The Association between Vitamin D Status and Autism Spectrum Disorder (ASD): A Systematic Review and Meta-Analysis
Abstract
1. Introduction
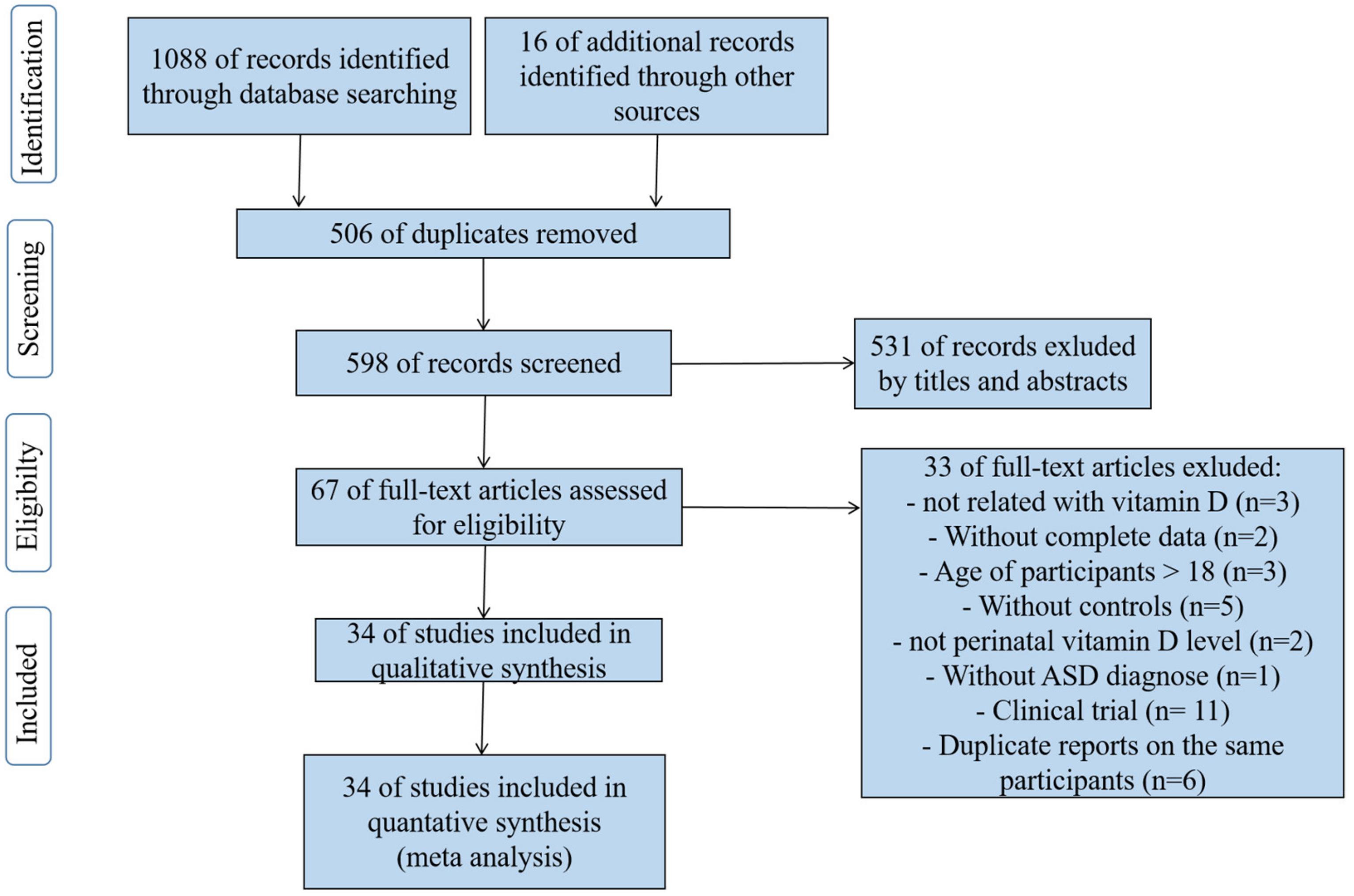
2. Materials and Methods
2.1. Search Strategy and Study Selection
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Study Quality Assessment
2.5. Statistical Analysis
3. Results
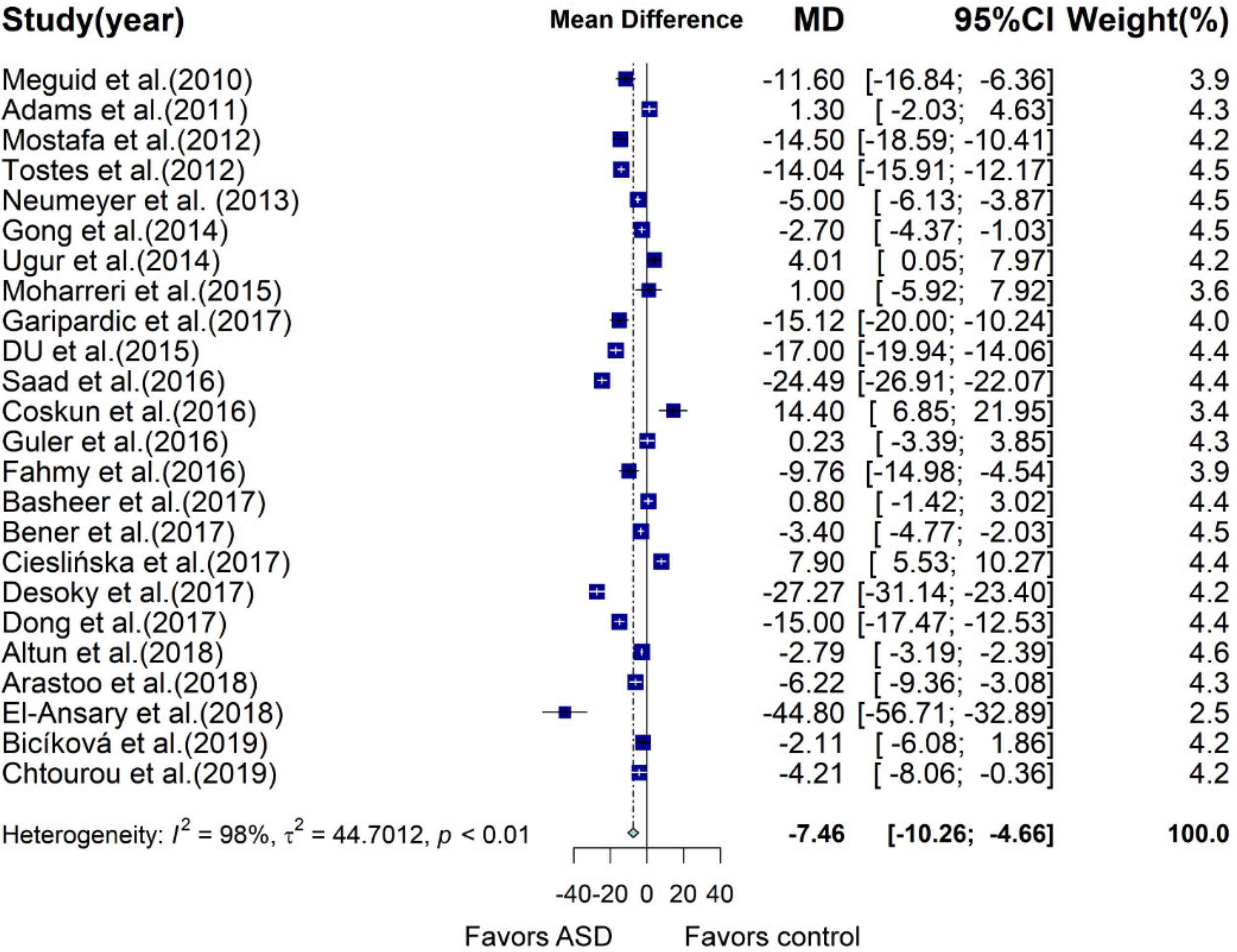
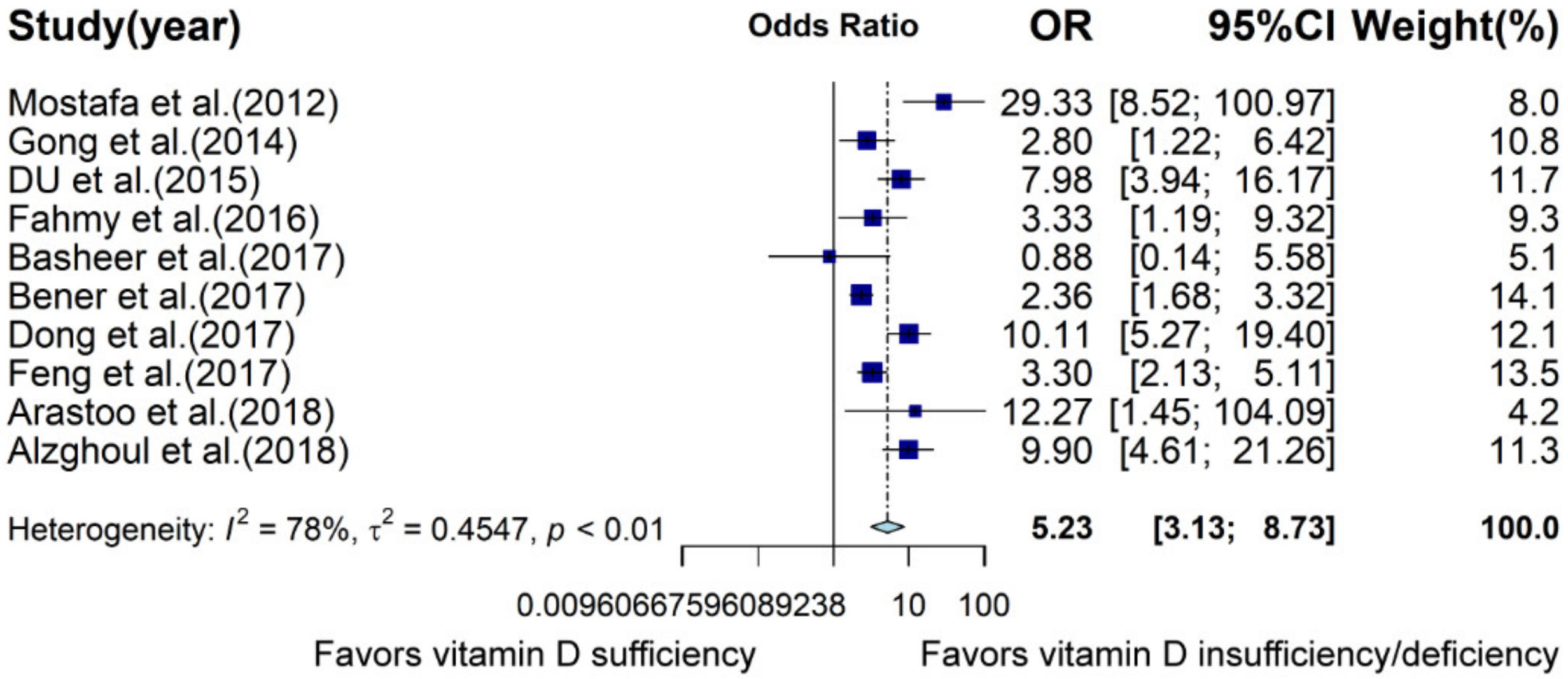
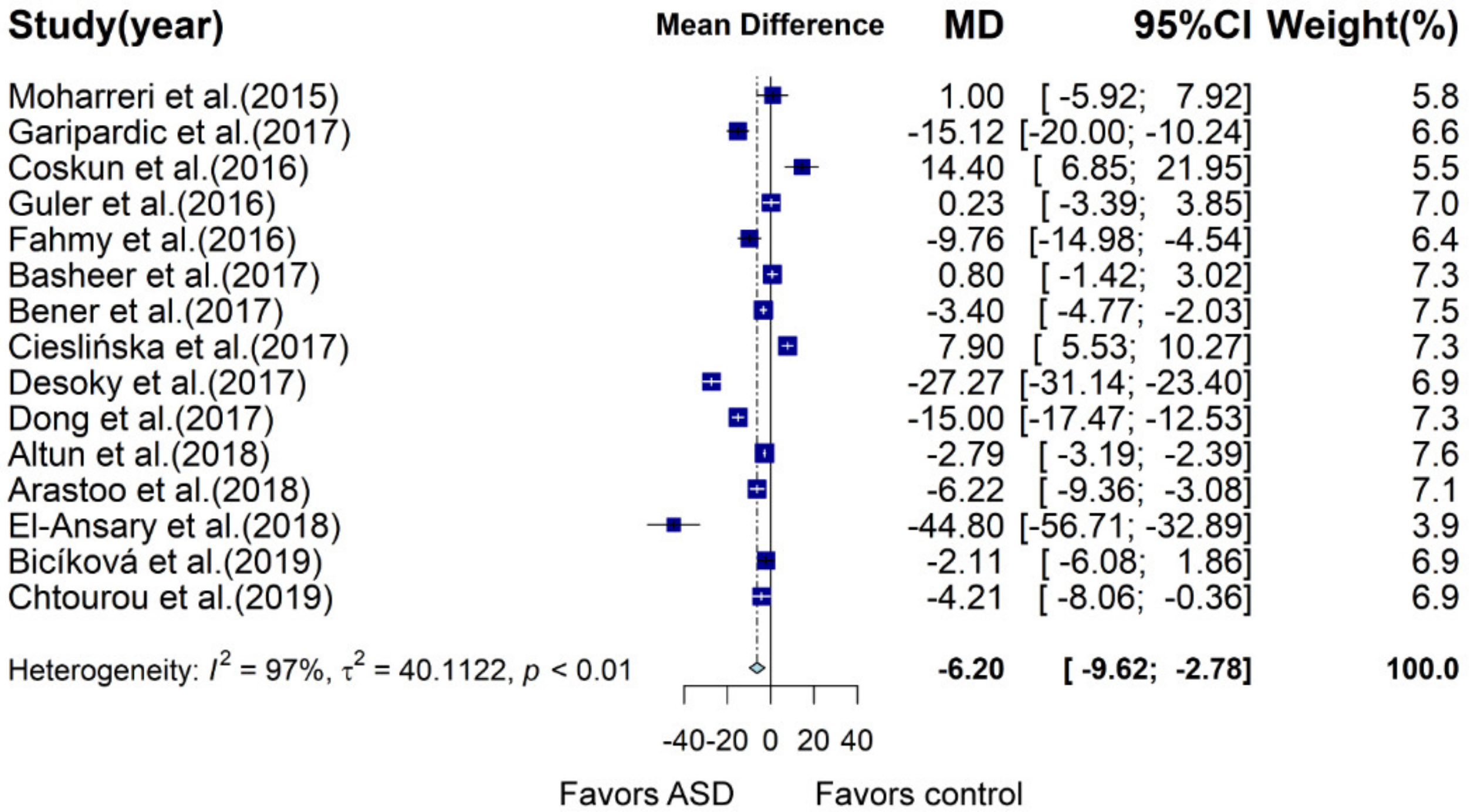
3.1. Meta-Analysis of Case–Control Studies Involving Children and Adolescents
3.2. Meta-Analysis of Case–Control Studies Barring Data from Previous Meta-Analysis
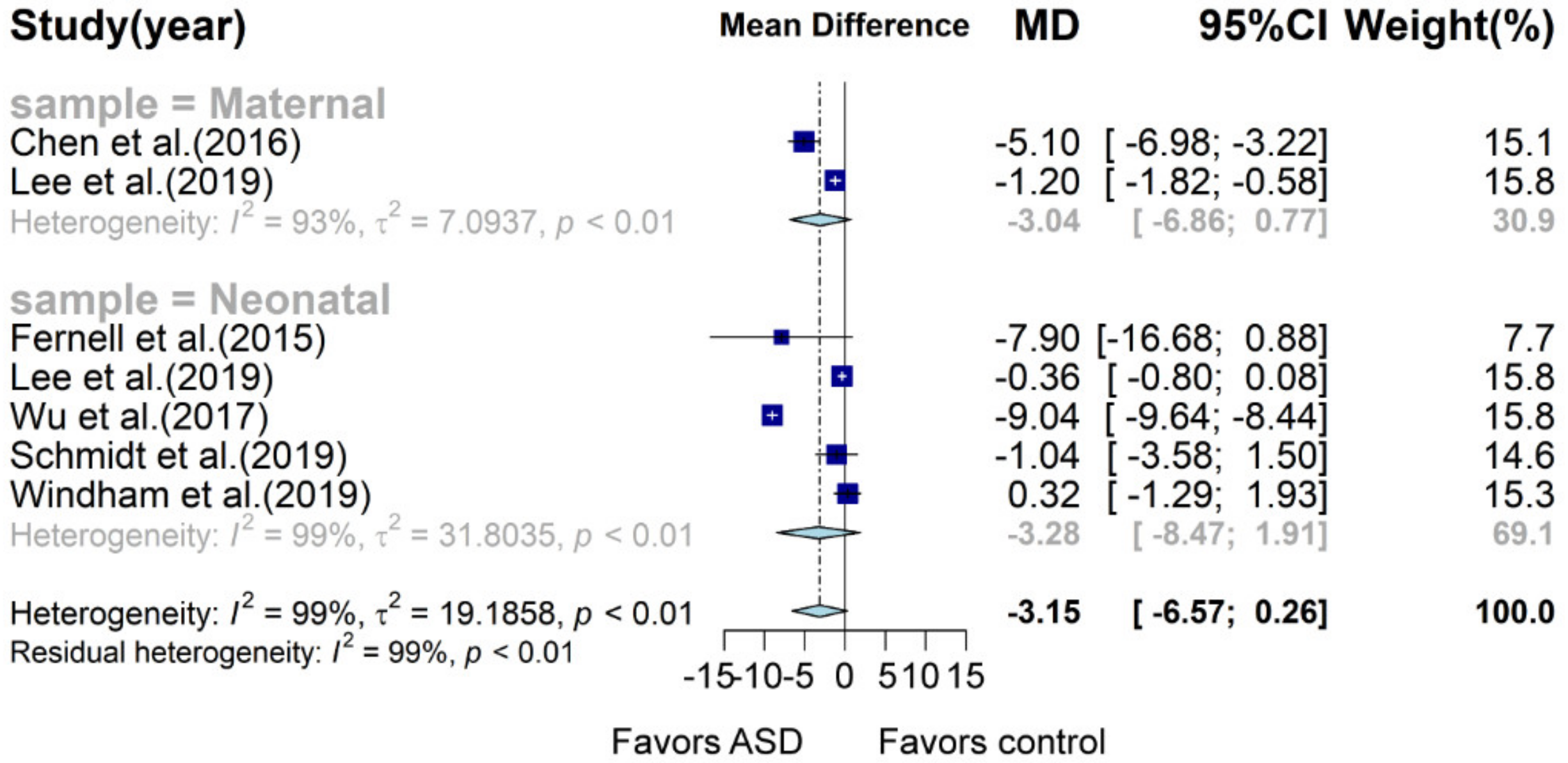
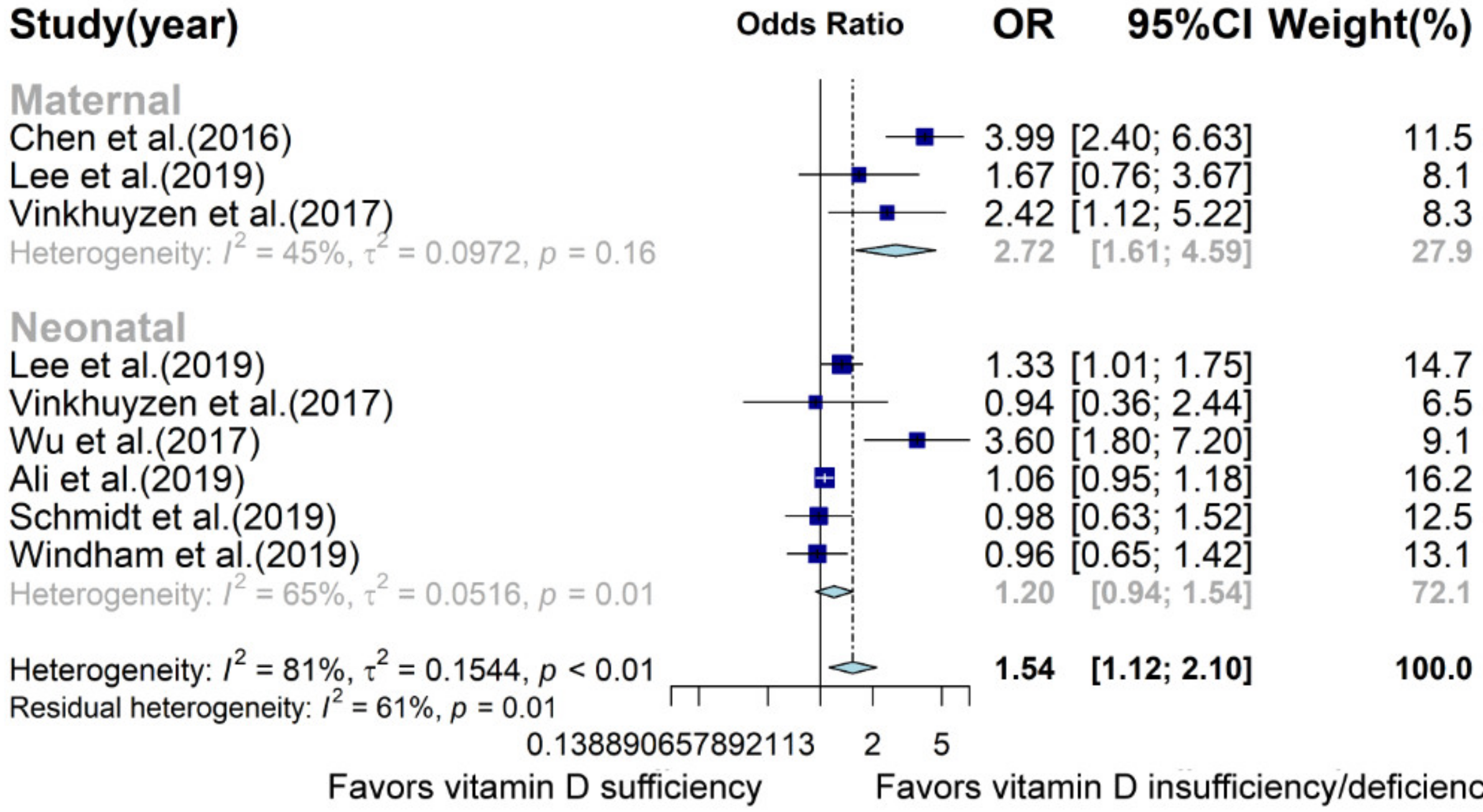
3.3. Meta-Analysis of Prospective Studies about Neonates and Pregnant Women
3.4. Sensitivity Analysis and Publication Bias
4. Discussion
4.1. Implication
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lord, C.; Elsabbagh, M.; Baird, G.; Veenstra-Vanderweele, J. Autism spectrum disorder. Lancet 2018, 392, 508–520. [Google Scholar] [CrossRef]
- Maenner, M.J.; Shaw, K.A.; Baio, J.; Washington, A.; Patrick, M.; DiRienzo, M.; Christensen, D.L.; Wiggins, L.D.; Pettygrove, S.; Andrews, J.G.; et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States. MMWR Surveill. Summ. 2020, 69, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.; Kassee, C.; Besney, R.; Bonato, S.; Hull, L.; Mandy, W.; Szatmari, P.; Ameis, S.H. Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. Lancet Psychiatry 2019, 6, 819–829. [Google Scholar] [CrossRef]
- Landa, R.J. Efficacy of early interventions for infants and young children with, and at risk for, autism spectrum disorders. Int. Rev. Psychiatry 2018, 30, 25–39. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.; Audhya, T.; Matthews, J.S.; Li, K.; Naviaux, J.C.; Naviaux, R.K.; Adams, R.L.; Coleman, D.M.; Quig, D.W.; Geis, E.; et al. Comprehensive Nutritional and Dietary Intervention for Autism Spectrum Disorder—A Randomized, Controlled 12-Month Trial. Nutrients 2018, 10, 369. [Google Scholar] [CrossRef] [PubMed]
