Augmented Renal Clearance, Muscle Catabolism and Urinary Nitrogen Loss: Implications for Nutritional Support in Critically Ill Trauma Patients
Abstract
1. Introduction
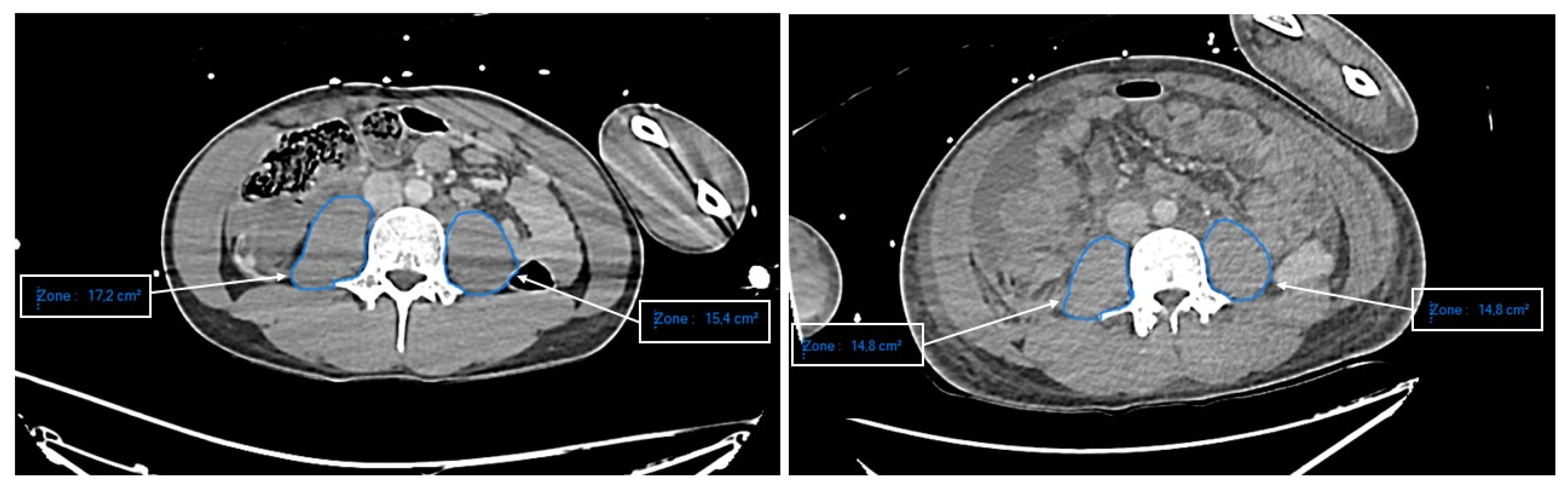
2. Materials and Methods
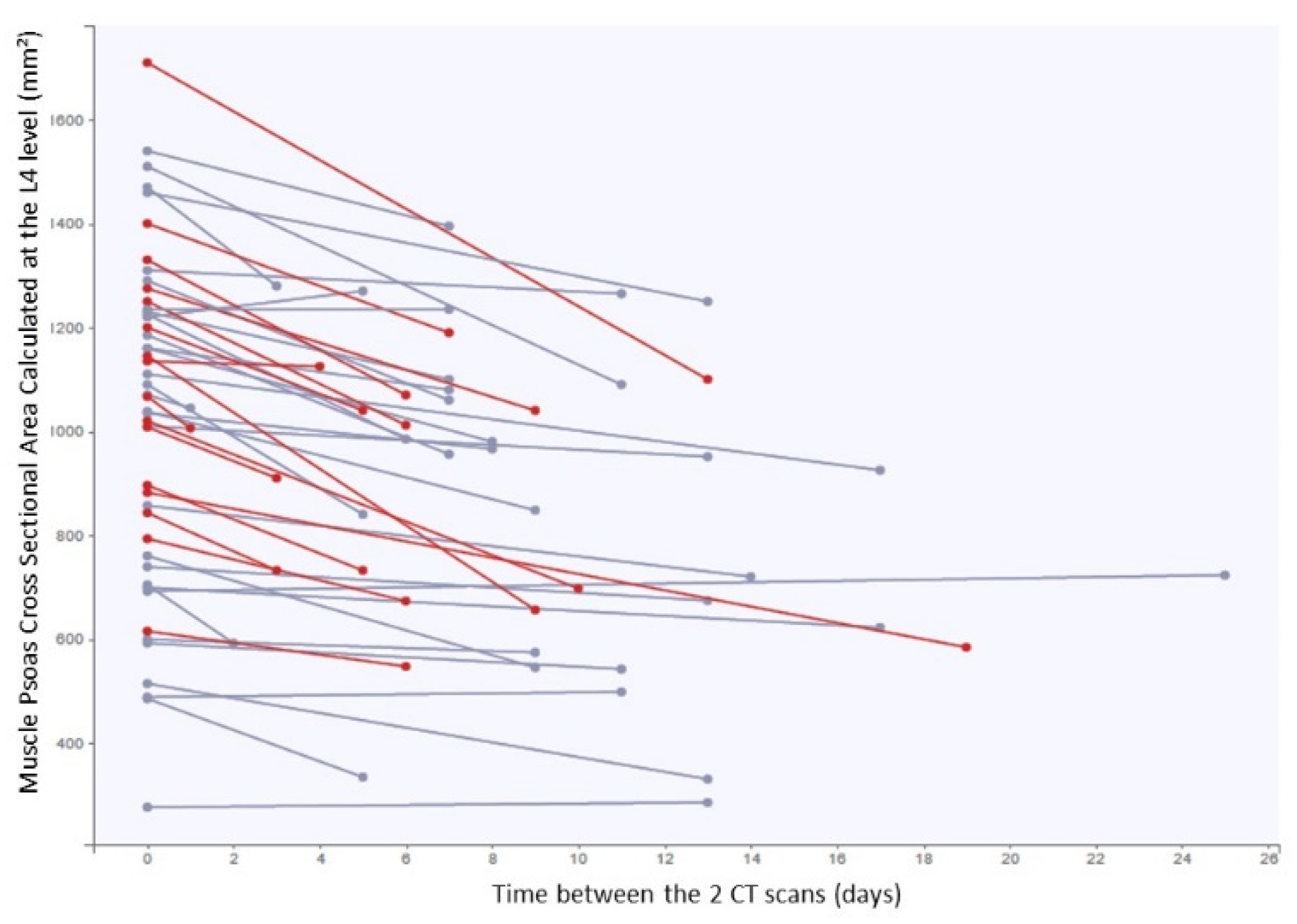
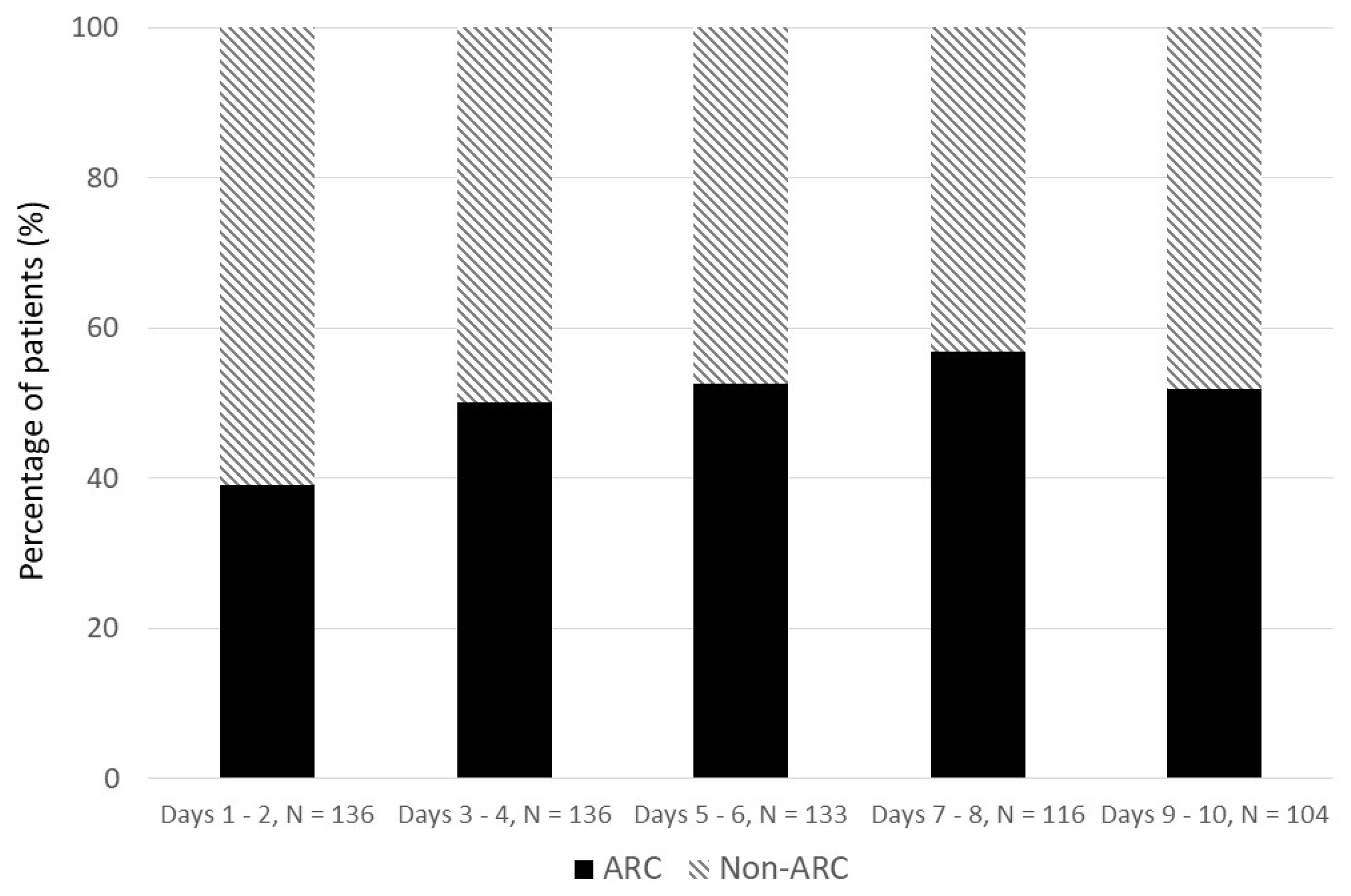
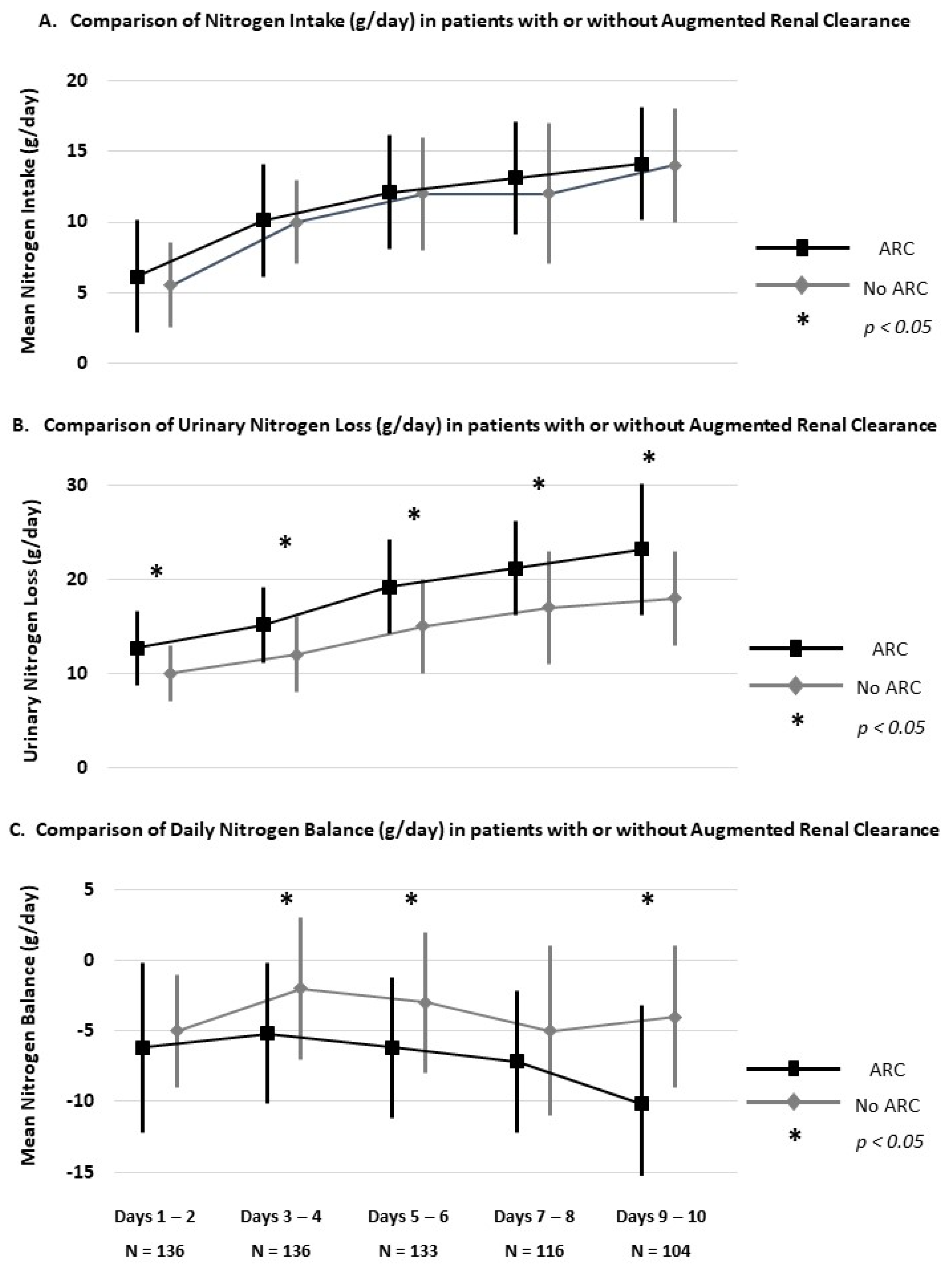
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Singer, P. Protein metabolism and requirements in the ICU. Clin. Nutr. 2020, 38, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Weijs, P.J.; Stapel, S.N.; de Groot, S.D.; Driessen, R.H.; de Jong, E.; Girbes, A.R.; van Schijndel, R.J.S.; Beishuizen, A. Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients: A prospective observational cohort study. J. Parenter. Enter. Nutr. 2012, 36, 60–68. [Google Scholar] [CrossRef]
- Gautier, J.B.O.; Martindale, R.G.; Rugeles, S.J.; Hurt, R.T.; Taylor, B.; Heyland, D.K.; McClave, S.A. How Much and What Type of Protein Should a Critically Ill Patient Receive? Nutr. Clin. Pract. 2017, 32, 6S–14S. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.J.; Park, S.H.; Jeong, H.B.; Ha, E.J.; Cho, W.S.; Kang, H.S.; Kim, J.E.; Ko, S.B. Optimizing Nitrogen Balance Is Associated with Better Outcomes in Neurocritically Ill Patients. Nutrients 2020, 12, 3137. [Google Scholar] [CrossRef]
- Dickerson, R.N.; Crawford, C.N.; Tsiu, M.K.; Bujanowski, C.E.; Van Matre, E.T.; Swanson, J.M.; Filiberto, D.M.; Minard, G. Augmented Renal Clearance Following Traumatic Injury in Critically Ill Patients Requiring Nutrition Therapy. Nutrients 2021, 13, 1681. [Google Scholar] [CrossRef]
- Cook, A.M.; Hatton-Kolpek, J. Augmented Renal Clearance. Pharmacotherapy 2019, 39, 346–354. [Google Scholar] [CrossRef]
