Serum Mac-2 Binding Protein Levels Associate with Metabolic Parameters and Predict Liver Fibrosis Progression in Subjects with Fatty Liver Disease: A 7-Year Longitudinal Study
Abstract
1. Introduction
2. Patients and Methods
2.1. Ethical Committee Approval
2.2. Subjects in Medical Health Check-Ups
2.3. Anthropometric and Laboratory Evaluation
2.4. Diagnostic Criteria for Metabolic Syndrome-Related Diseases
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Study Participants
3.2. Serum M2BP Levels were Significantly Correlated with Liver Enzymes and Metabolic-Related Variables
3.3. Among Metabolic Syndrome-Related Diseases, Fatty Liver Disease Was an Independent Determinant for Serum M2BP Levels
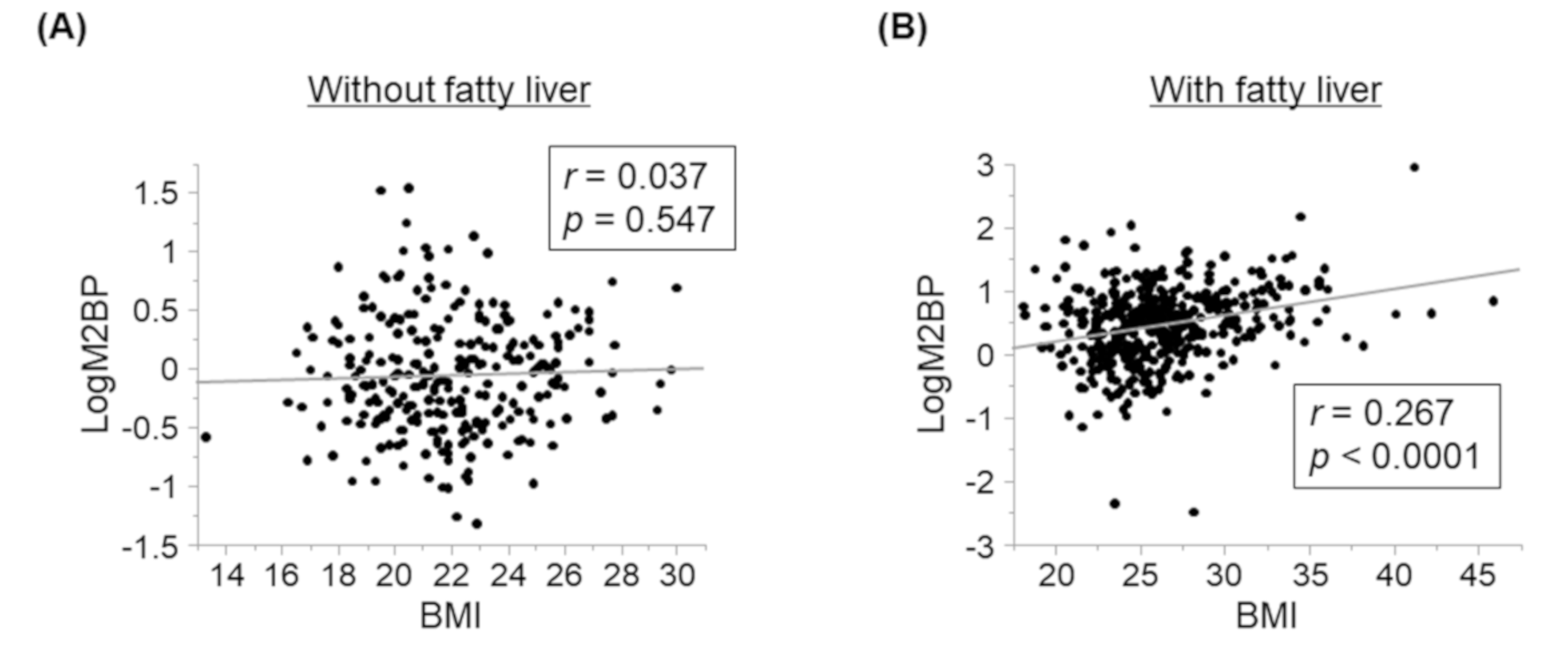
3.4. Serum M2BP Levels Were Significantly Correlated with BMI in FL+ Subjects but Not in FL− Subjects
3.5. Relationships between Serum M2BP Levels at Baseline and Changes in Various Parameters
3.6. Serum M2BP Levels Could Serve as a Predictive Biomarker for Liver Fibrosis Progression
3.7. Relationships between Changes in M2BP Levels and Other Parameters
3.8. Changes in GGT and CHE Were Independent Determinants for Changes in M2BP Levels
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ford, E.S.; Giles, W.H.; Dietz, W.H. Prevalence of the metabolic syndrome among us adults: Findings from the third national health and nutrition examination survey. JAMA 2002, 287, 356–359. [Google Scholar] [CrossRef] [PubMed]
- Shirabe, K.; Takeishi, K.; Taketomi, A.; Uchiyama, H.; Kayashima, H.; Maehara, Y. Improvement of Long-Term Outcomes in Hepatitis C Virus Antibody–Positive Patients with Hepatocellular Carcinoma after Hepatectomy in the Modern Era. World J. Surg. 2011, 35, 1072–1084. [Google Scholar] [CrossRef] [PubMed]
- Mazzaferro, V.; Regalia, E.; Doci, R.; Andreola, S.; Pulvirenti, A.; Bozzetti, F.; Montalto, F.; Ammatuna, M.; Morabito, A.; Gennari, L. Liver Transplantation for the Treatment of Small Hepatocellular Carcinomas in Patients with Cirrhosis. N. Engl. J. Med. 1996, 334, 693–700. [Google Scholar] [CrossRef]
- Bravo, A.A.; Sheth, S.G.; Chopra, S. Liver Biopsy. N. Engl. J. Med. 2001, 344, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Gebo, K.A.; Herlong, H.F.; Torbenson, M.S.; Jenckes, M.W.; Chander, G.; Ghanem, K.G.; El-Kamary, S.S.; Sulkowski, M.; Bass, E.B. Role of liver biopsy in management of chronic hepatitis C: A systematic review. Hepatology 2002, 36, s161–s172. [Google Scholar] [CrossRef]
- Piccinino, F.; Sagnelli, E.; Pasquale, G.; Giusti, G. Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J. Hepatol. 1986, 2, 165–173. [Google Scholar] [CrossRef]
- Ratziu, V.; Charlotte, F.; Heurtier, A.; Gombert, S.; Giral, P.; Bruckert, E.; Grimaldi, A.; Capron, F.; Poynard, T. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology 2005, 128, 1898–1906. [Google Scholar] [CrossRef]
