Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Data Collection
2.2.1. Questionnaire Survey
2.2.2. Physical Examination
2.2.3. Dietary Evaluation
2.2.4. Laboratory Tests
2.3. Quality Control
2.4. Definition of MetS
2.5. Covariates
2.6. Statistical Analysis
3. Results
3.1. General Characteristics of the Participants
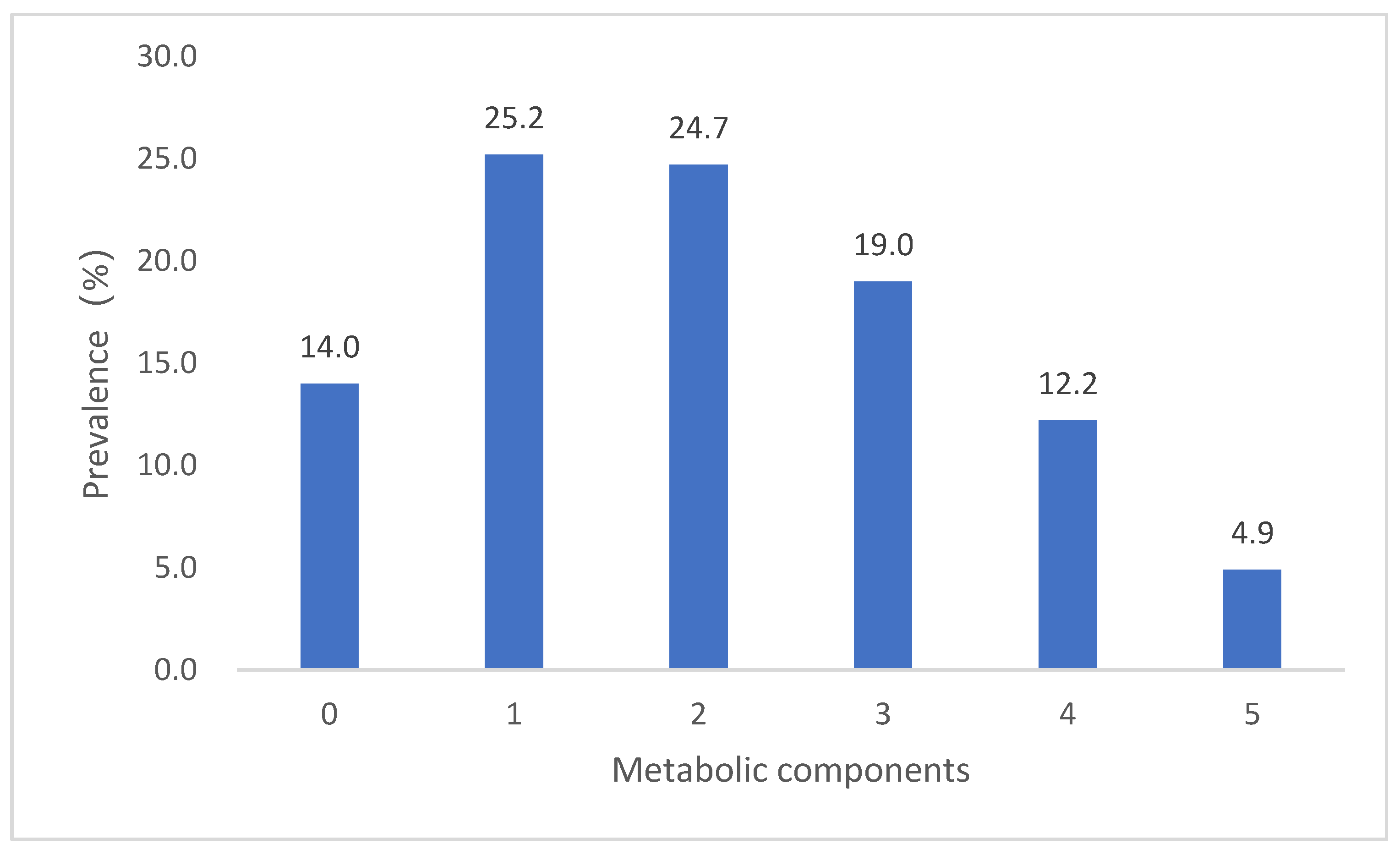
3.2. Standardised Prevalence of MetS and Its Components
3.3. Multivariate Logistic Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ozmen, M.; Yersal, O.; Ozturk, S.; Solmaz, D.; Koseeoglu, M.H. Prevalence of the metabolic syndrome in rheumatoid arthritis. Eur. J. Rheumatol. 2014, 1, 1–4. [Google Scholar] [CrossRef]
- Lim, S.; Shin, H.; Song, J.H.; Kwak, S.H.; Kang, S.M.; Won, Y.J.; Choi, S.H.; Cho, S.I.; Park, K.S.; Lee, H.K.; et al. Increasing prevalence of metabolic syndrome in Korea: The Korean National Health and Nutrition Examination Survey for 1998–2007. Diabetes Care 2011, 34, 1323–1328. [Google Scholar] [CrossRef] [Green Version]
- Aguilar, M.; Bhuket, T.; Torres, S.; Liu, B.; Wong, R.J. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA 2015, 313, 1973–1974. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Reynolds, K.; Wu, X.; Chen, J.; Duan, X.; Reynolds, R.F.; Whelton, P.K.; He, J.; For, T.I.C.G.; InterASIA, C.G. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet 2005, 365, 1398–1405. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, L.; Yu, D.; Wang, Z.; Ding, G. Metabolic syndrome prevalence and its risk factors among adults in China: A nationally representative cross-sectional study. PLoS ONE 2018, 13, e199293. [Google Scholar] [CrossRef]
- Yu, D.; Zhao, L.; Zhang, J.; Yang, Z.; Ding, G. China Nutrition and Health Surveys (19822017). China CDC Wkly. 2021, 3, 193–195. [Google Scholar] [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. Draft Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; IChemE: Rugby, UK, 2013. [Google Scholar]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Santos, A.C.; Ebrahim, S.; Barros, H. Gender, socio-economic status and metabolic syndrome in middle-aged and old adults. BMC Public Health 2008, 8, 62. [Google Scholar] [CrossRef] [Green Version]