- Linhong, Z.; Lin, X.; Wang, M.; Hu, Y.; Xue, K.; Gu, S.; Lv, L.; Huang, S.; Xie, W. Potential role of genomic imprinted genes and brain developmental related genes in autism. BMC Med. Genom. 2020, 13, 54. [Google Scholar] [CrossRef]
- Lord, C.; Brugha, T.S.; Charman, T.; Cusack, J.; Dumas, G.; Frazier, T.; Jones, E.J.H.; Jones, R.M.; Pickles, A.; State, M.W.; et al. Autism spectrum disorder. Nat. Rev. Dis. Prim. 2020, 6, 1–23. [Google Scholar] [CrossRef]
- Mazahery, H.; Camargo, C.A.; Conlon, C.; Beck, K.L.; Kruger, M.C.; Von Hurst, P. Vitamin D and Autism Spectrum Disorder: A Literature Review. Nutrients 2016, 8, 236. [Google Scholar] [CrossRef]
- Saraff, V.; Shaw, N. Sunshine and vitamin D. Arch. Dis. Child. 2016, 101, 190–192. [Google Scholar] [CrossRef]
- Bivona, G.; Gambino, C.M.; Iacolino, G.; Ciaccio, M. Vitamin D and the nervous system. Neurol. Res. 2019, 41, 827–835. [Google Scholar] [CrossRef]
- Landel, V.; Stephan, D.; Cui, X.; Eyles, D.; Féron, F. Differential expression of vitamin D-associated enzymes and receptors in brain cell subtypes. J. Steroid Biochem. Mol. Biol. 2018, 177, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhu, J.; DeLuca, H.F. Where is the vitamin D receptor? Arch. Biochem. Biophys. 2012, 523, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Trifonova, E.A.; Klimenko, A.I.; Mustafin, Z.S.; Lashin, S.A.; Kochetov, A.V. The mTOR Signaling Pathway Activity and Vitamin D Availability Control the Expression of Most Autism Predisposition Genes. Int. J. Mol. Sci. 2019, 20, 6332. [Google Scholar] [CrossRef] [PubMed]
- Meguid, N.A.; Hashish, A.F.; Anwar, M.; Sidhom, G. Reduced Serum Levels of 25-Hydroxy and 1,25-Dihydroxy Vitamin D in Egyptian Children with Autism. J. Altern. Complement. Med. 2010, 16, 641–645. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, G.A.; Al-Ayadhi, L.Y. Reduced serum concentrations of 25-hydroxy vitamin D in children with autism: Relation to autoimmunity. J. Neuroinflammation 2012, 9, 201. [Google Scholar] [CrossRef] [PubMed]
- Tostes, M.H.F.D.S.; Polonini, H.C.; Gattaz, W.F.; Raposo, N.R.B.; Baptista, E.B. Low serum levels of 25-hydroxyvitamin D (25-OHD) in children with autism. Trends Psychiatry Psychother. 2012, 34, 161–163. [Google Scholar] [CrossRef]
