Associations of Health Literacy with Blood Pressure and Dietary Salt Intake among Adults: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
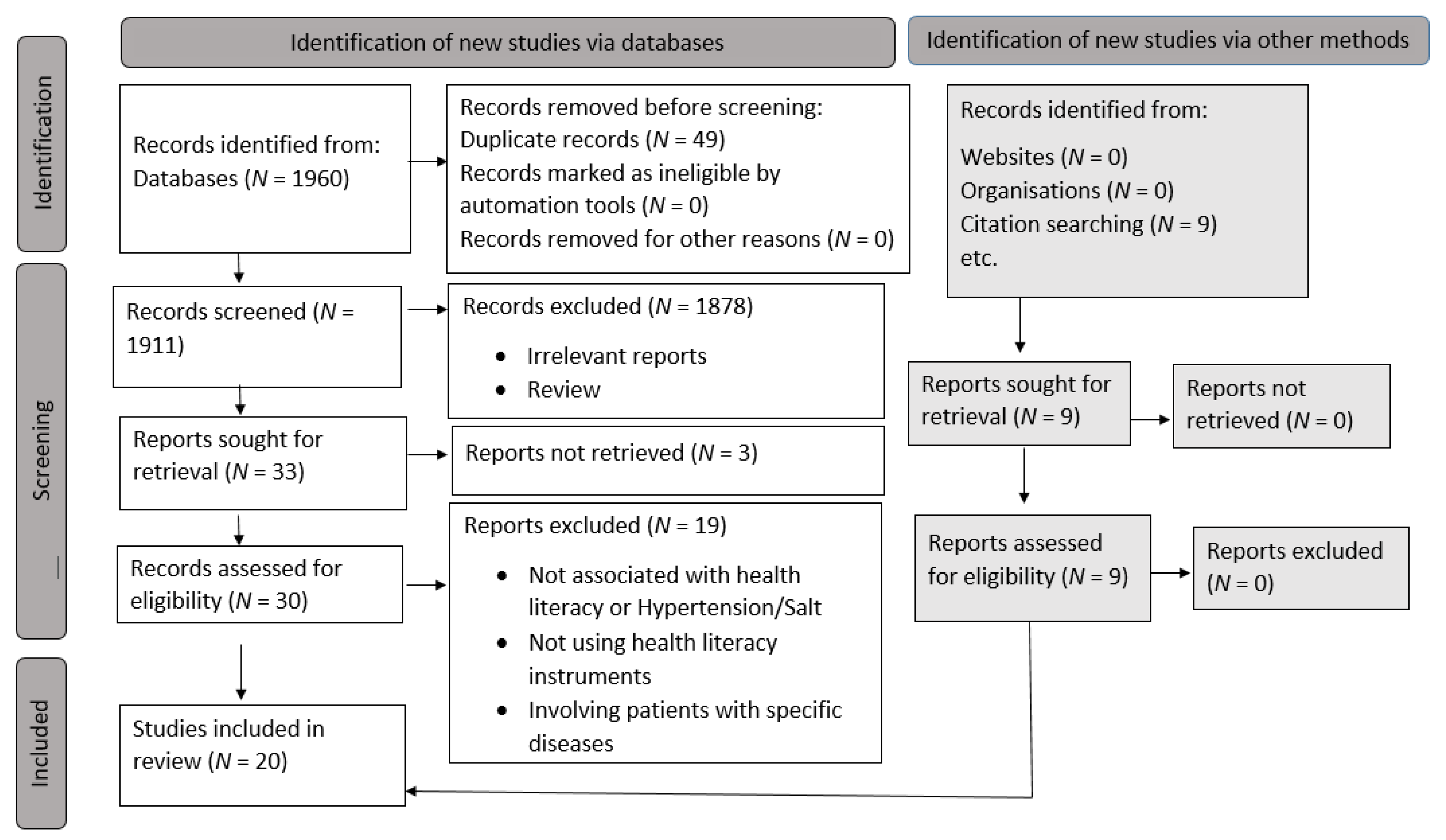
2.4. Selection Process
2.5. Data Collection Process
2.6. Data Items
2.7. Study Risk of Bias Assessment
2.8. Outcome Measures
2.9. Synthesis Methods
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality Assessment
3.4. Health Literacy Status
3.5. Health Literacy and Outcomes
3.5.1. Health Literacy and Blood Pressure (Blood Pressure Control and Knowledge)
3.5.2. Health Literacy and Salt Intake (Low Salt Diet Adherence, 24 h Urine, and Health Literacy Sodium on Sodium Restriction)
3.6. Health Literacy Domains
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benziger, C.P.; Roth, G.A.; Moran, A.E. The Global Burden of Disease Study and the Preventable Burden of NCD. Glob. Heart 2016, 11, 393–397. [Google Scholar] [CrossRef]
- World Health Organization. Cardiovascular Diseases. Available online: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (accessed on 15 November 2021).
