Prenatal and Postpartum Maternal Iodide Intake from Diet and Supplements, Urinary Iodine and Thyroid Hormone Concentrations in a Region of the United Kingdom with Mild-to-Moderate Iodine Deficiency
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Dietary Assessment
2.3. Iodide Intake from Supplements
2.4. Measurement of Urinary Iodine
2.5. Thyroid Measures
2.6. Statistical Methods
2.7. Sample Size Requirements
3. Results
3.1. Participant Characteristics at Recruitment
3.2. Dietary Intake During Pregnancy
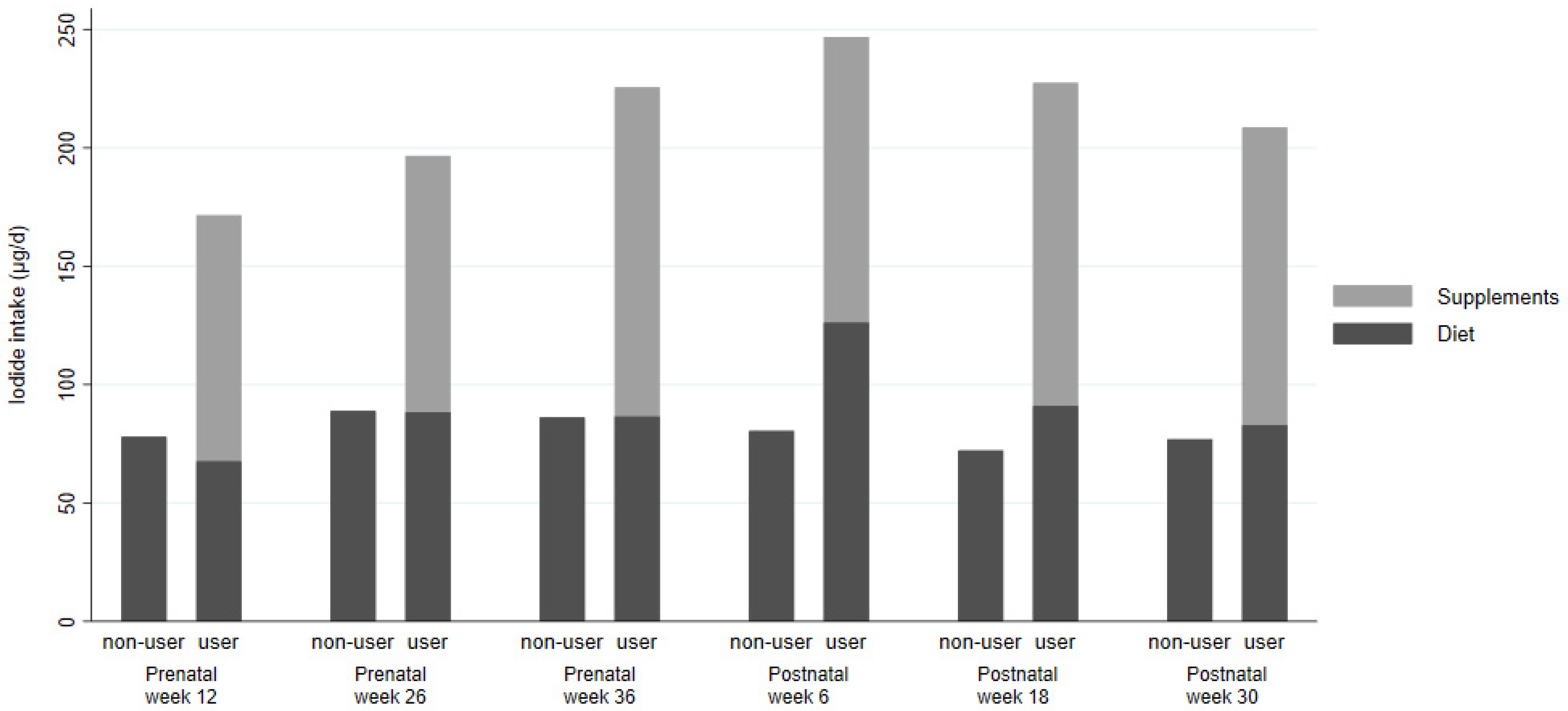
3.3. Supplement Use
3.4. Subgroup Analysis
3.5. Thyroid Hormones, Proteins and Goiter
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Scientific Advisory Committee on Nutrition. SACN Statement on Iodine and Health. 2014. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/339439/SACN_Iodine_and_Health_2014.pdf (accessed on 18 December 2020).
