Trajectories of Dietary Patterns, Sleep Duration, and Body Mass Index in China: A Population-Based Longitudinal Study from China Nutrition and Health Survey, 1991–2009
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Outcome Measures: Sleep Duration and BMI
2.3. Dietary Consumption
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Dietary Patterns
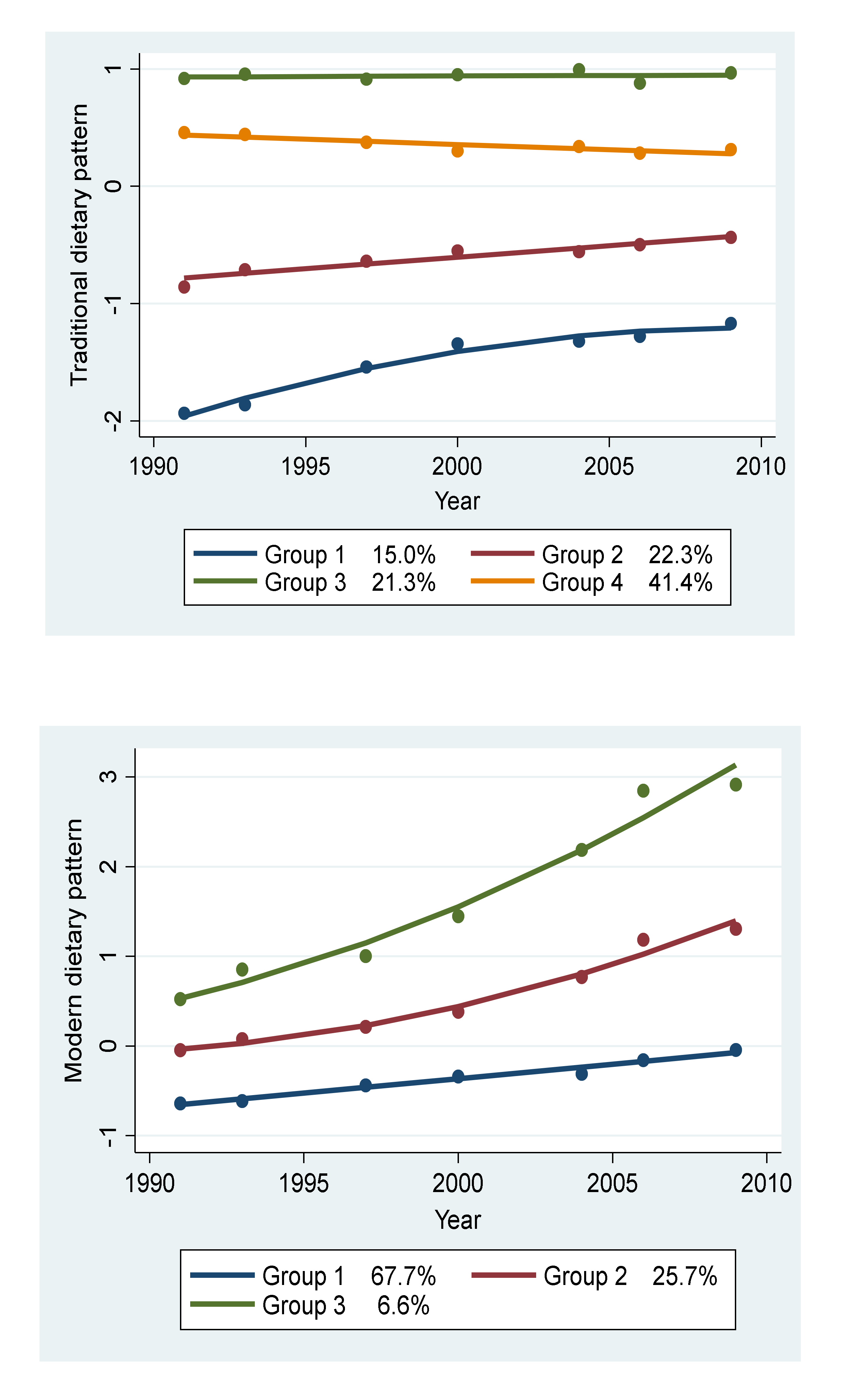
3.2. Trajectories of Dietary Patterns
3.3. Participants’ Characteristics by Trajectory Groups
3.4. Trajectory of Dietary Patterns and Sleep Duration
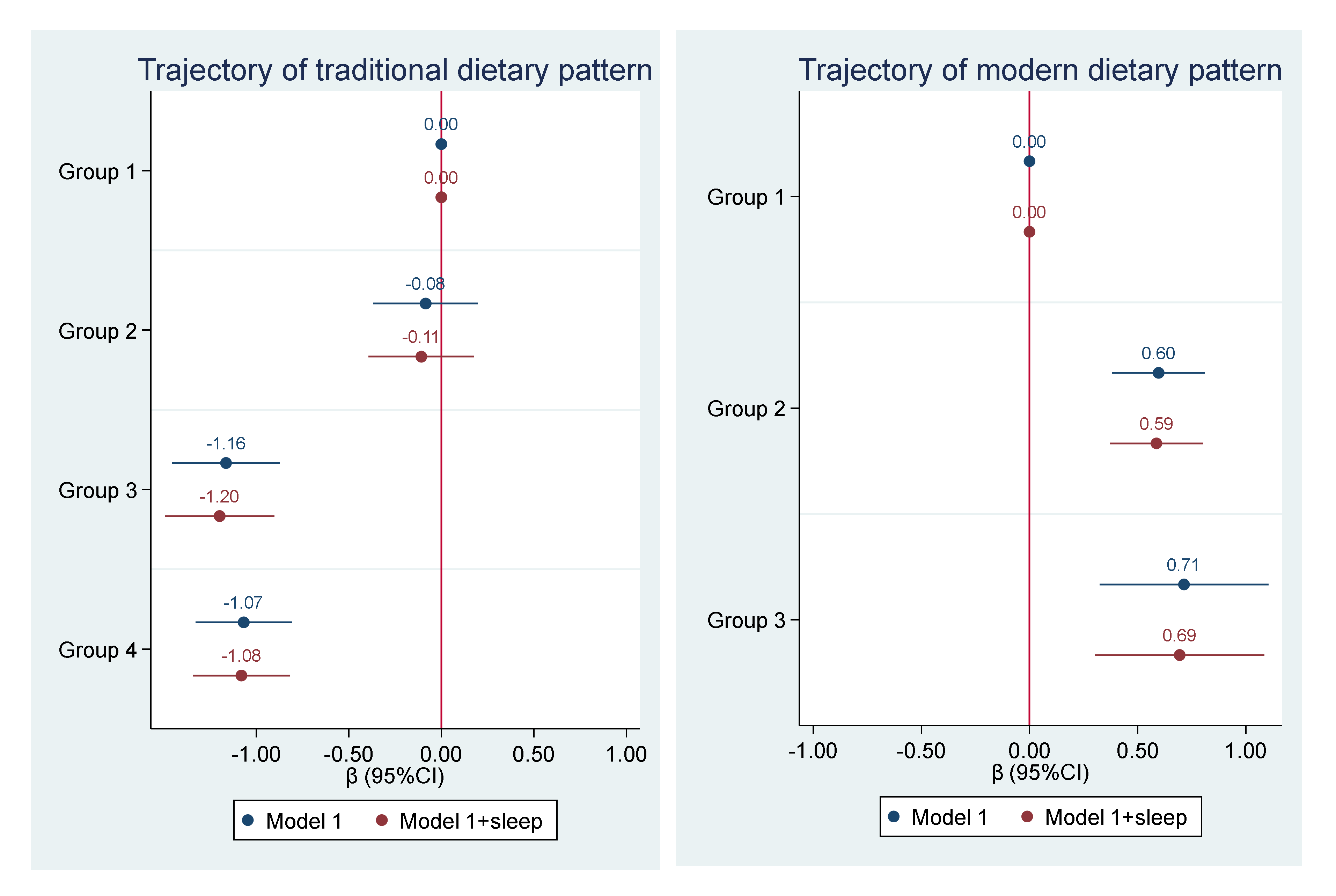
3.5. Trajectory of Dietary Patterns and BMI
4. Discussion
4.1. Demographic Characteristics among the Trajectories of Dietary Patterns
4.2. Trajectories of Dietary Patterns and Sleep Duration
4.3. Trajectories of Dietary Patterns and BMI
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Knutson, K.L. Sleep duration and cardiometabolic risk: A review of the epidemiologic evidence. Best Pr. Res. Clin. Endocrinol. Metab. 2010, 24, 731–743. [Google Scholar] [CrossRef] [PubMed]
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 2017, 32, 246–256. [Google Scholar] [CrossRef]
- Stranges, S.; Tigbe, W.; Gómez-Olivé, F.X.; Thorogood, M.; Kandala, N.-B. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 2012, 35, 1173–1181. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Kartsonaki, C.; Clarke, R.; Guo, Y.; Yu, C.; Bian, Z.; Jiang, Q.; Li, S.; Chen, J.; Li, L.; et al. Characteristics and correlates of sleep duration, daytime napping, snoring and insomnia symptoms among 0.5 million Chinese men and women. Sleep Med. 2018, 44, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Wang, S.-B.; Rao, W.-W.; Ungvari, G.S.; Ng, C.H.; Chiu, H.F.K.; Zhang, J.; Kou, C.; Jia, F.-J.; Xiang, Y.-T. Sleep Duration and Patterns in Chinese Older Adults: A Comprehensive Meta-analysis. Int. J. Boil. Sci. 2017, 13, 682–689. [Google Scholar] [CrossRef]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short sleep duration and dietary intake: Epidemiologic evidence, mechanisms, and health implications. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef]
