Efficacy of Dietary Supplements to Reduce Liver Fat
Abstract
1. Introduction
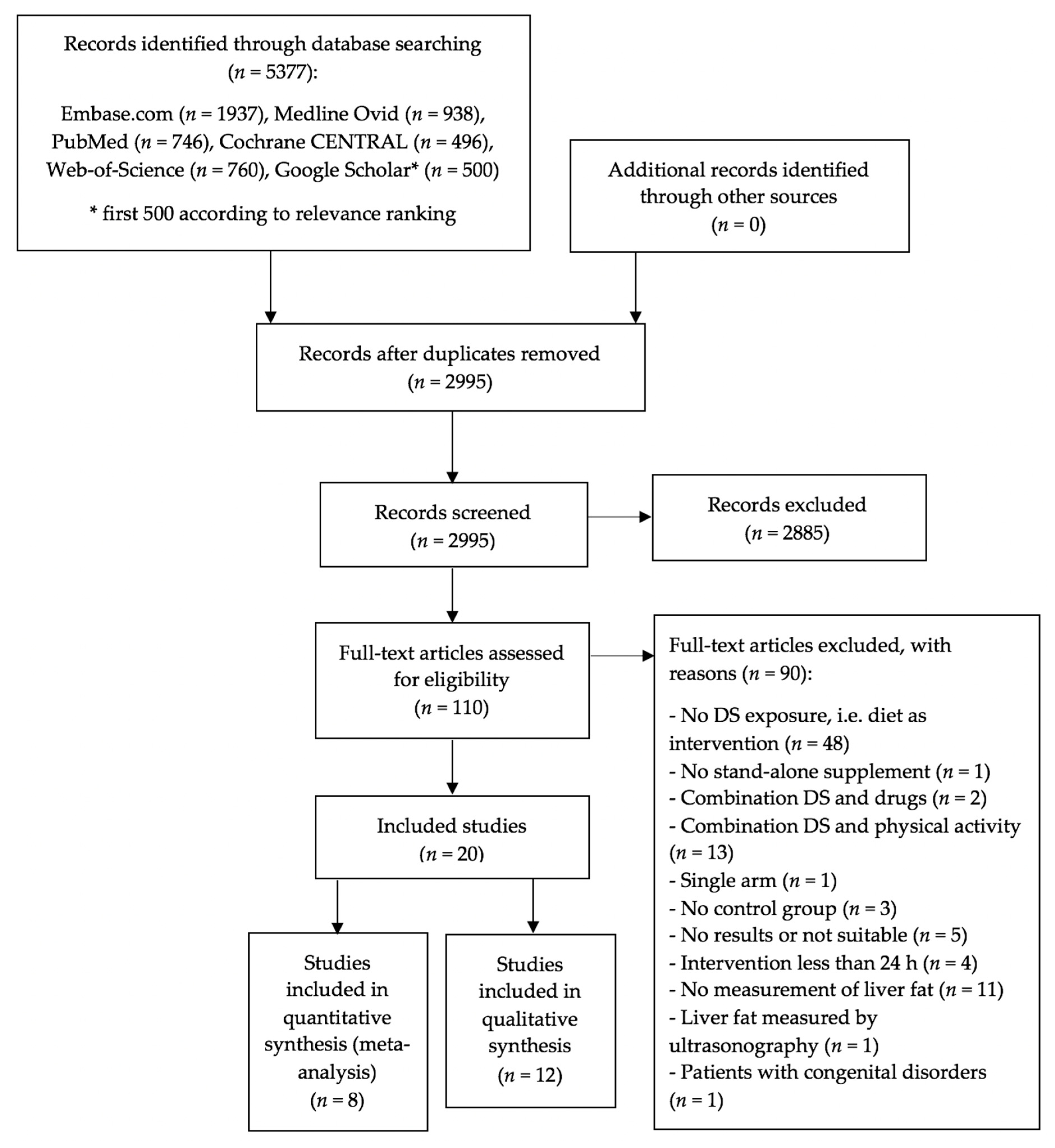
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Study Selection and Eligibility Criteria
2.3. Data Extraction
2.4. Assessing the Risk of Bias
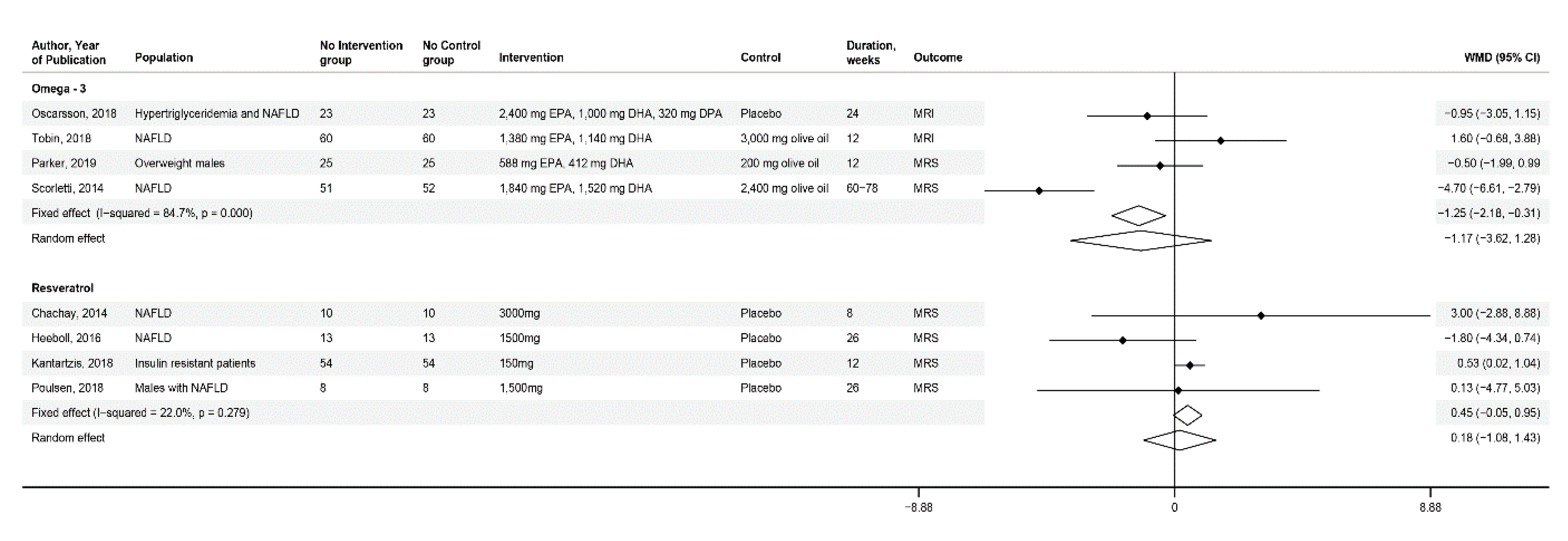
2.5. Data Synthesis and Analysis
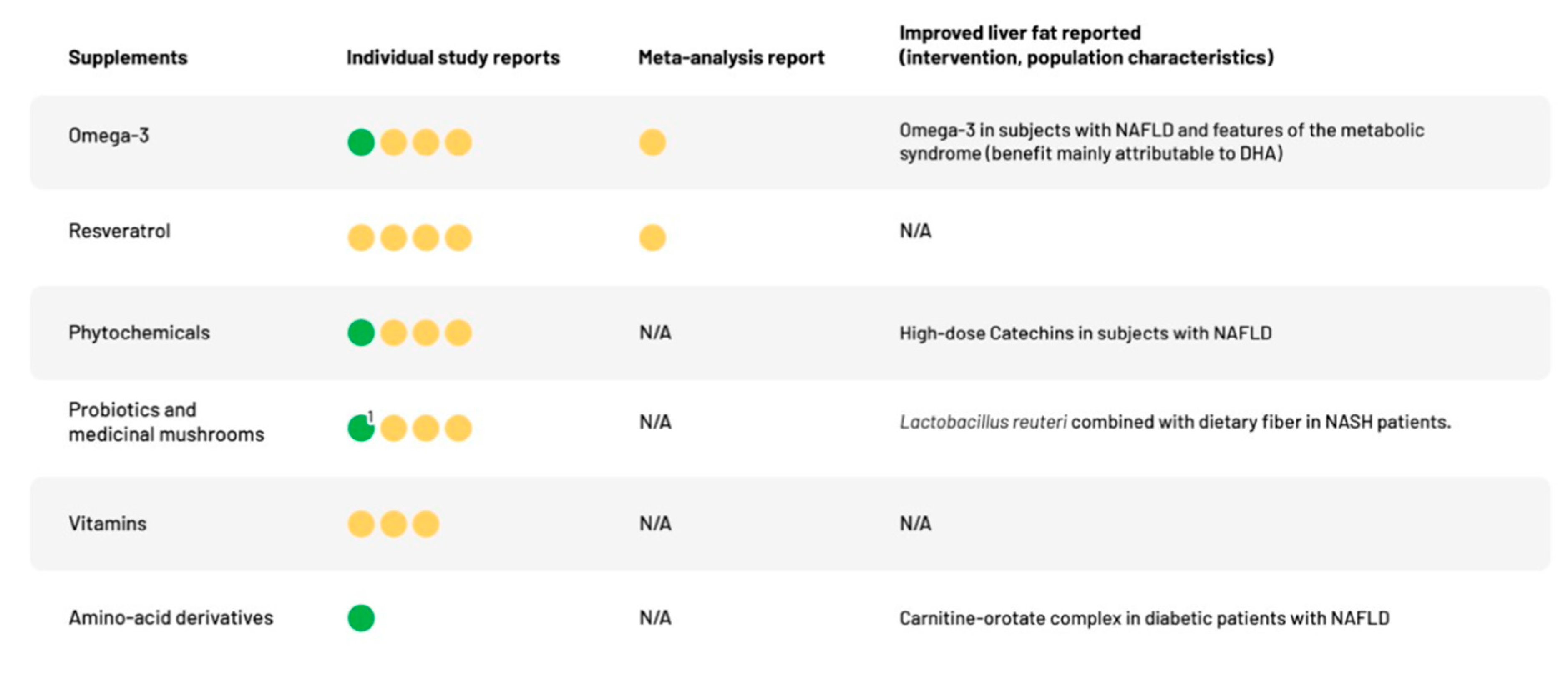
3. Results
3.1. Characteristics of RCTs
3.1.1. Omega-3
3.1.2. Phytochemicals
3.1.3. Probiotics and Medicinal Mushrooms
3.1.4. Vitamins
3.1.5. Amino-Acid Derivative
3.2. Further Outcomes and Safety
3.3. Assessment of Bias and Heterogeneity
4. Discussion
4.1. Strengths and Limitations of Current Systematic Review
4.2. Implications for Clinical Practice and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Paul, S.; Davis, A.M. Diagnosis and Management of Nonalcoholic Fatty Liver Disease. JAMA 2018, 320, 2474–2475. [Google Scholar] [CrossRef] [PubMed]