- Zimmermann, M.B. The importance of adequate iodine during pregnancy and infancy. World Rev. Nutr. Diet 2016, 115, 118–124. [Google Scholar] [PubMed]
- World Health Organization. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers, 3rd ed.; 2007; Available online: http://apps.who.int/iris/bitstream/10665/43781/1/9789241595827_eng.pdf (accessed on 18 December 2020).
- Snart, C.J.P.; Threapleton, D.E.; Keeble, C.; Taylor, E.; Waiblinger, D.; Reid, S.; Alwan, N.A.; Mason, D.; Azad, R.; Cade, J.E.; et al. Maternal iodine status, intrauterine growth, birth outcomes and congenital anomalies in a UK birth cohort. BMC Med. 2020, 18, 132. [Google Scholar] [CrossRef] [PubMed]
- Charoenratana, C.; Leelapat, P.; Traisrisilp, K.; Tongsong, T. Maternal iodine insufficiency and adverse pregnancy outcomes. Matern. Child Nutr. 2015, 12, 680–687. [Google Scholar] [CrossRef]
- Alvarez-Pedrerol, M.; Guxens, M.; Mendez, M.; Canet, Y.; Martorell, R.; Espada, M.; Plana, E.; Rebagliato, M.; Sunyer, J. Iodine levels and thyroid hormones in healthy pregnant women and birth weight of their offspring. Eur. J. Endocrinol. 2009, 160, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Murcia, M.; Espada, M.; Julvez, J.; Llop, S.; Lopez-Espinosa, M.-J.; Vioque, J.; Basterrechea, M.; Riaño, I.; González, L.; Alvarez-Pedrerol, M.; et al. Iodine intake from supplements and diet during pregnancy and child cognitive and motor development: The INMA Mother and Child Cohort Study. J. Epidemiol. Community Health 2018, 72, 216–222. [Google Scholar] [CrossRef]
- Bath, S.C.; Steer, C.D.; Golding, J.; Emmett, P.; Rayman, M.P. Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: Results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet 2013, 382, 331–337. [Google Scholar] [CrossRef]
- Markhus, W.M.; Dahl, L.; Moe, V.; Abel, H.M.; Brantsaeter, L.A.; Oyen, J.; Meltzer, M.H.; Stormark, M.K.; Graff, E.I.; Smith, L.; et al. Maternal Iodine Status is Associated with Offspring Language Skills in Infancy and Toddlerhood. Nutrients 2018, 10, 1270. [Google Scholar] [CrossRef] [PubMed]
- Threapleton, D.E.; Snart, C.J.P.; Keeble, C.; Waterman, A.H.; Taylor, E.; Mason, D.; Reid, S.; Azad, R.; Hill, L.J.B.; Meadows, S.; et al. Maternal iodine status in a multi-ethnic UK birth cohort: Associations with child cognitive and educational development. Paediatr. Perinat. Epidemiol. 2020, 12719. [Google Scholar] [CrossRef] [PubMed]
- Snart, C.J.P.; Keeble, C.; Taylor, E.; Cade, J.E.; Stewart, P.M.; Zimmermann, M.B.; Reid, S.; Threapleton, D.E.; Poston, L.; Myers, J.; et al. Maternal Iodine Status and Associations with Birth Outcomes in Three Major Cities in the United Kingdom. Nutrients 2019, 11, 441. [Google Scholar] [CrossRef]
- Torlinska, B.; Bath, S.C.; Janjua, A.; Boelaert, K.; Chan, S.-Y. Iodine Status during Pregnancy in a Region of Mild-to-Moderate Iodine Deficiency is not Associated with Adverse Obstetric Outcomes; Results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Nutrients 2018, 10, 291. [Google Scholar] [CrossRef]
- León, G.; Murcia, M.; Rebagliato, M.; Álvarez-Pedrerol, M.; Castilla, A.M.; Basterrechea, M.; Iñiguez, C.; Fernández-Somoano, A.; Blarduni, E.; Foradada, C.M.; et al. Maternal Thyroid Dysfunction during Gestation, Preterm Delivery, and Birthweight. The Infancia y Medio Ambiente Cohort, Spain. Paediatr. Perinat. Epidemiol. 2015, 29, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Dietary Reference Values for Food Energy and Nutrients for the United Kingdom: Report of the Panel on Dietary Reference Values of the Committee on Medical Aspects of Food Policy; The Stationery Office: London, UK, 1991. [Google Scholar]
- Roberts, C.; Steer, T.; Maplethorpe, N.; Cox, L.; Meadows, S.; Nicholson, S.; Page, P.; Swan, G. National Diet and Nutrition Survey Results from Years 7 and 8 (Combined) of the Rolling Programme (2014/2015 to 2015/2016). 2018. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/699241/NDNS_results_years_7_and_8.pdf (accessed on 18 December 2020).