- Angulo, P.; Kleiner, D.; Dam-Larsen, S.; Adams, L.A.; Björnsson, E.S.; Charatcharoenwitthaya, P.; Mills, P.R.; Keach, J.C.; Lafferty, H.D.; Stahler, A.; et al. Liver Fibrosis, but No Other Histologic Features, Is Associated with Long-term Outcomes of Patients with Nonalcoholic Fatty Liver Disease. Gastroenterology 2015, 149, 389–397.e10. [Google Scholar] [CrossRef]
- Yoneda, M.; Fujita, K.; Inamori, M.; Nakajima, A.; Tamano, M.; Hiraishi, H. Transient elastography in patients with non-alcoholic fatty liver disease (NAFLD). Gut 2007, 56, 1330–1331. [Google Scholar] [CrossRef]
- Yoneda, M.; Suzuki, K.; Kato, S.; Fujita, K.; Nozaki, Y.; Hosono, K.; Saito, S.; Nakajima, A. Nonalcoholic Fatty Liver Disease: US-based Acoustic Radiation Force Impulse Elastography. Radiology 2010, 256, 640–647. [Google Scholar] [CrossRef]
- Castera, L.; Forns, X.; Alberti, A. Non-invasive evaluation of liver fibrosis using transient elastography. J. Hepatol. 2008, 48, 835–847. [Google Scholar] [CrossRef] [PubMed]
- Angulo, P.; Hui, J.M.; Marchesini, G.; Bugianesi, E.; George, J.; Farrell, G.C.; Enders, F.; Saksena, S.; Burt, A.; Bida, J.P.; et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007, 45, 846–854. [Google Scholar] [CrossRef]
- Dixon, J.; Bhathal, P.S.; O’Brien, P.E. Nonalcoholic fatty liver disease: Predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology 2001, 121, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.A.; Oliver, D.; Arnold, H.L.; Gogia, S.; Neuschwander-Tetri, B. A Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut 2008, 57, 1441–1447. [Google Scholar] [CrossRef] [PubMed]
- Sumida, Y.; Japan Study Group of Nonalcoholic Fatty Liver Disease (JSG-NAFLD); Yoneda, M.; Hyogo, H.; Yamaguchi, K.; Ono, M.; Fujii, H.; Eguchi, Y.; Suzuki, Y.; Imai, S.; et al. A simple clinical scoring system using ferritin, fasting insulin, and type IV collagen 7S for predicting steatohepatitis in nonalcoholic fatty liver disease. J. Gastroenterol. 2010, 46, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Grassadonia, A.; Tinari, N.; Iurisci, I.; Piccolo, E.; Cumashi, A.; Innominato, P.; D’Egidio, M.; Natoli, C.; Piantelli, M.; Iacobelli, S. 90K (Mac-2 BP) and galectins in tumor progression and metastasis. Glycoconj. J. 2002, 19, 551–556. [Google Scholar] [CrossRef]
- Przybyło, M.; Martuszewska, D.; Pocheć, E.; Hoja-Łukowicz, D.; Litynska, A. Identification of proteins bearing β1–6 branched N-glycans in human melanoma cell lines from different progression stages by tandem mass spectrometry analysis. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2007, 1770, 1427–1435. [Google Scholar] [CrossRef]