- Grandner, M.A.; Kripke, D.F.; Naidoo, N.; Langer, R.D. Relationships among dietary nutrients and subjective sleep, objective sleep, and napping in women. Sleep Med. 2010, 11, 180–184. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Mikic, A.; Pietrolungo, C.E. Effects of Diet on Sleep Quality. Adv. Nutr. 2016, 7, 938–949. [Google Scholar] [CrossRef]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef]
- Cao, Y.; Taylor, A.W.; Wittert, G.; Adams, R.; Shi, Z. Dietary patterns and sleep parameters in a cohort of community dwelling Australian men. Asia Pac. J. Clin. Nutr. 2017, 26, 1158–1169. [Google Scholar]
- Mondin, T.C.; Stuart, A.L.; Williams, L.J.; Jacka, F.N.; Pasco, J.A.; Ruusunen, A. Diet quality, dietary patterns and short sleep duration: A cross-sectional population-based study. Eur. J. Nutr. 2019, 58, 641–651. [Google Scholar] [CrossRef] [PubMed]
- Zhai, F.; Wang, H.; Du, S.; He, Y.; Wang, Z.; Ge, K.; Popkin, B.M. Prospective study on nutrition transition in China. Nutr. Rev. 2009, 67, S56–S61. [Google Scholar] [CrossRef] [PubMed]
- Batis, C.; Sotres-Alvarez, D.; Gordon-Larsen, P.; Mendez, M.A.; Adair, L.; Popkin, B. Longitudinal analysis of dietary patterns in Chinese adults from 1991 to 2009. Br. J. Nutr. 2014, 111, 1441–1451. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Shi, Z. Dietary Pattern during 1991–2011 and Its Association with Cardio Metabolic Risks in Chinese Adults: The China Health and Nutrition Survey. Nutrients 2017, 9, 1218. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.; Shi, Z.; Lv, J.; Guo, Y.; Bian, Z.; Du, H.; Chen, Y.; Tao, R.; Huang, Y.; Chen, J.; et al. Dietary Patterns and Insomnia Symptoms in Chinese Adults: The China Kadoorie Biobank. Nutrients 2017, 9, 232. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.L.; Nagin, D.S. Advances in Group-Based Trajectory Modeling and an SAS Procedure for Estimating Them. Sociol. Methods Res. 2007, 35, 542–571. [Google Scholar] [CrossRef]