- Neumeyer, A.M.; Gates, A.; Ferrone, C.; Lee, H.; Misra, M. Bone Density in Peripubertal Boys with Autism Spectrum Disorders. J. Autism Dev. Disord. 2013, 43, 1623–1629. [Google Scholar] [CrossRef]
- Gong, Z.-L.; Luo, C.-M.; Wang, L.; Shen, L.; Wei, F.; Tong, R.-J.; Liu, Y. Serum 25-hydroxyvitamin D levels in Chinese children with autism spectrum disorders. Neuroreport 2013, 25, 23–27. [Google Scholar] [CrossRef]
- Garipardic, M.; Doğan, M.; Bala, K.A.; Mutluer, T.; Kaba, S.; Aslan, O.; Üstyol, L. Association of Attention Deficit Hyperactivity Disorder and Autism Spectrum Disorders with Mean Platelet Volume and Vitamin D. Med. Sci. Monit. 2017, 23, 1378–1384. [Google Scholar] [CrossRef]
- Du, L.; Shan, L.; Wang, B.; Feng, J.Y.; Xu, Z.D.; Jia, F.Y. Serum levels of 25-hydroxyvitamin D in children with autism spectrum disorders. Chin. J. Contemp. Pediatr. 2015, 17, 68–71. [Google Scholar] [CrossRef]
- Saad, K.; Abdel-Rahman, A.A.; Elserogy, Y.M.; Al-Atram, A.A.; Cannell, J.J.; Bjørklund, G.; Abdel-Reheim, M.K.; Othman, H.A.K.; El-Houfey, A.A.; El-Aziz, N.H.R.A.; et al. Vitamin D status in autism spectrum disorders and the efficacy of vitamin D supplementation in autistic children. Nutr. Neurosci. 2015, 19, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Fahmy, S.F.; Sabri, N.A.; El Hamamsy, M.H.; El Sawi, M.; Zaki, O.K. Vitamin D intake and sun exposure in autistic children. Int. J. Pharm. Sci. Res. 2016, 7, 1043–1049. [Google Scholar] [CrossRef]
- Bener, A.; Khattab, A.O.; Bhugra, D.; Hoffmann, G.F. Iron and vitamin D levels among autism spectrum disorders children. Ann. Afr. Med. 2017, 16, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Desoky, T.; Hassan, M.H.; Fayed, H.M.; Sakhr, H.M. Biochemical assessments of thyroid profile, serum 25-hydroxycholecalciferol and cluster of differentiation 5 expression levels among children with autism. Neuropsychiatr. Dis. Treat. 2017, 13, 2397–2403. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.Y.; Wang, B.; Li, H.H.; Shan, L.; Jia, F.Y. Correlation between serum 25-hydroxyvitamin D level and core symptoms of autism spectrum disorder in children. Chin. J. Pediatr. 2017, 55, 916–919. [Google Scholar]
