Dietary Patterns and Progression of Impaired Kidney Function in Japanese Adults: A Longitudinal Analysis for the Fukushima Health Management Survey, 2011–2015
Abstract
1. Introduction
2. Materials and Methods
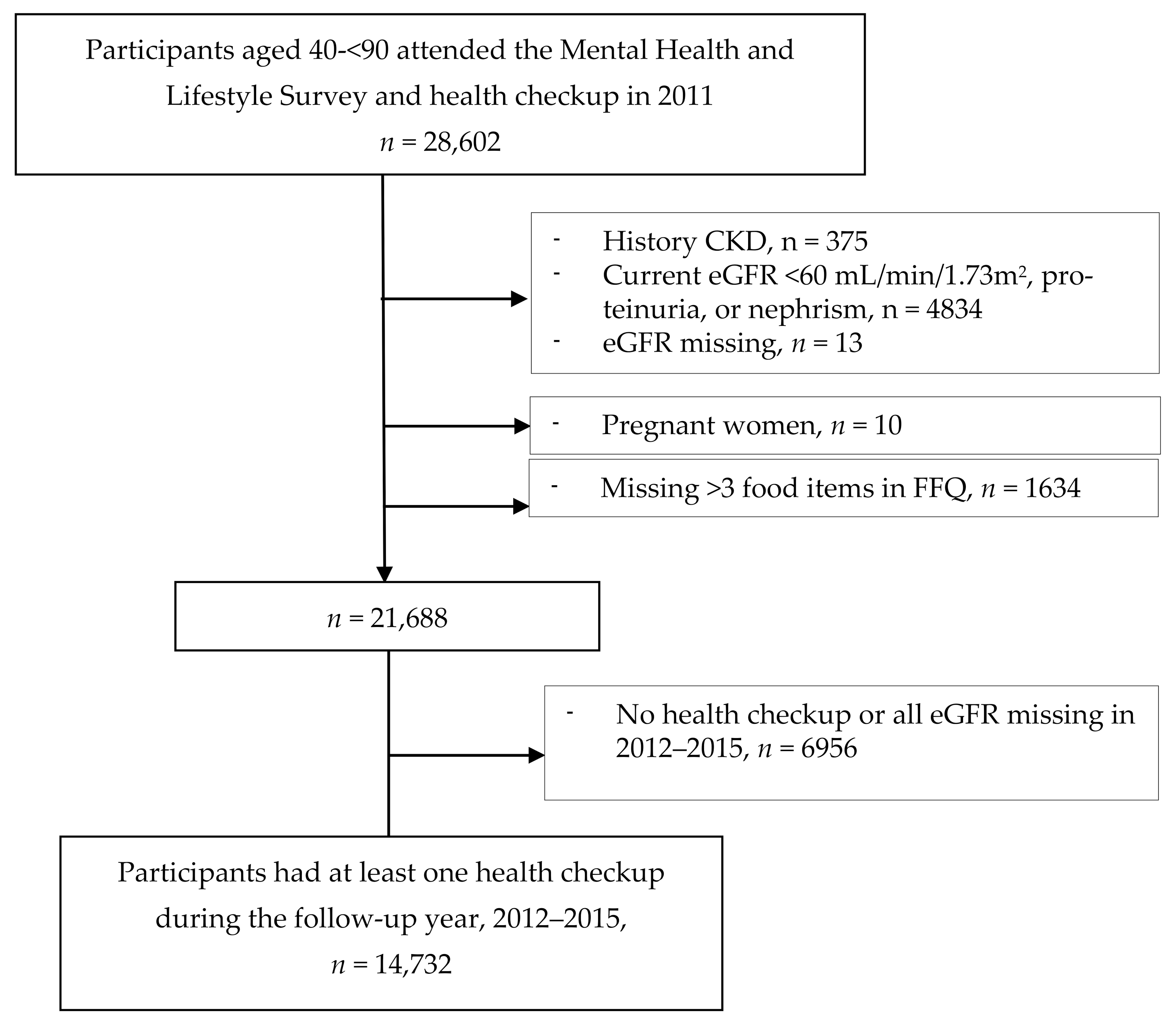
2.1. Study Participants
2.2. Dietary Intake Assessment
2.3. End-Point Determination
2.4. Other Variables
2.5. Statistical Analysis
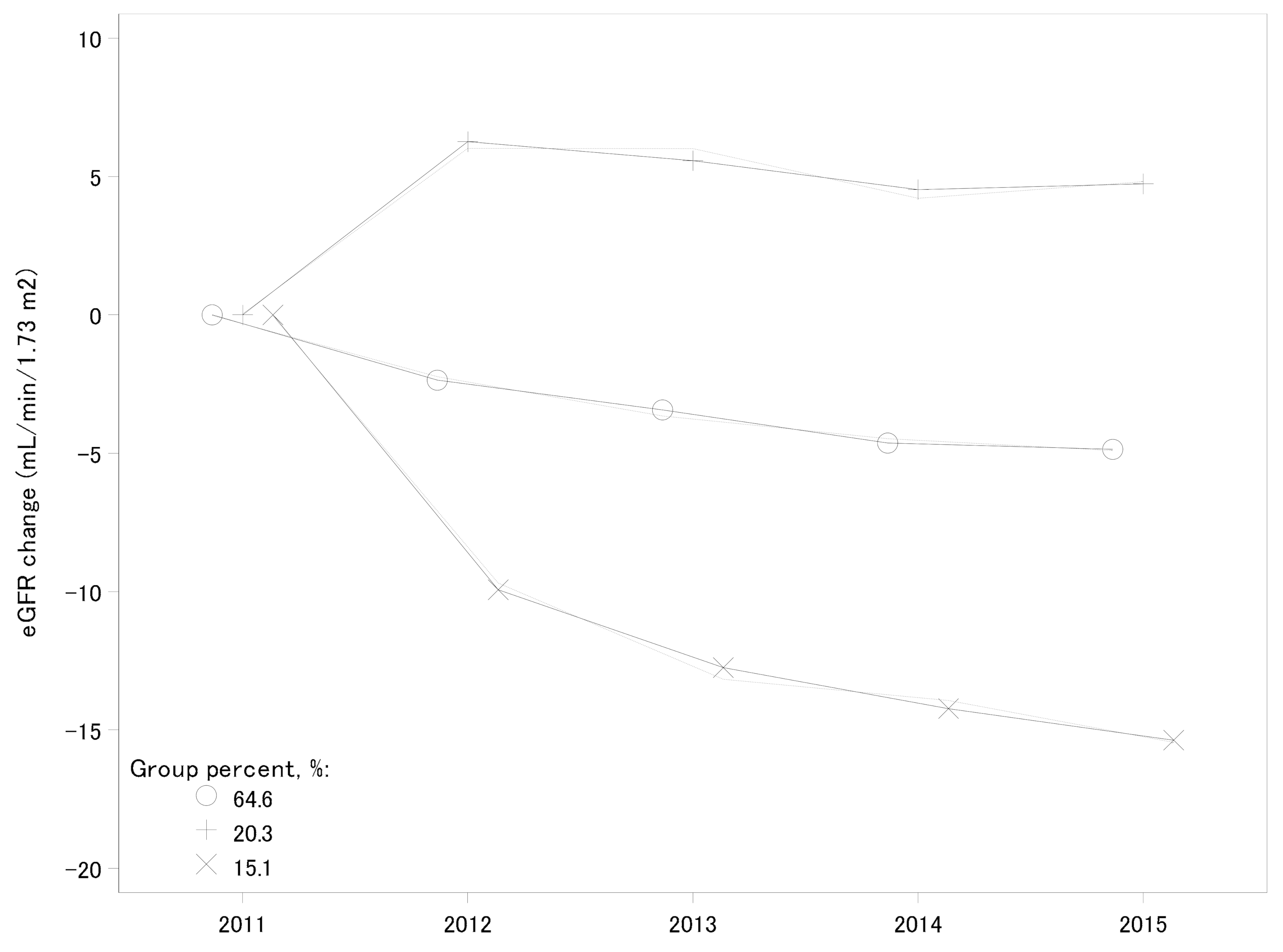
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- Tonelli, M.; Muntner, P.; Lloyd, A.; Manns, B.J.; Klarenbach, S.; Pannu, N.; James, M.T.; Hemmelgarn, B.R.; Alberta Kidney Disease Network. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: A population-level cohort study. Lancet 2012, 380, 807–814. [Google Scholar] [CrossRef]
- Muka, T.; Imo, D.; Jaspers, L.; Colpani, V.; Chaker, L.; van der Lee, S.J.; Mendis, S.; Chowdhury, R.; Bramer, W.M.; Falla, A.; et al. The global impact of non-communicable diseases on healthcare spending and national income: A systematic review. Eur. J. Epidemiol. 2015, 30, 251–277. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.T.; Lloyd, A.; Sanchez, J.J.G.; Sorstadius, E.; Briggs, A.; McFarlane, P. Health related quality of life utility weights for economic evaluation through different stages of chronic kidney disease: A systematic literature review. Health Qual. Life Outcomes 2020, 18, 310. [Google Scholar] [CrossRef]
- Daya, N.; Voskertchian, A.; Schneider, A.L.C.; Ballew, S.; McAdams DeMarco, M.; Coresh, J.; Appel, L.J.; Selvin, E.; Grams, M.E. Kidney Function and Fracture Risk: The Atherosclerosis Risk in Communities (ARIC) Study. Am. J. Kidney Dis. 2016, 67, 218–226. [Google Scholar] [CrossRef][Green Version]
- Pimentel, A.; Urena-Torres, P.; Zillikens, M.C.; Bover, J.; Cohen-Solal, M. Fractures in patients with CKD-diagnosis, treatment, and prevention: A review by members of the European Calcified Tissue Society and the European Renal Association of Nephrology Dialysis and Transplantation. Kidney Int. 2017, 92, 1343–1355. [Google Scholar] [CrossRef]
- Evenepoel, P.; Opdebeeck, B.; David, K.; D’Haese, P.C. Bone-Vascular Axis in Chronic Kidney Disease. Adv. Chronic. Kidney Dis. 2019, 26, 472–483. [Google Scholar] [CrossRef]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-Related Mechanisms in Chronic Kidney Disease Prediction, Progression, and Outcome. J. Immunol. Res. 2018, 2018, 2180373. [Google Scholar] [CrossRef]
- Graboski, A.L.; Redinbo, M.R. Gut-Derived Protein-Bound Uremic Toxins. Toxins 2020, 12. [Google Scholar] [CrossRef]
- Kaminski, T.W.; Pawlak, K.; Karbowska, M.; Mysliwiec, M.; Pawlak, D. Indoxyl sulfate—#he uremic toxin linking hemostatic system disturbances with the prevalence of cardiovascular disease in patients with chronic kidney disease. BMC Nephrol. 2017, 18, 35. [Google Scholar] [CrossRef]
- Felizardo, R.J.F.; Watanabe, I.K.M.; Dardi, P.; Rossoni, L.V.; Camara, N.O.S. The interplay among gut microbiota, hypertension and kidney diseases: The role of short-chain fatty acids. Pharmacol. Res. 2019, 141, 366–377. [Google Scholar] [CrossRef] [PubMed]
- Sabatino, A.; Regolisti, G.; Cosola, C.; Gesualdo, L.; Fiaccadori, E. Intestinal Microbiota in Type 2 Diabetes and Chronic Kidney Disease. Curr. Diabete Rep. 2017, 17, 16. [Google Scholar] [CrossRef] [PubMed]