- Luta, X.; Hayoz, S.; Gréa Krause, C.; Sommerhalder, K.; Roos, E.; Strazzullo, P.; Beer-Borst, S. The Relationship of Health/Food Literacy and Salt Awareness to Daily Sodium and Potassium Intake among a Workplace Population in Switzerland. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global Burden of Hypertension: Analysis of Worldwide Data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Department of Statistics Malaysia. Statistics on Causes of Death, Malaysia, 2020. Available online: https://www.dosm.gov.my/v1/index.php?r=column/cthemeByCat&cat=401&bul_id=QTU5T0dKQ1g4MHYxd3ZpMzhEMzdRdz09&menu_id=L0pheU43NWJwRWVSZklWdzQ4TlhUUT09 (accessed on 13 September 2021).
- Institute for Public Health 2020. National Health and Morbidity Survey (NHMS) 2019: Non-communicable Diseases, Healthcare Demand, and Health Literacy—Key Findings. Available online: https://iptk.moh.gov.my/images/technical_report/2020/4_Infographic_Booklet_NHMS_2019_-_English.pdf (accessed on 15 November 2021).
- McNicoll, G. World Health Report 2002: Reducing Risks, Promoting Healthy Life. (Short Reviews). Popul. Dev. Rev. 2003, 29, 137–140. [Google Scholar]
- Wang, G.; Labarthe, D. The Cost-Effectiveness of Interventions Designed to Reduce Sodium Intake. J. Hypertens. 2011, 29, 1693–1699. [Google Scholar] [CrossRef]
- He, F.J.; Tan, M.; Ma, Y.; MacGregor, G.A. Salt Reduction to Prevent Hypertension and Cardiovascular Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 632–647. [Google Scholar] [CrossRef]
- He, F.J.; Pombo-Rodrigues, S.; MacGregor, G.A. Salt Reduction in England from 2003 to 2011: Its Relationship to Blood Pressure, Stroke and Ischaemic Heart Disease Mortality. BMJ Open 2014, 4, 004549. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.A.; Tekle, D.; Rosewarne, E.; Flexner, N.; Cobb, L.; Al-Jawaldeh, A.; Kim, W.J.; Breda, J.; Whiting, S.; Campbell, N.; et al. A Systematic Review of Salt Reduction Initiatives around the World: A Midterm Evaluation of Progress towards the 2025 Global Non-Communicable Diseases Salt Reduction Target. Adv. Nutr. 2021, 12, 1768–1780. [Google Scholar] [CrossRef]
- Trieu, K.; Neal, B.; Hawkes, C.; Dunford, E.; Campbell, N.; Rodriguez-Fernandez, R.; Legetic, B.; McLaren, L.; Barberio, A.; Webster, J. Salt Reduction Initiatives around the World—A Systematic Review of Progress towards the Global Target. PLoS ONE 2015, 10, 0130247. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.K.; Shahar, S.; You, Y.X.; Michael, V.; Majid, H.A.; Manaf, Z.A.; Haron, H.; Sukiman, N.S.; Chia, Y.C.; He, F.J.; et al. Developing a Policy to Reduce the Salt Content of Food Consumed Outside the Home in Malaysia: Protocol of a Qualitative Study. BMJ Open 2021, 11, e044628. [Google Scholar] [CrossRef]
- Sørensen, K.; Van Den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health Literacy and Public Health: A Systematic Review and Integration of Definitions and Models. BMC Genom. 2003, 4, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D. Health Literacy as a Public Health Goal: A Challenge for Contemporary Health Education and Communication Strategies into the 21st Century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Ishikawa, H.; Yano, E. Patient Health Literacy and Participation in the Health-Care Process. Health Expect. 2008, 11, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, S.L.; Halpern, D.J.; Viera, A.J.; Berkman, N.D.; Donahue, K.E.; Crotty, K. Interventions for Individuals with Low Health Literacy: A Systematic Review. J. Health Commun. 2011, 16, 30–54. [Google Scholar] [CrossRef] [PubMed]
- Peerson, A.; Saunders, M. Health Literacy Revisited: What Do We Mean and Why Does It Matter? Health Promot. Int. 2009, 24, 285–296. [Google Scholar] [CrossRef]
- Pleasant, A. Advancing Health Literacy Measurement: A Pathway to Better Health and Health System Performance. J. Health Commun. 2014, 19, 1481–1496. [Google Scholar] [CrossRef]
- Du, S.; Zhou, Y.; Fu, C.; Wang, Y.; Du, X.; Xie, R. Health Literacy and Health Outcomes in Hypertension: An Integrative Review. Int. J. Nurs. Sci. 2018, 5, 301–309. [Google Scholar] [CrossRef]