- Udy, A.A.; Jarrett, P.; Stuart, J.; Lassig-Smith, M.; Starr, T.; Dunlop, R.; Wallis, S.C.; Roberts, J.A.; Lipman, J. Determining the mechanisms underlying augmented renal drug clearance in the critically ill: Use of exogenous marker compounds. Crit. Care 2014, 18, 657. [Google Scholar] [CrossRef]
- Carrie, C.; Lannou, A.; Rubin, S.; De Courson, H.; Petit, L.; Biais, M. Augmented renal clearance in critically ill trauma patients: A pathophysiologic approach using renal vascular index. Anaesth. Crit. Care Pain Med. 2019, 38, 371–375. [Google Scholar] [CrossRef]
- Helal, I.; Fick-Brosnahan, G.M.; Reed-Gitomer, B.; Schrier, R.W. Glomerular hyperfiltration: Definitions, mechanisms and clinical implications. Nat. Rev. Nephrol. 2012, 8, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Tonneijck, L.; Muskiet, M.; Smits, M.; van Bommel, E.; Heerpink, H.; van Raalte, D.; Joles, J. Glomerular hyperfiltration in diabetes: Mechanisms, clinical significance, and treatment. J. Am. Soc. Nephrol. 2017, 28, 1023–1039. [Google Scholar] [CrossRef]
- Han, E.; Lee, Y.H.; Lee, B.W.; Kang, E.S.; Cha, B.S. Pre-sarcopenia is associated with renal hyperfiltration independent of obesity or insulin resistance: Nationwide Surveys (KNHANES 2008-2011). Medicine 2017, 96, e7165. [Google Scholar] [CrossRef] [PubMed]
- Hyun, Y.Y.; Lee, K.B.; Rhee, E.J.; Park, C.Y.; Chang, Y.; Ryu, S. Chronic kidney disease and high eGFR according to body composition phenotype in adults with normal BMI. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Singer, P.; Blaser, A.R.; Berger, M.M.; Alhazzani, W.; Calder, P.C.; Casaer, M.P.; Hiesmayr, M.; Mayer, K.; Montejo, J.C.; Pichard, C.; et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 2019, 38, 48–79. [Google Scholar] [CrossRef]