- Bobot, M.; Thomas, L.; Moyon, A.; Fernandez, S.; McKay, N.; Balasse, L.; Garrigue, P.; Brige, P.; Chopinet, S.; Poitevin, S.; et al. Uremic Toxic Blood-Brain Barrier Disruption Mediated by AhR Activation Leads to Cognitive Impairment during Experimental Renal Dysfunction. J. Am. Soc. Nephrol. 2020, 31, 1509–1521. [Google Scholar] [CrossRef] [PubMed]
- Jhee, J.H.; Kee, Y.K.; Park, J.T.; Chang, T.I.; Kang, E.W.; Yoo, T.H.; Kang, S.W.; Han, S.H. A Diet Rich in Vegetables and Fruit and Incident CKD: A Community-Based Prospective Cohort Study. Am. J. Kidney Dis. 2019, 74, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- Borges, C.A.; Rinaldi, A.E.; Conde, W.L.; Mainardi, G.M.; Behar, D.; Slater, B. Dietary patterns: A literature review of the methodological characteristics of the main step of the multivariate analyzes. Rev. Bras. Epidemiol. 2015, 18, 837–857. [Google Scholar] [CrossRef]
- Wesolowska, E.; Jankowska, A.; Trafalska, E.; Kaluzny, P.; Grzesiak, M.; Dominowska, J.; Hanke, W.; Calamandrei, G.; Polanska, K. Sociodemographic, Lifestyle, Environmental and Pregnancy-Related Determinants of Dietary Patterns during Pregnancy. Int. J. Environ. Res. Public Health 2019, 16. [Google Scholar] [CrossRef]
- Khatri, M.; Moon, Y.P.; Scarmeas, N.; Gu, Y.; Gardener, H.; Cheung, K.; Wright, C.B.; Sacco, R.L.; Nickolas, T.L.; Elkind, M.S. The association between a Mediterranean-style diet and kidney function in the Northern Manhattan Study cohort. Clin. J. Am. Soc. Nephrol. 2014, 9, 1868–1875. [Google Scholar] [CrossRef]
- Huang, X.; Jimenez-Moleon, J.J.; Lindholm, B.; Cederholm, T.; Arnlov, J.; Riserus, U.; Sjogren, P.; Carrero, J.J. Mediterranean diet, kidney function, and mortality in men with CKD. Clin. J. Am. Soc. Nephrol. 2013, 8, 1548–1555. [Google Scholar] [CrossRef]
- Cai, Q.; Dekker, L.H.; Bakker, S.J.L.; de Borst, M.H.; Navis, G.J. Dietary Patterns Based on Estimated Glomerular Filtration Rate and Kidney Function Decline in the General Population: The Lifelines Cohort Study. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Lin, J.; Fung, T.T.; Hu, F.B.; Curhan, G.C. Association of dietary patterns with albuminuria and kidney function decline in older white women: A subgroup analysis from the Nurses’ Health Study. Am. J. Kidney Dis. 2011, 57, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Smyth, A.; Griffin, M.; Yusuf, S.; Mann, J.F.; Reddan, D.; Canavan, M.; Newell, J.; O’Donnell, M. Diet and Major Renal Outcomes: A Prospective Cohort Study. The NIH-AARP Diet and Health Study. J. Ren. Nutr. 2016, 26, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Taylor, A.W.; Riley, M.; Byles, J.; Liu, J.; Noakes, M. Association between dietary patterns, cadmium intake and chronic kidney disease among adults. Clin. Nutr. 2018, 37, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Asghari, G.; Momenan, M.; Yuzbashian, E.; Mirmiran, P.; Azizi, F. Dietary pattern and incidence of chronic kidney disease among adults: A population-based study. Nutr. Metab. 2018, 15, 88. [Google Scholar] [CrossRef]
