; Hegerl, U.; Kohls, E.; Owens, M.; Watkins, E.; et al. Effects of food-related behavioral activation therapy on eating styles, diet quality and body weight change: Results from the MooDFOOD Randomized Clinical Trial. J. Psychosom. Res. 2020, 137. [Google Scholar] [CrossRef]
- Palmeira, A.L.; Branco, T.L.; Martins, S.C.; Minderico, C.S.; Silva, M.N.; Vieria, P.N.; Barata, J.T.; Serpa, S.O.; Sardinha, L.B.; Teixeira, P.J. Changes in body image and psychological well-being during behavioral obesity treatment: Associations with weight loss and maintenance. Body Image 2010, 7, 187–193. [Google Scholar] [CrossRef]
- Cooper, A.; Doll, A.H.; Hawker, D.M.; Byrne, S.; Bonner, G.; Eeley, E.; O’Connor, M.E.; Fairbrun, C.G. Testing a new cognitive behavioral treatment for obesity: A randomized controlled trial with three-year-follow-up. Behav. Res. Ther. 2010, 48, 706–713. [Google Scholar] [CrossRef]
- Butryn, M.L.; Webb, V.; Wadden, T.A. Behavioral treatment of obesity. Psychiatr. Clin. N. Am. 2011, 34, 841–859. [Google Scholar] [CrossRef] [PubMed]
- Bogle, V.; Sykes, C. Psychological interventions in the treatment of childhood obesity: What we know and need to find out. J. Health Psychol. 2011, 16, 997–1014. [Google Scholar] [CrossRef] [PubMed]
- Karasu, S.R. Psychotherapy-lite: Obesity and its role of the mental health practitioner. Am. J. Psychother. 2013, 67, 3–22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shaw, K.; O’Rourke, P.; Del Mar, C.; Kenardy, J. Psychological interventions for overweight or obesity. Cochrane Database Syst. Rev. 2005, 18, 1–23. [Google Scholar] [CrossRef]
- Painot, D.; Jotterand, S.; Kammer, A.; Fossati, M.; Golay, A. Simultaneous nutritional cognitive—behavioural therapy in obese patients. Patient Educ. Couns. 2001, 42, 47–52. [Google Scholar] [CrossRef]
- Sbrocco, T.; Nedegaard, R.C.; Stone, J.M.; Lewis, E.L. Behavioral choice treatment promotes continuing weight loss: Preliminary results of a cognitive-behavioral decision-based treatment for obesity. J. Consult. Clin. Psychol. 1999, 67, 260–266. [Google Scholar] [CrossRef]
- Gade, H.; Friborg, O.; Rosenvinge, J.H.; Cvancarova Småstuen, M.; Hjelmesæth, J. The impact of a preoperative cognitive behavioural therapy (CBT) on dysfunctional eating behaviours, affective symptoms and body weight 1 year after bariatric surgery: A randomized controlled trial. Obes. Surg. 2015, 25, 2112–2119. [Google Scholar] [CrossRef]
- Loveman, E.; Frampton, G.K.; Shepherd, J.; Picot, J.; Cooper, K.; Bryant, J.; Welch, K.; Clegg, A. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: A systematic review. Health Technol. Assess 2011, 15, 1–182. [Google Scholar] [CrossRef]
- Parylak, S.L.; Koob, G.F.; Zorilla, E.P. The dark side of food addiction. Physiol. Behav. 2011, 104, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Beutel, M.; Thiede, R.; Wiltink, J.; Sobez, I. Effectiveness of behavioral and psychodynamic in-patient treatment of severe obesity—first results from a randomized study. Int. J. Obes. 2001, 25, S96–S98. [Google Scholar] [CrossRef][Green Version]