- Lannou, A.; Carrie, C.; Rubin, S.; Cane, G.; Cottenceau, V.; Petit, L.; Biais, M. Salt wasting syndrome in brain trauma patients: A pathophysiologic approach using sodium balance and urinary biochemical analysis. BMC Neurol. 2020, 20, 190. [Google Scholar] [CrossRef] [PubMed]
- Dickerson, R.N.; Tidwell, A.C.; Minard, G.; Croce, M.A.; Brown, R.O. Predicting total urinary nitrogen excretion from urinary urea nitrogen excretion in multiple-trauma patients receiving specialized nutritional support. Nutrition 2005, 21, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Nitenberg, G. Nutritional supply in the critically ill. Reanimation 2003, 12, 340–349. [Google Scholar] [CrossRef]
- Haines, R.W.; Zolfaghari, P.; Wan, Y.; Pearse, R.M.; Puthucheary, Z.; Prowle, J.R. Elevated urea-to-creatinine ratio provides a biochemical signature of muscle catabolism and persistent critical illness after major trauma. Intensive Care Med. 2019, 45, 1718–1731. [Google Scholar] [CrossRef]
- Yeh, D.D.; Ortiz-Reyes, L.A.; Quraishi, S.A.; Chokengarmwong, N.; Avery, L.; Kaafarani, H.M.A.; Lee, J.; Fagenholz, P.; Chang, Y.; DeMoya, M.; et al. Early nutritional inadequacy is associated with psoas muscle deterioration and worse clinical outcome in critically ill surgical patients. J. Crit. Care 2018, 45, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Lannou, A.; Carrié, C.; Rubin, S.; de Courson, H.; Biais, M. Renal response after traumatic brain injury: A potential relationship between augmented renal clearance and salt wasting syndrome? Anaesth. Crit. Care Pain Med. 2020, 39, 239–241. [Google Scholar] [CrossRef]
- Liebau, F.; Norberg, A.; Rooyackers, O. Does feeding induce maximal stimulation of protein balance? Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 120–124. [Google Scholar] [CrossRef]