- Feng, J.; Shan, L.; Du, L.; Wang, B.; Li, H.; Wang, W.; Wang, T.; Dong, H.; Yue, X.; Xu, Z.; et al. Clinical improvement following vitamin D3 supplementation in Autism Spectrum Disorder. Nutr. Neurosci. 2016, 20, 284–290. [Google Scholar] [CrossRef]
- Altun, H.; Kurutaş, E.B.; Şahin, N.; Güngör, O.; Fındıklı, E. The Levels of Vitamin D, Vitamin D Receptor, Homocysteine and Complex B Vitamin in Children with Autism Spectrum Disorders. Clin. Psychopharmacol. Neurosci. 2018, 16, 383–390. [Google Scholar] [CrossRef]
- Arastoo, A.A.; Khojastehkia, H.; Rahimi, Z.; Khafaie, M.A.; Hosseini, S.A.; Mansouri, M.T.; Yosefyshad, S.; Abshirini, M.; Karimimalekabadi, N.; Cheraghi, M.; et al. Evaluation of serum 25-Hydroxy vitamin D levels in children with autism Spectrum disorder. Ital. J. Pediatr. 2018, 44, 150. [Google Scholar] [CrossRef]
- El-Ansary, A.; Cannell, J.J.; Bjørklund, G.; Bhat, R.S.; Al Dbass, A.M.; Alfawaz, H.A.; Chirumbolo, S.; Al-Ayadhi, L. In the search for reliable biomarkers for the early diagnosis of autism spectrum disorder: The role of vitamin D. Metab. Brain Dis. 2018, 33, 917–931. [Google Scholar] [CrossRef]
- Bičíková, M.; Máčová, L.; Ostatníková, D.; Hanzlíková, L. Vitamin D in autistic children and healthy controls. Physiol. Res. 2019, 68, 317–320. [Google Scholar] [CrossRef]
- Chtourou, M.; Naifar, M.; Grayaa, S.; Hajkacem, I.; Ben Touhemi, D.; Ayadi, F.; Moalla, Y. Vitamin d status in TUNISIAN children with autism spectrum disorders. Clin. Chim. Acta 2019, 493, S619–S620. [Google Scholar] [CrossRef]
- Adams, J.B.; Audhya, T.; McDonough-Means, S.; Rubin, R.A.; Quig, D.W.; Geis, E.; Gehn, E.; Loresto, M.; Mitchell, J.; Atwood, S.; et al. Nutritional and metabolic status of children with autism vs. neurotypical children, and the association with autism severity. Nutr. Metab. 2011, 8, 34. [Google Scholar] [CrossRef]
- Uğur, Ç.; Gürkan, C.K. Serum vitamin D and folate levels in children with autism spectrum disorders. Res. Autism Spectr. Disord. 2014, 8, 1641–1647. [Google Scholar] [CrossRef]