- Kurniawan, A.L.; Hsu, C.Y.; Rau, H.H.; Lin, L.Y.; Chao, J.C. Association of kidney function-related dietary pattern, weight status, and cardiovascular risk factors with severity of impaired kidney function in middle-aged and older adults with chronic kidney disease: A cross-sectional population study. Nutr. J. 2019, 18, 27. [Google Scholar] [CrossRef]
- Ohira, T.; Nakano, H.; Nagai, M.; Yumiya, Y.; Zhang, W.; Uemura, M.; Sakai, A.; Hashimoto, S.; Fukushima Health Management Survey Group. Changes in Cardiovascular Risk Factors After the Great East Japan Earthquake. Asia Pac. J. Public Health 2017, 29, 47S–55S. [Google Scholar] [CrossRef]
- Hayashi, Y.; Nagai, M.; Ohira, T.; Satoh, H.; Sakai, A.; Ohtsuru, A.; Hosoya, M.; Kawasaki, Y.; Suzuki, H.; Takahashi, A.; et al. The impact of evacuation on the incidence of chronic kidney disease after the Great East Japan Earthquake: The Fukushima Health Management Survey. Clin. Exp. Nephrol. 2017, 21, 995–1002. [Google Scholar] [CrossRef][Green Version]
- Ma, E.; Ohira, T.; Sakai, A.; Yasumura, S.; Takahashi, A.; Kazama, J.; Shimabukuro, M.; Nakano, H.; Okazaki, K.; Maeda, M.; et al. Associations between Dietary Patterns and Cardiometabolic Risks in Japan: A Cross-Sectional Study from the Fukushima Health Management Survey, 2011–2015. Nutrients 2020, 12. [Google Scholar] [CrossRef]
- Yasumura, S.; Hosoya, M.; Yamashita, S.; Kamiya, K.; Abe, M.; Akashi, M.; Kodama, K.; Ozasa, K. Study protocol for the Fukushima Health Management Survey. J. Epidemiol. 2012, 22, 375–383. [Google Scholar] [CrossRef]
- Sauvaget, C.; Allen, N.; Hayashi, M.; Spencer, E.; Nagano, J. Validation of a food frequency questionnaire in the Hiroshima/Nagasaki Life Span Study. J. Epidemiol. 2002, 12, 394–401. [Google Scholar] [CrossRef]
- Matsuo, S.; Imai, E.; Horio, M.; Yasuda, Y.; Tomita, K.; Nitta, K.; Yamagata, K.; Tomino, Y.; Yokoyama, H.; Hishida, A.; et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 2009, 53, 982–992. [Google Scholar] [CrossRef] [PubMed]
- Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2020 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int. 2020, 98, S1–S115. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.L.; Manderscheid, R.W.; Walters, E.E.; et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Ohira, T.; Abe, M.; Kamiya, K.; Yamashita, S.; Yasumura, S.; Ohtsuru, A.; Masaharu, M.; Harigane, M.; Horikoshi, N.; et al. Evacuation after the Great East Japan Earthquake was associated with poor dietary intake: The Fukushima Health Management Survey. J. Epidemiol. 2017, 27, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Luger, E.; Aspalter, R.; Luger, M.; Longin, R.; Rieder, A.; Dorner, T.E. Changes of dietary patterns during participation in a web-based weight-reduction programme. Public Health Nutr. 2016, 19, 1211–1221. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kobayashi, A.; Matsuzawa, T.; Hosoya, T.; Yoshida, S. Sulfoxide synthesis from sulfinate esters under Pummerer-like conditions. Chem. Commun. 2020, 56, 5429–5432. [Google Scholar] [CrossRef]
- Burckhardt, P.; Nagin, D.S.; Padman, R. Multi-Trajectory Models of Chronic Kidney Disease Progression. AMIA Annu. Symp. Proc. 2016, 2016, 1737–1746. [Google Scholar]
- Nagai, M.; Ohira, T.; Takahashi, H.; Nakano, H.; Sakai, A.; Hashimoto, S.; Yasumura, S.; Abe, M.; Fukushima Health Management Survey. Impact of evacuation onstrends in the prevalence, treatment, and control of hypertension before and after a disaster. J. Hypertens 2018, 36, 924–932. [Google Scholar] [CrossRef]
