Development and Preliminary Feasibility of iByte4Health: A Mobile Health (mHealth) Pediatric Obesity Prevention Intervention to Engage Parents with Low-Income of Children 2–9 Years
Abstract
1. Introduction
2. Materials and Methods
2.1. Program Overview
2.2. Study 1: Formative Development
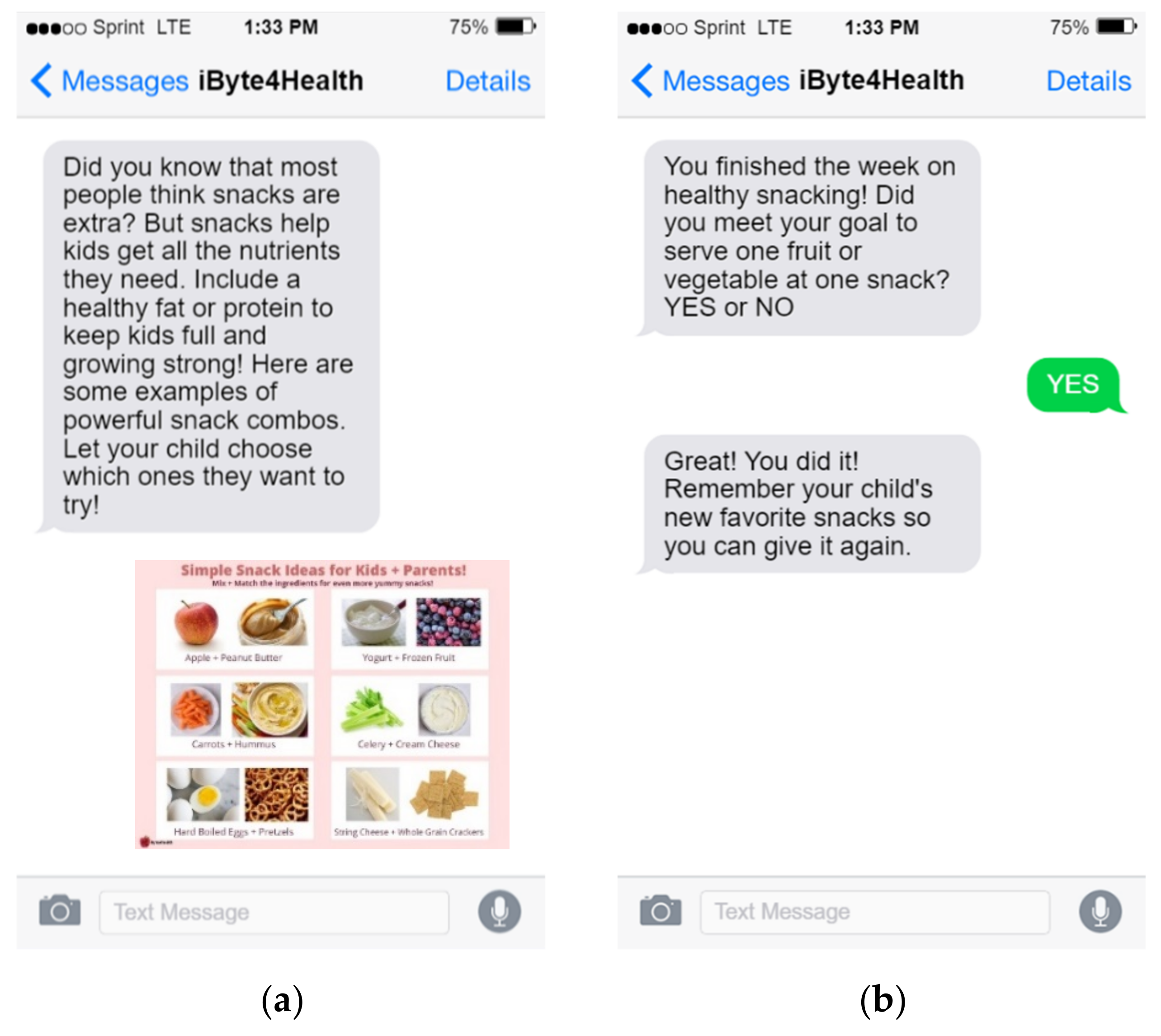
2.3. iByte4Health Program Development
2.4. Study 2: Proof-of-Concept Feasibility Testing
3. Results
3.1. Study 1: Formative Development
3.1.1. Participant Demographics
3.1.2. Preferences for Content Focus and Key Barriers to Improving Health in Children
3.1.3. Technology Access
3.1.4. Digital Program Format and Frequency
3.2. Study 2: Proof-of-Concept Feasibility Testing
3.2.1. Participant Demographics
3.2.2. Program Utilization and Engagement
3.2.3. Program Acceptability
3.2.4. Program Content and Dose
3.2.5. Behavioral Targets
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Taveras, E.M.; Marshall, R.; Sharifi, M.; Avalon, E.; Fiechtner, L.; Horan, C.; Orav, J.; Price, S.N.; Sequist, T.; Slater, D. Connect for Health: Design of a clinical-community childhood obesity intervention testing best practices of positive outliers. Contemp. Clin. Trials 2015, 45(Pt. B), 287–295. [Google Scholar] [CrossRef] [PubMed]
- Frederick, C.B.; Snellman, K.; Putnam, R.D. Increasing socioeconomic disparities in adolescent obesity. Proc. Natl. Acad. Sci. USA 2014, 111, 1338–1342. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef]
- Mohanan, S.; Tapp, H.; McWilliams, A.; Dulin, M. Obesity and asthma: Pathophysiology and implications for diagnosis and management in primary care. Exp. Biol. Med. 2014, 239, 1531–1540. [Google Scholar] [CrossRef] [PubMed]
- Fox, C.K.; Gross, A.C.; Rudser, K.D.; Foy, A.; Kelly, A.S. Depression, Anxiety, and Severity of Obesity in Adolescents. Clin. Pediatrics 2016, 55, 1120–1125. [Google Scholar] [CrossRef]
- Kumanyika, S.K. Environmental influences on childhood obesity: Ethnic and cultural influences in context. Physiol. Behav. 2008, 94, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Steinhubl, R.S.; Muse, E.D.; Topol, E.J. The emerging field of mobile health. Sci. Transl. Med. 2015, 7, 283rv3. [Google Scholar]
- Tate, E.B.; Spruijt-Metz, D.; O’Reilly, G.; Jordan-Marsh, M.; Gotsis, M.; Pentz, M.A.; Dunton, G.F. mHealth approaches to child obesity prevention: Successes, unique challenges, and next directions. Transl. Behav. Med. 2013, 3, 406–415. [Google Scholar] [CrossRef]
- Perrin, A. Smartphones Help Blacks, Hispanics Bridge Some- But Not All- Digital Gaps with Whites. 2017. Available online: http://www.pewresearch.org/fact-tank/2017/08/31/smartphones-help-blacks-hispanics-bridge-some-but-not-all-digital-gaps-with-whites/ (accessed on 1 August 2018).