- Kamada, Y.; Fujii, H.; Fujii, H.; Sawai, Y.; Doi, Y.; Uozumi, N.; Mizutani, K.; Akita, M.; Sato, M.; Kida, S.; et al. Serum Mac-2 binding protein levels as a novel diagnostic biomarker for prediction of disease severity and nonalcoholic steatohepatitis. Proteom. Clin. Appl. 2013, 7, 648–656. [Google Scholar] [CrossRef]
- Artini, M.; Natoli, C.; Tinari, N.; Costanzo, A.; Marinelli, R.; Balsano, C.; Porcari, P.; Angelucci, D.; D’Egidio, M.; Levrero, M.; et al. Elevated serum levels of 90K/MAC-2 BP predict unresponsiveness to α-interferon therapy in chronic HCV hepatitis patients. J. Hepatol. 1996, 25, 212–217. [Google Scholar] [CrossRef]
- Cheung, K.J.; Tilleman, K.; Deforce, D.; Colle, I.; Van Vlierberghe, H. The HCV serum proteome: A search for fibrosis protein markers. J. Viral Hepat. 2009, 16, 418–429. [Google Scholar] [CrossRef]
- Kamada, Y.; Ono, M.; Hyogo, H.; Fujii, H.; Sumida, Y.; Mori, K.; Tanaka, S.; Yamada, M.; Akita, M.; Mizutani, K.; et al. A novel noninvasive diagnostic method for nonalcoholic steatohepatitis using two glycobiomarkers. Hepatology 2015, 62, 1433–1443. [Google Scholar] [CrossRef] [PubMed]
- Kuno, A.; Ikehara, Y.; Tanaka, Y.; Ito, K.; Matsuda, A.; Sekiya, S.; Hige, S.; Sakamoto, M.; Kage, M.; Mizokami, M.; et al. A serum “sweet-doughnut” protein facilitates fibrosis evaluation and therapy assessment in patients with viral hepatitis. Sci. Rep. 2013, 3, 1065. [Google Scholar] [CrossRef] [PubMed]
- Abe, M.; Miyake, T.; Kuno, A.; Imai, Y.; Sawai, Y.; Hino, K.; Hara, Y.; Hige, S.; Sakamoto, M.; Yamada, G.; et al. Association between Wisteria floribunda agglutinin-positive Mac-2 binding protein and the fibrosis stage of non-alcoholic fatty liver disease. J. Gastroenterol. 2014, 50, 776–784. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Murotani, K.; Nakade, Y.; Inoue, T.; Nakao, H.; Sumida, Y.; Kamada, Y.; Yoneda, M. Serum Wisteria floribunda agglutinin-positive Mac-2-binding protein levels and liver fibrosis: A meta-analysis. J. Gastroenterol. Hepatol. 2017, 32, 1922–1930. [Google Scholar] [CrossRef]
- Zou, X.; Zhu, M.; Yu, D.; Li, W.; Zhang, D.; Lu, F.; Gong, Q.-M.; Liu, F.; Jiang, J.-H.; Zheng, M.; et al. Serum WFA+-M2BP levels for evaluation of early stages of liver fibrosis in patients with chronic hepatitis B virus infection. Liver Int. 2016, 37, 35–44. [Google Scholar] [CrossRef]
- Nishikawa, H.; Enomoto, H.; Iwata, Y.; Hasegawa, K.; Nakano, C.; Takata, R.; Nishimura, T.; Kazunori, Y.; Aizawa, N.; Sakai, Y.; et al. Impact of serum Wisteria floribunda agglutinin-positive Mac-2-binding protein and serum interferon-?-inducible protein-10 in primary biliary cirrhosis. Hepatol. Res. 2015, 46, 575–583. [Google Scholar] [CrossRef]
- Nishikawa, H.; Enomoto, H.; Iwata, Y.; Hasegawa, K.; Nakano, C.; Takata, R.; Nishimura, T.; Yoh, K.; Aizawa, N.; Sakai, Y.; et al. Clinical significance of serum Wisteria floribunda agglutinin positive Mac-2-binding protein level and high-sensitivity C-reactive protein concentration in autoimmune hepatitis. Hepatol. Res. 2015, 46, 613–621. [Google Scholar] [CrossRef]
