Relationship between Sleep and Hedonic Appetite in Shift Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Data Analysis
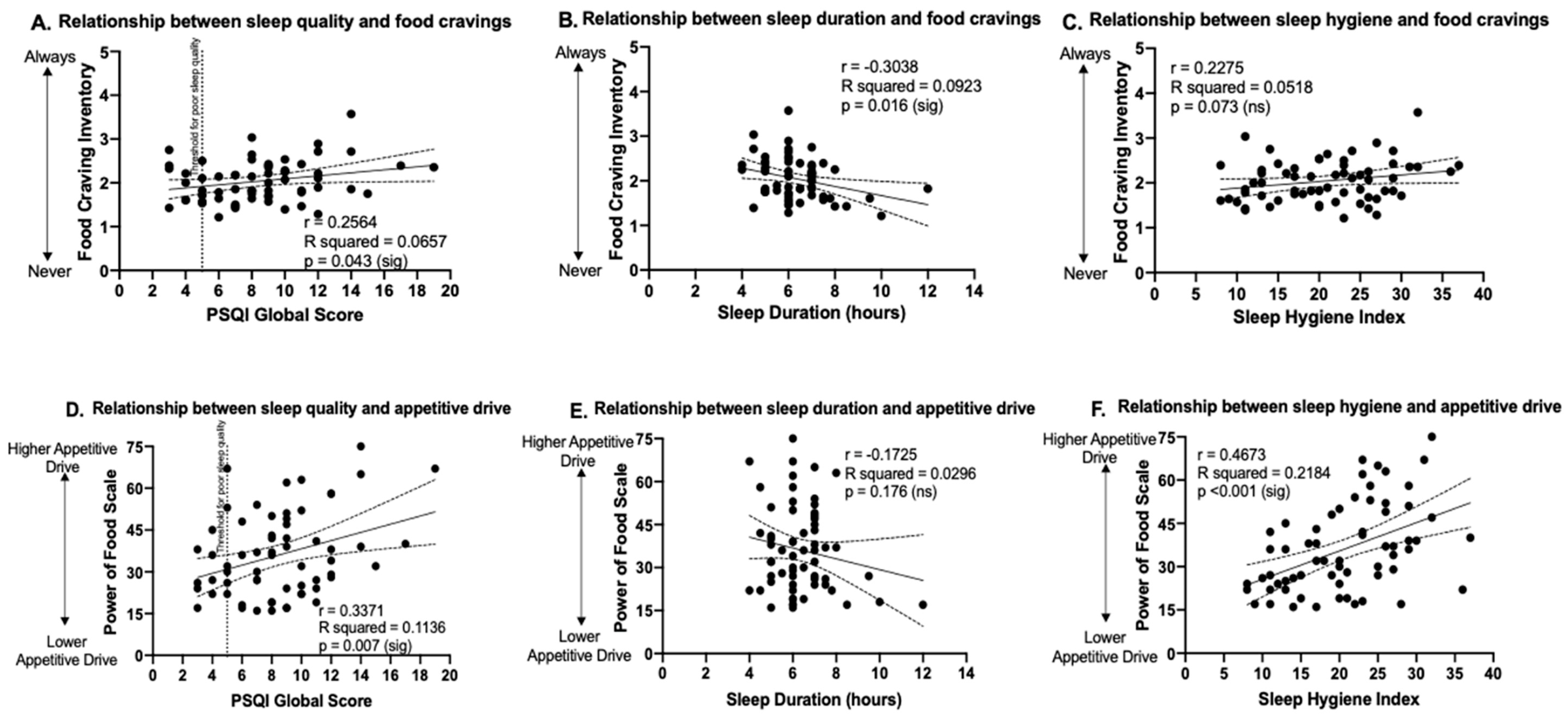
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- St-Onge, M.-P.; Grandner, M.A.; Brown, D.; Conroy, M.B.; Jean-Louis, G.; Coons, M.; Bhatt, D.L. Sleep duration and quality: Impact on lifestyle behaviors and cardiometabolic health: A scientific statement from the American Heart Association. Circulation 2016, 134, e367–e386. [Google Scholar] [CrossRef] [PubMed]
- Shechter, A.; Grandner, M.A.; St-Onge, M.-P. The role of sleep in the control of food intake. Am. J. Lifestyle Med. 2014, 8, 371–374. [Google Scholar] [CrossRef]
- Baron, K.G.; Reid, K.J.; Kern, A.S.; Zee, P.C. Role of sleep timing in caloric intake and BMI. Obesity 2011, 19, 1374–1381. [Google Scholar] [CrossRef] [PubMed]
- Zuraikat, F.M.; Makarem, N.; Redline, S.; Aggarwal, B.; Jelic, S.; St-Onge, M.-P. Sleep regularity and cardiometabolic heath: Is variability in sleep patterns a risk factor for excess adiposity and glycemic dysregulation? Curr. Diabetes Rep. 2020, 20, 38. [Google Scholar] [CrossRef]
- Lunsford-Avery, J.R.; Engelhard, M.M.; Navar, A.M.; Kollins, S.H. Validation of the sleep regularity index in older adults and associations with cardiometabolic risk. Sci. Rep. 2018, 8, 14158. [Google Scholar] [CrossRef] [PubMed]
- Van Drongelen, A.; Boot, C.R.; Merkus, S.L.; Smid, T.; Van Der Beek, A.J. The effects of shift work on body weight change—a systematic review of longitudinal studies. Scand. J. Work Environ. Health 2011, 37, 263–275. [Google Scholar] [CrossRef]
- Suwazono, Y.; Dochi, M.; Sakata, K.; Okubo, Y.; Oishi, M.; Tanaka, K.; Kobayashi, E.; Kido, T.; Nogawa, K. A longitudinal study on the effect of shift work on weight gain in male Japanese workers. Obesity 2008, 16, 1887–1893. [Google Scholar] [CrossRef] [PubMed]
- Åkerstedt, T.; Wright, K.P., Jr. Sleep loss and fatigue in shift work and shift work disorder. Sleep Med. Clin. 2009, 4, 257–271. [Google Scholar] [CrossRef]
- Gupta, C.C.; Coates, A.M.; Dorrian, J.; Banks, S. The factors influencing the eating behaviour of shiftworkers: What, when, where and why. Ind. Health 2019, 57, 419–453. [Google Scholar] [CrossRef]
- Bonnell, E.K.; Huggins, C.E.; Huggins, C.T.; McCaffrey, T.A.; Palermo, C.; Bonham, M.P. Influences on dietary choices during day versus night shift in shift workers: A mixed methods study. Nutrients 2017, 9, 193. [Google Scholar] [CrossRef] [PubMed]