- Hashemzadeh, M.; Moharreri, F.; SOltanifar, A. Comparative study of vitamin D levels in children with autism spectrum disorder and normal children: A case-control study. J. Fundam. Ment. Health 2015, 17, 197–201. [Google Scholar]
- Guler, S.; Yesil, G.; Ozdil, M.; Ekici, B.; Onal, H. Sleep disturbances and serum vitamin D levels in children with autism spectrum disorder. Int. J. Clin. Exp. Med. 2016, 9, 14691–14697. [Google Scholar]
- Basheer, S.; Natarajan, A.; Van Amelsvoort, T.; Venkataswamy, M.M.; Ravi, V.; Srinath, S.; Girimaji, S.C.; Christopher, R. Vitamin D status of children with Autism Spectrum Disorder: Case-control study from India. Asian J. Psychiatry 2017, 30, 200–201. [Google Scholar] [CrossRef]
- Cieślińska, A.; Kostyra, E.; Chwała, B.; Moszyńska, M.; Fiedorowicz, E.; Teodorowicz, M.; Savelkoul, H.F. Vitamin D Receptor Gene Polymorphisms Associated with Childhood Autism. Brain Sci. 2017, 7, 115. [Google Scholar] [CrossRef]
- Lee, B.K.; Eyles, D.W.; Magnusson, C.; Newschaffer, C.J.; McGrath, J.; Kvaskoff, D.; Ko, P.; Dalman, C.; Karlsson, H.; Gardner, R.M. Developmental vitamin D and autism spectrum disorders: Findings from the Stockholm Youth Cohort. Mol. Psychiatry 2019, 1–11. [Google Scholar] [CrossRef]
- Vinkhuyzen, A.; Eyles, D.W.; Burne, T.H.J.; Blanken, L.M.; Kruithof, C.J.; Verhulst, F.; Jaddoe, V.W.; Tiemeier, H.; McGrath, J. Gestational vitamin D deficiency and autism-related traits: The Generation R Study. Mol. Psychiatry 2018, 23, 240–246. [Google Scholar] [CrossRef]
- Erratum Re: Relationship Between Neonatal Vitamin D at Birth and Risk of Autism Spectrum Disorders: The NBSIB Study. J. Bone Miner. Res. 2018, 33, 550. [CrossRef]
- Ali, Y.; Anderson, L.N.; Smile, S.; Chen, Y.; Borkhoff, C.M.; Koroshegyi, C.; Lebovic, G.; Parkin, P.C.; Birken, C.S.; Szatmari, P.; et al. Prospective cohort study of vitamin D and autism spectrum disorder diagnoses in early childhood. Autism 2018, 23, 584–593. [Google Scholar] [CrossRef]
