The Role of Nutritional Status on Polypharmacy, Cognition, and Functional Capacity of Institutionalized Elderly: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
2.2. Search Strategy
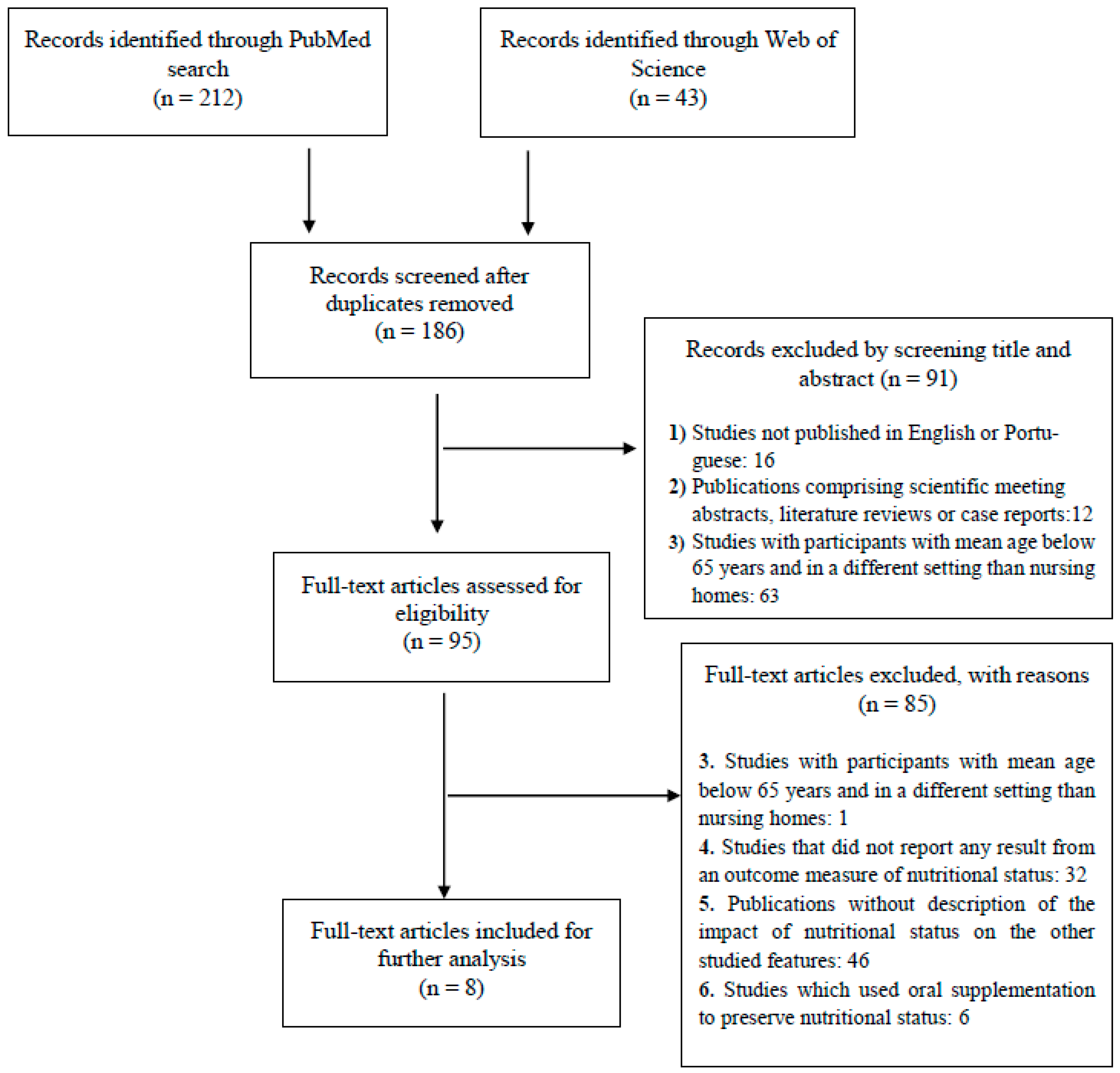
2.3. Selection Process
2.4. Data Extraction
2.5. Risk of Bias (RoB) Assessment and Overall Quality
3. Results
3.1. Study Selection and Literature Review
3.2. Literature Review
3.3. Quality Assessment
3.4. Participants and Follow-Up
3.5. Characteristics of Studies and Outcomes Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Malazonia, M.; Anuashvili, A.; Vashakmadze, N.; Corpas, E. Assessment of Nutritional Status in the Elderly, Causes and Management of Malnutrition in the Elderly. Endocrinol. Aging 2021, 651–687. [Google Scholar] [CrossRef]
- Rasheed, S.; Woods, R.T. Malnutrition and Quality of Life in Older People: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2013, 12, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Malafarina, V.; Uriz-Otano, F.; Gil-Guerrero, L.; Iniesta, R. The Anorexia of Ageing: Physiopathology, Prevalence, Associated Comorbidity and Mortality. A Systematic Review. Maturitas 2013, 74, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Elmadfa, I.; Meyer, A.L. Nutrition, Aging, and Requirements in the Elderly. Present Knowl. Nutr. 2020, 83–99. [Google Scholar] [CrossRef]
- Fonseca, A.C.d.C.; Scoralick, F.M.; Silva, C.L.D.; Bertolino, A.C.; Palma, D.P.; Piazzolla, L.P. Epidemiological Profile of Elderly and Determinants Factors to the Admission in Nursing Homes in the Distrito Federal. Rev. Brasília Médica 2011, 48. [Google Scholar]
- Lini, E.V.; Portella, M.R.; Doring, M. Factors Associated with the Institutionalization of the Elderly: A Case-Control Study. Rev. Bras. Geriatr. Gerontol. 2016, 19, 1004–1014. [Google Scholar] [CrossRef] [Green Version]
- De Medeiros, M.M.D.; Carletti, T.M.; Magno, M.B.; Maia, L.C.; Cavalcanti, Y.W.; Rodrigues-Garcia, R.C.M. Does the Institutionalization Influence Elderly’s Quality of Life? A Systematic Review and Meta-Analysis. BMC Geriatr. 2020, 20, 44. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Stephan, B.C.M.; Rosano, A.; Molfino, A.; Poggiogalle, E.; Lenzi, A.; Siervo, M.; Muscaritoli, M. What Are the Risk Factors for Malnutrition in Older-Aged Institutionalized Adults? Nutrients 2020, 12, 2857. [Google Scholar] [CrossRef]
- Fávaro-Moreira, N.C.; Krausch-Hofmann, S.; Matthys, C.; Vereecken, C.; Vanhauwaert, E.; Declercq, A.; Bekkering, G.E.; Duyck, J. Risk Factors for Malnutrition in Older Adults: A Systematic Review of the Literature Based on Longitudinal Data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef]
- Donini, L.M.; Poggiogalle, E.; Molfino, A.; Rosano, A.; Lenzi, A.; Rossi Fanelli, F.; Muscaritoli, M. Mini-Nutritional Assessment, Malnutrition Universal Screening Tool, and Nutrition Risk Screening Tool for the Nutritional Evaluation of Older Nursing Home Residents. J. Am. Med. Dir. Assoc. 2016, 17, 959.e11–959.e18. [Google Scholar] [CrossRef] [PubMed]
- Rathnayake, K.M.; Wimalathunga, M.; Weech, M.; Jackson, K.G.; Lovegrove, J.A. High Prevalence of Undernutrition and Low Dietary Diversity in Institutionalised Elderly Living in Sri Lanka. Public Health Nutr. 2015, 18, 2874–2880. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lavan, A.H.; Gallagher, P.F.; O’Mahony, D. Methods to Reduce Prescribing Errors in Elderly Patients with Multimorbidity. Clin. Interv. Aging 2016, 11, 857–866. [Google Scholar] [CrossRef] [Green Version]