- Kamada, Y.; Ono, M.; Hyogo, H.; Fujii, H.; Sumida, Y.; Yamada, M.; Mori, K.; Tanaka, S.; Maekawa, T.; Ebisutani, Y.; et al. Use of Mac-2 binding protein as a biomarker for nonalcoholic fatty liver disease diagnosis. Hepatol. Commun. 2017, 1, 780–791. [Google Scholar] [CrossRef]
- Åberg, F.; Helenius-Hietala, J.; Puukka, P.; Färkkilä, M.; Jula, A. Interaction between alcohol consumption and metabolic syndrome in predicting severe liver disease in the general population. Hepatology 2018, 67, 2141–2149. [Google Scholar] [CrossRef]
- Åberg, F.; Färkkilä, M. Drinking and Obesity: Alcoholic Liver Disease/Nonalcoholic Fatty Liver Disease Interactions. Semin. Liver Dis. 2020, 40, 154–162. [Google Scholar] [CrossRef]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Gomez, M.R.; Zelber-Sagi, S.; Wong, V.W.-S.; Dufour, J.-F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Saadeh, S.; Younossi, Z.M.; Remer, E.M.; Gramlich, T.; Ong, J.P.; Hurley, M.; Mullen, K.D.; Cooper, J.N.; Sheridan, M.J. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology 2002, 123, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Hamano, M.; Kamada, Y.; Kiso, S.; Furuta, K.; Kizu, T.; Chatani, N.; Egawa, M.; Takemura, T.; Ezaki, H.; Yoshida, Y.; et al. Adiponectin negatively correlates with alcoholic and non-alcoholic liver dysfunction: Health check-up study of Japanese men. Hepatol. Res. 2012, 43, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Sterling, R.K.; Lissen, E.; Clumeck, N.; Sola, R.; Correa, M.C.; Montaner, J.; Sulkowski, M.S.; Torriani, F.J.; Dieterich, D.T.; Thomas, D.L.; et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006, 43, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.G.; Lydecker, A.; Murray, K.; Tetri, B.N.; Contos, M.J.; Sanyal, A.J. NASH Clinical Research Network Comparison of Noninvasive Markers of Fibrosis in Patients with Nonalcoholic Fatty Liver Disease. Clin. Gastroenterol. Hepatol. 2009, 7, 1104–1112. [Google Scholar] [CrossRef]
- Kamada, Y.; Miyoshi, E. Mac-2 binding protein is a useful liver fibrosis biomarker for NAFLD/NASH. Trends Glycosci. Glycotechnol. 2019, 29, E85–E92. [Google Scholar] [CrossRef]
- Yoneda, M.; Fujii, H.; Sumida, Y.; Hyogo, H.; Itoh, Y.; Ono, M.; Eguchi, Y.; Suzuki, Y.; Aoki, N.; Kanemasa, K.; et al. Platelet count for predicting fibrosis in nonalcoholic fatty liver disease. J. Gastroenterol. 2011, 46, 1300–1306. [Google Scholar] [CrossRef]
- Sumida, Y.; Yoneda, M.; Hyogo, H.; Itoh, Y.; Ono, M.; Fujii, H.; Eguchi, Y.; Suzuki, Y.; Aoki, N.; Kanemasa, K.; et al. Validation of the FIB4 index in a Japanese nonalcoholic fatty liver disease population. BMC Gastroenterol. 2012, 12, 2. [Google Scholar] [CrossRef]