- Castelnuovo, G.; Pietrabissa, G.; Manzoni, G.M.; Cattivelli, R.; Rossi, A.; Novelli, M.; Varallo, G.; Molinari, E. Cognitive behavioral therapy to aid weight loss in obese patients: Current perspectives. Psychl. Res. Behav. Manag. 2017, 10, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Loos, R.J.F.; Bouchard, C. Obesity—Is it a genetic disorder? J. Intern. Med. 2003, 254, 401–425. [Google Scholar] [CrossRef] [PubMed]
| Total n = 60 | GI n = 15 | GII n = 15 | GIII n = 15 | GIV n = 15 | |
|---|---|---|---|---|---|
| Body weight (kg) | 87.4 ± 6.0 | 87.3 ± 5.9a | 87.0 ± 5.3a | 87.5 ± 7.5a | 87.9 ± 5.1a |
| (78.0–113.0) | (78.0–99.0) | (80.0–95.0) | (82.0–113.0) | (80.0–100.0) | |
| 87.0 | 88.0 | 85.0 | 85.0 | 89.0 | |
| BMI (kg/m2) | 32.0 ± 2.0 | 31.6 ± 2.4a | 32.3 ± 1.8a | 31.8 ± 1.9a | 32.3 ± 1.9a |
| (28.0–37.7) | (28.0–37.7) | (28.7–35.0) | (29.4–36.9) | (28.3–36.9) | |
| 31.6 | 31.2 | 32.4 | 31.2 | 32.0 | |
| Waist (cm) | 83.2 ± 6.7 | 83.5 ± 7.7a | 83.2 ± 6.8a | 82.4 ± 7.2a | 83.5 ± 4.8a |
| (69.0–94.0) | (69.0–93.0) | (72.0–94.0) | (69.0–92.0) | (74.0–90.0) | |
| 85.0 | 87.0 | 85.0 | 84.0 | 85.0 | |
| Hip (cm) | 94.3 ± 6.9 | 94.6 ± 5.9a | 94.5 ± 6.3a | 92.5 ± 5.8a | 95.4 ± 8.8a |
| (79.0–112.0) | (86.0–104.0) | (84.0–106.0) | (86.0–102.0) | (79.0–112.0) | |
| 94.5 | 96.0 | 94.5 | 89.0 | 98.0 | |
| WHR | 0.88 ± 0.05 | 0.88 ± 0.05a | 0.88 ± 0.05a | 0.89 ± 0.06a | 0.88 ± 0.06a |
| (0.80–0.99) | (0.80–0.97) | (0.81–0.97) | (0.80–0.99) | (0.80–0.99) | |
| 0.88 | 0.89 | 0.86 | 0.90 | 0.88 | |
| Body fat (%) | 33.3 ± 2.4 | 33.2 ± 2.4a | 33.1 ± 2.0a | 33.5 ± 2.4a | 33.5 ± 2.9a |
| (29.8–38.8) | (30.0–38.8) | (30.5–38.3) | (30.0–38.8) | (29.8–38.8) | |
| 33.4 | 33.0 | 33.2 | 33.6 | 33.4 |
| Total n = 58 | GI n = 14 | GII n = 14 | GIII n = 15 | GIV n = 15 | |
|---|---|---|---|---|---|
| Body weight (kg) | 85.0 ± 5.8 | 86.0 ± 6.2b | 85.4 ± 5.5ab | 85.2 ± 6.7ab | 83.2 ± 3.9a |
| (75.0–105.0) | (75.0–100.0) | (76.0–95.0) | (80.0–105.0) | (76.0–88.0) | |
| 85.0 | 87.0 | 84.0 | 84.0 | 85.0 | |
| BMI (kg/m2) | 31.1 ± 2.1 | 31.1 ± 2.5a | 31.6 ± 2.0a | 31.0 ± 1.5a | 30.6 ± 1.9a |
| (26.9–38.1) | (27.6–38.1) | (28.3–34.3) | (29.4–34.3) | (26.9–35.3) | |
| 30.8 | 30.5 | 32.0 | 30.5 | 30.5 | |
| Waist (cm) | 79.3 ± 6.5 | 80.3 ± 7.6b | 81.5 ± 6.1b | 78.5 ± 6.2ab | 76.9 ± 5.1a |
| (65.0–91.0) | (65.0–91.0) | (72.0–90.0) | (69.0–88.0) | (70.0–85.0) | |
| 80.0 | 82.0 | 83.0 | 80.0 | 78.0 | |
| Hip (cm) | 93.5 ± 6.5 | 93.8 ± 5.7a | 93.5 ± 5.2a | 91.7 ± 5.3a | 95.1 ± 8.7a |
| (79.0–110.0) | (85.0–103.0) | (84.0–100.0) | (85.0–102.0) | (79.0–110.0) | |
| 93.5 | 96.0 | 94.0 | 89.0 | 98.0 | |
| WHR | 0.85 ± 0.05 | 0.86 ± 0.05b | 0.87 ± 0.05b | 0.86 ± 0.05b | 0.81 ± 0.04a |
| (0.74–0.97) | (0.76–0.93) | (0.78–0.94) | (0.78–0.97) | (0.74–0.89) | |
| 0.85 | 0.85 | 0.86 | 0.86 | 0.80 | |
| Body fat (%) | 31.8 ± 2.5 | 32.0 ± 2.5a | 32.0 ± 2.1a | 31.4 ± 2.5a | 31.2 ± 2.4a |
| (27.0–38.3) | (28.7–38.3) | (28.6–37.9) | (28.0–37.0) | (27.0–35.5) | |
| 31.7 | 31.3 | 32.0 | 30.3 | 30.6 |
| KERRYPNX | Total n = 51 | GI n = 12 | GII n = 12 | GIII n = 14 | GIV n = 15 |
|---|---|---|---|---|---|
| Body weight (kg) | 83.3 ± 6.0 | 86.3 ± 7.3b | 84.8 ± 5.0b | 82.6 ± 4.9b | 79.5 ± 3.8a |
| (74.0–99.0) | (74.0–99.0) | (78.0–95.0) | (76.0–93.0) | (74.0–89.0) | |
