Health-Related Quality of Life in Spanish Women with Eating Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Short-Form Health Survey
2.2. Eating Attitudes Test-26
2.3. Evaluation of Results in Patient-Centered Health: Quality of Life
2.4. Attitudes towards Change in Eating Disorders Questionnaire (ACTA)
2.5. Ethics Consideration
2.6. Statistical Analysis
3. Results
3.1. Clinical and Sociodemographic Data
3.2. Health-Related Quality of Life (HRQoL) by Eating Disorder
3.3. Attitudes towards Change in Eating Disorders
3.4. Eating Attitudes Test-26
3.5. Determinants of HRQoL
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Institute of Medicine (US) Division of Health Care; Heithoff, K.A.; Lohr, K. Assessing Health-Related Quality of Life Outcomes; National Academies Press: Washington, DC, USA, 1990. [Google Scholar]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.E.; Grinspoon, S.K.; Klibanski, A.; Herzog, D.B. Eating Disorders. N. Engl. J. Med. 1999, 340, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Hsu, L.K.G. Eating Disorders; Guilford Press: New York, NY, USA, 1990; ISBN 978-0-89862-401-4. [Google Scholar]
- De la Rie, S.M.; Noordenbos, G.; van Furth, E.F. Quality of life and eating disorders. Qual. Life Res. 2005, 14, 1511–1522. [Google Scholar] [CrossRef] [PubMed]
- Doll, H.A.; Petersen, S.E.; Stewart-Brown, S.L. Eating disorders and emotional and physical well-being: Associations between student self-reports of eating disorders and quality of life as measured by the SF-36. Qual. Life Res. 2005, 14, 705–717. [Google Scholar] [CrossRef] [PubMed]
- González-Pinto, A.; Inmaculada, F.; Cristina, R.; de Corres Blanca, F.; Sonsoles, E.; Fernando, R.; Purificacion, L. Purging behaviors and comorbidity as predictive factors of quality of life in anorexia nervosa. Int. J. Eat. Disord. 2004, 36, 445–450. [Google Scholar] [CrossRef]
- Hay, P. Quality of life and bulimic eating disorder behaviors: Findings from a community-based sample. Int. J. Eat. Disord. 2003, 33, 434–442. [Google Scholar] [CrossRef]
- Pollack, L.O.; McCune, A.M.; Mandal, K.; Lundgren, J.D. Quantitative and Qualitative Analysis of the Quality of Life of Individuals With Eating Disorders. Prim. Care Companion CNS Disord. 2015, 17. [Google Scholar] [CrossRef]
- Singleton, C.; Kenny, T.E.; Hallett, D.; Carter, J.C. Depression Partially Mediates the Association Between Binge Eating Disorder and Health-Related Quality of Life. Front. Psychol. 2019, 10, 209. [Google Scholar] [CrossRef]
- Ágh, T.; Kovács, G.; Supina, D.; Pawaskar, M.; Herman, B.K.; Vokó, Z.; Sheehan, D.V. A systematic review of the health-related quality of life and economic burdens of anorexia nervosa, bulimia nervosa, and binge eating disorder. Eat. Weight Disord. 2016, 21, 353–364. [Google Scholar] [CrossRef]