- Bazi, T.; Takahashi, S.; Ismail, S.; Bo, K.; Ruiz-Zapata, A.M.; Duckett, J.; Kammerer-Doak, D. Prevention of pelvic floor disorders: International urogynecological association research and development committee opinion. Int. Urogynecol. J. 2016, 27, 1785–1795. [Google Scholar] [CrossRef]
- Maruyama, K.I.H.; Date, C.; Kikuchi, S.; Watanabe, Y.; Wada, Y.; Inaba, Y.; Tamakoshi, A. JACC Study Group. Dietary patterns and risk of cardiovascular deaths among middle-aged Japanese: JACC Study. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 8. [Google Scholar] [CrossRef]
- Okada, E.; Takahashi, K.; Nakamura, K.; Ukawa, S.; Takabayashi, S.; Nakamura, M.; Sasaki, S.; Tamakoshi, A.; Takimoto, H. Dietary patterns and abnormal glucose tolerance among Japanese: Findings from the National Health and Nutrition Survey, 2012. Public Health Nutr. 2019, 22, 2460–2468. [Google Scholar] [CrossRef] [PubMed]
- Sadakane, A.; Tsutsumi, A.; Gotoh, T.; Ishikawa, S.; Ojima, T.; Kario, K.; Nakamura, Y.; Kayaba, K. Dietary patterns and levels of blood pressure and serum lipids in a Japanese population. J. Epidemiol. 2008, 18, 58–67. [Google Scholar] [CrossRef]
- Tomata, Y.; Sugiyama, K.; Kaiho, Y.; Honkura, K.; Watanabe, T.; Zhang, S.; Sugawara, Y.; Tsuji, I. Dietary Patterns and Incident Dementia in Elderly Japanese: The Ohsaki Cohort 2006 Study. J. Gerontol A Biol. Sci. Med. Sci. 2016, 71, 1322–1328. [Google Scholar] [CrossRef] [PubMed]
- Murakami, K.; Shinozaki, N.; Fujiwara, A.; Yuan, X.; Hashimoto, A.; Fujihashi, H.; Wang, H.C.; Livingstone, M.B.E.; Sasaki, S. A Systematic Review of Principal Component Analysis-Derived Dietary Patterns in Japanese Adults: Are Major Dietary Patterns Reproducible Within a Country? Adv. Nutr. 2019, 10, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Nanri, A.; Yoshida, D.; Yamaji, T.; Mizoue, T.; Takayanagi, R.; Kono, S. Dietary patterns and C-reactive protein in Japanese men and women. Am. J. Clin. Nutr. 2008, 87, 1488–1496. [Google Scholar] [CrossRef]
- Ito, T.; Kawakami, R.; Tanisawa, K.; Miyawaki, R.; Ishii, K.; Torii, S.; Suzuki, K.; Sakamoto, S.; Muraoka, I.; Oka, K.; et al. Dietary patterns and abdominal obesity in middle-aged and elderly Japanese adults: Waseda Alumni’s Sports, Exercise, Daily Activity, Sedentariness and Health Study (WASEDA’S Health Study). Nutrition 2019, 58, 149–155. [Google Scholar] [CrossRef]
- Bach, K.E.; Kelly, J.T.; Palmer, S.C.; Khalesi, S.; Strippoli, G.F.M.; Campbell, K.L. Healthy Dietary Patterns and Incidence of CKD: A Meta-Analysis of Cohort Studies. Clin. J. Am. Soc. Nephrol. 2019, 14, 1441–1449. [Google Scholar] [CrossRef]
- Babio, N.; Bullo, M.; Salas-Salvado, J. Mediterranean diet and metabolic syndrome: The evidence. Public Health Nutr. 2009, 12, 1607–1617. [Google Scholar] [CrossRef]
- Goraya, N.; Simoni, J.; Jo, C.H.; Wesson, D.E. A comparison of treating metabolic acidosis in CKD stage 4 hypertensive kidney disease with fruits and vegetables or sodium bicarbonate. Clin. J. Am. Soc. Nephrol. 2013, 8, 371–381. [Google Scholar] [CrossRef]