- Smithers, L.G.; Golley, R.K.; Mittinty, M.N.; Brazionis, L.; Northstone, K.; Emmett, P.; Lynch, J.W. Do Dietary Trajectories between Infancy and Toddlerhood Influence IQ in Childhood and Adolescence? Results from a Prospective Birth Cohort Study. PLoS ONE 2013, 8, e58904. [Google Scholar] [CrossRef]
- Gao, M.; Wang, F.; Shen, Y.; Zhu, X.; Zhang, X.; Sun, X. Trajectories of Mediterranean Diet Adherence and Risk of Hypertension in China: Results from the CHNS Study, 1997–2011. Nutrients 2018, 10, 2014. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef]
- Xu, X.; Byles, J.E.; Shi, Z.; Hall, J.J. Evaluation of older Chinese people’s macronutrient intake status: Results from the China Health and Nutrition Survey. Br. J. Nutr. 2015, 113, 159–171. [Google Scholar] [CrossRef]
- Feng, X.; Liu, Q.; Li, Y.; Zhao, F.; Chang, H.; Lyu, J. Longitudinal study of the relationship between sleep duration and hypertension in Chinese adult residents (CHNS 2004–2011). Sleep Med. 2019, 58, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Lu, F.C. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed. Environ. Sci. 2004, 17, 1–36. [Google Scholar]
- Zhai, F.Y.; Du, S.F.; Wang, Z.H.; Zhang, J.G.; Du, W.W.; Popkin, B.M. Dynamics of the Chinese diet and the role of urbanicity, 1991–2011. Obes. Rev. 2014, 15, 16–26. [Google Scholar] [CrossRef]
- Foster, E.; Lee, C.; Imamura, F.; Hollidge, S.E.; Westgate, K.L.; Venables, M.C.; Poliakov, I.; Rowland, M.K.; Osadchiy, T.; Bradley, J.C.; et al. Validity and reliability of an online self-report 24-h dietary recall method (Intake24): A doubly labelled water study and repeated-measures analysis. J. Nutr. Sci. 2019, 8, e29. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R.; Schmitz, K.H., Jr.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef] [PubMed]
- Reeves, M.M.; Healy, G.N.; Owen, N.; Shaw, J.E.; Zimmet, P.Z.; Dunstan, D.W. Joint associations of poor diet quality and prolonged television viewing time with abnormal glucose metabolism in Australian men and women. Prev. Med. 2013, 57, 471–476. [Google Scholar] [CrossRef]