- Asrih, M.; Jornayvaz, F.R. Diets and nonalcoholic fatty liver disease: The good and the bad. Clin. Nutr. 2014, 33, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.N.; Fowler, K.J.; Hamilton, G.; Cui, J.Y.; Sy, E.Z.; Balanay, M.; Hooker, J.C.; Szeverenyi, N.; Sirlin, C.B. Liver fat imaging-a clinical overview of ultrasound, CT, and MR imaging. Br. J. Radio 2018, 91, 20170959. [Google Scholar] [CrossRef] [PubMed]
- Stern, C.; Castera, L. Non-invasive diagnosis of hepatic steatosis. Hepatol. Int. 2017, 11, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Koutoukidis, D.A.; Astbury, N.M.; Tudor, K.E.; Morris, E.; Henry, J.A.; Noreik, M.; Jebb, S.A.; Aveyard, P. Association of Weight Loss Interventions With Changes in Biomarkers of Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2019, 179, 1262–1271. [Google Scholar] [CrossRef]
- Abenavoli, L.; Milic, N.; Peta, V.; Alfieri, F.; De Lorenzo, A.; Bellentani, S. Alimentary regimen in non-alcoholic fatty liver disease: Mediterranean diet. World J. Gastroenterol. WJG 2014, 20, 16831. [Google Scholar] [CrossRef]
- Suárez, M.; Boqué, N.; Del Bas, J.M.; Mayneris-Perxachs, J.; Arola, L.; Caimari, A. Mediterranean diet and multi-ingredient-based interventions for the management of non-alcoholic fatty liver disease. Nutrients 2017, 9, 1052. [Google Scholar] [CrossRef]
- Plauth, M.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Bischoff, S.C. ESPEN guideline on clinical nutrition in liver disease. Clin. Nutr. 2019, 38, 485–521. [Google Scholar] [CrossRef]
- Incze, M. Vitamins and Nutritional Supplements: What Do I Need to Know? JAMA Intern. Med. 2019, 179, 460. [Google Scholar] [CrossRef]
- Food and Drug Administration. FDA 101: Dietary Supplements. Available online: https://www.fda.gov/consumers/consumer-updates/fda-101-dietary-supplements (accessed on 6 March 2020).
- European Food Safety Authority. Food Supplements. Available online: https://www.efsa.europa.eu/en/topics/topic/food-supplements (accessed on 6 March 2020).