- Hammersley, L.M.; Jones, R.A.; Okely, A.D. Parent-Focused Childhood and Adolescent Overweight and Obesity eHealth Interventions: A Systematic Review and Meta-Analysis. J. Med. Internet Res. 2016, 18, e203. [Google Scholar] [CrossRef]
- Wen, L.M.; Rissel, C.; Xu, H.; Taki, S.; Smith, W.; Bedford, K.; Hayes, A.J.; Phongsavan, P.; Simpson, J.M.; Shaw, M.J.; et al. Linking two randomised controlled trials for Healthy Beginnings(c): Optimising early obesity prevention programs for children under 3 years. BMC Public Health 2019, 19, 739. [Google Scholar] [CrossRef]
- Kohl, L.F.; Crutzen, R.; de Vries, N.K. Online prevention aimed at lifestyle behaviors: A systematic review of reviews. J. Med. Internet Res. 2013, 15, e146. [Google Scholar] [CrossRef] [PubMed]
- Anderson-Lewis, C.; Darville, G.; Mercado, R.E.; Howell, S.; Di Maggio, S. mHealth Technology Use and Implications in Historically Underserved and Minority Populations in the United States: Systematic Literature Review. JMIR Mhealth Uhealth 2018, 6, e128. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.T.; Bautista, J.R. Understanding the Relationships between mHealth Apps’ Characteristics, Trialability, and mHealth Literacy. J. Health Commun. 2017, 22, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Paige, S.R.; Alber, J.M.; Stellefson, M.L.; Krieger, J. Missing the mark for patient engagement: mHealth literacy strategies and behavior change processes in smoking cessation apps. Patient Educ. Couns. 2018, 101, 951–955. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Spring, B.J.; Riper, H.; Morrison, L.G.; Crane, D.H.; Curtis, K.; Merchant, G.C.; Naughton, F.; Blandford, A. Understanding and Promoting Effective Engagement With Digital Behavior Change Interventions. Am. J. Prev. Med. 2016, 51, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Kreps, G.L.; Thornton, B.C. Health Communication: Theory & Practice, 2nd ed.; Waveland Press: Prospect Heights, IL, USA, 1992. [Google Scholar]
- Ihmels, M.A.; Welk, G.J.; Eisenmann, J.C.; Nusser, S.M. Development and preliminary validation of a Family Nutrition and Physical Activity (FNPA) screening tool. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 14. [Google Scholar] [CrossRef]
- Ihmels, M.A.; Welk, G.J.; Eisenmann, J.C.; Nusser, S.M.; Myers, E.F. Prediction of BMI change in young children with the family nutrition and physical activity (FNPA) screening tool. Ann. Behav. Med. 2009, 38, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Peyer, K.L.; Bailey-Davis, L.; Welk, G. Development, Applications, and Refinement of the Family Nutrition and Physical Activity (FNPA) Child Obesity Prevention Screening. Health Promot. Pract. 2020, 22, 456–461. [Google Scholar] [CrossRef]
- National Cancer Institute (U.S.). Theory at a Glance: A Guide for Health Promotion Practice, 2nd ed.; Glanz, K., Ed.; U.S. Dept. of Health and Human Services, National Cancer Institute: Bethesda, MD, USA, 2005.