- Nelson, M.; Erens, B.; Bates, B.; Church, S.; Boshier, T. Low Income Diet and Nutrition Survey: Volume 2 Food Consumption Nutrient Intake; The Stationery Office: London, UK, 2007. [Google Scholar]
- Jiang, H.; Powers, H.J.; Rossetto, G.S. A systematic review of iodine deficiency among women in the UK. Public Health Nutr. 2019, 22, 1138–1147. [Google Scholar] [CrossRef]
- Henjum, S.; Lilleengen, A.M.; Aakre, I.; Dudareva, A.; Gjengedal, E.L.F.; Meltzer, H.M.; Brantsæter, A.L. Suboptimal Iodine Concentration in Breastmilk and Inadequate Iodine Intake among Lactating Women in Norway. Nutrients 2017, 9, 643. [Google Scholar] [CrossRef] [PubMed]
- Groufh-Jacobsen, S.; Mosand, L.M.; Oma, I.; Bakken, K.S.; Solvik, B.S.; Gjengedal, E.L.F.; Brantsæter, A.L.; Strand, T.A.; Henjum, S. Mild to Moderate Iodine Deficiency and Inadequate Iodine Intake in Lactating Women in the Inland Area of Norway. Nutrients 2020, 12, 630. [Google Scholar] [CrossRef] [PubMed]
- Pinchen, H.; Powell, N.; Weiner, D.; Fingas, P. McCance and Widdowson’s Composition of Foods Integrated Dataset 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/788485/McCance_Widdowson_Comp_Foods_Integrated_Dataset_User_Guide_2019__1_.pdf (accessed on 18 December 2020).
- Groufh-Jacobsen, S.; Hess, S.Y.; Aakre, I.; Gjengedal, E.L.F.; Pettersen, K.B.; Henjum, S. Vegans, Vegetarians and Pescatarians Are at Risk of Iodine Deficiency in Norway. Nutrients 2020, 12, 3555. [Google Scholar] [CrossRef]
- Fallon, N.; Dillon, S.A. Low Intakes of Iodine and Selenium Amongst Vegan and Vegetarian Women Highlight a Potential Nutritional Vulnerability. Front. Nutr. 2020, 7, 7. [Google Scholar] [CrossRef]
- Knight, B.A.; Shields, B.M.; He, X.; Pearce, E.N.; Braverman, L.E.; Sturley, R.; Vaidya, B. Iodine deficiency amongst pregnant women in South-West England. Clin. Endocrinol. 2016, 86, 451–455. [Google Scholar] [CrossRef]
- Bath, S.C.; Walter, A.; Taylor, A.; Wright, J.; Rayman, M.P. Iodine deficiency in pregnant women living in the South East of the UK: The influence of diet and nutritional supplements on iodine status. Br. J. Nutr. 2014, 111, 1622–1631. [Google Scholar] [CrossRef]
- Carter, M.C.; Hancock, N.; Albar, S.A.; Brown, H.; Greenwood, D.C.; Hardie, L.J.; Frost, G.S.; Wark, P.A.; Cade, J.E. Development of a New Branded UK Food Composition Database for an Online Dietary Assessment Tool. Nutrients 2016, 8, 480. [Google Scholar] [CrossRef]
- Wark, P.A.; Hardie, L.J.; Frost, G.S.; Alwan, N.A.; Carter, M.; Elliott, P.; Ford, H.E.; Hancock, N.; Morris, M.A.; Mulla, U.Z.; et al. Validity of an online 24-hour recall tool (myfood24) for dietary assessment in population studies: Comparison with biomarkers and standard interviews. BMC Med. 2018, 16, 136. [Google Scholar] [CrossRef]
- Gianfrancesco, C.; Darwin, Z.; McGowan, L.; Smith, D.M.; Haddrill, R.; Carter, M.; Scott, E.M.; Alwan, N.A.; Morris, M.A.; Albar, S.A.; et al. Exploring the Feasibility of Use of An Online Dietary Assessment Tool (myfood24) in Women with Gestational Diabetes. Nutrients 2018, 10, 1147. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Peng, S.; Zhang, X.; Xie, X.; Wang, D.; Mao, J.; Teng, X.; Shan, Z.; Teng, W. The Urine Iodine to Creatinine as an Optimal Index of Iodine During Pregnancy in an Iodine Adequate Area in China. J. Clin. Endocrinol. Metab. 2016, 101, 1290–1298. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; International Council for Control of Iodine Deficiency Disorders; United Nations Children’s Fund (UNICEF). Indicators for Assessing Iodine Deficiency Disorders and Their Control through Salt Iodization. Micronutrient Series 1994. Available online: https://apps.who.int/iris/handle/10665/70715 (accessed on 18 December 2020).