- Gopinath, B.; Harris, D.C.; Flood, V.M.; Burlutsky, G.; Brand-Miller, J.; Mitchell, P. Carbohydrate nutrition is associated with the 5-year incidence of chronic kidney disease. J. Nutr. 2011, 141, 433–439. [Google Scholar] [CrossRef]
- Lauretani, F.; Maggio, M.; Pizzarelli, F.; Michelassi, S.; Ruggiero, C.; Ceda, G.P.; Bandinelli, S.; Ferrucci, L. Omega-3 and renal function in older adults. Curr. Pharm. Des. 2009, 15, 4149–4156. [Google Scholar] [CrossRef] [PubMed]
- Yamori, Y.; Sagara, M.; Arai, Y.; Kobayashi, H.; Kishimoto, K.; Matsuno, I.; Mori, H.; Mori, M. Soy and fish as features of the Japanese diet and cardiovascular disease risks. PLoS ONE 2017, 12, e0176039. [Google Scholar] [CrossRef]
- Tsugane, S. Why has Japan become the world’s most long-lived country: Insights from a food and nutrition perspective. Eur. J. Clin. Nutr. 2020. [Google Scholar] [CrossRef] [PubMed]
- Iso, H.; Kobayashi, M.; Ishihara, J.; Sasaki, S.; Okada, K.; Kita, Y.; Kokubo, Y.; Tsugane, S.; Group, J.S. Intake of fish and n3 fatty acids and risk of coronary heart disease among Japanese: The Japan Public Health Center-Based (JPHC) Study Cohort I. Circulation 2006, 113, 195–202. [Google Scholar] [CrossRef]
- Kokubo, Y.; Iso, H.; Ishihara, J.; Okada, K.; Inoue, M.; Tsugane, S.; Group, J.S. Association of dietary intake of soy, beans, and isoflavones with risk of cerebral and myocardial infarctions in Japanese populations: The Japan Public Health Center-based (JPHC) study cohort I. Circulation 2007, 116, 2553–2562. [Google Scholar] [CrossRef]
- Budhathoki, S.; Sawada, N.; Iwasaki, M.; Yamaji, T.; Goto, A.; Kotemori, A.; Ishihara, J.; Takachi, R.; Charvat, H.; Mizoue, T.; et al. Association of Animal and Plant Protein Intake With All-Cause and Cause-Specific Mortality in a Japanese Cohort. JAMA Intern. Med. 2019, 179, 1509–1518. [Google Scholar] [CrossRef]
- Hruby, A.; Manson, J.E.; Qi, L.; Malik, V.S.; Rimm, E.B.; Sun, Q.; Willett, W.C.; Hu, F.B. Determinants and Consequences of Obesity. Am. J. Public Health 2016, 106, 1656–1662. [Google Scholar] [CrossRef]
- Onal, E.M.; Afsar, B.; Covic, A.; Vaziri, N.D.; Kanbay, M. Gut microbiota and inflammation in chronic kidney disease and their roles in the development of cardiovascular disease. Hypertens Res. 2019, 42, 123–140. [Google Scholar] [CrossRef]
- Nanri, H.; Nakamura, K.; Hara, M.; Higaki, Y.; Imaizumi, T.; Taguchi, N.; Sakamoto, T.; Horita, M.; Shinchi, K.; Tanaka, K. Association between dietary pattern and serum C-reactive protein in Japanese men and women. J. Epidemiol. 2011, 21, 122–131. [Google Scholar] [CrossRef]
- Semba, R.D.; Ferrucci, L.; Fink, J.C.; Sun, K.; Beck, J.; Dalal, M.; Guralnik, J.M.; Fried, L.P. Advanced glycation end products and their circulating receptors and level of kidney function in older community-dwelling women. Am. J. Kidney Dis. 2009, 53, 51–58. [Google Scholar] [CrossRef]
- Iso, H. Lifestyle and cardiovascular disease in Japan. J. Atheroscler. Thromb. 2011, 18, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Tormo, M.J.; Navarro, C.; Chirlaque, M.D.; Barber, X.; Cancer, E.G.o.S.E.P.I.o. Is there a different dietetic pattern depending on self-knowledge of high blood pressure? Eur. J. Epidemiol. 2000, 16, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, Y.; Arisawa, K.; Katsuura-Kamano, S.; Uemura, H.; Tsukamoto, M.; Kadomatsu, Y.; Okada, R.; Hishida, A.; Tanaka, K.; Hara, M.; et al. Associations of Nutrient Patterns with the Prevalence of Metabolic Syndrome: Results from the Baseline Data of the Japan Multi-Institutional Collaborative Cohort Study. Nutrients 2019, 11. [Google Scholar] [CrossRef] [PubMed]