- Hallsworth, K.; Thoma, C.; Moore, S.; Ploetz, T.; Anstee, Q.M.; Taylor, R.; Day, C.P.; Trenell, M.I. Non-alcoholic fatty liver disease is associated with higher levels of objectively measured sedentary behaviour and lower levels of physical activity than matched healthy controls. Frontline Gastroenterol. 2015, 6, 44–51. [Google Scholar] [CrossRef]
- Cui, J.; Philo, L.; Nguyen, P.; Hofflich, H.; Hernandez, C.; Bettencourt, R.; Richards, L.; Salotti, J.; Bhatt, A.; Hooker, J. Sitagliptin vs. placebo for non-alcoholic fatty liver disease: A randomized controlled trial. J. Hepatol. 2016, 65, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Muka, T.; Glisic, M.; Milic, J.; Verhoog, S.; Bohlius, J.; Bramer, W.; Chowdhury, R.; Franco, O.H. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur. J. Epidemiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Browning, J.D.; Baxter, J.; Satapati, S.; Burgess, S.C. The effect of short-term fasting on liver and skeletal muscle lipid, glucose, and energy metabolism in healthy women and men. J. Lipid Res. 2012, 53, 577–586. [Google Scholar] [CrossRef]
- Dusilová, T.; Kovář, J.; Drobný, M.; Šedivý, P.; Dezortová, M.; Poledne, R.; Zemánková, K.; Hájek, M. Different acute effects of fructose and glucose administration on hepatic fat content. Am. J. Clin. Nutr. 2019, 109, 1519–1526. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Scorletti, E.; Bhatia, L.; McCormick, K.G.; Clough, G.F.; Nash, K.; Hodson, L.; Moyses, H.E.; Calder, P.C.; Byrne, C.D. Effects of purified eicosapentaenoic and docosahexaenoic acids in nonalcoholic fatty liver disease: Results from the WELCOME* study. Hepatology 2014, 60, 1211–1221. [Google Scholar] [CrossRef]
- Parker, H.M.; Cohn, J.S.; O’connor, H.T.; Garg, M.L.; Caterson, I.D.; George, J.; Johnson, N.A. Effect of fish oil supplementation on hepatic and visceral fat in overweight men: A randomized controlled trial. Nutrients 2019, 11. [Google Scholar] [CrossRef]
- Oscarsson, J.; Önnerhag, K.; Risérus, U.; Sundén, M.; Johansson, L.; Jansson, P.A.; Moris, L.; Nilsson, P.M.; Eriksson, J.W.; Lind, L. Effects of free omega-3 carboxylic acids and fenofibrate on liver fat content in patients with hypertriglyceridemia and non-alcoholic fatty liver disease: A double-blind, randomized, placebo-controlled study. J. Clin. Lipidol. 2018, 12, 1390–1403.e4. [Google Scholar] [CrossRef]
- Tobin, D.; Brevik-Andersen, M.; Qin, Y.; Innes, J.K.; Calder, P.C. Evaluation of a high concentrate omega-3 for correcting the omega-3 fatty acid nutritional deficiency in non-alcoholic fatty liver disease (CONDIN). Nutrients 2018, 10. [Google Scholar] [CrossRef]
- Chachay, V.S.; Macdonald, G.A.; Martin, J.H.; Whitehead, J.P.; O’Moore-Sullivan, T.M.; Lee, P.; Franklin, M.; Klein, K.; Taylor, P.J.; Ferguson, M.; et al. Resveratrol Does Not Benefit Patients With Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2014, 12, 2092–2103. [Google Scholar] [CrossRef] [PubMed]
- Heebøll, S.; Kreuzfeldt, M.; Hamilton-Dutoit, S.; Poulsen, M.K.; Stødkilde-Jørgensen, H.; Møller, H.J.; Jessen, N.; Thorsen, K.; Hellberg, Y.K.; Pedersen, S.B.; et al. Placebo-controlled, randomised clinical trial: High-dose resveratrol treatment for non-alcoholic fatty liver disease. Scand. J. Gastroenterol. 2016, 51, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Kantartzis, K.; Fritsche, L.; Bombrich, M.; Machann, J.; Schick, F.; Staiger, H.; Kunz, I.; Schoop, R.; Lehn-Stefan, A.; Heni, M.; et al. Effects of resveratrol supplementation on liver fat content in overweight and insulin-resistant subjects: A randomized, double-blind, placebo-controlled clinical trial. DiabetesObes. Metab. 2018, 20, 1793–1797. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, M.K.; Nellemann, B.; Bibby, B.M.; Stødkilde-Jørgensen, H.; Pedersen, S.B.; Grønbæk, H.; Nielsen, S. No effect of resveratrol on VLDL-TG kinetics and insulin sensitivity in obese men with nonalcoholic fatty liver disease. DiabetesObes. Metab. 2018, 20, 2504–2509. [Google Scholar] [CrossRef]
- Lee, E.; Lim, Y.; Kwon, S.W.; Kwon, O. Pinitol consumption improves liver health status by reducing oxidative stress and fatty acid accumulation in subjects with non-alcoholic fatty liver disease: A randomized, double-blind, placebo-controlled trial. J. Nutr. Biochem. 2019, 68, 33–41. [Google Scholar] [CrossRef]
- Sakata, R.; Nakamura, T.; Torimura, T.; Ueno, T.; Sata, M. Green tea with high-density catechins improves liver function and fat infiltration in non-alcoholic fatty liver disease (NAFLD) patients: A double-blind placebo-controlled study. Int. J. Mol. Med. 2013, 32, 989–994. [Google Scholar] [CrossRef]
- Johnston, K.L.; Thomas, E.L.; Bell, J.D.; Frost, G.S.; Robertson, M.D. Resistant starch improves insulin sensitivity in metabolic syndrome. Diabet. Med. 2010, 27, 391–397. [Google Scholar] [CrossRef]
- Peterson, C.M.; Beyl, R.A.; Marlatt, K.L.; Martin, C.K.; Aryana, K.J.; Marco, M.L.; Martin, R.J.; Keenan, M.J.; Ravussin, E. Effect of 12 wk of resistant starch supplementation on cardiometabolic risk factors in adults with prediabetes: A randomized controlled trial. Am. J. Clin. Nutr. 2018, 108, 492–501. [Google Scholar] [CrossRef]
- Cussons, A.J.; Watts, G.F.; Mori, T.A.; Stuckey, B.G.A. Omega-3 fatty acid supplementation decreases liver fat content in polycystic ovary syndrome: A randomized controlled trial employing proton magnetic resonance spectroscopy. J. Clin. Endocrinol. Metab. 2009, 94, 3842–3848. [Google Scholar] [CrossRef]
- Ingredion. HI-MAIZE® 260 Resistant Starch. Available online: https://apac.ingredion.com/ingredients/emea/himaize-260-22000b01.html (accessed on 7 March 2020).