- Chapple, L.S.; Summers, M.J.; Bellomo, R.; Chapman, M.J.; Davies, A.R.; Ferrie, S.; Finnis, M.E.; Hurford, S.; Lange, K.; Little, L.; et al. Use of a high-protein enteral nutrition formula to Increase protein delivery to critically ill patients: A randomized, blinded, parallel-group, feasibility trial. J. Parenter. Enter. Nutr. 2021, 45, 699–709. [Google Scholar] [CrossRef]
- van Zanten, A.R.H.; Petit, L.; de Waele, J.; Kieft, H.; de Wilde, J.; van Horssen, P.; Klebach, M.; Hofman, Z. Very high intact-protein formula successfully provides protein intake according to nutritional recommendations in overweight critically ill patients: A double-blind randomized trial. Crit. Care 2018, 22, 156. [Google Scholar] [CrossRef] [PubMed]
- Bosch, J.P.; Lew, S.; Glabman, S.; Lauer, A. Renal hemodynamic changes in humans. Response to protein loading in normal and diseased kidneys. Am. J. Med. 1986, 81, 809–815. [Google Scholar] [CrossRef]
- Ronco, C.; Bellomo, R.; Kellum, J. Understanding renal functional reserve. Intensive Care Med. 2017, 43, 917–920. [Google Scholar] [CrossRef] [PubMed]
- Doig, G.S.; Simpson, F.; Bellomo, R.; Heighes, P.T.; Sweetman, E.A.; Chesher, D.; Pollock, C.; Davies, A.; Botha, J.; Harrigan, P.; et al. Intravenous amino acid therapy for kidney function in critically ill patients: A randomized controlled trial. Intensive Care Med. 2015, 41, 1197–1208. [Google Scholar] [CrossRef] [PubMed]
- Kitada, M.; Ogura, Y.; Monno, I.; Koya, D. A low-protein diet for diabetic kidney disease: Its effect and molecular mechanism, an approach from animal studies. Nutrients 2018, 10, 544. [Google Scholar] [CrossRef]
- Greig, P.D.; Elwyn, D.H.; Askanazi, J.; Kinney, J.M. Parenteral nutrition in septic patients: Effect of increasing nitrogen intake. Am. J. Clin. Nutr. 1987, 46, 1040–1047. [Google Scholar] [CrossRef]