- Villén, N.; Guisado-Clavero, M.; Guisado-Clavero, M.; Fernández-Bertolín, S.; Fernández-Bertolín, S.; Troncoso-Mariño, A.; Foguet-Boreu, Q.; Foguet-Boreu, Q.; Foguet-Boreu, Q.; Amado, E.; et al. Multimorbidity Patterns, Polypharmacy and Their Association with Liver and Kidney Abnormalities in People over 65 Years of Age: A Longitudinal Study. BMC Geriatr. 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Moreira, F.S.M.; Jerez-Roig, J.; de Brito Macedo Ferreira, L.M.; de Queiroz Medeiros Dantas, A.P.; Lima, K.C.; Ferreira, M.Â.F. Uso de Medicamentos Potencialmente Inapropriados Em Idosos Institucionalizados: Prevalência e Fatores Associados. Cienc. Saude Coletiva 2020, 25, 2073–2082. [Google Scholar] [CrossRef] [PubMed]
- Levy, H.B.; Barney, K.F. Pharmacology, pharmacy, and the aging adult: Implications for occupational therapy. In Occupational Therapy with Aging Adults: Promoting Quality of Life through Collaborative Practice; Elsevier Inc.: St. Louis, MO, USA, 2016; pp. 214–234. ISBN 9780323228169. [Google Scholar]
- Eyigor, S.; Kutsal, Y.G.; Toraman, F.; Durmus, B.; Gokkaya, K.O.; Aydeniz, A.; Paker, N.; Borman, P. Polypharmacy, Physical and Nutritional Status, and Depression in the Elderly: Do Polypharmacy Deserve Some Credits in These Problems? Exp. Aging Res. 2021, 47, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Kose, E.; Wakabayashi, H.; Yasuno, N. Polypharmacy and Malnutrition Management of Elderly Perioperative Patients with Cancer: A Systematic Review. Nutrients 2021, 13, 1961. [Google Scholar] [CrossRef] [PubMed]
- Kushkestani, M. The Relationship Between the Level of Physical Activity and Dementia in Elderly Residents of Nursing Homes in Tehran. Biomed. J. Sci. Tech. Res. 2020, 29. [Google Scholar] [CrossRef]
- Henskens, M.; Nauta, I.M.; van Eekeren, M.C.A.; Scherder, E.J.A. Effects of Physical Activity in Nursing Home Residents with Dementia: A Randomized Controlled Trial. Dement. Geriatr. Cogn. Disord. 2018, 46, 60–80. [Google Scholar] [CrossRef]
- Carvalho, A.; Rea, I.M.; Parimon, T.; Cusack, B.J. Physical Activity and Cognitive Function in Individuals over 60 Years of Age: A Systematic Review. Clin. Interv. Aging 2014, 9, 661. [Google Scholar] [CrossRef] [Green Version]
- Talhaoui, A.; Aboussaleh, Y.; Ahami, A.; Sbaibi, R.; Agoutim, N.; Rouim, F.Z.; Karjouh, K. Association between Physical Activity and Cognitive Function among the Elderly in the Health and Social Centers in Kenitra, Rabat, and Sidi Kacem City (Morocco). Nutr. Metab. Insights 2021, 14, 11786388211026758. [Google Scholar] [CrossRef]
- El Zoghbi, M.; Boulos, C.; Amal, A.H.; Saleh, N.; Awada, S.; Rachidi, S.; Bawab, W.; Salameh, P. Association between Cognitive Function and Nutritional Status in Elderly: A Cross-Sectional Study in Three Institutions of Beirut-Lebanon. Geriatr. Ment. Heal. Care 2013, 1, 73–81. [Google Scholar] [CrossRef]