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Michie, S.; Wood, C.E.; Johnston, M.; Abraham, C.; Francis, J.J.; Hardeman, W. Behaviour change techniques: The development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technol. Assess. 2015, 19, 1–188. [Google Scholar] [PubMed]
- American Academy of Pediatrics. Bright Futures: Nutrition Pocket Guide, 3rd ed.; Holt, K.A., Ed.; American Academy of Pediatrics: Washington, DC, USA, 2011. [Google Scholar]
- U.S. Department of Health and Human Services. 2015–2020 Dietary Guidelines for Americans, 8th ed.; U.S. Department of Agriculture: Washington, DC, USA, 2015. Available online: https://heatlh.gov/dietaryguidelines/2015/guidelines/ (accessed on 22 July 2021).
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd ed.; US Department of Health and Human Services: Washington, DC, USA, 2018.
- Carroll, N.; Sadowski, A.; Laila, A.; Hruska, V.; Nixon, M.; Ma, D.; Haines, J.; on behalf of the Guelph Family Health Study. The Impact of COVID-19 on Health Behavior, Stress, Financial and Food Security among Middle to High Income Canadian Families with Young Children. Nutrients 2020, 12, 2352. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Ganter, C.; Chuang, E.; Aftosmes-Tobio, A.; Blaine, R.E.; Giannetti, M.; Land, T.; Davison, K.K. Community stakeholders’ perceptions of barriers to childhood obesity prevention in low-income families, Massachusetts 2012–2013. Prev. Chronic. Dis. 2015, 12, E42. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The person-based approach to intervention development: Application to digital health-related behavior change interventions. J. Med. Internet Res. 2015, 17, e30. [Google Scholar] [CrossRef] [PubMed]
- Armanasco, A.A.; Miller, Y.D.; Fjeldsoe, B.; Marshall, A. Preventive Health Behavior Change Text Message Interventions: A Meta-analysis. Am. J. Prev. Med. 2017, 52, 391–402. [Google Scholar] [CrossRef]
- Eysenbach, G. The law of attrition. J. Med. Internet Res. 2005, 7, e11. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tripicchio, G.L.; Kay, M.; Herring, S.; Cos, T.; Bresnahan, C.; Gartner, D.; Sosinsky, L.S.; Bass, S.B. Development and Preliminary Feasibility of iByte4Health: A Mobile Health (mHealth) Pediatric Obesity Prevention Intervention to Engage Parents with Low-Income of Children 2–9 Years. Nutrients 2021, 13, 4240. https://doi.org/10.3390/nu13124240
Tripicchio GL, Kay M, Herring S, Cos T, Bresnahan C, Gartner D, Sosinsky LS, Bass SB. Development and Preliminary Feasibility of iByte4Health: A Mobile Health (mHealth) Pediatric Obesity Prevention Intervention to Engage Parents with Low-Income of Children 2–9 Years. Nutrients. 2021; 13(12):4240. https://doi.org/10.3390/nu13124240
Chicago/Turabian StyleTripicchio, Gina L., Melissa Kay, Sharon Herring, Travis Cos, Carolyn Bresnahan, Danielle Gartner, Laura Stout Sosinsky, and Sarah B. Bass. 2021. "Development and Preliminary Feasibility of iByte4Health: A Mobile Health (mHealth) Pediatric Obesity Prevention Intervention to Engage Parents with Low-Income of Children 2–9 Years" Nutrients 13, no. 12: 4240. https://doi.org/10.3390/nu13124240
APA StyleTripicchio, G. L., Kay, M., Herring, S., Cos, T., Bresnahan, C., Gartner, D., Sosinsky, L. S., & Bass, S. B. (2021). Development and Preliminary Feasibility of iByte4Health: A Mobile Health (mHealth) Pediatric Obesity Prevention Intervention to Engage Parents with Low-Income of Children 2–9 Years. Nutrients, 13(12), 4240. https://doi.org/10.3390/nu13124240