| 82.5 | 86.0 | 84.0 | 82.0 | 78.0 | |
| BMI (kg/m2) | 30.5 ± 2.4 | 31.3 ± 3.0b | 31.3 ± 1.8b | 30.1 ± 1.4a | 29.3 ± 2.3a |
| (25.4–37.3) | (27.6–37.3) | (28.4–34.3) | (28.3–34.2) | (25.4–32.3) | |
| 30.3 | 30.5 | 31.9 | 29.7 | 29.4 | |
| Waist (cm) | 78.2 ± 7.6 | 80.3 ± 8.8b | 81.1 ± 6.4b | 77.7 ± 5.9b | 73.7 ± 6.6a |
| (60.0–92.0) | (62.0–92.0) | (70.0–90.0) | (69.0–88.0) | (60.0–82.0) | |
| 80.0 | 81.0 | 83.0 | 80.0 | 74.0 | |
| Hip (cm) | 92.9 ± 6.2 | 93.9 ± 6.0a | 93.4 ± 5.1a | 91.5 ± 5.3a | 92.8 ± 7.8a |
| (79.0–105.0) | (84.0–105.0) | (84.0–100.0) | (85.0–102.0) | (79.0–105.0) | |
| 93.0 | 96.0 | 94.0 | 89.0 | 94.0 | |
| WHR | 0.84 ± 0.06 | 0.85 ± 0.06b | 0.87 ± 0.05b | 0.85 ± 0.05b | 0.80 ± 0.05a |
| (0.69–0.97) | (0.72–0.94) | (0.80–0.94) | (0.78–0.97) | (0.69–0.89) | |
| 0.83 | 0.85 | 0.85 | 0.85 | 0.80 | |
| Body fat (%) | 31.0 ± 2.7 | 31.9 ± 3.0b | 31.8 ± 2.3b | 30.3 ± 2.3a | 30.1 ± 2.6a |
| (27.0–38.3) | (28.0–38.3) | (28.0–37.9) | (28.0–37.0) | (27.0–36.5) | |
| 30.9 | 31.3 | 32.0 | 30.0 | 29.3 |
| Group | GI | GII | GIII | GIV | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time point | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 |
| BMI > 30.0 | 85 | 67 | 67 | 87 | 70 | 67 | 87 | 65 | 47 | 87 | 53 | 40 |
| BMI 25.0–24.9 | 15 | 33 | 33 | 13 | 30 | 33 | 13 | 35 | 53 | 13 | 47 | 60 |
| χ2 (p) | 8.9 (0.003) | 8.6 (0.003) | 13.3 (0.000) | 27.5 (0.000) | ||||||||
| 5.5 (0.064) | 12.3 (0.002) | 35.9 (0.000) | 29.0 (0.000) | |||||||||
| WHR > 0.85 | 73 | 60 | 53 | 75 | 73 | 65 | 70 | 60 | 53 | 72 | 30 | 20 |
| WHR 0.8–0.84 | 27 | 33 | 40 | 25 | 20 | 35 | 30 | 33 | 40 | 28 | 47 | 47 |
| WHR < 0.79 | 0 | 7 | 7 | 0 | 7 | 0 | 0 | 7 | 7 | 0 | 23 | 33 |
| χ2 (p) | 6.6 (0.037) | 4.9 (0.087) | 5.5 (0.063) | 42.9 (0.000) | ||||||||
| 11.1 (0.025) | 12.8 (0.012) | 11.1 (0.025) | 68.5 (0.000) | |||||||||
| Body fat > 30% | 100 | 88 | 80 | 100 | 83 | 78 | 100 | 83 | 73 | 93 | 70 | 59 |
| Body fat < 30% | 0 | 12 | 20 | 0 | 17 | 22 | 0 | 17 | 27 | 7 | 30 | 41 |
| χ2 (p) | 9.9 (0.002) | 15.6 (0.000) | 15.6 (0.000) | 17.5 (0.000) | ||||||||
| 18.6 (0.000) | 20.8 (0.000) | 27.0 (0.000) | 31.3 (0.000) | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juchacz, K.; Kłos, P.; Dziedziejko, V.; Wójciak, R.W. The Effectiveness of Supportive Psychotherapy in Weight Loss in a Group of Young Overweight and Obese Women. Nutrients 2021, 13, 532. https://doi.org/10.3390/nu13020532
Juchacz K, Kłos P, Dziedziejko V, Wójciak RW. The Effectiveness of Supportive Psychotherapy in Weight Loss in a Group of Young Overweight and Obese Women. Nutrients. 2021; 13(2):532. https://doi.org/10.3390/nu13020532
Chicago/Turabian StyleJuchacz, Krzysztof, Patrycja Kłos, Violetta Dziedziejko, and Rafał W. Wójciak. 2021. "The Effectiveness of Supportive Psychotherapy in Weight Loss in a Group of Young Overweight and Obese Women" Nutrients 13, no. 2: 532. https://doi.org/10.3390/nu13020532
APA StyleJuchacz, K., Kłos, P., Dziedziejko, V., & Wójciak, R. W. (2021). The Effectiveness of Supportive Psychotherapy in Weight Loss in a Group of Young Overweight and Obese Women. Nutrients, 13(2), 532. https://doi.org/10.3390/nu13020532