- Hajian-Tilaki, K.; Heidari, B.; Firouzjahi, A.; Bagherzadeh, M.; Hajian-Tilaki, A.; Halalkhor, S. Prevalence of metabolic syndrome and the association with socio-demographic characteristics and physical activity in urban population of Iranian adults: A population-based study. Diabetes Metab. Syndr. Clin. Res. Rev. 2014, 8, 170–176. [Google Scholar] [CrossRef]
- Xu, T.; Zhu, G.; Han, S. Prevalence of and lifestyle factors associated with metabolic syndrome determined using multi-level models in Chinese adults from a cross-sectional survey. Medicine 2020, 99, e22883. [Google Scholar] [CrossRef]
- Fujimoto, W.Y.; Bergstrom, R.W.; Boyko, E.J.; Chen, K.; Kahn, S.E.; Leonetti, D.L.; McNeely, M.J.; Newell, L.L.; Shofer, J.B.; Wahl, P.W. Type 2 diabetes and the metabolic syndrome in Japanese Americans. Diabetes Res. Clin. Pract. 2000, 50, S73–S76. [Google Scholar] [CrossRef]
- Wang, G.; Li, L.; Pan, Y.; Tian, G.; Lin, W.; Li, Z.; Chen, Z.; Gong, Y.; Kikano, G.E.; Stange, K.C.; et al. Prevalence of metabolic syndrome among urban community residents in China. BMC Public Health 2013, 13, 599. [Google Scholar] [CrossRef] [Green Version]
- Xi, B.; He, D.; Hu, Y.; Zhou, D. Prevalence of metabolic syndrome and its influencing factors among the Chinese adults: The China Health and Nutrition Survey in 2009. Prev. Med. 2013, 57, 867–871. [Google Scholar] [CrossRef] [Green Version]
- Zhou, W.; Li, C.L.; Cao, J.; Feng, J. Metabolic syndrome prevalence in patients with obstructive sleep apnea syndrome and chronic obstructive pulmonary disease: Relationship with systemic inflammation. Clin. Respir. J. 2020, 14, 1159–1165. [Google Scholar] [CrossRef]
- Hannoun, Z.; Harraqui, K.; Ben, A.R.; Tahiri, K.; Smail, O.B.; Samara, I.; Arabi, F.E.; Bour, A. Epidemiological profile and clinical characteristics of metabolic syndrome in Marrakesh, Morocco. Pan Afr. Med. J. 2020, 36, 133. [Google Scholar] [CrossRef]
- Park, H.S. The metabolic syndrome and associated lifestyle factors among South Korean adults. Int. J. Epidemiol. 2004, 33, 328–336. [Google Scholar] [CrossRef]
- Prasad, D.S.; Kabir, Z.; Dash, A.K.; Das, B.C. Prevalence and risk factors for metabolic syndrome in Asian Indians: A community study from urban Eastern India. J. Cardiovasc. Dis. Res. 2012, 3, 204–211. [Google Scholar] [CrossRef] [Green Version]
- Carmelli, D.; Cardon, L.R.; Fabsitz, R. Clustering of hypertension, diabetes, and obesity in adult male twins: Same genes or same environments? Am. J. Hum. Genet. 1994, 55, 566–573. [Google Scholar]