- Ferolla, S.M.; Couto, C.A.; Costa-Silva, L.; Armiliato, G.N.A.; Pereira, C.A.S.; Martins, F.S.; Ferrari, M.L.A.; Vilela, E.G.; Torres, H.O.G.; Cunha, A.S.; et al. Beneficial effect of synbiotic supplementation on hepatic steatosis and anthropometric parameters, but not on gut permeability in a population with nonalcoholic steatohepatitis. Nutrients 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.W.; Won, G.L.; Chim, A.M.; Chu, W.C.; Yeung, D.K.; Li, K.C.; Chan, H.L. Treatment of nonalcoholic steatohepatitis with probiotics. A proof-of-concept study. Ann. Hepatol. 2013, 12, 256–262. [Google Scholar] [CrossRef]
- Scorletti, E.; Afolabi, P.R.; Miles, E.A.; Smith, D.E.; Almehmadi, A.; Alshathry, A.; Childs, C.E.; Del Fabbro, S.; Bilson, J.; Moyses, H.E.; et al. Synbiotics Alter Fecal Microbiomes, But Not Liver Fat or Fibrosis, in a Randomized Trial of Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology 2020, 158, 1597–1610.e7. [Google Scholar] [CrossRef]
- Heo, J.Y.; Baik, H.W.; Kim, H.J.; Lee, J.M.; Kim, H.W.; Choi, Y.S.; Won, J.H.; Kim, H.M.; Park, W.I.; Kim, C.Y. The Efficacy and Safety of Cordyceps militaris in Korean Adults Who Have Mild Liver Dysfunction. J. Clin. Nutr. 2015, 7, 81–86. [Google Scholar] [CrossRef]
- Barchetta, I.; Del Ben, M.; Angelico, F.; Di Martino, M.; Fraioli, A.; La Torre, G.; Saulle, R.; Perri, L.; Morini, S.; Tiberti, C.; et al. No effects of oral vitamin D supplementation on non-alcoholic fatty liver disease in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial. BMC Med. 2016, 14, 92. [Google Scholar] [CrossRef] [PubMed]
- Wamberg, L.; Kampmann, U.; Stødkilde-Jørgensen, H.; Rejnmark, L.; Pedersen, S.B.; Richelsen, B. Effects of vitamin D supplementation on body fat accumulation, inflammation, and metabolic risk factors in obese adults with low vitamin D levels—Results from a randomized trial. Eur. J. Intern. Med. 2013, 24, 644–649. [Google Scholar] [CrossRef] [PubMed]
- Dollerup, O.L.; Christensen, B.; Svart, M.; Schmidt, M.S.; Sulek, K.; Ringgaard, S.; Stødkilde-Jørgensen, H.; Møller, N.; Brenner, C.; Treebak, J.T.; et al. A randomized placebo-controlled clinical trial of nicotinamide riboside in obese men: Safety, insulin-sensitivity, and lipid-mobilizing effects. Am. J. Clin. Nutr. 2018, 108, 343–353. [Google Scholar] [CrossRef]
- Bae, J.C.; Lee, W.Y.; Yoon, K.H.; Park, J.Y.; Son, H.S.; Han, K.A.; Lee, K.W.; Woo, J.T.; Ju, Y.C.; Lee, W.J.; et al. Improvement of Nonalcoholic Fatty Liver Disease With Carnitine-Orotate Complex in Type 2 Diabetes (CORONA): A Randomized Controlled Trial. Diabetes Care 2015, 38, 1245–1252. [Google Scholar] [CrossRef]
- Parker, H.M.; Johnson, N.A.; Burdon, C.A.; Cohn, J.S.; O’Connor, H.T.; George, J. Omega-3 supplementation and non-alcoholic fatty liver disease: A systematic review and meta-analysis. J. Hepatol. 2012, 56, 944–951. [Google Scholar] [CrossRef]
- Alwayn, I.P.; Gura, K.; Nosé, V.; Zausche, B.; Javid, P.; Garza, J.; Verbesey, J.; Voss, S.; Ollero, M.; Andersson, C. Omega-3 fatty acid supplementation prevents hepatic steatosis in a murine model of nonalcoholic fatty liver disease. Pediatric Res. 2005, 57, 445–452. [Google Scholar] [CrossRef]
- Alwayn, I.P.; Andersson, C.; Zauscher, B.; Gura, K.; Nosé, V.; Puder, M. Omega-3 fatty acids improve hepatic steatosis in a murine model: Potential implications for the marginal steatotic liver donor. Transplantation 2005, 79, 606–608. [Google Scholar] [CrossRef] [PubMed]