- Jyväkorpi, S.K.; Pitkälä, K.H.; Puranen, T.M.; Björkman, M.P.; Kautiainen, H.; Strandberg, T.E.; Soini, H.H.; Suominen, M.H. High Proportions of Older People with Normal Nutritional Status Have Poor Protein Intake and Low Diet Quality. Arch. Gerontol. Geriatr. 2016, 67, 40–45. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, A.R.; Dias, C.C.; Fernandes, L. Needs in Nursing Homes and Their Relation with Cognitive and Functional Decline, Behavioral and Psychological Symptoms. Front. Aging Neurosci. 2016, 8, 72. [Google Scholar] [CrossRef] [Green Version]
- Leão, L.L.; Engedal, K.; Monteiro-Junior, R.S.; Tangen, G.G.; Krogseth, M. Malnutrition Is Associated With Impaired Functional Status in Older People Receiving Home Care Nursing Service. Front. Nutr. 2021, 8, 684438. [Google Scholar] [CrossRef] [PubMed]
- Caçador, C.; Teixeira-Lemos, E.; Oliveira, J.; Pinheiro, J.; Mascarenhas-Melo, F.; Ramos, F. The Relationship between Nutritional Status and Functional Capacity: A Contribution Study in Institutionalised Portuguese Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 3789. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Estarli, M.; Barrera, E.S.A.; et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Rev. Esp. Nutr. Humana y Diet. 2016, 20, 148–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; Mckenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ Open 2021, 372, n71. [Google Scholar] [CrossRef]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing Bias in Studies of Prognostic Factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Li, I.C.; Kuo, H.T.; Lin, Y.C. The Mediating Effects of Depressive Symptoms on Nutritional Status of Older Adults in Long-Term Care Facilities. J. Nutr. Health Aging 2013, 17, 633–636. [Google Scholar] [CrossRef]
- Mendonca, N.; Granic, A.; Mathers, J.C.; Martin-Ruiz, C.; Wesnes, K.A.; Seal, C.J.; Jagger, C.; Hill, T.R. One-Carbon Metabolism Biomarkers and Cognitive Decline in the Very Old: The Newcastle 85+Study. J. Am. Med. Dir. Assoc. 2017, 18, 806.e19–806.e27. [Google Scholar] [CrossRef] [Green Version]
- Pedrero-Chamizo, R.; Albers, U.; Palacios, G.; Pietrzik, K.; Meléndez, A.; González-Gross, M. Health Risk, Functional Markers and Cognitive Status in Institutionalized Older Adults: A Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 7303. [Google Scholar] [CrossRef] [PubMed]
- Assis, A.P.M.; de Oliveira, B.T.N.; Gomes, A.L.; Soares, A.D.N.; Guimarães, N.S.; Gomes, J.M.G. The Association between Nutritional Status, Advanced Activities of Daily Living, and Cognitive Function among Brazilian Older Adults Living in Care Homes. Geriatr. Nurs. 2020, 41, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Cereda, E.; Pedrolli, C.; Zagami, A.; Vanotti, A.; Piffer, S.; Faliva, M.; Rondanelli, M.; Caccialanza, R. Nutritional Risk, Functional Status and Mortality in Newly Institutionalised Elderly. Br. J. Nutr. 2013, 110, 1903–1909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira, M.L.A.S.; de Almeida Moreira, P.; De Oliveira, C.C.; Roriz, A.K.C.; Amaral, M.T.R.; Mello, A.L.; Ramos, L.B. Nutritional Status of Institutionalized Elderly Brazilians: A Study with the Mini Nutritional Assessment. Nutr. Hosp. 2015, 31, 1198–1204. [Google Scholar] [CrossRef]
- Serrano-Urrea, R.; García-Meseguer, M.J. Relationships between Nutritional Screening and Functional Impairment in Institutionalized Spanish Older People. Maturitas 2014, 78, 323–328. [Google Scholar] [CrossRef]