- Pleasant, A.; Cabe, J.; Patel, K.; Cosenza, J.; Carmona, R. Health Literacy Research and Practice: A Needed Paradigm Shift. Health Commun. 2015, 30, 1176–1180. [Google Scholar] [CrossRef] [PubMed]
- Halladay, J.R.; Donahue, K.E.; Cené, C.W.; Li, Q.; Cummings, D.M.; Hinderliter, A.L.; Miller, C.L.; Garcia, B.A.; Little, E.; Rachide, M.; et al. The Association of Health Literacy and Blood Pressure Reduction in a Cohort of Patients with Hypertension: The Heart Healthy Lenoir Trial. Patient Educ. Couns. 2017, 100, 542–549. [Google Scholar] [CrossRef]
- Shi, D.; Li, J.; Wang, Y.; Wang, S.; Liu, K.; Shi, R.; Zhang, Q.; Chen, X. Association between Health Literacy and Hypertension Management in a Chinese Community: A Retrospective Cohort Study. Intern. Emerg. Med. 2017, 12, 765–776. [Google Scholar] [CrossRef]
- Delavar, F.; Pashaeypoor, S.; Negarandeh, R. The Effects of Self-Management Education Tailored to Health Literacy on Medication Adherence and Blood Pressure Control among Elderly People with Primary Hypertension: A Randomized Controlled Trial. Patient Educ. Couns. 2020, 103, 336–342. [Google Scholar] [CrossRef]
- Gaffari-Fam, S.; Babazadeh, T.; Oliaei, S.; Behboodi, L.; Daemi, A. Adherence to a Health Literacy and Healthy Lifestyle with Improved Blood Pressure Control in Iran. Patient Prefer. Adherence 2020, 14, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Santos Costa, V.R.; Rezende Costa, P.D.; Nakano, E.Y.; Apolinario, D.; Cruz Santana, A.N. Functional Health Literacy in Hypertensive Elders at Primary Health Care. Rev. Bras. Enferm. 2019, 72, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Borges, F.M.; Silva, A.R.; Lima, L.H.; Almeida, P.C.; Vieira, N.F.; Machado, A.L. Health Literacy of Adults with and without Arterial Hypertension. Rev. Bras. Enferm. 2019, 72, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Selcuk, K.T.; Mercan, Y.; Aydin, T.; Selçuk, K.T.; Mercan, Y.; Aydın, T. Uncontrolled Blood Pressure in Patients with Hypertension and Associated Factors: The Role of Low Health Literacy. Erciyes Med. J. 2018, 40, 222–227. [Google Scholar] [CrossRef]
- Hu, K.; Wu, S.; Sun, K.; Zhang, X.; He, C.; Zhao, Y.; Li, Z.; Sun, X. Health Literacy and Its Association with Medication Adherence and Blood Pressure Control among Patients with Hypertension. J. Am. Coll. Cardiol. 2017, 70, C85. [Google Scholar] [CrossRef]
- Yilmazel, G.; Çetinkaya, F. Relation between Health Literacy Levels, Hypertension Awareness and Control among Primary-Secondary School Teachers in Turkey. AIMS Public Health 2017, 4, 314–325. [Google Scholar] [CrossRef]
- Hall, E.; Lee, S.-Y.; Clark, P.C.; Perilla, J. Social Ecology of Adherence to Hypertension Treatment in Latino Migrant and Seasonal Farmworkers. J. Transcult. Nurs. 2016, 27, 33–41. [Google Scholar] [CrossRef]
- Termsirikulchai, L.; Wannasirikul, P.; Sujirarat, D.; Benjakul, S.; Tanasugarn, C. Medication Adherence Of Hypertensive Older Adults Health Literacy, Medication Adherence, and Blood Pressure Level Among Hypertensive Older Adults Treated at Primary Health Care Centers. Southeast Asian J. Trop. Med. 2016, 47, 109. [Google Scholar]
- Glashen, M.R. Health Literacy and Hypertension Levels in Urban Latinos; Walden University: Ann Arbor, MI, USA, 2015. [Google Scholar]
- McNaughton, C.D.; Kripalani, S.; Cawthon, C.; Mion, L.C.; Wallston, K.A.; Roumie, C.L. Association of Health Literacy with Elevated Blood Pressure a Cohort Study of Hospitalized Patients. Med. Care 2014, 52, 346–353. [Google Scholar] [CrossRef]
- McNaughton, C.D.; Jacobson, T.A.; Kripalani, S. Low Literacy Is Associated with Uncontrolled Blood Pressure in Primary Care Patients with Hypertension and Heart Disease. Patient Educ. Couns. 2014, 96, 165–170. [Google Scholar] [CrossRef]
- Ko, Y.; Balasubramanian, T.D.; Wong, L.; Tan, M.L.; Lee, E.; Tang, W.E.; Chan, S.C.; Tan, A.S.L.; Toh, M.P.H.S. Health Literacy and Its Association with Disease Knowledge and Control in Patients with Hypertension in Singapore. Int. J. Cardiol. 2013, 168, e116–e117. [Google Scholar] [CrossRef]