- Jenkins, P.E.; Hoste, R.R.; Meyer, C.; Blissett, J.M. Eating disorders and quality of life: A review of the literature. Clin. Psychol. Rev. 2011, 31, 113–121. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing: Washington, DC, USA, 2013; ISBN 978-0-89042-557-2. [Google Scholar]
- Latner, J.D.; Vallance, J.K.; Buckett, G. Health-related quality of life in women with eating disorders: Association with subjective and objective binge eating. J. Clin. Psychol. Med. Settings 2008, 15, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Peláez-Fernández, M.A.; Raich, R.; Labrador, F. Eating disorders in Spain: Revision of empirical epidemiological studies. Mex. J. Eat. Disord. 2010, 1, 62–75. [Google Scholar]
- Smith, A.R.; Ortiz, S.N.; Forrest, L.N.; Velkoff, E.A.; Dodd, D.R. Which Comes First? An Examination of Associations and Shared Risk Factors for Eating Disorders and Suicidality. Curr. Psychiatry Rep. 2018, 20, 77. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.J.; Vartanian, L.R.; Brownell, K.D. The relationship between eating disorder not otherwise specified (EDNOS) and officially recognized eating disorders: Meta-analysis and implications for DSM. Psychol. Bull. 2009, 135, 407–433. [Google Scholar] [CrossRef]
- Engel, S.G.; Adair, C.E.; Las Hayas, C.; Abraham, S. Health-related quality of life and eating disorders: A review and update. Int. J. Eat. Disord. 2009, 42, 179–187. [Google Scholar] [CrossRef]
- Fayers, P.; Machin, D. Quality of Life: The Assessment, Analysis and Interpretation of Patient-Reported Outcomes; John Wiley & Sons: Hoboken, NJ, USA, 2007; ISBN 978-0-470-02450-8. [Google Scholar]
- Leung, S.F.; Ma, J.L.; Russell, J. Enhancing quality of life in people with disordered eating using an online self-help programme. J. Eat. Disord. 2013, 1, 9. [Google Scholar] [CrossRef]
- Vancampfort, D.; Probst, M.; Adriaens, A.; Pieters, G.; De Hert, M.; Stubbs, B.; Soundy, A.; Vanderlinden, J. Changes in physical activity, physical fitness, self-perception and quality of life following a 6-month physical activity counseling and cognitive behavioral therapy program in outpatients with binge eating disorder. Psychiatry Res. 2014, 219, 361–366. [Google Scholar] [CrossRef]
- Badia, X.; Roset, M.; Herdman, M.; Kind, P. A comparison of United Kingdom and Spanish general population time trade-off values for EQ-5D health states. Med. Decis. Mak. 2001, 21, 7–16. [Google Scholar] [CrossRef]
- Hart, L.M.; Gordon, A.R.; Sarda, V.; Calzo, J.P.; Sonneville, K.R.; Samnaliev, M.; Austin, S.B. The association of disordered eating with health-related quality of life in U.S. young adults and effect modification by gender. Qual. Life Res. 2020, 29, 1203–1215. [Google Scholar] [CrossRef]