- Yu, M.; Xu, C.; Zhu, H.; Hu, R.; Zhang, J.; Wang, H.; He, Q.; Su, D.; Zhao, M.; Wang, L.; et al. Associations of Cigarette Smoking and Alcohol Consumption with Metabolic Syndrome in a Male Chinese Population: A Cross-Sectional Study. J. Epidemiol. 2014, 24, 361–369. [Google Scholar] [CrossRef] [Green Version]
- Jeong, J.; Yu, J. Prevalence and Influencing Factors of Metabolic Syndrome among Persons with Physical Disabilities. Asian Nurs. Res. 2018, 12, 50–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tresserra-Rimbau, A.; Medina-Remón, A.; Lamuela-Raventós, R.M.; Bulló, M.; Salas-Salvadó, J.; Corella, D.; Fitó, M.; Gea, A.; Gómez-Gracia, E.; Lapetra, J. Moderate red wine consumption is associated with a lower prevalence of the metabolic syndrome in the PREDIMED population. Br. J. Nutr. 2015, 113, S121–S130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.; Kim, Y.; Jeon, J.Y. Association between physical activity and the prevalence of metabolic syndrome: From the Korean National Health and Nutrition Examination Survey, 1999–2012. SpringerPlus 2016, 5, 1870. [Google Scholar] [CrossRef] [Green Version]
- Houti, L.; Hamani-Medjaoui, I.; Lardjam-Hetraf, S.A.; Ouhaibi-Djellouli, H.; Chougrani, S.; Goumidi, L.; Mediene-Benchekor, S. Prevalence of Metabolic Syndrome and its Related Risk Factors in the City of Oran, Algeria: The ISOR Study. Ethn. Dis. 2016, 26, 99–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, L.N.; Wang, H.J.; Wang, Z.H.; Zhang, J.G.; Jia, X.F.; Zhang, B.; Ding, G.Q. Association of Red Meat Usual Intake with Serum Ferritin and the Risk of Metabolic Syndrome in Chinese Adults: A Longitudinal Study from the China Health and Nutrition Survey. Biomed. Environ. Sci. 2020, 33, 19–29. [Google Scholar] [CrossRef]
- Shang, X.; Scott, D.; Hodge, A.; English, D.R.; Giles, G.G.; Ebeling, P.R.; Sanders, K.M. Dietary protein from different food sources, incident metabolic syndrome and changes in its components: An 11-year longitudinal study in healthy community-dwelling adults. Clin. Nutr. 2017, 36, 1540–1548. [Google Scholar] [CrossRef]
- Esmaillzadeh, A.; Kimiagar, M.; Mehrabi, Y.; Azadbakht, L.; Hu, F.B.; Willett, W.C. Fruit and vegetable intakes, C-reactive protein, and the metabolic syndrome. Am. J. Clin. Nutr. 2006, 84, 1489–1497. [Google Scholar] [CrossRef]