- Cheung, A.; Figueredo, C.; Rinella, M.E. Nonalcoholic Fatty Liver Disease. Am. J. Gastroenterol. 2019, 114, 579–590. [Google Scholar] [CrossRef]
- Srivastava, A.; Gailer, R.; Tanwar, S.; Trembling, P.; Parkes, J.; Rodger, A.; Suri, D.; Thorburn, U.; Sennett, K.; Morgan, S.; et al. Prospective evaluation of a primary care referral pathway for patients with non-alcoholic fatty liver disease. J. Hepatol. 2019, 71, 371–378. [Google Scholar] [CrossRef]
- Iwata, A.; Kamada, Y.; Ebisutani, Y.; Yamamoto, A.; Ueda, Y.; Arai, H.; Fujii, H.; Takamatsu, S.; Maruyama, N.; Maeda, M.; et al. Establishment of mouse Mac-2 binding protein enzyme-linked immunosorbent assay and its application for mouse chronic liver disease models. Hepatol. Res. 2016, 47, 902–909. [Google Scholar] [CrossRef] [PubMed]
- Resnick, D.; Pearson, A.; Krieger, M. The SRCR superfamily: A family reminiscent of the Ig superfamily. Trends Biochem. Sci. 1994, 19, 5–8. [Google Scholar] [CrossRef]
- Trahey, M.; Weissman, I.L. Cyclophilin C-associated protein: A normal secreted glycoprotein that down-modulates endotoxin and proinflammatory responses in vivo. Proc. Natl. Acad. Sci. USA 1999, 96, 3006–3011. [Google Scholar] [CrossRef] [PubMed]
- Umemura, T.; Joshita, S.; Sekiguchi, T.; Usami, Y.; Shibata, S.; Kimura, T.; Komatsu, M.; Matsumoto, A.; Ota, M.; Tanaka, E. Serum Wisteria floribunda Agglutinin-Positive Mac-2-Binding Protein Level Predicts Liver Fibrosis and Prognosis in Primary Biliary Cirrhosis. Am. J. Gastroenterol. 2015, 110, 857–864. [Google Scholar] [CrossRef] [PubMed]
| Variable | Baseline Parameters | Follow-Up Parameters after 7 Years | ||||
|---|---|---|---|---|---|---|
| Fatty Liver (−) | Fatty Liver (+) | p Value * | Fatty Liver (–) | Fatty Liver (+) | p Value * | |
| Number of study subjects | 273 | 442 | 292 | 423 | <0.0001 # | |
| Age (years) | 54.0 ± 8.3 | 53.5 ± 6.8 | N.S. | 61.4 ± 8.7 | 59.8 ± 6.3 | <0.05 |
| Gender (M/F) | 155/118 | 366/76 | <0.0001 | 175/117 | 346/77 | <0.0001 |
| BMI (kg/m2) | 22.0 ± 2.7 | 26.3 ± 3.8 | <0.0005 | 21.9 ± 2.8 | 26.0 ± 3.8 | <0.0001 |
| Alcohol consumption (g/week) | 86.6 ± 112.6 | 109.3 ± 128.5 | N.S. | 91.0 ± 123.5 | 114.1 ± 132.2 | <0.05 |
| SBP (mm Hg) | 110.4 ± 14.3 | 120.0 ± 15.4 | <0.0001 | 106.8 ± 15.8 | 114.2 ± 14.2 | <0.0001 |
| AST (U/L) | 24.3 ± 13.1 | 32.1 ± 15.4 | <0.0001 | 23.2 ± 10.2 | 30.4 ± 18.3 | <0.0001 |
| ALT (U/L) | 23.4 ± 17.4 | 43.8 ± 24.8 | <0.01 | 19.5 ± 10.0 | 35.7 ± 23.4 | <0.0001 |
| GGT (U/L) | 50.8 ± 85.2 | 74.0 ± 78.7 | <0.0001 | 42.3 ± 62.3 | 62.8 ± 66.5 | <0.0001 |
| T-Bil (mg/dL) | 0.79 ± 0.32 | 0.80 ± 0.30 | N.S. | 0.80 ± 0.30 | 0.86 ± 0.34 | <0.05 |
| Albumin (g/dL) | 4.23 ± 0.24 | 4.40 ± 0.22 | <0.0001 | 4.33 ± 0.23 | 4.46 ± 0.23 | <0.0001 |