- Peterson, S.; Sanga, A.; Eklöf, H.; Bunga, B.; Taube, A.; Gebre-Medhin, M.; Rosling, H. Classification of thyroid size by palpation and ultrasonography in field surveys. Lancet 2000, 355, 106–110. [Google Scholar] [CrossRef]
- Stolwijk, A.M.; Straatman, H.; Zielhuis, G.A. Studying seasonality by using sine and cosine functions in regression analysis. J. Epidemiol. Community Health 1999, 53, 235–238. [Google Scholar] [CrossRef] [PubMed]
- König, F.; Andersson, M.; Hotz, K.; Aeberli, I.; Zimmermann, M.B. Ten Repeat Collections for Urinary Iodine from Spot Samples or 24-Hour Samples Are Needed to Reliably Estimate Individual Iodine Status in Women. J. Nutr. 2011, 141, 2049–2054. [Google Scholar] [CrossRef] [PubMed]
- Combet, E.; Bouga, M.; Pan, B.; Lean, M.E.J.; Christopher, C.O. Iodine and pregnancy—A UK cross-sectional survey of dietary intake, knowledge and awareness. Br. J. Nutr. 2015, 114, 108–117. [Google Scholar] [CrossRef]
- Alwan, N.; Greenwood, D.; Simpson, N.; McArdle, H.; Cade, J.E. The relationship between dietary supplement use in late pregnancy and birth outcomes: A cohort study in British women. BJOG Int. J. Obstet. Gynaecol. 2010, 117, 821–829. [Google Scholar] [CrossRef]
- Moleti, M.; Presti, V.P.L.; Campolo, M.C.; Mattina, F.; Galletti, M.; Mandolfino, M.; Violi, M.A.; Giorgianni, G.; De Domenico, D.; Trimarchi, F.; et al. Iodine Prophylaxis Using Iodized Salt and Risk of Maternal Thyroid Failure in Conditions of Mild Iodine Deficiency. J. Clin. Endocrinol. Metab. 2008, 93, 2616–2621. [Google Scholar] [CrossRef]
- Bath, S.C.; Sleeth, M.L.; McKenna, M.; Walter, A.; Taylor, A.; Rayman, M.P. Iodine intake and status of UK women of childbearing age recruited at the University of Surrey in the winter. Br. J. Nutr. 2014, 112, 1715–1723. [Google Scholar] [CrossRef]
- Bath, S.C.; Furmidge-Owen, V.L.; Redman, C.W.; Rayman, M.P. Gestational changes in iodine status in a cohort study of pregnant women from the United Kingdom: Season as an effect modifier. Am. J. Clin. Nutr. 2015, 101, 1180–1187. [Google Scholar] [CrossRef]
- Caldwell, K.L.; Makhmudov, A.; Jones, R.L.; Hollowell, J.G. EQUIP: A worldwide program to ensure the quality of urinary iodine procedures. Accredit. Qual. Assur. 2005, 10, 356–361. [Google Scholar] [CrossRef]
- Knudsen, N.; Christiansen, E.; Brandt-Christensen, M.; Nygaard, B.; Perrild, H. Age- and sex-adjusted iodine/creatinine ratio. A new standard in epidemiological surveys? Evaluation of three different estimates of iodine excretion based on casual urine samples and comparison to 24 h values. Eur. J. Clin. Nutr. 2000, 54, 361–363. [Google Scholar] [CrossRef] [PubMed]
- Vejbjerg, P.; Knudsen, N.; Perrild, H.; Laurberg, P.; Andersen, S.; Rasmussen, L.B.; Ovesen, L.; Jørgensen, T. Estimation of Iodine Intake from Various Urinary Iodine Measurements in Population Studies. Thyroid 2009, 19, 1281–1286. [Google Scholar] [CrossRef] [PubMed]
- Knuppel, R.A.; Sbarra, A.J.; Cetrulo, C.L.; Kappy, K.A.; Ingardia, C.J.; Selvaraj, R.J. 24-hour urine creatinine excretion in pregnancy. Obstet. Gynecol. 1979, 54, 327–329. [Google Scholar]