- Schmidt, R.J.; Niu, Q.; Eyles, D.W.; Hansen, R.L.; Iosif, A. Neonatal vitamin D status in relation to autism spectrum disorder and developmental delay in the CHARGE case–Control study. Autism Res. 2019, 12, 976–988. [Google Scholar] [CrossRef] [PubMed]
- Windham, G.; Pearl, M.; Anderson, M.C.; Poon, V.; Eyles, D.; Jones, K.L.; Lyall, K.; Kharrazi, M.; Croen, L.A. Newborn vitamin D levels in relation to autism spectrum disorders and intellectual disability: A case–control study in California. Autism Res. 2019, 12, 989–998. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Shan, L.; Du, L.; Feng, J.; Xu, Z.; Staal, W.G.; Yue, X.-J. Serum concentration of 25-hydroxyvitamin D in autism spectrum disorder: A systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 2015, 25, 341–350. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B.; et al. Meta-analysis of Observational Studies in EpidemiologyA Proposal for Reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Ugur, C.; Gurkan, K. Vitamin D levels in children with autism spectrum disorders. Klinik Psikofarmakoloji Bulteni 2014, 24, S117–S118. [Google Scholar]
- Coşkun, S.; Şimşek, Ş.; Camkurt, M.A.; Çim, A.; Çelik, S.B. Association of polymorphisms in the vitamin D receptor gene and serum 25-hydroxyvitamin D levels in children with autism spectrum disorder. Gene 2016, 588, 109–114. [Google Scholar] [CrossRef]
- Alzghoul, L.; Al-Eitan, L.N.; Aladawi, M.; Odeh, M.; Abu Hantash, O. The Association Between Serum Vitamin D3 Levels and Autism Among Jordanian Boys. J. Autism Dev. Disord. 2019, 50, 3149–3154. [Google Scholar] [CrossRef]
- Fernell, E.; Bejerot, S.; Westerlund, J.; Miniscalco, C.; Simila, H.; Eyles, D.W.; Gillberg, C.; Humble, M.B. Autism spectrum disorder and low vitamin D at birth: A sibling control study. Mol. Autism 2015, 6, 1–9. [Google Scholar] [CrossRef]
- Chen, J.; Xin, K.; Wei, J.; Zhang, K.; Xiao, H. Lower maternal serum 25(OH) D in first trimester associated with higher autism risk in Chinese offspring. J. Psychosom. Res. 2016, 89, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Figuerola, P.E.; Canals, J.; Fernández-Cao, J.C.; Val, V.A. Differences in food consumption and nutritional intake between children with autism spectrum disorders and typically developing children: A meta-analysis. Autism 2018, 23, 1079–1095. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Zhan, J.-Y.; Shao, J. Environmental risk factors for autism spectrum disorders in children. Chin. J. Contemp. Pediatr. 2015, 17, 1147–1153. [Google Scholar]