| Creatinine (mg/dL) | 0.78 ± 0.16 | 0.83 ± 0.16 | <0.0001 | 0.80 ± 0.18 | 0.87 ± 0.30 | <0.0001 |
| CHE (U/L) | 314.7±62.0 | 378.7 ± 67.5 | <0.0001 | 315.1 ± 63.9 | 358.9 ± 65.5 | <0.0001 |
| TG (mg/dL) | 92.0 ± 83.3 | 157.7 ± 108.3 | <0.0001 | 89.6 ± 50.4 | 143.5 ± 115.2 | <0.0001 |
| T-Chol (mg/dL) | 199.1 ± 34.6 | 208.4 ± 34.0 | <0.0001 | 202.1 ± 35.6 | 197.9 ± 33.3 | N.S. |
| HDL-C (mg/dL) | 65.5 ± 13.9 | 53.8 ± 10.7 | <0.0001 | 67.9 ± 15.3 | 56.5 ± 12.3 | <0.0001 |
| LDL-C (mg/dL) | 120.8 ± 33.0 | 138.7 ± 30.5 | <0.0001 | 121.4 ± 30.7 | 125.7 ± 29.1 | <0.05 |
| Uric Acid (mg/dL) | 5.30 ± 1.35 | 6.13 ± 1.32 | <0.0001 | 5.27 ± 1.32 | 5.89 ± 1.26 | <0.0001 |
| FBG (mg/dL) | 108.0 ± 27.9 | 120.4 ± 32.6 | <0.0001 | 107.9 ± 22.7 | 120.7 ± 26.9 | <0.0001 |
| HbA1c (%) | 6.09 ± 0.99 | 6.49 ± 1.08 | <0.0001 | 6.14 ± 0.82 | 6.52 ± 0.99 | <0.0001 |
| Iron (µg/dL) | 111.1 ± 38.2 | 117.1 ± 37.8 | N.S. | 112.8 ± 38.3 | 121.0 ± 38.3 | <0.005 |
| Platelet count (×104/μL) | 21.4 ± 4.9 | 21.8 ± 5.0 | N.S. | 21.3 ± 5.3 | 21.0 ± 4.9 | N.S. |
| FIB4-index | 1.39 ± 0.6 | 1.30 ± 0.61 | <0.05 | 1.67 ± 0.82 | 1.61±1.03 | <0.05 |
| NFS | −1.32 ± 1.04 | −1.31 ± 1.07 | N.S. | −1.23 ± 1.17 | −1.02 ± 1.13 | <0.05 |
| M2BP (μg/mL) | 1.06 ± 0.61 | 1.85 ± 1.34 | <0.0001 | 1.12 ± 0.95 | 1.61 ±1.30 | <0.0001 |
| Variable | M2BP | |
|---|---|---|
| r | p Value | |
| Age (years old) | 0.023 | N.S. |
| BMI (kg/m2) | 0.374 | <0.0001 |
| Alcohol consumption (g/week) | 0.018 | N.S. |
| SBP (mm Hg) | 0.233 | <0.0001 |
| AST (U/L) | 0.328 | <0.0001 |
| ALT (U/L) | 0.351 | <0.0001 |
| GGT (U/L) | 0.279 | <0.0001 |
| T-Bil (mg/dL) | −0.105 | <0.01 |
| Albumin (mg/dL) | 0.085 | <0.05 |
| Creatinine (mg/dL) | −0.045 | N.S. |
| CHE (U/L) | 0.303 | <0.0001 |
| TG (mg/dL) | 0.326 | <0.0001 |
| T-Chol (mg/dL) | 0.113 | <0.005 |
| HDL-C (mg/dL) | −0.191 | <0.0001 |
| LDL-C (mg/dL) | 0.132 | <0.0005 |
| Uric acid (mg/dL) | 0.115 | <0.005 |
| FBG (mg/dL) | 0.099 | <0.05 |
| HbA1c (%) | 0.119 | <0.005 |
| Iron (μg/dL) | −0.002 | N.S. |
| Platelet count (×104/μL) | 0.043 | N.S. |
| FIB4-index | 0.061 | N.S. |
| NFS | 0.058 | N.S. |
| (A) | ||||
|---|---|---|---|---|
| Disease | Positive | Negative | pValue | |
| Obesity | 1.88 ± 1.38 | 1.29 ± 0.92 | <0.0001 | |
| Hypertension | 1.80 ± 1.10 | 1.41 ± 1.20 | <0.0001 | |
| Dyslipidemia | 1.77 ± 1.11 | 1.40 ± 1.20 | <0.0001 | |
| Diabetes mellitus | 1.62 ± 1.30 | 1.43 ± 0.95 | <0.05 | |
| Fatty liver | 1.85 ± 1.34 | 1.06 ± 0.61 | <0.0001 | |
| (B) | ||||
| Factor | tValue | pValue | 95% CI | |
| Lower | Upper | |||
| Obesity (y = 1, n = 2) | 3 | <0.005 | 0.0496 | 0.237 |
| Hypertension (y = 1, n = 2) | 1.64 | N.S. | −0.0150 | 0.168 |
| Dyslipidemia (y = 1, n = 2) | 0.4 | N.S. | −0.0732 | 0.110 |
| Diabetes mellitus (y = 1, n = 2) | 0.95 | N.S. | −0.0444 | 0.127 |