- Flahr, H.; Brown, W.J.; Kolbe-Alexander, T.L. A systematic review of physical activity-based interventions in shift workers. Prev. Med. Rep. 2018, 10, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Van Amelsvoort, L.G.P.M.; Schouten, E.G.; Kok, F.J. Impact of one year of shift work on cardiovascular disease risk factors. J. Occup. Environ. Med. 2004, 46, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Van Amelsvoort, L.G.P.M.; Jansen, N.W.H.; Kant, I. Smoking among shift workers: More than a confounding factor. Chronobiol. Int. 2006, 23, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- McHill, A.W.; Melanson, E.L.; Higgins, J.; Connick, E.; Moehlman, T.M.; Stothard, E.R.; Wright, K.P., Jr. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc. Natl. Acad. Sci. USA 2014, 111, 17302–17307. [Google Scholar] [CrossRef] [PubMed]
- Buxton, O.M.; Cain, S.W.; O’Connor, S.P.; Porter, J.H.; Duffy, J.F.; Wang, W.; Czeisler, C.A.; Shea, S.A. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci. Transl. Med. 2012, 4, 129ra43. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; McReynolds, A.; Trivedi, Z.B.; Roberts, A.L.; Sy, M.; Hirsch, J. Sleep restriction leads to increased activation of brain regions sensitive to food stimuli. Am. J. Clin. Nutr. 2012, 95, 818–824. [Google Scholar] [CrossRef]
- Benedict, C.; Brooks, S.J.; O’Daly, O.G.; Almen, M.S.; Morell, A.; Aberg, K.; Gingnell, M.; Schultes, B.; Hallschmis, M.; Broman, J.-E.; et al. Acute sleep deprivation enhances the brain’s response to hedonic food stimuli: An fMRI study. J. Clin. Endocrinol. Metab. 2012, 97, E443–E447. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Wolfe, S.; Sy, M.; Shechter, A.; Hirsch, J. Sleep restriction increases the neuronal response to unhealthy food in normal-weight individuals. Int. J. Obes. 2014, 38, 411–416. [Google Scholar] [CrossRef]
- Duraccio, K.M.; Zaugg, K.; Jensen, C.D. Effects of sleep restriction on food-related inhibitory control and reward in adolescents. J. Pediatric Psychol. 2019, 44, 692–702. [Google Scholar] [CrossRef]
- Blumfield, M.L.; Bei, B.; Zimberg, I.Z.; Cain, S.W. Dietary disinhibition mediates the relationship between poor sleep quality and body weight. Appetite 2018, 120, 602–608. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [PubMed]
- Kitamura, S.; Hida, A.; Watanabe, M.; Enomoto, M.; Aritake-Okada, S.; Moriguchi, Y.; Kamei, Y.; Mishima, K. Evening preference is related to the incidence of depressive states independent of sleep-wake conditions. Chronobiol. Int. 2010, 27, 1797–1812. [Google Scholar]
- Mastin, D.; Bryson, J.; Corwyn, R. Assessment of sleep hygiene using the sleep hygiene index. J. Behav. Med. 2006, 29, 223–227. [Google Scholar] [PubMed]
- White, M.A.; Whisenhunt, B.L.; Williamson, D.A.; Greenway, F.L.; Netemeyer, R.G. Development and validation of the food-craving inventory. Obes. Res. 2002, 10, 107. [Google Scholar]
- Lowe, M.R.; Butryn, M.L.; Didie, E.R.; Annunziato, R.A.; Thomas, J.G.; Crerand, C.E.; Ochner, C.N.; Coletta, M.C.; Bellace, D.; Wallaert, M.; et al. The power of food scale. A new measure of the psychological influence of the food environment. Appetite 2009, 53, 114–118. [Google Scholar] [PubMed]