- Prochaska, J.O.; DiClemente, C.C. Stages and processes of self-change of smoking: Toward an integrative model of change. J. Consult. Clin. Psychol. 1983, 51, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Junne, F.; Ziser, K.; Mander, J.; Martus, P.; Denzer, C.; Reinehr, T.; Wabitsch, M.; Wiegand, S.; Renner, T.; Giel, K.E.; et al. Development and psychometric validation of the ‘Parent Perspective University of Rhode Island Change Assessment-Short’ (PURICA-S) Questionnaire for the application in parents of children with overweight and obesity. BMJ Open 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Hasler, G.; Delsignore, A.; Milos, G.; Buddeberg, C.; Schnyder, U. Application of Prochaska’s transtheoretical model of change to patients with eating disorders. J. Psychosom. Res. 2004, 57, 67–72. [Google Scholar] [CrossRef]
- Panea-Pizarro, I.; López-Espuela, F.; Martos-Sánchez, A.; Domínguez-Martín, A.T.; Beato-Fernández, L.; Moran-García, J.M. Internet addiction and Facebook addiction in Spanish women with eating disorders. Arch. Psychiatr. Nurs. 2020. [Google Scholar] [CrossRef]
- Loria Kohen, V.; Gómez Candela, C.; Lourenço Nogueira, T.; Pérez Torres, A.; Castillo Rabaneda, R.; Villarino Marin, M.; Bermejo López, L.; Zurita, L. Evaluation of the utility of a Nutrition Education Program with Eating Disorders. Nutr. Hosp. 2009, 24, 558–567. [Google Scholar] [PubMed]
- Beato Fernández, L.; Rodríguez Cano, T. Attitudes towards change in eating disorders (ACTA). Development and psychometric properties. Actas Esp. Psiquiatr. 2003, 31, 111–119. [Google Scholar]
- Rodríguez-Cano, T.; Beato-Fernández, L. Attitudes towards change and treatment outcome in eating disorders. Eat. Weight Disord. 2005, 10, 59–65. [Google Scholar] [CrossRef]
- Padierna, A.; Quintana, J.M.; Arostegui, I.; Gonzalez, N.; Horcajo, M.J. The health-related quality of life in eating disorders. Qual. Life Res. 2000, 9, 667–674. [Google Scholar] [CrossRef]
- Pohjolainen, V.; Koponen, S.; Räsänen, P.; Roine, R.P.; Sintonen, H.; Karlsson, H. Long-term health-related quality of life in eating disorders. Qual. Life Res. 2016, 25, 2341–2346. [Google Scholar] [CrossRef]
- Keski-Rahkonen, A.; Hoek, H.W.; Susser, E.S.; Linna, M.S.; Sihvola, E.; Raevuori, A.; Bulik, C.M.; Kaprio, J.; Rissanen, A. Epidemiology and course of anorexia nervosa in the community. Am. J. Psychiatry 2007, 164, 1259–1265. [Google Scholar] [CrossRef]
- Masheb, R.M.; Grilo, C.M. Quality of life in patients with binge eating disorder. Eat. Weight Disord. 2004, 9, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Grenon, R.; Tasca, G.A.; Cwinn, E.; Coyle, D.; Sumner, A.; Gick, M.; Bissada, H. Depressive symptoms are associated with medication use and lower health-related quality of life in overweight women with binge eating disorder. Womens Health Issues 2010, 20, 435–440. [Google Scholar] [CrossRef]
- Strand, M.; Bulik, C.M.; Gustafsson, S.A.; von Hausswolff-Juhlin, Y.; Welch, E. Self-admission to inpatient treatment in anorexia nervosa: Impact on healthcare utilization, eating disorder morbidity, and quality of life. Int. J. Eat. Disord. 2020. [Google Scholar] [CrossRef]