- Dresen, E.; Weiβbrich, C.; Fimmers, R.; Putensen, C.; Stehle, P. Medical high-protein nutrition therapy and loss of muscle mass in adult ICU patients: A randomized controlled trial. Clin. Nutr. 2021, 40, 1562–1570. [Google Scholar] [CrossRef]
- Kim, K.E.; Onesti, G.; Swartz, C. Creatinine clearance and glomerular filtration rate. Br. Med. J. 1972, 1, 379–380. [Google Scholar] [CrossRef]
- Delanaye, P.; Lambermont, B.; Chapelle, J.P.; Gielen, J.; Gerard, P.; Rorive, G. Plasmatic cystatin C for the estimation of glomerular filtration rate in intensive care units. Intensive Care Med. 2004, 30, 980–983. [Google Scholar] [CrossRef][Green Version]
- Baczek, J.; Silkiewicz, M.; Wojszel, Z.B. Myostatin as a Biomarker of Muscle Wasting and other Pathologies-State of the Art and Knowledge Gaps. Nutrients 2020, 12, 2401. [Google Scholar] [CrossRef] [PubMed]
| Urinary Nitrogen Loss (g/day) | Urinary Urea [mmol/L] × 0.056/2.14 + 2 g/day (assumption of non-urea nitrogen) |
| Total Nitrogen Loss (g/day) | Urinary Nitrogen Loss + 2 g/day (assumption of extra-urinary Nitrogen Loss) |
| Nitrogen Intake (g/day) | Protein Intake [g/day]/6.25 |
| Nitrogen Balance (g/day) | Nitrogen Intake—Total Nitrogen Loss |
| ARC Population N = 75 (46) | Non-ARC Population N = 87 (54) | p | |
|---|---|---|---|
| Demographic and Medical History | |||
| Age (years) | 34 [26; 50] | 54 [35; 69] | <0.001 |
| Male sex | 64 (85) | 63 (72) | 0.046 |
| TBW at ICU admission (kg) | 74 [64; 84] | 77 [69; 85] | 0.105 |
| BMI (kg/m2) | 23 [21; 26] | 26 [23; 29] | 0.002 |
| Charlson comorbidity index | 0 [0; 1] | 1 [0; 3] | <0.001 |
| Poor nutritional status before admission * | 7 (8) | 6 (8) | 0.991 |
| Severity Scores | |||
| Initial GCS | 7 [4; 14] | 11 [7; 15] | 0.016 |
| ISS | 38 [25; 50] | 43 [33; 51] | 0.091 |
| SAPS 2 at ICU admission | 44 [35; 53] | 44 [39; 58] | 0.467 |
| Traumatic Injuries (AIS > 3) | |||