- Willens, D.E.; Kripalani, S.; Schildcrout, J.S.; Cawthon, C.; Wallston, K.; Mion, L.C.; Davis, C.; Danciu, I.; Rothman, R.L.; Roumie, C.L. Association of Brief Health Literacy Screening and Blood Pressure in Primary Care. J. Health Commun. 2013, 18, 129–142. [Google Scholar] [CrossRef]
- Aboumatar, H.J.; Carson, K.A.; Beach, M.C.; Roter, D.L.; Cooper, L.A. The Impact of Health Literacy on Desire for Participation in Healthcare, Medical Visit Communication, and Patient Reported Outcomes among Patients with Hypertension. J. Gen. Intern. Med. 2013, 28, 1469–1476. [Google Scholar] [CrossRef] [PubMed]
- Lenahan, J.L.; McCarthy, D.M.; Davis, T.C.; Curtis, L.M.; Serper, M.; Wolf, M.S. A Drug by Any Other Name: Patients’ Ability to Identify Medication Regimens and Its Association with Adherence and Health Outcomes. J. Health Commun. 2013, 18, 31–39. [Google Scholar] [CrossRef]
- Shibuya, A.; Inoue, R.; Ohkubo, T.; Takeda, Y.; Teshima, T.; Imai, Y.; Kondo, Y. The Relation between Health Literacy, Hypertension Knowledge, and Blood Pressure among Middle-Aged Japanese Adults. Blood Press. Monit. 2011, 16, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Suon, M.; Ruaisungnoen, W. Health Literacy on Sodium Restriction and Associated Factors among Patients with Hypertension in Phnom Penh, Cambodia. Nurs. Sci. J. Thail. 2019, 37, 32–41. [Google Scholar]
- Hutchison, J.; Warren-Findlow, J.; Dulin, M.; System, H.; Tapp, H.; Kuhn, L. The Association between Health Literacy and Diet Adherence among Primary Care Patients with Hypertension. J. Health Disparities Res. Pract. 2014, 7, 7. [Google Scholar]
- Jiang, S.Z.; Lu, W.; Zong, X.F.; Ruan, H.Y.; Liu, Y. Obesity and Hypertension. Exp. Ther. Med. 2016, 12, 2395. [Google Scholar] [CrossRef]
- Poulter, N.R.; Borghi, C.; Parati, G.; Pathak, A.; Toli, D.; Williams, B.; Schmieder, R.E. Medication Adherence in Hypertension. J. Hypertens. 2020, 38, 579–587. [Google Scholar] [CrossRef]
- Beilin, L.J. Lifestyle and Hypertension--an Overview. Clin. Exp. Hypertens. 1999, 21, 749–762. [Google Scholar] [CrossRef] [PubMed]
- Levy, H.; Janke, A. Health Literacy and Access to Care. J. Health Commun. 2016, 21, 43–50. [Google Scholar] [CrossRef]
- Amann, J.; Rubinelli, S.; Kreps, G.L. Revisiting the Concept of Health Literacy. The Patient as Information Seeker and Provider. Eur. J. Health Psychol. 2015, 17, 286–290. [Google Scholar]
- Cline, R.J.; Haynes, K.M. Consumer Health Information Seeking on the Internet: The State of the Art. Health Educ. Res. 2001, 16, 671–692. [Google Scholar] [CrossRef]
- Temple, N.J.; Fraser, J. Food Labels: A Critical Assessment. Nutrition 2014, 30, 257–260. [Google Scholar] [CrossRef]
- Aldoory, L. The Status of Health Literacy Research in Health Communication and Opportunities for Future Scholarship. Health Commun. 2017, 32, 211–218. [Google Scholar] [CrossRef]
- Diviani, N. On the Centrality of Information Appraisal in Health Literacy Research. HLRP Health Lit. Res. Pract. 2019, 3, e21–e24. [Google Scholar] [CrossRef][Green Version]
- McLean, R.M. Measuring Population Sodium Intake: A Review of Methods. Nutrients 2014, 6, 4651–4662. [Google Scholar] [CrossRef] [PubMed]
- Wielgosz, A.; Robinson, C.; Mao, Y.; Jiang, Y.; Campbell, N.R.; Muthuri, S.; Morrison, H. The Impact of Using Different Methods to Assess Completeness of 24-Hour Urine Collection on Estimating Dietary Sodium. J. Clin. Hypertens. 2016, 18, 581–584. [Google Scholar] [CrossRef]
- Land, M.A.; Webster, J.; Christoforou, A.; Praveen, D.; Jeffrey, P.; Chalmers, J.; Smith, W.; Woodward, M.; Barzi, F.; Nowson, C.; et al. Salt Intake Assessed by 24 h Urinary Sodium Excretion in a Random and Opportunistic Sample in Australia. BMJ Open 2014, 4, 003720. [Google Scholar] [CrossRef] [PubMed]
- Van Dam, R.M.; Hunter, D. Biochemical Indicators of Dietary Intake. Nutr. Epidemiol. 2012, 3, 150–154. [Google Scholar] [CrossRef]
- Public Health Guideline. Overview | Cardiovascular Disease Prevention Guidance. Available online: https://www.nice.org.uk/guidance/ph25 (accessed on 28 December 2020).