| Food Groups | Vegetable | Juice | Meat |
|---|---|---|---|
| White vegetables | 0.69 | 0.14 | 0.22 |
| Green vegetables | 0.65 | 0.20 | 0.18 |
| Tofu | 0.64 | 0.13 | 0.06 |
| Miso soup | 0.63 | −0.12 | −0.09 |
| Red/yellow vegetables | 0.63 | 0.30 | 0.25 |
| Fish | 0.51 | 0.06 | 0.23 |
| Fermented beans | 0.48 | 0.14 | −0.13 |
| Fruit | 0.45 | 0.41 | 0.01 |
| Boiled beans | 0.38 | 0.37 | 0.08 |
| Rice | 0.34 | −0.22 | −0.05 |
| Vegetable juice | −0.02 | 0.71 | 0.004 |
| Fruit juice | −0.01 | 0.68 | 0.08 |
| Yogurt | 0.22 | 0.53 | 0.004 |
| Soybean milk | 0.08 | 0.40 | −0.04 |
| Bread | −0.23 | 0.35 | 0.31 |
| Milk | 0.19 | 0.34 | 0.06 |
| Beef/pork | 0.15 | −0.05 | 0.74 |
| Ham/sausage | −0.01 | 0.07 | 0.69 |
| Chicken | 0.16 | 0.04 | 0.68 |
| % Variance explained | 3.26 | 2.21 | 1.81 |
| All | Men (n = 5964) | Women (n = 8768) | p Value | |
|---|---|---|---|---|
| Age (years), mean (SD) | 61.4 (10.0) | 62.6 (9.9) | 60.5 (9.9) | <0.001 |
| Education ≥ vocational university, % | 20.9 | 19.3 | 22.1 | <0.001 |
| Current smoker, % | 13.3 | 24.9 | 5.4 | <0.001 |
| Current alcohol drinking, % | 45.3 | 71.8 | 27.2 | <0.001 |
| Physical activity ≥ 2 times/week, % | 42 | 45.1 | 39.9 | <0.001 |
| Distress scale ≥ 13, % | 14.6 | 11.1 | 16.9 | <0.001 |
| Live at shelter/temporary house, % | 39.8 | 39.1 | 40.3 | 0.094 |
| BMI (kg/m2), mea(SD) | 23.7 (3.4) | 24.2 (3.1) | 23.3 (3.5) | <0.001 |
| BMI ≥ 25 kg/m2, % | 32.2 | 38.2 | 28.1 | <0.001 |
| Hypertension, % | 50.5 | 58.1 | 45.4 | <0.001 |
| SBP (mmHg), mean (SD) | 131 (15.8) | 133.5 (15.0) | 129.3 (16.1) | <0.001 |
| DBP (mmHg), mean (SD) | 78.6 (10.1) | 80.6.0 (9.9) | 77.2 (10) | <0.001 |
| Fast blood glucose (mg/dL), median (IQR) | 97 (90, 105) | 100 (93, 110) | 95 (89, 102) | <0.001 |
| Fast blood glucose ≥ 126 mg/dl, % | 7 | 10 | 4.9 | <0.001 |
| HbA1C1 ≥ 6.5%, % | 6.6 | 9.1 | 5 | <0.001 |
| LDL-C (mg/dL), mean (SD) | 126.8 (31.7) | 122.6 (31.9) | 129.7 (31.3) | <0.001 |
| LDL-C ≥ 140 mg/dL, % | 33.2 | 29.1 | 36 | <0.001 |
| HDL-C (mg/dL), mean (SD) | 60.8 (15.2) | 56.1 (14.5) | 64 (14.9.0) | <0.001 |
| HDL-C < 40 mg/dL, % | 5.7 | 9.8 | 2.8 | <0.001 |
| Triglycerides (mg/dL), median (IQR) | 97 (69, 136) | 106 (75, 152) | 91 (66, 126) | <0.001 |
| Triglycerides ≥ 150 mg/dL, % | 19.5 | 25.9 | 15.1 | <0.001 |
| eGFR, mL/min/1.73 m2, median (IQR) | 74 (67, 82) | 73 (67, 82) | 74 (68, 82) | <0.001 |
| Vegetable pattern score, median (IQR) | 0.01 (−0.68, 0.73) | −0.09 (−0.77, 0.65) | 0.08 (−0.61, 0.78) | <0.001 |
| Juice/milk pattern score, median (IQR) | −0.17 (−0.69, 0.47) | −0.33 (−0.84, 0.29) | −0.06 (−0.58, 0.58) | <0.001 |
| Meat pattern score, median (IQR) | −0.21 (−0.67, 0.46) | −0.31 (−0.71, 0.34) | −0.14 (−0.63, 0.54) | <0.001 |
| 2011 | 2012 | 2013 | 2014 | 2015 | p Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 14,732) | (n = 10,999) | (n = 9597) | (n = 8713) | (n = 8477) | |||||||