| Total Iodide Intake (Diet + Supplements) | ||||
|---|---|---|---|---|
| Participant Characteristics | All | Lower Third (<91 µg/d) | Middle Third (91–162 µg/d) | Upper Third (>162 µg/d) |
| (n = 246) 2 | (n = 82) | (n = 81) | (n = 81) | |
| Total iodide intake (µg/d) geometric mean (95% CI) | 111 (100, 124) | 43 (37, 51) | 126 (121, 131) | 253 (233, 276) |
| Total iodide intake (µg/d) median (IQR) | 129 (73, 196) | 56 (28, 73) | 129 (111, 148) | 239 (196, 293) |
| Age (years) median (IQR) | 31 (27, 34) | 30 (26, 34.5) | 31 (28, 34) | 31 (28, 34) |
| BMI (kg/m2) median (IQR) | 27 (23, 31) | 29 (24, 31) | 27 (23, 30) | 26 (23, 30) |
| First pregnancy, n (%) | 79 (32) | 28 (34) | 21 (26) | 29 (36) |
| Smoked in first trimester, n (%) | 15 (6) | 8 (10) | 3 (4) | 4 (5) |
| Alcohol in first trimester, n (%) | 17 (7) | 3 (4) | 5 (6) | 9 (11) |
| Vegan or vegetarian, n (%) 3 | 11 (4) | 3 (4) | 5 (6) | 3 (4) |
| Ethnic background, n (%) | ||||
| White British and European | 89 (36) | 29 (35) | 24 (30) | 36 (44) |
| Pakistani | 131 (53) | 42 (51) | 50 (62) | 37 (46) |
| Other | 26 (11) | 11 (13) | 7 (9) | 8 (10) |
| Highest education level, n (%) 4 | ||||
| <5 GCSEs or equivalent | 32 (13) | 12 (15) | 14 (17) | 6 (7) |
| 5+ GCSEs or equivalent | 58 (24) | 23 (28) | 17 (21) | 18 (22) |
| A-level equivalent | 43 (17) | 12 (15) | 15 (19) | 16 (20) |
| Higher than A-level | 105 (43) | 33 (40) | 30 (37) | 39 (48) |
| Other/Don’t know | 8 (3) | 2 (2) | 5 (6) | 2 (2) |
| NS-SEC (n (%)) 5 | ||||
| Managerial, administrative and professional | 81 (33) | 27 (33) | 21 (26) | 33 (41) |
| Intermediate occupations or small employers and own account workers | 40 (16) | 10 (12) | 18 (22) | 12 (15) |
| Lower supervisory and technical or semi-routine and routine | 42 (17) | 13 (16) | 14 (17) | 15 (19) |
| Never worked | 83 (34) | 32 (39) | 28 (35) | 21 (26) |
| TSH (µIU/mL) median (IQR) | 1.15 (0.81, 1.75) | 1.15 (0.87, 1.70) | 1.07 (0.71, 1.50) | 1.31 (0.86, 1.93) |
| Tg (µg/L) median (IQR) | 6.21 (2.64, 12.38) | 5.55 (2.79, 10.90) | 8.69 (2.38, 20.88) | 5.87 (2.50, 12.18) |
| fT3 (pg/mL) median (IQR) | 2.49 (2.11, 2.87) | 2.47 (2.15, 3.00) | 2.49 (2.09, 2.77) | 2.48 (2.07, 2.91) |
| fT4 (pg/mL) median (IQR) | 9.69 (8.31, 11.27) | 9.65 (8.23, 11.16) | 9.43 (8.35, 10.96) | 9.84 (8.20, 11.51) |
| During Pregnancy | Postpartum | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Visit 1 12 Weeks’ Gestation | Visit 2 26 Weeks’ Gestation | Visit 3 36 Weeks’ Gestation | Visits 1–3 1 | Visit 4 6 Weeks Postpartum | Visit 5 18 Weeks Postpartum | Visit 6 30 Weeks Postpartum | Visits 4–6 1 | All Visits 1 | |
| (n = 244) | (n = 217) | (n = 206) | (n = 246) | (n = 206) | (n = 193) | (n = 192) | (n = 225) | (n = 246) | |
| Total iodide intake from dietary sources (food and drink) and supplements (µg/d) | |||||||||
| Geometric mean 2,3 (95% CI) | 111 (100, 124) | 127 (114, 141) | 112 (99, 128) | 136 (126, 146) | 89 (79, 100) | 76 (65, 88) | 81 (71, 92) | 98 (89, 107) | 125 (118, 134) |