- Denton, D.; Weisinger, R.; Mundy, N.I.; Wickings, E.J.; Dixson, A.; Moisson, P.; Pingard, A.M.; Shade, R.; Carey, D.; Ardaillou, R.; et al. The Effect of Increased Salt Intake on Blood Pressure of Chimpanzees. Nat. Med. 1995, 1, 1009–1016. [Google Scholar] [CrossRef]
- He, F.J.; MacGregor, G.A. Effect of Modest Salt Reduction on Blood Pressure: A Meta-Analysis of Randomized Trials. Implications for Public Health. J. Hum. Hypertens. 2002, 16, 761–770. [Google Scholar] [CrossRef]
- Rose, G.; Stamler, J.; Stamler, R.; Elliott, P.; Marmot, M.; Pyorala, K.; Kesteloot, H.; Joossens, J.; Hansson, L.; Mancia, G.; et al. Intersalt: An International Study of Electrolyte Excretion and Blood Pressure. Results for 24 Hour Urinary Sodium and Potassium Excretion. Br. Med. J. 1988, 297, 319–328. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Thakur, J.S.; Singh, A. Knowledge Attitude, and Practice Regarding Dietary Salt Intake among Urban Slum Population of North India. J. Fam. Med. Prim. Care 2018, 7, 526. [Google Scholar] [CrossRef] [PubMed]
- Jessen, N.; Santos, A.; Damasceno, A.; Silva-Matos, C.; Severo, M.; Padrão, P.; Lunet, N. Knowledge and Behaviors Regarding Salt Intake in Mozambique. Eur. J. Clin. Nutr. 2018, 72, 1690–1699. [Google Scholar] [CrossRef]
- Ko, Y.J.; Karanicolas, P.J. Hepatic Arterial Infusion Pump Chemotherapy for Colorectal Liver Metastases: An Old Technology in a New Era. Curr. Oncol. 2014, 21, e116–e121. [Google Scholar] [CrossRef]
- Osborn, C.Y.; Paasche-Orlow, M.K.; Bailey, S.C.; Wolf, M.S. The Mechanisms Linking Health Literacy to Behavior and Health Status. Am. J. Health Behav. 2011, 35, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Gazmararian, J.A.; Williams, M.V.; Peel, J.; Baker, D.W. Health Literacy and Knowledge of Chronic Disease. Patient Educ. Couns. 2003, 51, 267–275. [Google Scholar] [CrossRef]
- Williams, M.V.; Baker, D.W.; Parker, R.M.; Nurss, J.R. Relationship of Functional Health Literacy to Patients’ Knowledge of Their Chronic Disease: A Study of Patients with Hypertension and Diabetes. Arch. Intern. Med. 1998, 158, 166–172. [Google Scholar] [CrossRef]
- White, R.O.; Wolff, K.; Cavanaugh, K.L.; Rothman, R. Addressing Health Literacy and Numeracy to Improve Diabetes Education and Care. Diabetes Spectr. 2010, 23, 238–243. [Google Scholar] [CrossRef] [PubMed]
| Criteria | Description |
|---|---|
| Participants | Adults aged ≥18 years, including those with the hypertensive condition. Animal studies and individuals with other specific diseases were excluded |
| Intervention/Exposure | Health literacy |
| Comparison | High vs low health literacy in relation to the outcomes (blood pressure and dietary salt intake) either by mean scores, quartiles, or cut-off values such as limited, adequate, marginal, and excellent health literacy |
| Outcomes | Dietary salt intake and blood pressure using validated measurements and protocol |
| Study Design | Randomised controlled trial (RCT), non-RCT, cohort, and cross-sectional studies |
| Concept 1 | AND | Concept 2 |
| Health Literacy OR Literacy OR Numeracy | Salt OR Salty OR Sodium Blood Pressure OR Hypertension |
| Author (Year) | Design | Instrument | Quality Score | Study Sample | Outcomes (Blood Pressure/Knowledge/Salt Intake) |
| Delavar et al., 2020 [24] | RCT (January–March 2018) | Health Literacy for Iranian Adults (HELIA) | Good | Through block randomization, 118 older adults with uncontrolled hypertension were allocated to a control or intervention group at random. Age more than 60 years old. | Blood pressure: After Health Literacy-tailored intervention, blood pressure among the intervention group is improved; nevertheless, there was no evident difference between the groups (p > 0.05). |
| Gaffari-fam et al., 2020 [25] | Cross-sectional | HELIA | Good | 210 hypertensive patients in Iran. Age more than 30 years (Mean age was 56.7 years) | Blood pressure: The health literacy dimensions contributed to a significant increase of 4.7% for the variance in high blood pressure. |