- Tian, Y.; Su, L.; Wang, J.; Duan, X.; Jiang, X. Fruit and vegetable consumption and risk of the metabolic syndrome: A meta-analysis. Public Health Nutr. 2018, 21, 756–765. [Google Scholar] [CrossRef]

| Men | Women | Total | |
|---|---|---|---|
| N | 61,775 | 68,243 | 130,018 |
| Age, years * | 53.0 (43.4,63.2) | 51.8 (42.4,61.7) | 52.3 (42.9,62.4) |
| Residence location, N (%) * | |||
| City | 25,371 (41.1) | 29,878 (43.8) | 55,249 (42.5) |
| Countryside | 36,404 (58.9) | 38,365 (56.2) | 74,769 (57.5) |
| Area of the country, N (%) * | |||
| South | 31,232 (50.6) | 35,253 (51.7) | 66,485 (51.1) |
| North | 30,543 (49.4) | 32,990 (48.3) | 63,533 (48.9) |
| Education level, N (%) * | |||
| Low | 24,315 (39.4) | 36,645 (53.7) | 60,960 (46.9) |
| Moderate | 22,516 (36.5) | 18,608 (27.3) | 41,124 (31.6) |
| High | 14,944 (24.2) | 12,990 (19.0) | 27,934 (21.5) |
| Income, N (%) * | |||
| Low | 17,612 (28.5) | 18,535 (27.2) | 36,147 (27.8) |
| Moderate | 15,524 (25.1) | 17,265 (25.3) | 32,789 (25.2) |
| High | 15,715 (25.4) | 17,995 (26.4) | 33,710 (25.9) |
| Very high | 12,924 (20.9) | 14,448 (21.2) | 27,372 (21.1) |
| Family history of hypertension, N (%) * | 20,313 (32.9) | 23,619 (34.6) | 43,932 (33.8) |
| Family history of diabetes, N (%) * | 5609 (9.1) | 7149 (10.5) | 12,758 (9.8) |
| Smoking, N (%) * | |||
| Never | 20,433 (33.1) | 65,732 (96.3) | 86,165 (66.3) |
| Former | 8673 (14.0) | 569 (0.8) | 9242 (7.1) |
| Current | 32,669 (52.9) | 1942 (2.9) | 34,611 (26.6) |
| Alcohol consumption, N (%) * | |||
| Never | 21,429 (34.7) | 51,799 (75.9) | 73,228 (56.3) |
| Moderate | 28,415 (46.0) | 15,377 (22.5) | 43,792 (33.7) |
| Excessive | 11,931 (19.3) | 1067 (1.6) | 12,998 (10.0) |
| Physically active, N (%) * | 41,112 (66.6) | 50,741 (74.4) | 91,853 (70.7) |
| Insufficient fruit and vegetable intake, N (%) * | 32,012 (51.8) | 34,970 (51.2) | 66,982 (51.5) |
| Red meat intake, N (%) * | |||
| Moderate | 4606 (7.5) | 5714 (8.4) | 10,320 (7.9) |
| Insufficient | 24,442 (39.6) | 31,533 (46.2) | 55,975 (43.1) |
| Excessive | 32,727 (53.0) | 30,996 (45.4) | 63,723 (49.0) |
| BMI (kg/m²) * | 24.2 (22.0,26.6) | 24.2 (22.0,26.7) | 24.2 (22.0,26.6) |
| WC (cm) * | 85.3 ± 10.0 | 81.9 ± 9.7 | 83.5 ± 10.0 |
| Systolic blood pressure (mmHg) * | 136.6 ± 19.7 | 134.4 ± 22.2 | 135.4 ± 21.0 |