- Iyar, M.M.; Cox, D.W.; Kealy, D.; Srikameswaran, S.; Geller, J. Is stage of change enough? Confidence as a predictor of outcome in inpatient treatment for eating disorders. Int. J. Eat. Disord. 2019, 52, 283–291. [Google Scholar] [CrossRef]
- Gusella, J.; Butler, G.; Nichols, L.; Bird, D. A brief questionnaire to assess readiness to change in adolescents with eating disorders: Its applications to group therapy. Eur. Eat. Disord. Rev. 2003, 11, 58–71. [Google Scholar] [CrossRef]
- Oliveira-Cardoso, É.A.; Coimbra, A.C.; Santos, M.A. Quality of life of patients with anorexia and Bulimia Nervosa. Psicol. Teoria Pesqui. 2018, 34. [Google Scholar] [CrossRef]
- Schwartz, C.E.; Andresen, E.M.; Nosek, M.A.; Krahn, G.L.; RRTC Expert Panel on Health Status Measurement. Response shift theory: Important implications for measuring quality of life in people with disability. Arch. Phys. Med. Rehabil. 2007, 88, 529–536. [Google Scholar] [CrossRef]
- Sprangers, M.A.G.; Schwartz, C.E. Integrating response shift into health-related quality of life research: A theoretical model. Soc. Sci. Med. 1999, 48, 1507–1515. [Google Scholar] [CrossRef]
| Variable | Mean (SD)/n (%) | Median | IQR | p-Value (Baseline vs. 6-Months) a |
|---|---|---|---|---|
| Age (years) | 27.3 (10.5) | 25 | 17 | |
| Weight (kg) | 28.4 (23.1) | 50.9 | 15.5 | 0.710 |
| Weight (6-months) (kg) | 28.5 (24.4) | 50.0 | 17.8 | |
| Height (meters) | 1.62 (0.06) | 1.62 | 0.09 | |
| Body mass index (BMI) (kg/m2) | 22.18 (8.38) | 19.19 | 6.04 | 0.730 |
| BMI (6-months) (kg/m2) | 22.19 (8.79) | 19.05 | 6.37 | |
| Smoking # | ||||
| Yes | 68 (54.80%) | |||
| No | 56 (45.20%) | |||
| Eating disorder # | ||||
| Anorexia nervosa | 59 (47.6%) | |||
| Bulimia nervosa | 35 (28.2%) | |||
| Other specified feeding or eating disorder | 19 (15.3%) | |||
| Binge eating disorder | 11 (8.9%) | |||
| Years since the eating disorder diagnosis (years) | 10.3 (7.9) | 8.0 | 12.5 | |
| Years of treatment in the eating disorders unit (years) | 8 (6.5) | 6.0 | 10 | |
| Ever hospitalized # | ||||
| Yes | 64 (51.6%) | |||
| No | 60 (48.4%) | |||
| Marital status # | ||||
| Married | 22 (17.9%) | |||
| Single | 102 (82.1%) | |||
| Education level # | ||||
| Low (primary school) | 5 (4%) | |||
| High school | 79 (63.7%) | |||
| University | 40 (32.3%) | |||
| Mental health (comorbidities) | ||||
| Depression | 35 (41.2%) | |||
| Anxiety | 39 (45.9%) | |||
| Obsessive-compulsive disorder | 11 (12.9%) | |||
| Mental health (comorbidities) (6-months) | ||||
| Depression | 35 (40.7%) | |||
| Anxiety | 38 (44.2%) | |||
| Obsessive-compulsive disorder | 13 (15.1%) | |||
| Autolytic attempt # | ||||
| Yes | 99 (79.8%) | |||
| No | 25 (20.20%) |
| SF-36 Subscales | Anorexia Nervosa (n = 59) | Bulimia Nervosa (n = 35) | Other Specified Feeding or Eating Disorder (n = 19) | Binge Eating Disorder (n = 11) | |