- Cappelleri, J.C.; Bushmakin, A.G.; Gerber, R.A.; Leidy, N.K.; Sexton, C.C.; Karlsson, J.; Lowe, M.R. Evaluating the Power of Food Scale in obese subjects and a general sample of individuals: Development and measurement properties. Int. J. Obes. 2009, 33, 913. [Google Scholar]
- Tucker, P.; Smith, L.; Macdonald, I.; Folkard, S. Effects of direction of rotation in continuous and discontinuous 8 hour shift systems. Occup Environ. Med. 2000, 57, 678–684. [Google Scholar]
- Duchon, J.; Wagner, J.; Keran, C. Forward versus backward shift rotation. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 1989, 33, 806–810. [Google Scholar]
- Kilkus, J.M.; Booth, J.N.; Bromley, L.E.; Darukhanavala, A.P.; Imperial, J.G.; Penev, P.D. Sleep and eating behavior in adults at risk for type 2 diabetes. Obesity 2012, 20, 112–117. [Google Scholar]
- Markwald, R.R.; Melanson, E.L.; Smith, M.R.; Higgins, J.; Perreault, L.; Eckel, R.H.; Wright, K.P., Jr. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc. Natl. Acad. Sci. USA 2013, 110, 5695–5700. [Google Scholar]
- Kracht, C.; Chaput, J.-P.; Martin, C.; Champagne, C.; Katzmarzyk, P.; Staiano, A. Associations of sleep with food cravings, diet, and obesity in adolescence. Nutrients 2019, 11, 2899. [Google Scholar] [CrossRef] [PubMed]
- Goel, N.; Rao, H.; Durmer, J.S.; Dinges, D.F. Neurocognitive consequences of sleep deprivation. Semin Neurol 2009, 29, 320–339. [Google Scholar] [CrossRef] [PubMed]
- Whitney, P.; Hinson, J.M.; Jackson, M.L.; Van Dongen, H.P.A. Feedback blunting: Total sleep deprivation impairs decision making that requires updating based on feedback. Sleep 2015, 38, 745–754. [Google Scholar] [CrossRef]
- Dorrian, J.; Centofanti, S.; Smith, A.; McDermott, K.D. Chapter 4—Self-Regulation and Social Behavior During Sleep Deprivation. In Progress in Brain Research; Van Dongen, H.P.A., Whitney, P., Hinson, J.M., Honn, K.A., Chee, M.W.L., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 73–110. [Google Scholar]
- Nilsson, J.P.; Söderström, M.; Karlsson, A.U.; Lekander, M.; Åkerstedt, T.; Lindroth, N.E.; Axelsson, J. Less effective executive functioning after one night’s sleep deprivation. J. Sleep Res. 2005, 14, 1–6. [Google Scholar] [CrossRef]
- Gissoni, N.B.; dos Santos Quaresma, M.V.L. Short sleep duration and food intake: An overview and analysis of the influence of the homeostatic and hedonic system. Nutrire 2020, 45, 8. [Google Scholar] [CrossRef]
- Chaput, J.-P.; St-Onge, M.-P. Increased food intake by insufficient sleep in humans: Are we jumping the gun on the hormonal explanation? Front. Endocrinol. 2014, 5, 116. [Google Scholar] [CrossRef] [PubMed]