| Costa et al., 2019 [26] | Cross-sectional | The Short Assessment of Health Literacy for Portuguese-speaking Adults (18 items) SAHLPA-18 | Good | 392 hypertensive elderly patients. More than 60 years. | Blood pressure: Inadequate (high) blood pressure was linked to the following factor: inadequate functional health literacy. |
| Borges et al., 2019 [27] | Cross-sectional | Short Test of Functional Health Literacy in Adults (S-TOFHLA) | Good | 357 adults from basic health units in Brazil. Aged between 18 to 39 years | Blood pressure: There was a statistically significant decrease in associations evaluated (p < 0.05) when it came to hypertension and participants’ health literacy level. |
| Study, Year (References) | Design | Instrument | Quality Score | Study Sample | Outcomes (Blood Pressure/Knowledge/Salt Intake) |
| Selcuk et al., 2018 [28] | Cross-sectional | European Health Literacy Survey Questionnaire (HLS-EU-Q) | Good | 556 hypertensive patients in Turkey. Aged 18 years and above. Mean age was 55.74 ± 13.69 years (range 18–88) | Blood pressure: According to multivariate logistic regression analysis, health illiterate patients had higher uncontrolled blood pressure (OR: 2.06, 95% CI: 1.34–2.94). |
| # Halladay et al., 2017 [22] | Cohort | STOFHLA | Fair | 493 patients with uncontrolled hypertension in rural primary care, US. The mean age was 57 (min = 20, max = 92) years. | Blood pressure: There were statistically significant reductions in mean Systolic Blood Pressure (SBP) in both the low and high health literacy groups (6.6 and 5.3 mmHg, respectively) after a year, however, there was no significant difference between the groups (Δ 1.3 mmHg, p = 0.067). The low and high health literacy groups both reported lower blood pressure in 2 years by 8.1 and 4.6 mm Hg, respectively, with no significant between-group difference (Δ 3.5 mm Hg, p = 0.25). |
| Study, Year (References) | Design | Instrument | Quality Score | Study Sample | Outcomes (Blood Pressure/Knowledge/Salt Intake) |
| # Shi et al., 2017 [23] | Cohort | Chinese health literacy scale for hypertension (CHLSH) | Poor | 360 hypertensive patients in China. The age range of participants was 31–88 years. | Blood pressure: Low health literacy indicates high SBP. The rate of hypertension control increased as the CHLSH score increased (p < 0.001). The findings show that for three-quarters of the year, patients in the high literacy group have better SBP management than those in the low literacy group. |
| Hu et al., 2017 [29] | Cross-sectional | Health Literacy Scale for Hypertension | Good | 596 hypertensive patients in China | Blood pressure: Blood pressure control was linked to total health literacy (z = 2.493, p = 0.013), ability to comprehend pictures (z = 3.187, p = 0.001), and accessing health-related information (z = 3.274, p = 0.001). |
| Yilmazel and Centikaya, 2017 [30] | Cross-sectional | Newest Vital Sign Scale and Blood Pressure Concept Test (adapted from REALM) | Good | 500 volunteer teachers aged 35–49. The mean age of the study group was 42.91 ± 8.75 and in the hypertensive subjects, 48.35 ± 7.53. | Blood pressure: Health literacy was shown to be insignificant when it came to hypertension awareness and control.Knowledge: Those with hypertension who were aware of the disease had a higher health literacy level than those who were not (p > 0.05). |
| Study, Year (References) | Design | Instrument | Quality Score | Study Sample | Outcomes (Blood Pressure/Knowledge/Salt Intake) |
| Hall et al., 2016 [31] | Cross-sectional | SAHLSA (Short Assessment of Health Literacy for Spanish-Speaking Adults) | Good | 45 Latino Migrant and Seasonal Farmworkers. Ages ranged from 29 to 60 | Blood pressure: Higher levels of acculturation and health literacy were linked to improved blood pressure control (p = 0.01). |
| Wannasirikul et al., 2016 [32] | Cross-sectional | Adopted from Ishikawa et al. (2008) | Good | 600 aged 60 to 70 years with a mean age of 65.3 years for hypertensive patients in Primary Health Care Centres in Thailand | Blood pressure: Blood pressure is strongly linked with health literacy (β = −0.14, p < 0.05). |