- Nishiura, C.; Noguchi, J.; Hashimoto, H. Dietary patterns only partially explain the effect of short sleep duration on the incidence of obesity. Sleep 2010, 33, 753–757. [Google Scholar] [CrossRef]
- Cao, X.L.; Wang, S.B.; Zhong, B.L.; Zhang, L.; Ungvari, G.S.; Ng, C.H.; Li, L.; Chiu, H.F.; Lok, G.K.; Lu, J.P.; et al. The prevalence of insomnia in the general population in China: A meta-analysis. PLoS ONE 2017, 12, e0170772. [Google Scholar] [CrossRef]
- Xu, X.; Hall, J.; Byles, J.; Shi, Z. Dietary Pattern Is Associated with Obesity in Older People in China: Data from China Health and Nutrition Survey (CHNS). Nutrients 2015, 7, 8170–8188. [Google Scholar] [CrossRef]
- Murakami, K.; Sasaki, S.; Okubo, H.; Takahashi, Y.; Hosoi, Y.; Itabashi, M. Dietary fiber intake, dietary glycemic index and load, and body mass index: A cross-sectional study of 3931 Japanese women aged 18–20 years. Eur. J. Clin. Nutr. 2007, 61, 986–995. [Google Scholar] [CrossRef]
- Prentice, A.M.; Jebb, S.A. Fast foods, energy density and obesity: A possible mechanistic link. Obes. Rev. 2003, 4, 187–194. [Google Scholar] [CrossRef]
- Batis, C.; Mendez, M.A.; Sotres-Alvarez, D.; Gordon-Larsen, P.; Popkin, B. Dietary pattern trajectories during 15|years of follow-up and HbA1c, insulin resistance and diabetes prevalence among Chinese adults. J. Epidemiol. Community Health 2014, 68, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Sadeh, A. The role and validity of actigraphy in sleep medicine: An update. Sleep Med. Rev. 2011, 15, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Jurado-Fasoli, L.; De-la, O.A.; Molina-Hidalgo, C.; Migueles, J.H.; Castillo, M.J.; Amaro-Gahete, F.J. Exercise training improves sleep quality: A randomized controlled trial. Eur. J. Clin. Investig. 2020, 50, e13202. [Google Scholar] [CrossRef] [PubMed]
| Group 1: Low and Rapid Increase | Group 2: Medium and Slow Increase | Group 3: High and Stable | Group 4: High and Slow Decrease | p-Value | |
|---|---|---|---|---|---|
| n = 1030 | n = 1508 | n = 1473 | n = 2932 | ||
| Age (years), mean (SD) | 53.7 (12.9) | 54.9 (13.3) | 52.1 (11.9) | 55.2 (13.7) | <0.001 |
| Sex, n (%) | <0.001 | ||||