- Hogenkamp, P.S.; Shechter, A.; St-Onge, M.-P.; Sclafani, A.; Kissileff, H. A sipometer for measuring motivation to consume and reward value of foods and beverages in humans: Description and proof of principle. Physiol. Behav. 2017, 171, 216–227. [Google Scholar] [CrossRef]
- Qian, J.; Morris, C.J.; Caputo, R.; Wang, W.; Garaulet, M.; Scheer, F.A.J.L. Sex differences in the circadian misalignment effects on energy regulation. Proc. Natl. Acad. Sci. USA 2019, 116, 23806–23812. [Google Scholar] [CrossRef]
| Sample Size (n) | Mean (Standard Deviation) or % | |
| Age (years) | 63 | 36.7 (12) |
| Females | 37 | 59% |
| Males | 26 | 41% |
| Body mass index, Females | 28.3 (8.2) kg/m2 | |
| Body mass index, Males | 31.7 (11.5) kg/m2 | |
| Work schedule type | ||
| Night shifts | 11 | 17% |
| Forward rotating shifts | 15 | 24% |
| Backward rotating shifts | 6 | 10% |
| Early morning shifts | 6 | 10% |
| Evening/swing shifts | 4 | 6% |
| On-call | 2 | 3% |
| Other (e.g., 24 h on, 24 h off) | 19 | 30% |
| Workforce sector | ||
| Emergency responders | 21 | 33% |
| Health care workers | 26 | 41% |
| Goods and services | 6 | 10% |
| Transport | 9 | 14% |
| YES | NO | N/A | |
|---|---|---|---|
| Shift Work Affects Weight Maintenance | 83% (n = 52) | 17% (n = 11) | -- |
| Night shifts (n = 11) | 73% (n = 8) | 27% (n = 3) | |
| Forward rotating shifts (n = 15) | 73% (n = 11) | 27% (n = 4) | |
| Backward rotating shifts (n = 6) | 83% (n = 5) | 17% (n = 1) | |
| Early morning shifts (n = 6) | 67% (n = 4) | 33% (n = 2) | |
| Evening/swing shifts (n = 4) | 50% (n = 2) | 50% (n = 2) | |
| On-call (n = 2) | 100% (n = 2) | 0% (n = 0) | |
| Other (e.g., 24 h on, 24 h off; n = 19) | 68% (n = 13) | 32% (n = 6) | |
| Weight change since starting shift work | 71% (n = 45) | 29% (n = 18) | -- |
| Weight gain: 84%, n = 38, +11.3 (9.1) kg | |||
| Weight loss: 16%, n = 7, −11.0 (12.9) kg | |||
| Weight loss attempt since shift work | 60% (n = 38) | 8% (n = 5) | 32% (n = 20) |
| Successful weight loss attempt | 21% (n = 13) | 41% (n = 26) | 38% (n = 24) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vidafar, P.; Cain, S.W.; Shechter, A. Relationship between Sleep and Hedonic Appetite in Shift Workers. Nutrients 2020, 12, 2835. https://doi.org/10.3390/nu12092835
Vidafar P, Cain SW, Shechter A. Relationship between Sleep and Hedonic Appetite in Shift Workers. Nutrients. 2020; 12(9):2835. https://doi.org/10.3390/nu12092835
Chicago/Turabian StyleVidafar, Parisa, Sean W. Cain, and Ari Shechter. 2020. "Relationship between Sleep and Hedonic Appetite in Shift Workers" Nutrients 12, no. 9: 2835. https://doi.org/10.3390/nu12092835
APA StyleVidafar, P., Cain, S. W., & Shechter, A. (2020). Relationship between Sleep and Hedonic Appetite in Shift Workers. Nutrients, 12(9), 2835. https://doi.org/10.3390/nu12092835