| Diastolic blood pressure (mmHg) * | 81.7 ± 11.4 | 77.7 ± 11.4 | 79.6 ± 11.5 |
| TG (mmol/L) * | 1.3 (0.9,2.0) | 1.2 (0.8,1.8) | 1.2 (0.8,1.9) |
| HDL-C (mmol/L) * | 1.2 ± 0.4 | 1.3 ± 0.3 | 1.3 ± 0.3 |
| Fasting plasma glucose (mmol/L) * | 5.2 (4.8,5.7) | 5.2 (4.8,5.6) | 5.2 (4.8,5.7) |
| Prevalence | 95% CI | Rao-Scott X2 | p-Value | ||
|---|---|---|---|---|---|
| Total | 31.1 | 30.0–32.2 | |||
| Sex | 10.9707 | 0.0009 | |||
| Men | 30.0 | 28.8–31.3 | |||
| Women | 32.3 | 30.9–33.6 | |||
| Age, years | 1420.8214 | <0.0001 | |||
| 20–44 | 23.3 | 22.1–24.5 | |||
| 45–59 | 39.0 | 37.9–40.1 | |||
| 60–74 | 43.9 | 42.4–45.5 | |||
| ≥75 | 44.2 | 41.3–47.2 | |||
| Residence location | 2.8593 | 0.0908 | |||
| City | 32.0 | 30.2–33.8 | |||
| Countryside | 30.1 | 28.8–31.4 | |||
| Area of the country | 232.4353 | <0.0001 | |||
| South | 27.4 | 26.2–28.6 | |||
| North | 35.9 | 34.7–37.2 | |||
| BMI | 54,564.5498 | <0.0001 | |||
| Normal | 11.8 | 11.1–12.6 | |||
| Overweight | 41.0 | 39.9–42.0 | |||
| Obese | 70.5 | 69.0–72.0 | |||
| Education level | 59.5475 | <0.0001 | |||
| Low | 35.8 | 34.4–37.2 | |||
| Moderate | 30.3 | 29.0–31.6 | |||
| High | 27.1 | 24.9–29.3 | |||
| Income | 1.5158 | 0.6786 | |||
| Low | 30.9 | 29.5–32.4 | |||
| Moderate | 30.4 | 29.2–31.6 | |||
| High | 31.7 | 30.4–33.1 | |||
| Very high | 31.4 | 28.7–34.1 | |||
| Family history of hypertension | 87.8033 | <0.0001 | |||
| No | 29.0 | 28.0–30.0 | |||
| Yes | 34.8 | 33.1–36.4 | |||
| Family history of diabetes | 107.2048 | <0.0001 | |||
| No | 30.0 | 28.9–31.0 | |||
| Yes | 39.9 | 37.5–42.3 | |||
| Physical activity | 6.7119 | 0.0096 | |||
| Not active | 32.1 | 30.7–33.5 | |||
| Active | 30.6 | 29.5–31.8 | |||
| Smoking status | 34.7917 | <0.0001 | |||
| Never | 31.2 | 30.0–32.5 | |||
| Former | 37.7 | 35.4–40.0 | |||
| Current | 29.6 | 28.1–31.0 | |||
| Alcohol consumption | 40.8781 | <0.0001 | |||
| Never | 32.6 | 31.6–33.7 | |||
| Moderate | 28.7 | 27.2–30.2 | |||
| Excessive | 33.2 | 30.9–35.5 | |||
| Fruit and vegetable intake | 2.3882 | 0.1223 | |||
| Sufficient | 31.6 | 30.5–32.7 | |||
| Insufficient | 30.6 | 29.2–32.0 | |||
| Red meat intake | 36.6381 | <0.0001 | |||
| Moderate | 30.8 | 29.0–32.5 | |||
| Insufficient | 32.8 | 31.5–34.1 | |||
| Excessive | 29.8 | 28.6–31.0 |
| Influencing Factor | β | SE | Wald X2 | p | OR | 95% CI | |
|---|---|---|---|---|---|---|---|