- Schmidt, R.J.; Hansen, R.L.; Hartiala, J.; Allayee, H.; Sconberg, J.L.; Schmidt, L.C.; Volk, H.E.; Tassone, F. Selected vitamin D metabolic gene variants and risk for autism spectrum disorder in the CHARGE Study. Early Hum. Dev. 2015, 91, 483–489. [Google Scholar] [CrossRef]
- Bahrami, A.; Sadeghnia, H.R.; Tabatabaeizadeh, S.-A.; Bahrami-Taghanaki, H.; Behboodi, N.; Esmaeili, H.; Ferns, G.A.; Ghayour-Mobarhan, M.; Avan, A. Genetic and epigenetic factors influencing vitamin D status. J. Cell. Physiol. 2018, 233, 4033–4043. [Google Scholar] [CrossRef]
- Ramos-Lopez, E.; Brück, P.; Jansen, T.; Herwig, J.; Badenhoop, K. CYP2R1 (vitamin D 25-hydroxylase) gene is associated with susceptibility to type 1 diabetes and vitamin D levels in Germans. Diabetes/Metabol. Res. Rev. 2007, 23, 631–636. [Google Scholar] [CrossRef]
- Yıldız, E.P.; Poyrazoglu, Ş.; Bektas, G.; Kardelen, A.D.; Aydinli, N. Potential risk factors for vitamin D levels in medium- and long-term use of antiepileptic drugs in childhood. Acta Neurol. Belg. 2017, 5, 111–453. [Google Scholar] [CrossRef]
- Woon, F.C.; Chin, Y.S.; Ismail, I.H.; Batterham, M.; Latiff, A.H.A.; Gan, W.Y.; Appannah, G.; Hussien, S.H.M.; Edi, M.; Tan, M.L.; et al. Vitamin D deficiency during pregnancy and its associated factors among third trimester Malaysian pregnant women. PLoS ONE 2019, 14, e0216439. [Google Scholar] [CrossRef]
- López-Vicente, M.; Sunyer, J.; Lertxundi, N.; González, L.; Rodríguez-Dehli, C.; Sáenz-Torre, M.E.; Vrijheid, M.; Tardón, A.; Llop, S.; Torrent, M.; et al. Maternal circulating Vitamin D3 levels during pregnancy and behaviour across childhood. Sci. Rep. 2019, 9, 14792. [Google Scholar] [CrossRef]