| Craniofacial trauma | 56 (75) | 63 (72) | 0.746 |
| Chest trauma | 29 (39) | 42 (48) | 0.219 |
| Abdominal trauma | 20 (27) | 29 (33) | 0.357 |
| Spine fracture | 24 (32) | 23 (26) | 0.437 |
| Patient Management and Complications | |||
| Time under vasopressors | 3 [1; 6] | 4 [2; 6] | 0.325 |
| Time under sedation | 2 [1; 6] | 3 [1; 7] | 0.184 |
| Time under mechanical ventilation | 14 [7; 19] | 12 [7; 17] | 0.509 |
| Intracranial hypertension | 26 (35) | 23 (26) | 0.284 |
| ARDS | 21 (28) | 33 (38) | 0.233 |
| Need for antibiotics | 66 (88) | 75 (86) | 0.886 |
| Need for multiple surgeries | 23 (31) | 24 (28) | 0.807 |
| Need for multiple transfusion | 22 (29) | 36 (42) | 0.114 |
| Patient Outcome | |||
| ICU mortality | 1 (1) | 9 (10) | 0.017 |
| ICU length of stay | 22 [15; 33] | 19 [13; 28] | 0.173 |
| TBW at ICU discharge | 66 [56; 78] | 67 [50; 80] | 0.286 |
| Weight Loss at ICU discharge, kg (%) | 11 [4; 17] | 10 [0; 22] | 0.944 |
| ARC Population N = 75 (46) | Non-ARC Population N = 87 (54) | p | |
|---|---|---|---|
| Use of enteral nutrition | 74 (99) | 84 (97) | 0.387 |
| Use of parenteral nutrition | 27 (36) | 49 (56) | 0.010 |
| Caloric Intake *, Kcals/kg/day (%) | 20 [18; 24] | 19 [17; 22] | 0.019 |
| Energy Target Achievement at Day 10 † (%) | 81 [71; 96] | 76 [66; 87] | 0.019 |
| Protein Intake *, g/kg/day | 0.7 [0.6; 0.8] | 0.7 [0.5; 0.8] | 0.010 |
| Protein Target Achievement at Day 10 † (%) | 60 [53; 71] | 55 [46; 64] | 0.010 |
| ARC Population N = 75 (46) | Non-ARC Population N = 87 (54) | p | |
|---|---|---|---|
| Plasma Biological Analyses * | |||
| Plasma Urea, mmol/L | 5 [4; 6] | 7 [5; 8] | <0.001 |
| Plasma Creatinine, µmol/L | 54 [47; 61] | 63 [55; 74] | <0.001 |
| Urea/Creatinine Ratio | 97 [86; 117] | 103 [84; 126] | 0.485 |
| Neutrophil-to-lymphocyte ratio | 9 [6; 10] | 7 [5; 9] | 0.250 |