| Men | 516 (50.1%) | 650 (43.1%) | 956 (64.9%) | 1242 (42.4%) | |
| Women | 514 (49.9%) | 858 (56.9%) | 517 (35.1%) | 1690 (57.6%) | |
| Education, n (%) | <0.001 | ||||
| Low | 585 (56.8%) | 704 (46.7%) | 541 (36.8%) | 1429 (48.9%) | |
| Medium | 317 (30.8%) | 478 (31.7%) | 555 (37.8%) | 876 (30.0%) | |
| High | 128 (12.4%) | 325 (21.6%) | 374 (25.4%) | 618 (21.1%) | |
| Urbanization, n (%) | <0.001 | ||||
| Low | 421 (40.9%) | 286 (19.0%) | 151 (10.3%) | 196 (6.7%) | |
| Medium | 361 (35.0%) | 580 (38.5%) | 425 (28.9%) | 1317 (44.9%) | |
| High | 248 (24.1%) | 642 (42.6%) | 897 (60.9%) | 1419 (48.4%) | |
| Smoking, n (%) | <0.001 | ||||
| Nonsmoker | 679 (65.9%) | 1034 (68.6%) | 849 (57.7%) | 2107 (71.9%) | |
| Ex-smokers | 53 (5.1%) | 50 (3.3%) | 60 (4.1%) | 97 (3.3%) | |
| Current smokers | 298 (28.9%) | 423 (28.1%) | 563 (38.2%) | 727 (24.8%) | |
| Alcohol drinking, n (%) | 330 (32.3%) | 458 (30.4%) | 670 (45.8%) | 852 (29.2%) | <0.001 |
| Tea consumption (cups/d), n (%) | <0.001 | ||||
| None | 784 (76.2%) | 1066 (70.8%) | 795 (54.5%) | 1874 (64.1%) | |
| <2 cup/d | 67 (6.5%) | 132 (8.8%) | 177 (12.1%) | 312 (10.7%) | |
| 2–3.9 cup/d | 91 (8.8%) | 154 (10.2%) | 204 (14.0%) | 360 (12.3%) | |
| ≥4 cup/d | 87 (8.5%) | 153 (10.2%) | 283 (19.4%) | 378 (12.9%) | |
| Physical activity (MET, hour/week), mean (SD) | 138.2 (116.8) | 138.0 (121.5) | 127.0 (102.2) | 118.8 (104.6) | <0.001 |
| BMI (kg/m2), mean (SD) | 24.0 (3.4) | 24.2 (3.5) | 23.2 (3.2) | 23.1 (3.5) | <0.001 |
| BMI >24 (kg/m2), n (%) | 468 (48.0%) | 712 (48.9%) | 501 (36.4%) | 1022 (36.5%) | <0.001 |
| Hypertension, n (%) | 295 (29.7%) | 514 (34.8%) | 382 (27.6%) | 828 (29.2%) | <0.001 |
| Diabetes, n (%) | 22 (2.1%) | 61 (4.1%) | 34 (2.3%) | 91 (3.1%) | 0.012 |
| Stroke, n (%) | 25 (2.4%) | 29 (1.9%) | 13 (0.9%) | 39 (1.3%) | 0.008 |
| Sleep duration (hour/d), mean (SD) | 8.1 (1.2) | 7.9 (1.2) | 7.9 (1.1) | 7.9 (1.2) | <0.001 |
| Sleep duration, n (%) | <0.001 | ||||
| 7–9 h | 794 (77.1%) | 1174 (77.9%) | 1191 (80.9%) | 2252 (76.8%) | |
| ≤6 h | 86 (8.3%) | 163 (10.8%) | 149 (10.1%) | 333 (11.4%) | |