| Glashen, 2015 [33] | Cross-sectional | STOFHLA | Good | 136 hypertensive Latino adults in the US aged 18 to 49 years | Blood pressure: Health literacy and hypertension association were not statistically significant (χ2 (1) = 0.811, p = 0.368). |
| McNaughton et al., 2014 [34] | Cross-sectional evaluation between 1 November 2010 and 30 April 2012 | Brief Health Literacy Screen (BHLS) | Good | 46,263 hospitalizations were available for analysis. Aged 18 years or older | Blood pressure: Low health literacy indicates extreme high blood pressure (aOR 1.08, 95% confidence CI 1.01, 1.16) and high blood pressure in people who had never been diagnosed with hypertension (OR 1.09, 95% CI 1.02, 1.16). Such associations were not found among patients with low health literacy and diagnosed hypertension. |
| McNaughton et al., 2014 [35] | Cross-sectional | The Rapid Estimate of Adult Literacy in Medicine (REALM) | Good | 423 urban hypertensive patients with coronary disease in the US | Blood pressure: Limited health literacy indicates uncontrolled blood pressure (OR 1.75, 95% CI 1.06–2.87). |
| Study, Year (References) | Design | Instrument | Quality Score | Study Sample | Outcomes (Blood Pressure/Knowledge/Salt Intake) |
| Ko et al., 2013 [36] | Cross-sectional | STOFHLA Singapore | Good | 306 hypertensive patients in the primary clinic in Singapore | Blood pressure: The degree of health literacy did not affect achieving the target blood pressure (p = 0.71). Knowledge: Higher health literacy level indicates higher hypertension knowledge scores (p < 0.001). |
| Willens et al., 2013 [37] | Cross-sectional | BHLS | Good | 10644 hypertensive patients aged more than 18 years | Blood pressure: Health literate patients had a slightly lower odds of having their hypertension under control. |
| Aboumatar et al., 2013 [38] | Cross-sectional | REALM | Good | 275 hypertensive patients in the US | Blood pressure: Patients with limited literacy reported poorer blood pressure management at the baseline. |
| Lenahan et al., 2013 [39] | Cross-sectional | TOFHLA | Good | 215 hypertensive patients in the United States with an average age of 60 years old (SD = 8.0 years) | Blood pressure: Uncontrolled blood pressure (p = 0.03) and medication identification (p = 0.001) were both associated with health literacy. |
| Shibuya et al., 2011 [40] | Cross-sectional | Chinese Health Literacy (CHL) | Good | 320 Middle-aged participants in an urban clinic, Japan (53 to 57 years) with an average age of 54.4 years old | Blood pressure: Limited health literacy and hypertension knowledge indicate poor health and raised blood pressure |
| Study, Year (References) | Design | Instrument | Quality Score | Study Sample | Outcomes (Blood Pressure/Knowledge/ Salt Intake) |
| Suon and Ruaisungnoen, 2019 [41] | Cross-sectional | Health Literacy Sodium Restriction (HL-SR) | Good | 317 hypertensive patients in Cambodia. Age (21–72 years old) with average age of 54 years (SD = 8.95) | Salt Intake: Literacy skills (β = 0.125, p = 0.019), knowledge of hypertension and sodium restriction (β = 0.266, p < 0.001), and health professional communication (β = 0.359, p < 0.001) were reported to be strongly associated to Health Literacy-Sodium Restriction. |
| Luta et al., 2018 [3] | Cross-sectional | European Health Literacy Survey Questionnaire 47-item (HLS-EU-Q47) | Good | 141 workplace population in Switzerland. Ages of 15 and 65 | Salt Intake: The health literacy index and food literacy score did not have a significant relationship with salt intake (24 h urine), however, the awareness variable “salt content impacts food/menu choice” did. |
| Hutchison et al., 2014 [42] | Cross-sectional | Newest Vital Sign | Good | 250 hypertensive patients in primary clinical care in the US. Age from 30 to 85 years (with an average age of 55 years). | Salt Intake: Adequate health literacy indicates a higher chance of adhering to the low salt plus diet (OR = 1.18, 95% CI: 0.50–2.79) than those with limited health literacy, but the results were not significant. |
| Studies/Domains | Selection | Comparability | Outcome | |||||
|---|---|---|---|---|---|---|---|---|