- Berg, A.O.; Jørgensen, K.N.; Nerhus, M.; Athanasiu, L.; Popejoy, A.B.; Bettella, F.; Norbom, L.C.B.; Gurholt, T.P.; Dahl, S.R.; Andreassen, O.A.; et al. Vitamin D levels, brain volume, and genetic architecture in patients with psychosis. PLoS ONE 2018, 13, e0200250. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D Deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef] [PubMed]
- Lisi, G.; Ribolsi, M.; Siracusano, A.; Niolu, C. Maternal Vitamin D and its Role in Determining Fetal Origins of Mental Health. Curr. Pharm. Des. 2020, 26, 2497–2509. [Google Scholar] [CrossRef] [PubMed]
- Heidari, H.; Amani, R.; Feizi, A.; Askari, G.; Kohan, S.; Tavasoli, P. Vitamin D Supplementation for Premenstrual Syndrome-Related inflammation and antioxidant markers in students with vitamin D deficient: A randomized clinical trial. Sci. Rep. 2019, 9, 14939. [Google Scholar] [CrossRef] [PubMed]
- Kasatkina, L.A.; Tarasenko, A.S.; Krupko, O.A.; Kuchmerovska, T.M.; Lisakovska, O.O.; Trikash, I. Vitamin D deficiency induces the excitation/inhibition brain imbalance and the proinflammatory shift. Int. J. Biochem. Cell Biol. 2020, 119, 105665. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Ma, J.; Huang, R.; Wen, Y.; Liu, G.; Xuan, M.; Yang, L.; Yang, J.; Song, L. Prevalence of vitamin D deficiency in the pregnant women: An observational study in Shanghai, China. Arch. Public Health 2020, 78, 31. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Z.; Ding, R.; Wang, J. The Association between Vitamin D Status and Autism Spectrum Disorder (ASD): A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 86. https://doi.org/10.3390/nu13010086
Wang Z, Ding R, Wang J. The Association between Vitamin D Status and Autism Spectrum Disorder (ASD): A Systematic Review and Meta-Analysis. Nutrients. 2021; 13(1):86. https://doi.org/10.3390/nu13010086
Chicago/Turabian StyleWang, Zuqun, Rui Ding, and Juan Wang. 2021. "The Association between Vitamin D Status and Autism Spectrum Disorder (ASD): A Systematic Review and Meta-Analysis" Nutrients 13, no. 1: 86. https://doi.org/10.3390/nu13010086
APA StyleWang, Z., Ding, R., & Wang, J. (2021). The Association between Vitamin D Status and Autism Spectrum Disorder (ASD): A Systematic Review and Meta-Analysis. Nutrients, 13(1), 86. https://doi.org/10.3390/nu13010086