|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | p-Value * | |
| Baseline (n = 124) | |||||
| Physical functioning | 80 (50) | 80 (60) | 60 (45) | 35 (15) | 0.014 1 |
| Physical role | 75 (100) | 75 (100) | 25 (100) | 0 (75) | 0.113 |
| Bodily pain | 5 (20) | 0 (40) | 20 (40) | 20 (20) | 0.114 |
| General health | 57 (5.75) | 56.25 (12) | 56.25 (8) | 57 (7) | 0.224 |
| Vitality | 65 (10) | 65 (10) | 65 (15) | 60 (15) | 0.696 |
| Social functioning | 50 (25) | 50 (25) | 50 (12.5) | 50 (37.5) | 0.917 |
| Emotional role | 0 (33.33) | 33.33 (66.67) | 0 (33.33) | 0 (66.67) | 0.2 |
| Mental health | 60 (8) | 64 (12) | 60 (16) | 64 (12) | 0.623 |
| 6-month follow-up (n = 120) | |||||
| Physical functioning | 90 (30) (p < 0.001)) | 64 (12) (p = 0.009) | 80 (35) (p = 0.007) | 45 (55) | 0.01 2 |
| Physical role | 75 (100) | 90 (60) | 25 (100) | 0 (75) | 0.113 |
| Bodily pain | 10 (40) | 0 (40) | 20 (40) | 40 (40) | 0.01 3 |
| General health | 57 (6.25) (p = 0.038) | 56.25 (10) | 57 (8) | 60 (12) | 0.08 |
| Vitality | 65 (10) | 65 (10) | 65 (15) | 60 (15) | 0.696 |
| Social functioning | 50 (12.5) | 50 (25) | 50 (25) | 50 (25) | 0.484 |
| Emotional role | 0 (33.33) | 33.33 (66.67) | 0 (33.33) | 0 (66.67) | 0.2 |
| Mental health | 60 (8) | 64 (12) | 60 (16) | 64 (12) | 0.623 |
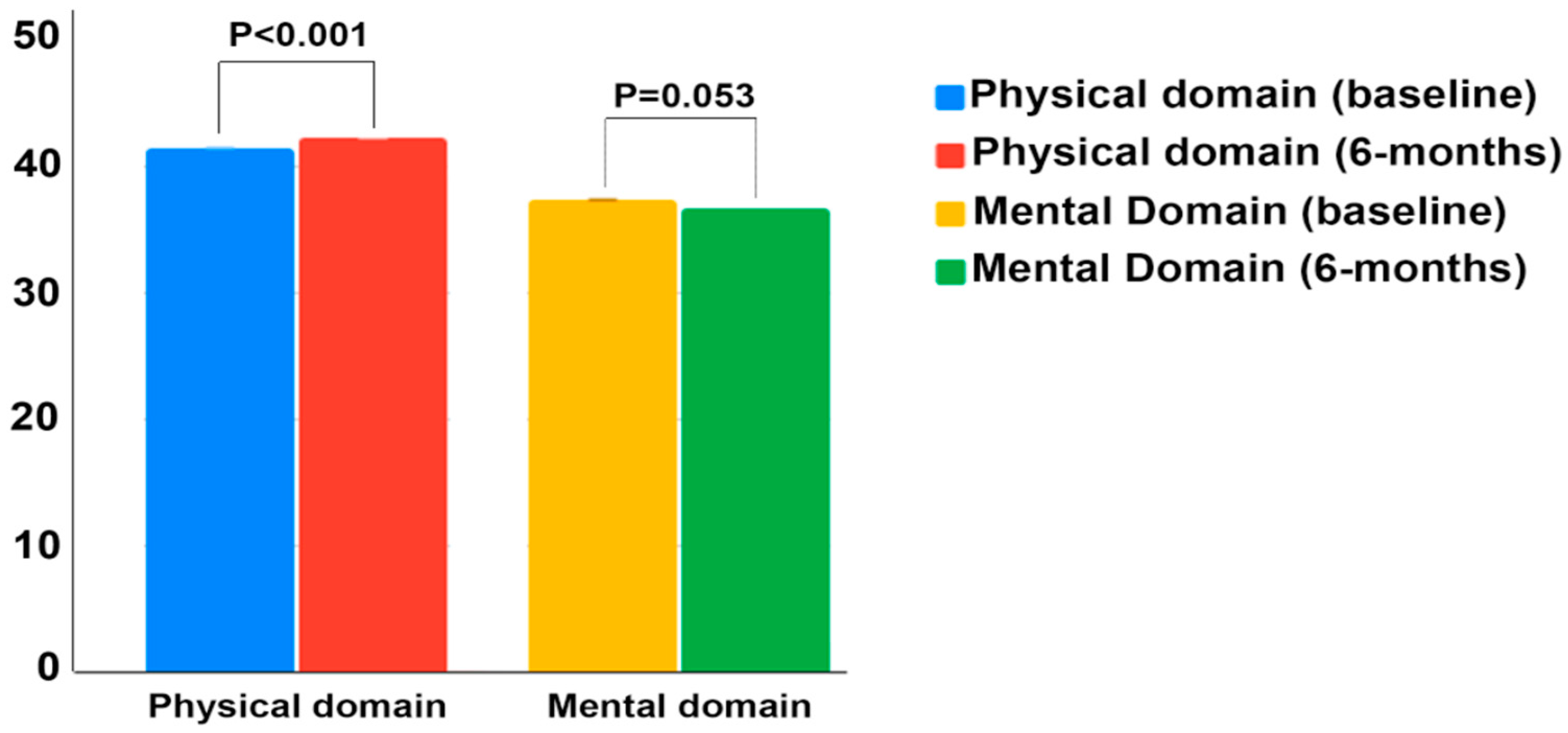
| SF-36 Summary Scores | Anorexia Nervosa (n = 59) | Bulimia Nervosa (n = 35) | Other Specified Feeding or Eating Disorder (n = 19) | Binge Eating Disorder (n = 11) | |
|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | p-Value * | |
| Baseline | |||||
| Physical domain | 43.44 (8.69) | 40.6 (6.38) | 41.96 (9.79) | 33.94 (8.32) | 0.045 1 |
| Mental Domain | 35.32 (7.48) | 39.51 (9.51) | 36.12 (10.72) | 41.86 (8.5) | 0.02 2 |
| 6-month follow-up | |||||
| Physical domain | 44.56 (8.3) (p = 0.004) | 41.02 (6.76) (p = 0.039) | 41.77 (9.22) | 35.92 (6.99) (p = 0.043) | 0.001 3 |
| Mental Domain | 35.04 (7.55) | 37.93 (8.36) | 37.37 (8.38) | 41.46 (6.89) | 0.006 4 |
| Items | Total Sample N (%) | Anorexia Nervosa (n = 59) N (%) | Bulimia Nervosa (n = 35) N (%) | Other Specified Feeding or Eating Disorder (n = 19) N (%) | Binge Eating Disorder (n = 11) N (%) | p-Value a | |
|---|---|---|---|---|---|---|---|
| Mobility (baseline) | I have no problems walking about | 107 (86.3%) | 57 (96.6%) | 28 (80%) | 17 (89.5%) | 5 (45.50%) | <0.001 |
| I have some problems walking about | 17 (13.7%) | 2 (3.4%) | 7 (7%) | 2 (10.5%) | 6 (54.50%) | ||
| I am confined to bed | 0 (0%) | 0 (0.0%) | 0 (0%) | 0 (0%) | 0 (0.00%) | ||
| Mobility (6-months) | I have no problems walking about | 112 (93.3%) | 56 (98.2% | 32 (94.1%) | 17 (94.4%) | 7 (63.6%) | 0.001 |
| I have some problems walking about | 7 (5.8%) | 0 (0%) | 2 (5.9%) | 1 (5.6%) | 4 (36.4%) | ||