| Fatty liver (y = 1, n = 2) | 5.83 | <0.0001 | 0.197 | 0.396 |
| M2BP | ||
|---|---|---|
| Variable | r | p Value |
| ΔBMI (kg/m2) | −0.094 | <0.05 |
| Δalcohol consumption (g/week) | 0.031 | N.S. |
| ΔSBP (mm Hg) | −0.087 | <0.05 |
| ΔAST (U/L) | 0.012 | N.S. |
| ΔALT (U/L) | −0.069 | N.S. |
| ΔGGT (U/L) | −0.032 | N.S. |
| ΔT-Bil (mg/dL) | 0.111 | N.S. |
| ΔAlbumin (mg/dL) | −0.042 | N.S. |
| ΔCreatinine (mg/dL) | 0.013 | N.S. |
| ΔCHE (U/L) | −0.196 | <0.0001 |
| ΔTG (mg/dL) | −0.157 | N.S. |
| ΔT-Chol (mg/dL) | −0.187 | <0.05 |
| ΔHDL-C (mg/dL) | 0.001 | N.S. |
| ΔLDL-C (mg/dL) | −0.152 | <0.001 |
| ΔUric acid (mg/dL) | −0.080 | N.S. |
| ΔFBG (mg/dL) | 0.039 | N.S. |
| ΔHbA1c (%) | −0.0056 | N.S. |
| ΔIron (μg/dL) | 0 | N.S. |
| ΔPlatelet count (×104/μL) | −0.19 | <0.05 |
| ΔFIB4-index | 0.2 | <0.0001 |
| ΔNFS | 0.18 | <0.0001 |
| FIB4-Index | NFS | M2BP | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 1.30 (n = 424) | 1.30 < (n = 291) | < −1.455 (n = 303) | −1.455 < (n = 379) | <1.80 μg/Ml (n = 510) | 1.80 μg/mL < (n = 205) | |||||||
| r | p Value | R | p Value | r | p Value | r | p Value | r | p Value | r | p Value | |
| ΔFIB4-index | 0.048 | N.S. | 0.096 | N.S. | 0.099 | N.S. | 0.16 | <0.005 | 0.111 | <0.05 | 0.309 | <0.0001 |
| (A) | ||||
|---|---|---|---|---|
| Variable | t Value | p Value | 95% CI | |
| Lower | Upper | |||
| Gender (F) | 0.93 | N.S. | −0.232 | 0.645 |
| Age | −1.48 | N.S. | −0.06942 | 0.00980 |
| BMI (kg/m2) | −2.01 | <0.05 | −0.170 | −0.0018 |
| Alcohol consumption (g/week) | −1.24 | N.S. | −0.0042 | 0.000948 |
| SBP (mm Hg) | −0.34 | N.S. | −0.0227 | 0.0160 |
| ALT (U/L) | −0.71 | N.S. | −0.0195 | 0.00918 |
| GGT (U/L) | −0.72 | N.S. | −0.00553 | 0.00258 |
| T-Bil (mg/dL) | 0.57 | N.S. | −0.703 | 1.28 |
| Albumin (mg/dL) | −0.99 | N.S. | −1.83 | 0.605 |
| Creatinine (mg/dL) | 1.5 | N.S. | −0.546 | 4.05 |
| CHE (U/L) | −0.43 | N.S. | −0.00569 | 0.00365 |
| TG (mg/dL) | 2.94 | <0.005 | 0.00151 | 0.00756 |
| T-Chol (mg/dL) | −1.61 | N.S. | −0.0155 | 0.00154 |
| Uric acid (mg/dL) | −0.56 | N.S. | −0.322 | 0.179 |
| Iron (μg/dL) | 2.39 | <0.05 | 0.00171 | 0.0176 |
| FBG (mg/dL) | 1.86 | N.S. | −0.00091 | 0.0327 |
| HbA1c (%) | −0.93 | N.S. | −0.751 | 0.269 |
| M2BP (µg/mL) | −2.93 | <0.005 | −0.628 | −0.124 |
| (B) | ||||
| Variable | tValue | pValue | 95% CI | |
| Lower | Upper | |||
| Gender (F) | −1.75 | N.S. | −0.151 | 0.00889 |
| Age | 1.98 | N.S. | 5.51 × 10−5 | 0.0145 |
| BMI (kg/m2) | 0.75 | N.S. | −0.00954 | 0.0213 |
| Alcohol consumption (g/week) | 0.62 | N.S. | −0.00032 | 0.000619 |
| SBP (mm Hg) | −0.86 | N.S. | −0.00509 | 0.00200 |
| ALT (U/L) | −1.43 | N.S. | −0.00454 | 0.00071 |
| GGT (U/L) | 1.19 | N.S. | −0.00029 | 0.00119 |
| T-Bil (mg/dL) | 1.12 | N.S. | −0.0776 | 0.286 |
| Albumin (mg/dL) | −0.92 | N.S. | −0.326 | 0.119 |