| >9 h | 150 (14.6%) | 171 (11.3%) | 133 (9.0%) | 347 (11.8%) |
| Group 1: Low and Slow Increase | Group 2: Medium and Moderate Increase | Group 3: High and Rapid Increase | p-Value | |
|---|---|---|---|---|
| n = 4864 | n = 1689 | n = 390 | ||
| Age (years), mean (SD) | 54.4 (13.3) | 53.9 (12.8) | 54.0 (13.6) | 0.41 |
| Sex, n (%) | <0.001 | |||
| Men | 2274 (46.8%) | 856 (50.4%) | 234 (60.8%) | |
| Women | 2584 (53.2%) | 844 (49.6%) | 151 (39.2%) | |
| Education, n (%) | <0.001 | |||
| Low | 2666 (55.0%) | 531 (31.3%) | 62 (16.1%) | |
| Medium | 1552 (32.0%) | 564 (33.2%) | 110 (28.6%) | |
| High | 629 (13.0%) | 604 (35.6%) | 212 (55.2%) | |
| Urbanization, n (%) | <0.001 | |||
| Low | 959 (19.7%) | 90 (5.3%) | 5 (1.3%) | |
| Medium | 2245 (46.2%) | 392 (23.1%) | 46 (11.9%) | |
| High | 1654 (34.0%) | 1218 (71.6%) | 334 (86.8%) | |
| Smoking, n (%) | <0.001 | |||
| Nonsmoker | 3287 (67.7%) | 1148 (67.6%) | 234 (60.8%) | |
| Ex-smokers | 164 (3.4%) | 67 (3.9%) | 29 (7.5%) | |
| Current smokers | 1405 (28.9%) | 484 (28.5%) | 122 (31.7%) | |
| Alcohol drinking, n (%) | 1462 (30.3%) | 652 (38.5%) | 196 (51.0%) | <0.001 |
| Tea consumption (cups/d) | <0.001 | |||
| None | 3357 (69.4%) | 1003 (59.3%) | 159 (41.3%) | |
| <2 cup/d | 449 (9.3%) | 186 (11.0%) | 53 (13.8%) | |
| 2–3.9 cup/d | 515 (10.6%) | 229 (13.5%) | 65 (16.9%) | |
| ≥4 cup/d | 519 (10.7%) | 274 (16.2%) | 108 (28.1%) | |
| Physical activity (MET, hour/week), mean (SD) | 135.0 (116.0) | 110.8 (95.3) | 106.3 (77.8) | <0.001 |
| BMI (kg/m2), mean (SD) | 23.2 (3.4) | 24.1 (3.5) | 24.2 (3.6) | <0.001 |
| BMI >24 (kg/m2), n (%) | 1733 (37.6%) | 785 (48.2%) | 185 (50.4%) | <0.001 |
| Hypertension, n (%) | 1369 (29.3%) | 530 (32.2%) | 120 (31.7%) | 0.073 |
| Diabetes, n (%) | 104 (2.1%) | 80 (4.7%) | 24 (6.2%) | <0.001 |
| Stroke, n (%) | 74 (1.5%) | 24 (1.4%) | 8 (2.1%) | 0.63 |
| Sleep (hour/week), mean (SD) | 8.0 (1.2) | 7.7 (1.1) | 7.6 (1.1) | <0.001 |
| Sleep duration, n (%) | <0.001 | |||
| 7–9 h | 3731 (76.8%) | 1361 (80.1%) | 319 (82.9%) | |
| ≤6 h | 469 (9.7%) | 217 (12.8%) | 45 (11.7%) | |
| >9 h | 658 (13.5%) | 122 (7.2%) | 21 (5.5%) |