| I am confined to bed | 1 (0.8%) | 1 (1.8%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| p-value b | 0.059 | 1 | 0.025 | 0.564 | 0.317 | ||
| Self-care (baseline) | I have no problems with self-care | 120 (96.8%) | 58 (98.3%) | 35 (100%) | 19 (100%) | 8 (72.70%) | <0.001 |
| I have some problems with self-care | 4 (3.20%) | 1 (1.7%) | 0 (0%) | 0 (0%) | 3 (27.30%) | ||
| I am unable to wash or dress myself | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0.00%) | ||
| Self-care (6-months) | I have no problems with self-care | 116 (96.7%) | 55 (96.5%) | 34 (100%) | 17 (94.4%) | 10 (90.9%) | 0.460 |
| I have some problems with self-care | 4 (3.3%) | 3 (3.5%) | 0 (0%) | 1 (5.6%) | 1 (9.1%) | ||
| I am unable to wash or dress myself | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| p-value b | 1 | 0.564 | N/A | 0.317 | 0.317 | ||
| Activity (baseline) | I have no problems with performing my usual activities | 95 (76.6%) | 52 (88.1%) | 25 (71.4%) | 15 (78.9%) | 3 (27.3%) | 0.001 |
| I have some problems with performing my usual activities | 25 (20.2%) | 6 (10.2%) | 9 (25.7%) | 4 (21.1%) | 6 (54.6%) | ||
| I am unable to perform my usual activities | 4 (3.2%) | 1 (1.7%) | 1 (2.9%) | 0 (0%) | 2 (18.2%) | ||
| Activity (6-months) | I have no problems with performing my usual activities | 96 (80%) | 47 (82.5%) | 30 (88.2%) | 13 (72.2%) | 6 (54.5%) | 0.079 |
| I have some problems with performing my usual activities | 24 (20%) | 10 (17.5%) | 4 (11.8%) | 5 (27.8%) | 5 (45.5%) | ||
| I am unable to perform my usual activities | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (%) | ||
| p-value b | 0.206 | 0.439 | 0.071 | 0.665 | 0.025 | ||
| Pain (baseline) | I have no pain or discomfort | 84 (67.7%) | 45 (76.3%) | 22 (62.9%) | 12 (63.2%) | 5 (45.50%) | 0.483 |
| I have moderate pain or discomfort | 33 (26.6%) | 12 (20.3%) | 10 (28.6%) | 6 (31.6%) | 5 (45.50%) | ||
| I have extreme pain or discomfort | 7 (5.6%) | 2 (3.4%) | 3 (9.6%) | 1 (5.3%) | 1 (9.10%) | ||
| Pain (6-months) | I have no pain or discomfort | 76 (63.3%) | 42 (73.7%) | 17 (50.0%) | 12 (66.7%) | 5 (45.5%) | 0.088 |
| I have moderate pain or discomfort | 39 (32.5%) | 12 (21.1%) | 17 (50.0%) | 5 (27.8%) | 5 (45.5%) | ||
| I have extreme pain or discomfort | 5 (4.2%) | 3 (5.3%) | 0 (0%) | 1 (5.6%) | 1 (9.1%) | ||
| p-value b | 0.522 | 0.353 | 0.827 | 0.705 | 1 | ||
| Anxiety (baseline) | I am not anxious or depressed | 44 (35.5%) | 16 (27.1%) | 19 (54.3%) | 5 (26.3%) | 4 (36.40%) | 0.122 |
| I am moderately anxious or depressed | 55 (44.4%) | 32 (54.2%) | 11 (31.4%) | 8 (42.1%) | 4 (36.40%) | ||
| I am extremely anxious or depressed | 25 (20.2%) | 11 (18.6%) | 5 (14.3%) | 6 (31.6%) | 3 (27.30%) | ||
| Anxiety (6-months) | I am not anxious or depressed | 49 (40.8%) | 25 (43.9%) | 13 (38.2%) | 6 (33.3%) | 5 (45.5%) | 0.047 |