| Urinary Biochemical Analyses * | |||
| Urine Volume, L/day | 2.5 [2.1; 3.0] | 2.2 [1.8; 2.9] | 0.036 |
| Urinary Creatinine Excretion, mmol/L | 7 [5; 8] | 5 [4; 7] | 0.027 |
| Creatinine Clearance, mL/min/1.73 m2 | 158 [144; 170] | 110 [87; 120] | <0.001 |
| Urinary Urea Excretion, mmol/L | 256 [177; 325] | 228 [166; 281] | 0.110 |
| Urinary Nitrogen Loss, g/day | 17 [14; 21] | 14 [11; 17] | <0.001 |
| Nitrogen Balance * | |||
| Nitrogen Balance, g/day | −6 [−9; −3] | −4 [−6; −1] | <0.001 |
| Cumulated Nitrogen Balance at Day 10, g | −56 [−92; −30] | −35 [−62; −13] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dreydemy, G.; Coussy, A.; Lannou, A.; Petit, L.; Biais, M.; Carrié, C. Augmented Renal Clearance, Muscle Catabolism and Urinary Nitrogen Loss: Implications for Nutritional Support in Critically Ill Trauma Patients. Nutrients 2021, 13, 3554. https://doi.org/10.3390/nu13103554
Dreydemy G, Coussy A, Lannou A, Petit L, Biais M, Carrié C. Augmented Renal Clearance, Muscle Catabolism and Urinary Nitrogen Loss: Implications for Nutritional Support in Critically Ill Trauma Patients. Nutrients. 2021; 13(10):3554. https://doi.org/10.3390/nu13103554
Chicago/Turabian StyleDreydemy, Guilhem, Alexis Coussy, Alexandre Lannou, Laurent Petit, Matthieu Biais, and Cédric Carrié. 2021. "Augmented Renal Clearance, Muscle Catabolism and Urinary Nitrogen Loss: Implications for Nutritional Support in Critically Ill Trauma Patients" Nutrients 13, no. 10: 3554. https://doi.org/10.3390/nu13103554
APA StyleDreydemy, G., Coussy, A., Lannou, A., Petit, L., Biais, M., & Carrié, C. (2021). Augmented Renal Clearance, Muscle Catabolism and Urinary Nitrogen Loss: Implications for Nutritional Support in Critically Ill Trauma Patients. Nutrients, 13(10), 3554. https://doi.org/10.3390/nu13103554