- Lauque, S.; Arnaud-Battandier, F.; Mansourian, R.; Guigoz, Y.; Paintin, M.; Nourhashemi, F.; Vellas, B. Protein-Energy Oral Supplementation in Malnourished Nursing-Home Residents. A Controlled Trial. Age Ageing 2000, 29, 51–56. [Google Scholar] [CrossRef] [Green Version]
- de Oliveira, L.F.S.; Wanderley, R.L.; de Medeiros, M.M.D.; de Figueredo, O.M.C.; Pinheiro, M.A.; Rodrigues Garcia, R.C.M.; deAlmeida, L.d.F.D.; Cavalcanti, Y.W. Health-Related Quality of Life of Institutionalized Older Adults: Influence of Physical, Nutritional and Self-Perceived Health Status. Arch. Gerontol. Geriatr. 2021, 92, 104278. [Google Scholar] [CrossRef]
- Nieuwenhuis-Mark, R.E. The Death Knoll for the MMSE: Has It Outlived Its Purpose? J. Geriatr. Psychiatry Neurol. 2010, 23, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Little, M.O. Updates in Nutrition and Polypharmacy. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 4–9. [Google Scholar] [CrossRef]
- Jyrkkä, J.; Enlund, H.; Lavikainen, P.; Sulkava, R.; Hartikainen, S. Association of Polypharmacy with Nutritional Status, Functional Ability and Cognitive Capacity over a Three-Year Period in an Elderly Population. Pharmacoepidemiol. Drug Saf. 2011, 20, 514–522. [Google Scholar] [CrossRef] [PubMed]
| Author /Year | Study Design | Participants | Outcome Measurements | Main Results | |||
|---|---|---|---|---|---|---|---|
| Nutritional Status | Cognitive Function | Functional Capacity | Other | ||||
| Li et al., 2013 [30] | Cross-sectional study | 306 (Mean age: 80.6 ± 7.1, 47.7% female) | MNA | SPMSQ | Modified BI | NA | Both ADLs and depressive symptoms were significantly associated with nutritional status (p < 0.001). |
| Mendonca et al., 2017 [31] | Prospective longitudinal study Follow-up: 1.5, 3, and 5 years | 765 (Age over 85 years old, 66.0% female) | BMI and Biochemical parameters: Baseline RBC folate, plasma vitamin B12, and tHcy concentrations | MMSE | NA | NA | Higher RBC folate and lower tHcy concentration measured at baseline were associated with better global cognition as measured by the MMSE (p < 0.001). |
| Donini et al., 2020 [8] | Cross-sectional study | 246 (Mean age: 80.4 ± 10.5, 66.7% females) | Height, weight, and calf and mid-arm circumference measurements Modified MNA | MMSE | Katz Scale SPPB | Disease-related multi-morbidity: Cumulative Illness Rating Scale | Physical performance, depression and cognitive function ere significantly and positively associated with the M-MNA total score (p < 0.001). |
| Pedrero-Chamizo et al., 2020 [32] | Prospective longitudinal study Follow-up: 1 year | 60 (Mean age: 80.6 ± 9.9, 68.3% females) | Biochemical parameters: Serum cobalamin, Total-cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides, apolipoprotein A1 (ApoA), apolipoprotein B (ApoB), lipoprotein A (LpA), glucose, albumin, and creatinine | MMSE | HGS, Upper body strength (Arm curl test), and Lower body strength (30 s chair stand test) | NA | MMSE scores showed a significant positive correlation with sCbl, HDL-cholesterol, ApoA, and albumin (p < 0.05). Significant negative correlations with HGS were observed for RBC folate, total cholesterol, LDL-cholesterol, and triglycerides. Biomarkers, except HDL-cholesterol lost their association with HGS when observed as covariates. HDL-cholesterol became the sole marker presenting a positive significant association. |