| I am moderately anxious or depressed | 41 (34.2%) | 21 (36.8%) | 15 (44.1%) | 2 (11.1%) | 3 (27.3%) | ||
| I am extremely anxious or depressed | 30 (25%) | 11 (19.3%) | 6 (17.6%) | 10 (55.6%) | 3 (27.3%) | ||
| p-value b | 0.927 | 0.327 | 0.223 | 0.637 | 0.808 |
| Total Sample | Anorexia Nervosa (n = 59) | Bulimia Nervosa (n = 35) | Other Specified Feeding or Eating Disorder (n = 19) | Binge Eating Disorder (n = 11) | p-Value a | |
|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | ||
| EQ-VAS (baseline) | 79.89 (35.46) | 79.86 (26.1) | 79.86 (35.46) | 79.86 (32.27) | 64.54 (46.75) | 0.103 |
| EQ-VAS (6-months follow-up) | 79.44 (46.45) | 79.86 (26.1) | 79.02 (11.47) | 53.55 (31.82) | 79.02 (66.89) | 0.146 |
| p-value b | 0.560 | 0.941 | 0.351 | 0.264 | 0.314 | |
| EQ-Index (baseline) | 0.914 (0.29) | 0.914 (0.175) | 0.914 (0.29) | 0.914 (0.462) | 0.71 (0.639) | 0.095 |
| EQ-Index (6-months follow-up) | 0.901 (0.469) | 0.914 (0.175) | 0.887 (0.16) | 0.541 (0.444) | 0.887 (0.725) | 0.143 |
| p-value b | 0.599 | 0.786 | 0.799 | 0.223 | 0.374 |
| Subscale | Total Sample Mean (SD) | Anorexia Nervosa (n = 59) Median (IQR) | Bulimia Nervosa (n = 35) Median (IQR) | Other Specified Feeding or Eating Disorder (n = 19) Median (IQR) | “Binge Eating Disorder (n = 11)” Median (IQR) | p-Value a |
|---|---|---|---|---|---|---|
| Precontemplation (baseline) | 21 (7) | 22 (6) | 20 (7) | 21 (5) | 19 (11) | 0.590 |
| Precontemplation (6-months follow-up) | 20.5 (7) | 19.5 (8.5) | 22 (6) | 19 (7.5) | 20 (5) | |
| p-value b | 0.384 | 0.251 | 0.269 | 0.271 | 0.953 | |
| Contemplation (baseline) | 23.6 (4.1) | 23.6 (3.63) | 22.7 (6.3) | 24.5 (3.6) | 24.5 (10.9) | 0.492 |
| Contemplation (6-months follow-up) | 24 (6) | 24 (4.5) | 24 (4) | 19.5 (9.5) | 21 (7) | |
| p-value b | 0.217 | 0.877 | 0.976 | 0.133 | 0.407 | |
| Preparation (baseline) | 26.3 (7.2) | 27.2 (6.3) | 25.4 (6.3) | 26.3 (7.2) | 27.2 (7.2) | 0.888 |
| Preparation (6-months follow-up) | 25 (5) | 25 (5) | 24 (4) | 23 (75) | 24 (6) | |
| p-value b | 0.001 | 0.122 | 0.021 | 0.066 | 0.374 | |
| Action (baseline) | 25 (9) | 24 (9) | 26 (9) | 23 (7) | 26 (8) | 0.680 |
| Action (6-months follow-up) | 24 (5.5) | 24.5 (6.5) | 23 (5) | 25 (5) | 23 (7) | |
| p-value b | 0.122 | 0.092 | 0.122 | 0.209 | 0.593 | |
| Maintenance (baseline) | 10.5 (8) | 9 (7) | 11 (8) | 12 (8) | 13 (11) | 0.006 1 |
| Maintenance (follow-up) | 15 (9) | 15 (9.5) | 14 (8) | 16 (14) | 14 (7) | |
| p-value b | 0.013 | 0.119 | 0.148 | 0.127 | 0.953 | |
| Relapse (baseline) | 22.8 (12.1) | 22.85 (10) | 20 (15.7) | 27.1 (11.4) | 22.8 (24.2) | 0.190 |
| Relapse (follow-up) | 23 (7) | 23 (4) | 23 (7) | 21.5 (12) | 20 (8) | |
| p-value b | 0.314 | 0.794 | 0.988 | 0.013 | 0.635 |
| Total Sample Median (IQR) | Anorexia Nervosa (n = 59) Median (IQR) | Median (IQR) | Other Specified Feeding or Eating Disorder (n = 19) Median (IQR) | “Binge Eating Disorder (n = 11)” Median (IQR) | p-Value a | |