- Levy, J.R.; Clore, J.N.; Stevens, W. Dietary n-3 polyunsaturated fatty acids decrease hepatic triglycerides in Fischer 344 rats. Hepatology 2004, 39, 608–616. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Zorita, S.; Fernández-Quintela, A.; Macarulla, M.; Aguirre, L.; Hijona, E.; Bujanda, L.; Milagro, F.; Martínez, J.; Portillo, M. Resveratrol attenuates steatosis in obese Zucker rats by decreasing fatty acid availability and reducing oxidative stress. Br. J. Nutr. 2012, 107, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Glisic, M.; Kastrati, N.; Gonzalez-Jaramillo, V.; Bramer, W.M.; Ahmadizar, F.; Chowdhury, R.; Danser, A.J.; Roks, A.J.; Voortman, T.; Franco, O.H.; et al. Associations between Phytoestrogens, Glucose Homeostasis, and Risk of Diabetes in Women: A Systematic Review and Meta-Analysis. Adv. Nutr. 2018, 9, 726–740. [Google Scholar] [CrossRef] [PubMed]
- Sivakumar, S.; Palsamy, P.; Subramanian, S.P. Impact of D-pinitol on the attenuation of proinflammatory cytokines, hyperglycemia-mediated oxidative stress and protection of kidney tissue ultrastructure in streptozotocin-induced diabetic rats. Chem.-Biol. Interact. 2010, 188, 237–245. [Google Scholar] [CrossRef]
- Ley, R.E.; Turnbaugh, P.J.; Klein, S.; Gordon, J.I. Microbial ecology: Human gut microbes associated with obesity. Nature 2006, 444, 1022–1023. [Google Scholar] [CrossRef]
- Turnbaugh, P.J.; Ley, R.E.; Mahowald, M.A.; Magrini, V.; Mardis, E.R.; Gordon, J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006, 444, 1027–1031. [Google Scholar] [CrossRef]
- Noland, R.C.; Koves, T.R.; Seiler, S.E.; Lum, H.; Lust, R.M.; Ilkayeva, O.; Stevens, R.D.; Hegardt, F.G.; Muoio, D.M. Carnitine insufficiency caused by aging and overnutrition compromises mitochondrial performance and metabolic control. J. Biol. Chem. 2009, 284, 22840–22852. [Google Scholar] [CrossRef]
- Cantó, C.; Houtkooper, R.H.; Pirinen, E.; Youn, D.Y.; Oosterveer, M.H.; Cen, Y.; Fernandez-Marcos, P.J.; Yamamoto, H.; Andreux, P.A.; Cettour-Rose, P.; et al. The NAD(+) precursor nicotinamide riboside enhances oxidative metabolism and protects against high-fat diet-induced obesity. Cell Metab. 2012, 15, 838–847. [Google Scholar] [CrossRef]
- Zhou, Q.G.; Hou, F.F.; Guo, Z.J.; Liang, M.; Wang, G.B.; Zhang, X. 1,25-Dihydroxyvitamin D improved the free fatty-acid-induced insulin resistance in cultured C2C12 cells. Diabetes Metab. Res. Rev. 2008, 24, 459–464. [Google Scholar] [CrossRef]
- Choi, S.B.; Park, C.H.; Choi, M.K.; Jun, D.W.; Park, S. Improvement of insulin resistance and insulin secretion by water extracts of Cordyceps militaris, Phellinus linteus, and Paecilomyces tenuipes in 90% pancreatectomized rats. Biosci. Biotechnol. Biochem. 2004, 68, 2257–2264. [Google Scholar] [CrossRef] [PubMed]
- Maki, K.C.; Pelkman, C.L.; Finocchiaro, E.T.; Kelley, K.M.; Lawless, A.L.; Schild, A.L.; Rains, T.M. Resistant starch from high-amylose maize increases insulin sensitivity in overweight and obese men. J. Nutr. 2012, 142, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.; Ge, J.; Zhao, C.; Le, S.; Yang, Y.; Ke, D.; Wu, N.; Tan, X.; Zhang, X.; Du, X.; et al. Effect of aerobic exercise and diet on liver fat in pre-diabetic patients with non-alcoholic-fatty-liver-disease: A randomized controlled trial. Sci. Rep. 2017, 7, 15952. [Google Scholar] [CrossRef] [PubMed]
- Haufe, S.; Engeli, S.; Kast, P.; Böhnke, J.; Utz, W.; Haas, V.; Hermsdorf, M.; Mähler, A.; Wiesner, S.; Birkenfeld, A.L.; et al. Randomized comparison of reduced fat and reduced carbohydrate hypocaloric diets on intrahepatic fat in overweight and obese human subjects. Hepatology 2011, 53, 1504–1514. [Google Scholar] [CrossRef]