| Intercept | −12.4553 | 0.0961 | 16,784.5555 | <0.0001 | |||
| Sex | Women vs. Men | 0.5727 | 0.0189 | 918.6448 | <0.0001 | 1.773 | 1.709–1.840 |
| Age | 0.0368 | 0.0005 | 4751.4066 | <0.0001 | 1.037 | 1.036–1.039 | |
| Residence location | Countryside vs. City | −0.0411 | 0.0148 | 7.7242 | 0.0054 | 0.960 | 0.932–0.988 |
| Area of the country | North vs. South | 0.0835 | 0.0136 | 37.4822 | <0.0001 | 1.087 | 1.058–1.117 |
| BMI | 0.3377 | 0.0024 | 19,715.8134 | <0.0001 | 1.402 | 1.395–1.408 | |
| Income | Moderate vs. Low | 0.0433 | 0.0188 | 5.3170 | 0.0211 | 1.044 | 1.007–1.083 |
| High vs. Low | 0.0800 | 0.0190 | 17.6248 | <0.0001 | 1.083 | 1.044–1.124 | |
| Very high vs. Low | 0.1160 | 0.0208 | 30.9902 | <0.0001 | 1.123 | 1.078–1.170 | |
| Family history of hypertension | Yes vs. No | 0.2130 | 0.0146 | 212.8383 | <0.0001 | 1.237 | 1.203–1.273 |
| Family history of diabetes | Yes vs. No | 0.3992 | 0.0225 | 315.9245 | <0.0001 | 1.491 | 1.426–1.558 |
| Smoking status | Former vs. Never | 0.0289 | 0.0292 | 0.9808 | 0.3220 | 1.029 | 0.972–1.090 |
| Current vs. Never | 0.1339 | 0.0207 | 41.6962 | <0.0001 | 1.143 | 1.098–1.191 | |
| Alcohol consumption | Moderate vs. Never | −0.0868 | 0.0160 | 29.6303 | <0.0001 | 0.917 | 0.889–0.946 |
| Excessive vs. Never | 0.0001 | 0.0254 | 0.0000 | 0.9957 | 1.000 | 0.952–1.051 | |
| Physical activity | Active vs. Not active | −0.1197 | 0.0149 | 64.7071 | <0.0001 | 0.887 | 0.862–0.913 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yao, F.; Bo, Y.; Zhao, L.; Li, Y.; Ju, L.; Fang, H.; Piao, W.; Yu, D.; Lao, X. Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017. Nutrients 2021, 13, 4475. https://doi.org/10.3390/nu13124475
Yao F, Bo Y, Zhao L, Li Y, Ju L, Fang H, Piao W, Yu D, Lao X. Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017. Nutrients. 2021; 13(12):4475. https://doi.org/10.3390/nu13124475
Chicago/Turabian StyleYao, Fan, Yacong Bo, Liyun Zhao, Yaru Li, Lahong Ju, Hongyun Fang, Wei Piao, Dongmei Yu, and Xiangqian Lao. 2021. "Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017" Nutrients 13, no. 12: 4475. https://doi.org/10.3390/nu13124475
APA StyleYao, F., Bo, Y., Zhao, L., Li, Y., Ju, L., Fang, H., Piao, W., Yu, D., & Lao, X. (2021). Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017. Nutrients, 13(12), 4475. https://doi.org/10.3390/nu13124475