| eGFR (mL/min/1.73 m2), mean (SD) | 75.7 | (11.0) | 73.9 | (11.9) | 72.3 | (11.5) | 71.0 | (11.5) | 70.8 | (11.7) | <0.001 |
| eGFR (mL/min/1.73 m2) category, n (%) | <0.001 | ||||||||||
| <60 | 0 | 889 | (8.1) | 1060 | (11.1) | 1195 | (13.7) | 1262 | (14.9) | ||
| 60–90 | 13,131 | (89.1) | 9035 | (82.1) | 7777 | (81.2) | 6981 | (80.1) | 6673 | (78.7) | |
| ≥90 | 1601 | (10.9) | 1075 | (9.8) | 733 | (7.7) | 536 | (6.1) | 541 | (6.4) | |
| Proteinuria | 0.049 | ||||||||||
| Negative | 14,602 | (99.4) | 10,771 | (97.9) | 9358 | (97.7) | 8528 | (97.8) | 8254 | (97.4) | |
| Trace | 91 | (0.6) | 123 | (1.1) | 100 | (1.0) | 79 | (0.9) | 102 | (1.2) | |
| Positive | 0 | 95 | (0.9) | 104 | (1.1) | 97 | (1.1) | 115 | (1.4) | ||
| eGFR < 60 mL/min/1.73 m2 or proteinuria, n (%) | 0 | 973 | (8.8) | 1143 | (11.9) | 1270 | (14.6) | 1350 | (15.9) | <0.001 | |
| 2011–2012 | 2012–2013 | 2013–2014 | 2014–2015 | p Value | |||||||
| (n = 10,999) | (n = 7342) | (n = 6612) | (n = 6337) | ||||||||
| Annual change of eGFR (mL/min/1.73 m2 per year), mean (SD) | −1.8 | (7.3) | −1.2 | (6.9) | −1.3 | (6.2) | −0.3 | (6.0) | <0.001 | ||
| Annual change category, n (%) | <0.001 | ||||||||||
| <−30% | 6589 | (59.9) | 3954 | (41.3) | 3715 | (42.6) | 3034 | (35.8) | |||
| −30—< 15% | 666 | (6.1) | 507 | (5.3) | 457 | (5.2) | 479 | (5.6) | |||
| ≥15% | 3744 | (34.0) | 2881 | (30.1) | 2440 | (28.0) | 2824 | (33.3) | |||
| eGFR < 60 (mL/min/1.73 m2) | Proteinuria | eGFR < 60 (mL/min/1.73 m2) or Proteinuria | |||||
|---|---|---|---|---|---|---|---|
| CIR a | 95% CI | CIR a | 95% CI | CIR a | 95% CI | ||
| Vegetable | |||||||
| Model 1 | T1 (lowest) | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | 0.97 | 0.88, 1.07 | 0.80 | 0.61, 1.04 | 0.95 | 0.87, 1.05 | |
| T3 | 0.89 | 0.81, 0.98 | 0.67 | 0.51, 0.88 | 0.87 | 0.79, 0.95 | |
| P for trend | 0.013 | 0.005 | 0.001 | ||||
| Model 2 | T1 (lowest) | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | 0.98 | 0.89, 1.08 | 0.80 | 0.62, 1.04 | 0.96 | 0.88, 1.06 | |
| T3 | 0.90 | 0.82, 1.00 | 0.68 | 0.52, 0.90 | 0.88 | 0.80, 0.97 | |
| P for trend | 0.031 | 0.007 | 0.005 | ||||
| Juice | |||||||
| Model 1 | T1 (lowest) | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | 1.08 | 0.98, 1.19 | 0.97 | 0.74, 1.26 | 1.07 | 0.97, 1.17 | |
| T3 | 1.20 | 1.09, 1.32 | 1.08 | 0.83, 1.41 | 1.19 | 1.09, 1.30 | |
| P for trend | <0.001 | 0.543 | <0.001 | ||||
| Model 2 | T1 (lowest) | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | 1.07 | 0.97, 1.18 | 0.94 | 0.72, 1.22 | 1.05 | 0.96, 1.15 | |
| T3 | 1.19 | 1.08, 1.31 | 1.04 | 0.79, 1.36 | 1.18 | 1.08, 1.29 | |
| P for trend | <0.001 | 0.738 | <0.001 | ||||
| Meat | |||||||
| Model 1 | T1 (lowest) | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | 0.97 | 0.89, 1.06 | 1.00 | 0.77, 1.31 | 0.97 | 0.89, 1.06 | |
| T3 | 0.96 | 0.88, 1.06 | 1.17 | 0.90, 1.52 | 0.98 | 0.90, 1.08 | |
| P for trend | 0.459 | 0.214 | 0.809 | ||||
| Model 2 | T1 (lowest) | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | 0.97 | 0.89, 1.07 | 1.02 | 0.78, 1.33 | 0.98 | 0.90, 1.06 | |
| T3 | 0.98 | 0.89, 1.07 | 1.20 | 0.92, 1.55 | 1.00 | 0.92, 1.09 | |
| P for trend | 0.695 | 0.158 | 0.898 | ||||
| Annual Change in eGFR (mL/min/1.73 m2 Per Year) | Increasing eGFR | Rapid Decline in eGFR | |||||