| Median (IQR) | 129 (73, 196) | 148 (76, 216) | 134 (73, 218) | 143 (94, 196) | 105 (47, 164) | 90 (41, 145) | 87 (42, 149) | 104 (64, 152) | 132 (90, 173) |
| Iodide intake from dietary sources (food and drink) only (µg/d) | |||||||||
| Geometric mean 2,3 (95% CI) | 74 (66, 82) | 89 (79, 99) | 86 (75, 98) | 96 (89, 105) | 84 (75, 94) | 73 (63, 85) | 78 (68, 88) | 93 (85, 102) | 101 (94, 108) |
| Median (IQR) | 83 (46, 134) | 89 (54, 152) | 99 (57, 157) | 101 (64, 142) | 98 (45, 147) | 86 (38, 144) | 122 (41, 143) | 100 (64, 149) | 104 (69, 138) |
| Proportion of dietary iodide from each food source (%) | |||||||||
| Dairy | 38% | 41% | 43% | 42% | 40% | 34% | 35% | 38% | 41% |
| Dairy with cereal | 12% | 9% | 12% | 11% | 12% | 12% | 12% | 12% | 12% |
| Eggs | 13% | 11% | 12% | 12% | 11% | 12% | 13% | 13% | 13% |
| Cereals | 6% | 6% | 4% | 5% | 6% | 6% | 5% | 5% | 4% |
| White Fish | 5% | 7% | 7% | 9% | 5% | 7% | 6% | 10% | 12% |
| Other seafood | 2% | 1% | 2% | 2% | 1% | 2% | 1% | 1% | 2% |
| Poultry and red meat | 11% | 12% | 10% | 10% | 15% | 15% | 17% | 12% | 9% |
| Fruit, vegetables and pulses | 10% | 8% | 9% | 7% | 6% | 10% | 8% | 6% | 6% |
| Confectionery | 2% | 3% | 1% | 2% | 3% | 2% | 1% | 2% | 2% |
| Other | 1% | 1% | 1% | 1% | 1% | 1% | <1% | 1% | 1% |
| Fish consumption (n (%)) 4 | |||||||||
| Any white fish (n (%)) | 16 (7%) | 22 (10%) | 20 (10%) | 50 (20%) | 16 (8%) | 16 (8%) | 18 (9%) | 42 (19%) | 80 (33%) |
| Iodide intake from fish in fish consumers (µg/d) | |||||||||
| Geometric mean 2,3 (95% CI) | 159 (85, 297) | 178 (122, 262) | 187 (127, 274) | 67 (49, 90) | 138 (87, 218) | 302 (201, 454) | 178 (114, 279) | 81 (60, 110) | 41 (32 to 51) |
| Supplement use (n (%)) | |||||||||
| Used any supplement | 220 (89%) | 183 (84%) | 159 (77%) | 230 (94%) | 63 (31%) | 39 (20%) | 26 (14%) | 54 (24%) | 233 (95%) |
| Used any supplement containing iodide | 110 (45%) | 98 (45%) | 57 (28%) | 160 (65%) | 17 (8%) | 8 (4%) | 8 (4%) | 23 (10%) | 163 (66%) |
| Iodide intake from supplements (µg/d) geometric mean 2,3 (95% CI) | |||||||||
| In iodide supplement users 5 | 87 (77, 97) | 89 (81, 98) | 120 (111, 130) | 54 (48, 60) | 93 (63, 136) | 118 (93, 150) | 120 (80, 179) | 52 (38, 72) | 31 (28, 35) |
| Proportion of total iodide intake from supplements (%) | |||||||||
| In all participants | 25% | 23% | 16% | 25% | 4% | 2% | 2% | 4% | 17% |
| In iodide supplement users 5 | 55% | 51% | 56% | 38% | 45% | 55% | 59% | 34% | 26% |
| Urinary iodine concentration (µg/L) | |||||||||
| Geometric mean (95% CI) | 123 (111, 138) | 107 (96,121) | 127 (112, 143) | 131 (121, 143) | 92 (82, 104) | 114 (103, 126) | 128 (115, 143) | 119 (109, 130) | 133 (124, 142) |
| Median (IQR) | 122 (77, 212) | 122 (70, 176) | 129 (75, 234) | 135 (90, 207) | 96 (56, 153) | 114 (74, 171) | 139 (83, 220) | 121 (77, 190) | 143 (90, 195) |
| Iodine/creatinine (µg/g) | |||||||||