| Traditional Pattern | ||||
| Group 1: Low and rapid increase | Group 2: Medium and slow increase | Group 3: High and stable | Group 4: High and slow decrease | |
| Model 1 | Reference | −0.18 (−0.27, −0.08) | −0.21 (−0.31, −0.11) | −0.15 (−0.24, −0.06) |
| Model 2 | Reference | −0.02 (−0.12, 0.08) | 0.00 (−0.10, 0.11) | 0.02 (−0.07, 0.12) |
| Model 3 | Reference | −0.01 (−0.11, 0.09) | 0.01 (−0.09, 0.12) | 0.02 (−0.07, 0.12) |
| Model 4 | Reference | 0.01 (−0.12, 0.13) | 0.07 (−0.06, 0.20) | 0.02 (−0.09, 0.13) |
| Modern Pattern | ||||
| Group 1: Low and slow increase | Group 2: Medium and moderate increase | Group 3: High and rapid increase | ||
| Model 1 | Reference | −0.30 (−0.36, −0.23) | −0.39 (−0.52, −0.27) | |
| Model 2 | Reference | −0.20 (−0.28, −0.13) | −0.26 (−0.40, −0.13) | |
| Model 3 | Reference | −0.20 (−0.28, −0.13) | −0.26 (−0.40, −0.12) | |
| Model 4 | Reference | −0.18 (−0.27, −0.09) | −0.15 (−0.33, 0.02) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, Y.; Xu, X.; Shi, Z. Trajectories of Dietary Patterns, Sleep Duration, and Body Mass Index in China: A Population-Based Longitudinal Study from China Nutrition and Health Survey, 1991–2009. Nutrients 2020, 12, 2245. https://doi.org/10.3390/nu12082245
Cao Y, Xu X, Shi Z. Trajectories of Dietary Patterns, Sleep Duration, and Body Mass Index in China: A Population-Based Longitudinal Study from China Nutrition and Health Survey, 1991–2009. Nutrients. 2020; 12(8):2245. https://doi.org/10.3390/nu12082245
Chicago/Turabian StyleCao, Yingting, Xiaoyue Xu, and Zumin Shi. 2020. "Trajectories of Dietary Patterns, Sleep Duration, and Body Mass Index in China: A Population-Based Longitudinal Study from China Nutrition and Health Survey, 1991–2009" Nutrients 12, no. 8: 2245. https://doi.org/10.3390/nu12082245
APA StyleCao, Y., Xu, X., & Shi, Z. (2020). Trajectories of Dietary Patterns, Sleep Duration, and Body Mass Index in China: A Population-Based Longitudinal Study from China Nutrition and Health Survey, 1991–2009. Nutrients, 12(8), 2245. https://doi.org/10.3390/nu12082245