| Representativeness of the Sample | Sample Size | Non-Respondents: | Ascertainment of the Exposure (Risk Factor) | Comparability | Assessment of the Outcome | Statistical Test | Quality | |
| Willens et al., 2013 [37] | * | * | * | ** | ** | ** | * | Good (5 + 2 + 3) |
| McNaughton et al., 2014 [35] | * | * | * | ** | ** | * | * | Good (5 + 2 + 2) |
| Glashen, 2015 [33] | Good (5 + 2 + 2) | |||||||
| Gaffari-fam et al., 2020 [25] | * | * | * | ** | ** | * | * | Good (5 + 2 + 2) |
| Aboumatar et al., 2013 [38] | * | * | * | ** | * | * | * | Good (5 + 1 + 2) |
| Suon and Ruaisungnoen, 2019 [41] | * | * | * | ** | * | * | * | Good (5 + 1 + 2) |
| Yilmazel and Centikaya, 2017 [30] | * | * | * | ** | * | * | * | Good (5 + 1 + 2) |
| Lenahan et al., 2013 [39] | * | * | ** | ** | * | * | Good (4 + 2 + 2) | |
| Hutchison et al., 2014 [42] | * | * | ** | ** | * | * | Good (4 + 2 + 2) | |
| Luta et al., 2018 [3] | * | * | ** | ** | * | * | Good (4 + 2 + 2) | |
| Hall et al., 2016 [31] | * | * | ** | ** | * | * | Good (4 + 2 + 2) | |
| Hu et al., 2017 [29] | * | * | ** | ** | * | * | Good (4 + 2 + 2) | |
| Costa et al., 2019 [26] | * | * | ** | ** | * | * | Good (4 + 2 + 2) | |
| Selcuk et al., 2018 [28] | * | * | ** | * | * | * | Good (4 + 1 + 2) | |
| Borges et al., 2019 [27] | * | * | ** | * | * | * | Good (4 + 1 + 2) | |
| Wannasirikul et al., 2016 [32] | * | * | * | * | * | * | * | Good (4 + 1 + 2) |
| Ko et al., 2013 [36] | * | ** | ** | * | * | Good (3 + 2 + 2) | ||
| Shibuya et al., 2011 [40] | * | * | * | ** | * | * | Good (3 + 2 + 2) | |
| Studies/Domains | Selection | Comparability | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the Exposed Cohort | Selection of the Non-Exposed Cohort | Ascertainment of Exposure | Demonstration that Outcome of Interest was not Present at the Start of the Study | Comparability | Assessment of Outcome | Was Follow-Up Long Enough for Outcomes to Occur | Adequacy of Follow-Up of Cohorts | Quality | |
| McNaughton et al., 2014 [34] | * | * | * | ** | * | * | * | Good (3 + 2 + 3) | |
| # Halladay et al., 2017 [22] | * | * | ** | * | * | * | Fair (2 + 2 + 3) | ||
| # Shi et al., 2017 [23] | * | * | * | ** | * | Poor (3 + 2 + 1) | |||
| Random Sequence Generation | Allocation Concealment | Blinding of Participant and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Bias Due to Problems Not Covered Elsewhere | Quality | |
|---|---|---|---|---|---|---|---|---|
| Delavar et al., 2020 [24] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Good |
| Category | Outcome | Design (Total Number of Studies by Design) | Positive Results (p < 0.05) | Negative Results (p < 0.05) | Non-Significant Results (p > 0.05) |
|---|---|---|---|---|---|
| Blood pressure | Blood pressure control | Cross-sectional (N = 15) | 11 | 1 | 3 |
| Cohort (N = 1) | 1 | ||||
| RCT (N = 1) | 1 | ||||
| Blood pressure/Hypertension knowledge | Cross-sectional (N = 2) | 2 | |||
| Salt | Low salt diet adherence | Cross-sectional (N = 1) | 1 | ||
| Salt awareness | Cross-sectional (N = 1) | 1 | |||
| 24 h urine | Cross-sectional (N = 1) | 1 | |||
| Health literacy sodium restriction | Cross-sectional (N = 1) | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Isa, D.; Shahar, S.; He, F.J.; Majid, H.A. Associations of Health Literacy with Blood Pressure and Dietary Salt Intake among Adults: A Systematic Review. Nutrients 2021, 13, 4534. https://doi.org/10.3390/nu13124534
Mohd Isa D, Shahar S, He FJ, Majid HA. Associations of Health Literacy with Blood Pressure and Dietary Salt Intake among Adults: A Systematic Review. Nutrients. 2021; 13(12):4534. https://doi.org/10.3390/nu13124534
Chicago/Turabian StyleMohd Isa, Darwish, Suzana Shahar, Feng J. He, and Hazreen Abdul Majid. 2021. "Associations of Health Literacy with Blood Pressure and Dietary Salt Intake among Adults: A Systematic Review" Nutrients 13, no. 12: 4534. https://doi.org/10.3390/nu13124534
APA StyleMohd Isa, D., Shahar, S., He, F. J., & Majid, H. A. (2021). Associations of Health Literacy with Blood Pressure and Dietary Salt Intake among Adults: A Systematic Review. Nutrients, 13(12), 4534. https://doi.org/10.3390/nu13124534