|---|---|---|---|---|---|---|---|
| β a | 95% CI | OR b | 95% CI | OR b | 95% CI | ||
| Vegetable | |||||||
| Model 1 | T1 (lowest) | 0 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | 0.24 | 0.03, 0.44 | 0.96 | 0.86, 1.06 | 0.86 | 0.76, 0.98 | |
| T3 | 0.27 | 0.06, 0.49 | 0.95 | 0.85, 1.06 | 0.83 | 0.73, 0.94 | |
| P for trend | 0.012 | 0.4 | 0.006 | ||||
| Model 2 | T1 (lowest) | 0 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | 0.23 | 0.02, 0.43 | 0.96 | 0.86, 1.06 | 0.88 | 0.77, 1.00 | |
| T3 | 0.26 | 0.04, 0.47 | 0.94 | 0.84, 1.06 | 0.85 | 0.75, 0.98 | |
| P for trend | 0.019 | 0.422 | 0.009 | ||||
| Juice | |||||||
| Model 1 | T1 (lowest) | 0 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | −0.08 | −0.28, 0.12 | 0.92 | 0.82, 1.02 | 1.11 | 0.98, 1.26 | |
| T3 | 0.08 | −0.12, 0.28 | 0.92 | 0.83, 1.03 | 0.99 | 0.87, 1.13 | |
| P for trend | 0.553 | 0.204 | 0.836 | ||||
| Model 2 | T1 | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | −0.08 | −0.28, 0.12 | 0.92 | 0.83, 1.03 | 1.10 | 0.98, 1.25 | |
| T3 | 0.07 | −0.13, 0.28 | 0.94 | 0.85, 1.05 | 1.00 | 0.88, 1.14 | |
| P for trend | 0.607 | 0.284 | 0.937 | ||||
| Meat | |||||||
| Model 1 | T1 (lowest) | 0 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | −0.06 | −0.26, 0.14 | 0.93 | 0.83, 1.03 | 1.04 | 0.92, 1.18 | |
| T3 | 0.04 | −0.16, 0.24 | 1.07 | 0.96, 1.19 | 1.08 | 0.95, 1.23 | |
| P for trend | 0.62 | 0.099 | 0.256 | ||||
| Model 2 | T1 (lowest) | 0 | Referent | 1.00 | Referent | 1.00 | Referent |
| T2 | −0.07 | −0.27, 0.13 | 0.92 | 0.83, 1.02 | 1.04 | 0.92, 1.18 | |
| T3 | 0.03 | −0.18, 0.23 | 1.06 | 0.96, 1.18 | 1.09 | 0.96, 1.23 | |
| P for trend | 0.732 | 0.095 | 0.176 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, E.; Ohira, T.; Yasumura, S.; Nakano, H.; Eguchi, E.; Miyazaki, M.; Hosoya, M.; Sakai, A.; Takahashi, A.; Ohira, H.; et al. Dietary Patterns and Progression of Impaired Kidney Function in Japanese Adults: A Longitudinal Analysis for the Fukushima Health Management Survey, 2011–2015. Nutrients 2021, 13, 168. https://doi.org/10.3390/nu13010168
Ma E, Ohira T, Yasumura S, Nakano H, Eguchi E, Miyazaki M, Hosoya M, Sakai A, Takahashi A, Ohira H, et al. Dietary Patterns and Progression of Impaired Kidney Function in Japanese Adults: A Longitudinal Analysis for the Fukushima Health Management Survey, 2011–2015. Nutrients. 2021; 13(1):168. https://doi.org/10.3390/nu13010168
Chicago/Turabian StyleMa, Enbo, Tetsuya Ohira, Seiji Yasumura, Hironori Nakano, Eri Eguchi, Makoto Miyazaki, Mitsuaki Hosoya, Akira Sakai, Atsushi Takahashi, Hiromasa Ohira, and et al. 2021. "Dietary Patterns and Progression of Impaired Kidney Function in Japanese Adults: A Longitudinal Analysis for the Fukushima Health Management Survey, 2011–2015" Nutrients 13, no. 1: 168. https://doi.org/10.3390/nu13010168
APA StyleMa, E., Ohira, T., Yasumura, S., Nakano, H., Eguchi, E., Miyazaki, M., Hosoya, M., Sakai, A., Takahashi, A., Ohira, H., Kazama, J., Shimabukuro, M., Yabe, H., Maeda, M., Ohto, H., & Kamiya, K. (2021). Dietary Patterns and Progression of Impaired Kidney Function in Japanese Adults: A Longitudinal Analysis for the Fukushima Health Management Survey, 2011–2015. Nutrients, 13(1), 168. https://doi.org/10.3390/nu13010168