| Geometric mean (95% CI) | 123 (112, 134) | 109 (101, 118) | 137 (125, 151) | 128 (119, 137) | 97 (88, 108) | 96 (87, 106) | 107 (97, 118) | 106 (98, 115) | 120 (114, 128) |
| Median (IQR) | 120 (75, 200) | 104 (73, 150) | 136 (91, 223) | 126 (88, 187) | 99 (61, 162) | 94 (64, 147) | 104 (71, 168) | 111 (72, 160) | 121 (90, 163) |
| All n = 246 | Pakistani n = 131 | White European n = 89 | Other n = 26 | |||
|---|---|---|---|---|---|---|
| Total iodide intake (µg/d) | All visits | Geometric mean (95% CI) | 125 (118, 134) | 117 (108, 127) | 133 (121, 147) | 143 (102, 199) |
| Median (IQR) | 132 (90, 173) | 123 (81, 162) | 138 (108, 182) | 146 (98, 285) | ||
| Antenatal visits | Geometric mean (95% CI) | 136 (126, 146) | 126 (114, 139) | 150 (134, 168) | 139 (101, 192) | |
| Median (IQR) | 143 (94, 196) | 129 (87, 190) | 159 (114, 215) | 142 (112, 226) | ||
| Postnatal visits | Geometric mean (95% CI) | 98 (89, 107) | 89 (78, 100) | 102 (89, 116) | 151 (103, 222) | |
| Median (IQR) | 104 (64, 152) | 91 (60, 144) | 110 (69, 151) | 180 (81, 242) | ||
| Total iodide intake < UK RNI (140 µg/day) | Any visits | n (%) | 145 (59%) | 86 (66%) | 46 (52%) | 13 (50%) |
| Antenatal visits | n (%) | 119 (48%) | 74 (56%) | 33 (37%) | 12 (46%) | |
| Postnatal visits | n (%) | 160 (71%) | 91 (75%) | 59 (72%) | 10 (48%) | |
| Dietary iodide (µg/d) | All visits | Geometric mean (95% CI) | 101 (94, 108) | 96 (88, 105) | 103 (94, 114) | 119 (84, 169) |
| Median (IQR) | 104 (69, 138) | 97 (66, 132) | 111 (79, 140) | 130 (72, 218) | ||
| Antenatal visits | Geometric mean (95% CI) | 96 (89, 105) | 92 (82, 102) | 103 (91, 117) | 99 (69, 141) | |
| Median (IQR) | 101 (64, 142) | 91 (63, 132) | 114 (69, 153) | 91 (66, 173) | ||
| Postnatal visits | Geometric mean (95% CI) | 93 (85, 102) | 86 (76, 97) | 93 (82, 106) | 151 (103, 222) | |
| Median (IQR) | 100 (64, 149) | 87 (59, 141) | 104 (67, 143) | 180 (81, 242) | ||
| Used any supplement containing iodide | Any visits | n (%) | 163 (66%) | 84 (64%) | 64 (72%) | 15 (58%) |
| Antenatal visits | n (%) | 160 (65%) | 82 (63%) | 63 (71%) | 15 (58%) | |
| Postnatal visits | n (%) | 23 (10%) | 9 (7%) | 14 (17%) | 0 (0%) | |
| Iodide from supplements in any users of supplements containing iodide 1 (µg/d) | All visits | Geometric mean (95% CI) | 31 (28, 35) | 29 (25, 34) | 35 (28, 42) | 29 (17, 48) |
| Median (IQR) | 32 (20, 52) | 29 (18, 45) | 35 (22, 62) | 33 (21, 52) | ||
| Antenatal visits | Geometric mean (95% CI) | 54 (48, 60) | 51 (44, 58) | 58 (49, 69) | 51 (31, 83) | |
| Median (IQR) | 54 (36, 89) | 50 (36, 75) | 60 (36, 100) | 62 (36, 96) | ||
| Postnatal visits | Geometric mean (95% CI) | 52 (38, 72) | 46 (23, 93) | 56 (38, 83) | / | |
| Median (IQR) | 56 (36, 98) | 56 (36, 88) | 57 (40, 99) | / |
| UIC | I/Cr | TSH | Tg | fT3 | fT4 | fT3/fT4 | Palpable Goiter 1,2 | ||
|---|---|---|---|---|---|---|---|---|---|
| All visits | Total iodide intake | 3% (1 to 5) | 7% (5 to 9) | 1% (−1 to 2) | −4% (−6 to −2) | −1% (−2 to 0) | 0% (−1 to 1) | −1% (−1 to 0) | −5% (−18 to 8) |