| Assis et al., 2020 [33] | Cross-sectional study | 95 (Mean age: 73.3±12.5, 69.8% female) | MNA Anthropometric values: weight and height (to calculate body mass index—BMI), mid-upper arm circumference (AC), calf circumference (CC), waist circumference (WC), and hip circumference (HC) | MMSE | ADL | NA | The participants with higher scores in MNA (normal and at risk of malnutrition) had higher scores in MMSE compared to malnourished ones (p < 0.001). Participants that practiced more AADLs (9 to 13 activities) had higher MMSE scores (p = 0.031) compared to those that practiced fewer activities. |
| Cereda et al., 2013 [34] | Multicenter prospective cohort study Follow-up: 5 years | 346 (Mean age: 85.7 ± 9.1, 74.6% female) | GNRI | NA | BI | NA | Functional status was significantly associated with nutritional risk by GNRI (p < 0.001). |
| Pereira et al., 2014 [35] | Cross-sectional study | 359 (Mean age: 79.5 ± 9.3, 72.7% female) | MNA | MMSE GDS | Scale of ADL | Presence of comorbidity (hypertension, diabetes mellitus, and dyslipidemia) | Nutritional status was associated with dyslipidemia (p = 0.029), cognitive capacity (p = 0.006), the suspicion of depression (p = 0.048), and functional capacity for ADLs (p < 0.001) |
| Serrano-Urreaand García-Meseguer, 2014 [36] | Cross-sectional study | 895 (Mean age: 82.3 ± 7.1, 58.4% female) | MNA | NA | BI | NA | MNA and the BI scores were positively associated (r = 0.375; p < 0.001) |
| Study | 1 | 2 | 3 | 4 | 5 | 6 | Overall RoB Rating |
|---|---|---|---|---|---|---|---|
| Donini et al. [8] | ++ | + | ++ | ++ | - | + | Low |
| Li et al. [30] | ++ | + | ++ | ++ | - | + | Low |
| Mendonca et al. [31] | ++ | + | ++ | ++ | + | + | Low |
| Pedrero-Chamizo et al., 2020 [32] | + | + | ++ | ++ | + | + | High |
| Assis et al., 2020 [33] | ++ | + | ++ | ++ | - | + | Low |
| Cereda et al., 2013 [34] | + | - | + | + | + | + | High |
| Pereira et al., 2014 [35] | + | - | + | + | + | + | High |
| Serrano-Urrea and García-Meseguer, 2014 [36] | ++ | + | ++ | ++ | - | + | Low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caçador, C.; Teixeira-Lemos, E.; Martins, S.O.; Ramos, F. The Role of Nutritional Status on Polypharmacy, Cognition, and Functional Capacity of Institutionalized Elderly: A Systematic Review. Nutrients 2021, 13, 3477. https://doi.org/10.3390/nu13103477
Caçador C, Teixeira-Lemos E, Martins SO, Ramos F. The Role of Nutritional Status on Polypharmacy, Cognition, and Functional Capacity of Institutionalized Elderly: A Systematic Review. Nutrients. 2021; 13(10):3477. https://doi.org/10.3390/nu13103477
Chicago/Turabian StyleCaçador, Catarina, Edite Teixeira-Lemos, Sofia Oliveira Martins, and Fernando Ramos. 2021. "The Role of Nutritional Status on Polypharmacy, Cognition, and Functional Capacity of Institutionalized Elderly: A Systematic Review" Nutrients 13, no. 10: 3477. https://doi.org/10.3390/nu13103477
APA StyleCaçador, C., Teixeira-Lemos, E., Martins, S. O., & Ramos, F. (2021). The Role of Nutritional Status on Polypharmacy, Cognition, and Functional Capacity of Institutionalized Elderly: A Systematic Review. Nutrients, 13(10), 3477. https://doi.org/10.3390/nu13103477