- Sorkin, B.C.; Kuszak, A.J.; Bloss, G.; Fukagawa, N.K.; Hoffman, F.A.; Jafari, M.; Barrett, B.; Brown, P.N.; Bushman, F.D.; Casper, S.J.; et al. Improving natural product research translation: From source to clinical trial. FASEB J. 2020, 34, 41–65. [Google Scholar] [CrossRef]
- Wu, B.; Han, W.; Li, Z.; Zhao, Y.; Ge, M.; Guo, X.; Wu, X. Reproducibility of Intra- and Inter-scanner Measurements of Liver Fat Using Complex Confounder-corrected Chemical Shift Encoded MRI at 3.0 Tesla. Sci. Rep. 2016, 6, 19339. [Google Scholar] [CrossRef]
- Angulo, P. Obesity and nonalcoholic fatty liver disease. Nutr. Rev. 2007, 65, S57–S63. [Google Scholar] [CrossRef]
- Ekstedt, M.; Hagström, H.; Nasr, P.; Fredrikson, M.; Stål, P.; Kechagias, S.; Hultcrantz, R. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 2015, 61, 1547–1554. [Google Scholar] [CrossRef]
| Omega-3 | Phytochemicals (Incl. Resveratrol) | Probiotics | Vitamins | Amino Acid Derivatives | |
|---|---|---|---|---|---|
| Number of RCTs | 4 | 8 | 4 | 3 | 1 |
| Location | |||||
| Europe | 3 | 4 | 1 | 3 | - |
| Asia | - | 2 | 2 | - | 1 |
| Australia | 1 | 1 | - | - | - |
| North America | - | 1 | - | - | - |
| South America | - | - | 1 | - | - |
| Demographics and anthropometrics | |||||
| Total participants (n) | 375 | 369 | 231 | 138 | 72 |
| Age (yrs) | 52 (10.9) 1 | 49 (9.9) 1 | 49.7 (11.6) 1 | 53 (8.3) 1 | 51 (9.2) 1 |
| BMI (kg/m2) | 31.6 (6.2) 1 | 31.6 (3.6) 1 | 32.5 (4.8) 1,2 | 33 (3.5) 1 | 27.5 (3.2) 1 |
| % women | 40 | 36 | 38 | 35 | 31 |
| Specific restricted study population 3 | |||||
| NAFLD | 3 | 5 | 1 | 1 4 | 1 4 |
| NASH | - | - | 2 | - | - |
| PCOS | 1 | - | - | - | - |
| Prediabetic | - | 1 | - | - | - |
| Insulin-resistant | - | 2 | - | - | - |
| T2DM | - | - | - | 1 4 | 1 4 |
| Others | 1 | - | 1 | 2 | - |
| Duration (weeks) | 12–78 | 8–26 | 4–61 | 12–26 | 12 |
| Liver fat measured by | |||||
| MRS | 3 | 6 | 2 | 2 | - |
| MRI | - | - | - | 1 | - |
| MRI-PDFF | 2 | 1 | 1 | - | - |
| CT | - | 1 | 1 | - | 1 |
| Lead Author, Publication Year | Treatment Characteristics | Main Findings 1 | ||
|---|---|---|---|---|
| Dietary Supplement | Control | Duration | ||
| Phytochemicals | ||||
| Lee et al., 2019 | Pinitol, 300 mg or 500 mg | Placebo | 12 weeks | Although there were no significant differences among the treatment groups in the LF content changes using MRI-PDFF, LF content decreased significantly in the low-dose group (p = 0.01), whereas no significant change was detected with the higher pinitol dose.1 |
| Sakata et al., 2013 | Catechins, 200 mg or 1080 mg | Placebo | 12 weeks | The improvement in liver-to-spleen CT attenuation was 11.3% (2.8%) in the high density and −6.1% (12.1%) in the low-density intervention groups vs. −3.3% (8.5%) in the placebo group. Compared to control group, the difference was −2.8% (7.4%) for the low-dose and 14.6% (6.5%), p < 0.05 for the high-dose intervention group. |
| Johnston et al., 2010 | Hi-Maize 260, 40,000 mg | Amioca | 12 weeks | LF fat reduction was −1.7% (7.3%) in the intervention vs. −0.3% (4.5%) in the control group. The between group difference was 1.4% (4.6%) (p = n.s.), measured by MRS. |
| Peterson et al., 2018 | Hi-Maize 260, 45,000 mg | Amioca | 12 weeks | MRS measurements could not show any significant decrease in LF neither in the intervention 0.2% (6.6%) nor in the control group 1.6% (6.7%) and between both groups −1.3% (4.0%), p = 0.23. |
| Probiotics and medicinal mushrooms | ||||