|---|---|---|---|---|---|---|
| EAT score (baseline) | 52 (30) | 59 (11) | 37 (39) | 50 (29) | 17 (39) | p < 0.001 1 |
| EAT score (6-month follow-up) | 47 (30) | 54 (31) | 38 (27) | 51 (21) | 29 (35) | 0.088 |
| p-value b | 0.022 | 0.002 | 0.650 | 0.513 | 0.260 |
| Total Sample | Anorexia Nervosa (n = 59) | Bulimia Nervosa (n = 35) | Eating Disorder Not Otherwise Specified (n = 19) | Binge Eating Disorder (n = 11) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Explained Variance | Significant Predictors | Explained Variance | Significant Predictors | Significant Predictors | Significant Predictors | Explained Variance | Significant Predictors | ||
| Physical domain | R2 = 0.413 | EQ-5D index (baseline): B = 7.139 (1.981); p = 0.001 | R2 = 0.315 | EQ-5D index (baseline): B = 15.231 (3.798): p < 0.001 | No significant predictors detected. | No significant predictors detected. | R2 = 0.738 | EQ-5D (VAS) (baseline): B = 14.266 (3.214): p = 0.003 | |
| BMI (follow-up): B = −0.213 (0.062): p = 0.001 | |||||||||
| ACTA (action) (follow-up): B = −0.247 (0.077): p = 0.02 | |||||||||
| OCT (baseline): B = 4.619 (1.581): p = 0.005 | |||||||||
| Mental domain | R2 = 0.220 | EAT26 (baseline): B = −0.131 (0.033): p < 0.001 | R2 = 0.270 | EAT26 (baseline): B = −0.199 (0.055): p = 0.001 | R2 = 0.412 | EQ-5D (VAS) (baseline): B = 15.905 (4.149): p = 0.001 | No significant predictors detected. | R2 = 0.805 | Age: B = 0.521 (0.097): p = 0.001 |
| EQ-5D (VAS) (baseline): B = 7.233 (2.647): p = 0.008 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panea-Pizarro, I.; Moran, J.M.; Lavado-García, J.; Beato-Fernández, L.; Domínguez-Martin, A.T.; Huerta-González, S.; Novo, A.; Pedrera-Zamorano, J.D.; López-Espuela, F. Health-Related Quality of Life in Spanish Women with Eating Disorders. Nutrients 2021, 13, 403. https://doi.org/10.3390/nu13020403
Panea-Pizarro I, Moran JM, Lavado-García J, Beato-Fernández L, Domínguez-Martin AT, Huerta-González S, Novo A, Pedrera-Zamorano JD, López-Espuela F. Health-Related Quality of Life in Spanish Women with Eating Disorders. Nutrients. 2021; 13(2):403. https://doi.org/10.3390/nu13020403
Chicago/Turabian StylePanea-Pizarro, Isabel, José M. Moran, Jesús Lavado-García, Luis Beato-Fernández, Ana Teresa Domínguez-Martin, Sara Huerta-González, Andre Novo, Juan D. Pedrera-Zamorano, and Fidel López-Espuela. 2021. "Health-Related Quality of Life in Spanish Women with Eating Disorders" Nutrients 13, no. 2: 403. https://doi.org/10.3390/nu13020403
APA StylePanea-Pizarro, I., Moran, J. M., Lavado-García, J., Beato-Fernández, L., Domínguez-Martin, A. T., Huerta-González, S., Novo, A., Pedrera-Zamorano, J. D., & López-Espuela, F. (2021). Health-Related Quality of Life in Spanish Women with Eating Disorders. Nutrients, 13(2), 403. https://doi.org/10.3390/nu13020403