| Dietary iodide | 2% (0 to 4) | 5% (3 to 6) | 1% (0 to 3) | −2% (−5 to 0) | 0% (−1 to 1) | 0% (−1 to 0) | 0% (−1 to 1) | −6% (−19 to 8) | |
| Iodide from supplements | 6% (1 to 11) | 11% (7 to 15) | −3% (−6 to 0) | −12% (−17 to −7) | −5% (−7 to −4) | 1% (−1 to 2) | −6% (−8 to −4) | −12% (−37 to 13) | |
| Antenatal visits | Total iodide intake | 4% (1 to 7) | 5% (3 to 7) | 1% (0 to 3) | −1% (−4 to 3) | 0% (−1 to 1) | 0% (−1 to 1) | 0% (−1 to 1) | −21% (−32 to −9) |
| Dietary iodide | 3% (0 to 6) | 4% (2 to 7) | 2% (0 to 4) | −1% (−5 to 2) | 0% (−1 to 1) | −1% (−2 to 0) | 1% (0 to 2) | −31% (−44 to −18) | |
| Iodide from supplements | 5% (−1 to 10) | 8% (4 to 13) | −2% (−5 to 2) | 4% (−3 to 10) | 1% (−1 to 3) | 2% (0 to 4) | −1% (−3 to 1) | 12% (−20 to 44) | |
| Postnatal visits | Total iodide intake | 1% (−1 to 4) | 3% (0 to 5) | −1% (−3 to 2) | −2% (−5 to 2) | 1% (0 to 2) | 0% (−1 to 2) | 0% (−1 to 2) | / |
| Dietary iodide | 2% (−1 to 4) | 3% (0 to 6) | 0% (−3 to 3) | −2% (−6 to 2) | 1% (0 to 2) | 0% (−1 to 2) | 0% (−1 to 2) | / | |
| Iodide from supplements | 2% (−9 to 13) | 4% (−5 to 13) | −12% (−23 to −2) | 4% (−11 to 20) | 0% (−4 to 4) | 2% (−3 to 7) | −1% (−8 to 6) | / |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Threapleton, D.E.; Waiblinger, D.; Snart, C.J.P.; Taylor, E.; Keeble, C.; Ashraf, S.; Bi, S.; Ajjan, R.; Azad, R.; Hancock, N.; et al. Prenatal and Postpartum Maternal Iodide Intake from Diet and Supplements, Urinary Iodine and Thyroid Hormone Concentrations in a Region of the United Kingdom with Mild-to-Moderate Iodine Deficiency. Nutrients 2021, 13, 230. https://doi.org/10.3390/nu13010230
Threapleton DE, Waiblinger D, Snart CJP, Taylor E, Keeble C, Ashraf S, Bi S, Ajjan R, Azad R, Hancock N, et al. Prenatal and Postpartum Maternal Iodide Intake from Diet and Supplements, Urinary Iodine and Thyroid Hormone Concentrations in a Region of the United Kingdom with Mild-to-Moderate Iodine Deficiency. Nutrients. 2021; 13(1):230. https://doi.org/10.3390/nu13010230
Chicago/Turabian StyleThreapleton, Diane E., Dagmar Waiblinger, Charles J.P. Snart, Elizabeth Taylor, Claire Keeble, Samina Ashraf, Shazia Bi, Ramzi Ajjan, Rafaq Azad, Neil Hancock, and et al. 2021. "Prenatal and Postpartum Maternal Iodide Intake from Diet and Supplements, Urinary Iodine and Thyroid Hormone Concentrations in a Region of the United Kingdom with Mild-to-Moderate Iodine Deficiency" Nutrients 13, no. 1: 230. https://doi.org/10.3390/nu13010230
APA StyleThreapleton, D. E., Waiblinger, D., Snart, C. J. P., Taylor, E., Keeble, C., Ashraf, S., Bi, S., Ajjan, R., Azad, R., Hancock, N., Mason, D., Reid, S., Cromie, K. J., Alwan, N. A., Zimmermann, M., Stewart, P. M., Simpson, N. A. B., Wright, J., Cade, J. E., ... Greenwood, D. C. (2021). Prenatal and Postpartum Maternal Iodide Intake from Diet and Supplements, Urinary Iodine and Thyroid Hormone Concentrations in a Region of the United Kingdom with Mild-to-Moderate Iodine Deficiency. Nutrients, 13(1), 230. https://doi.org/10.3390/nu13010230