| Ferolla et al., 2016 | Synbiotic (Lactobaccillus reuteri), 0.1 × 109 CFU | Usual diet | 13 weeks | LF, measured by MRI-PDFF, decreased by −2.5% (4.5%) in the intervention (p = 0.03) and by 3.0% (5.5%) in the control group (p = 0.15). The between group difference was 5.5% (3.3%) (p-value not reported). |
| Scorletti et al., 2020 | Synbiotic (Bifidobacterium animalis (subspecies lactis BB-12)), 1.0 × 109 CFU | Maltodextrin, 8000 mg | 44–61 weeks | LF, measured by MRS, changed by −3.8% (4.3%) in the intervention and by −6.1% (4.0%) in the control group. No significant between group difference was detected 2.3% (2.6%), p = 0.30. |
| Wong et al., 2013 | Probiotics (Lactobaccillus plantarum, L. delbrueckii spp. bulgaricus, L. acidophilus, L. rhamnosus; Bifidobacterium bifidum), 0.2 × 109 CFU | Usual diet | 26 weeks | LF, measured by MRS, decreased significantly in the intervention −7.7% (9.8%), p = 0.03, and remained static in the control group at −0.9% (4.9%), p = 0.15. No significant change between the groups was detected (between group difference −6.8% (2.0%), p = 0.07). |
| Heo et al., 2015 | Ascomycetes (Cordyceps militaris), 1500 mg | Placebo | 4 weeks | In analysis of the liver CT scan the mean ratio of change of Hounsfield increased by an average of 21.4% (45.1%; mean (SEM)) in the intervention group and 9.6% (11.4%; mean (SEM)) in the control group (p = 0.10). |
| Vitamins | ||||
| Barchetta et al., 2016 | Vitamin D, 2000 IU | Placebo | 24 weeks | Changes in LF, measured by MRI, of −0.4% (2.1%) in the intervention and of −0.7% (1.5%) in the control group, did not differ significantly between both groups 0.3% (1.3%; p = 0.57). |
| Wamberg et al., 2011 | Vitamin D, 7000 IU | Placebo | 26 weeks | LF, assessed by MRS as the arbitrary lipid:water ratio, changed by 0.05% (0.07%), p = 0.11 in the intervention group and by 0.00% (0.06%), p = 0.61 in the control group. The difference between the groups of 0.05% (0.04%) was not significant (p = 0.51). |
| Dollerup et al., 2018 | Nicotinamide riboside, 2000 mg | Placebo | 12 weeks | A 2% (2.6%) reduction in LF in the intervention group was measured by MRS compared to a 0.2% (2.6%) reduction in the control group. No significant difference between groups was found −1.8% (1.7%), p = 0.13. |
| Amino-acid derivatives | ||||
| Bae et al., 2015 | Carnitine-orotate, 2472 mg | Placebo | 12 weeks | On the hepatic CT analysis, mean changes in liver-to-spleen attenuation ratio were 6.2% (9.0%), p < 0.01 in the intervention group and 0.7% (8.1%), p = 0.58 in the control group. These results showed a significant difference in LF reduction between both groups 5.5% (5.4%), p = 0.01. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kilchoer, B.; Vils, A.; Minder, B.; Muka, T.; Glisic, M.; Bally, L. Efficacy of Dietary Supplements to Reduce Liver Fat. Nutrients 2020, 12, 2302. https://doi.org/10.3390/nu12082302
Kilchoer B, Vils A, Minder B, Muka T, Glisic M, Bally L. Efficacy of Dietary Supplements to Reduce Liver Fat. Nutrients. 2020; 12(8):2302. https://doi.org/10.3390/nu12082302
Chicago/Turabian StyleKilchoer, Brittanie, Anina Vils, Beatrice Minder, Taulant Muka, Marija Glisic, and Lia Bally. 2020. "Efficacy of Dietary Supplements to Reduce Liver Fat" Nutrients 12, no. 8: 2302. https://doi.org/10.3390/nu12082302
APA StyleKilchoer, B., Vils, A., Minder, B., Muka, T., Glisic, M., & Bally, L. (2020). Efficacy of Dietary Supplements to Reduce Liver Fat. Nutrients, 12(8), 2302. https://doi.org/10.3390/nu12082302