| Creatinine (mg/dL) | −1.35 | N.S. | −0.709 | 0.132 |
| CHE (U/L) | −1.23 | N.S. | −0.00139 | 0.00032 |
| TG (mg/dL) | −3.46 | <0.001 | −0.00153 | −0.00042 |
| T-Chol (mg/dL) | −0.62 | N.S. | −0.00205 | 0.00107 |
| Uric acid (mg/dL) | 0.97 | N.S. | −0.0232 | 0.0685 |
| Iron (μg/dL) | −1.07 | N.S. | −0.00224 | 0.000661 |
| FBG (mg/dL) | 0.25 | N.S. | −0.00269 | 0.00346 |
| HbA1c (%) | 0.03 | N.S. | −0.0921 | 0.0944 |
| M2BP (µg/mL) | 11.89 | <0.0001 | 0.233 | 0.325 |
| (A) | ||||
|---|---|---|---|---|
| Variable | ΔM2BP | |||
| r | p Value | |||
| ΔBMI (kg/m2) | 0.136 | <0.001 | ||
| Δalcohol consumption (g/week) | 0.082 | <0.05 | ||
| ΔSBP (mm Hg) | 0.114 | <0.005 | ||
| ΔAST (U/L) | 0.118 | <0.005 | ||
| ΔALT (U/L) | 0.089 | <0.05 | ||
| ΔGGT (U/L) | 0.153 | <0.0005 | ||
| ΔAlbumin (mg/dL) | 0.01 | N.S. | ||
| ΔCHE (U/L) | 0.183 | <0.001 | ||
| ΔTG (mg/dL) | 0.1 | <0.05 | ||
| ΔT-Chol (mg/dL) | 0.133 | <0.0005 | ||
| ΔHDL-C (mg/dL) | −0.11 | <0.01 | ||
| ΔLDL-C (mg/dL) | 0.135 | <0.001 | ||
| ΔUric acid (mg/dL) | −0.016 | N.S. | ||
| ΔCreatinine (mg/dL) | −0.014 | N.S. | ||
| ΔFBG (mg/dL) | 0.14 | <0.001 | ||
| ΔHbA1c (%) | 0.177 | <0.001 | ||
| ΔIron (μg/dL) | −0.046 | N.S. | ||
| ΔPlatelet count (×104/μL) | −0.046 | N.S. | ||
| ΔFIB4-index | −0.051 | N.S. | ||
| ΔNFS | −0.039 | N.S. | ||
| (B) | ||||
| Variable | tValue | pValue | 95% CI | |
| Lower | Upper | |||
| ΔBMI (kg/m2) | 1.04 | N.S. | −0.0290 | 0.0942 |
| Δalcohol consumption (g/week) | 0.47 | N.S. | −8.89 × 10−4 | 0.00146 |
| ΔSBP (mm Hg) | 2.32 | <0.05 | 0.00105 | 0.0126 |
| ΔALT (U/L) | −0.43 | N.S. | −0.005323 | 0.00342 |
| ΔGGT (U/L) | 2.69 | <0.01 | 0.000603 | 0.00386 |
| ΔAlbumin (mg/dL) | 0.47 | N.S. | −0.345 | 0.562 |
| ΔCHE (U/L) | 2.27 | <0.05 | 0.000371 | 0.00516 |
| ΔTG (mg/dL) | 0.18 | N.S. | −0.00101 | 0.00122 |
| ΔT-Chol (mg/dL) | 1.31 | N.S. | −0.000987 | 0.00494 |
| ΔUric acid (mg/dL) | −1.27 | N.S. | −0.147 | 0.0315 |
| ΔCreatinine (mg/dL) | 1.36 | N.S. | −0.132 | 0.725 |
| ΔFBG (mg/dL) | −0.07 | N.S. | −0.00489 | 0.00453 |
| ΔHbA1c (%) | 2.37 | <0.05 | 0.0314 | 0.335 |
| ΔIron (μg/dL) | −1.94 | N.S. | −0.00382 | 2.63 × 10−5 |
| ΔPlatelet count (×104/μL) | 0.78 | N.S. | −0.0156 | 0.0360 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamada, Y.; Morishita, K.; Koseki, M.; Nishida, M.; Asuka, T.; Naito, Y.; Yamada, M.; Takamatsu, S.; Sakata, Y.; Takehara, T.; et al. Serum Mac-2 Binding Protein Levels Associate with Metabolic Parameters and Predict Liver Fibrosis Progression in Subjects with Fatty Liver Disease: A 7-Year Longitudinal Study. Nutrients 2020, 12, 1770. https://doi.org/10.3390/nu12061770
Kamada Y, Morishita K, Koseki M, Nishida M, Asuka T, Naito Y, Yamada M, Takamatsu S, Sakata Y, Takehara T, et al. Serum Mac-2 Binding Protein Levels Associate with Metabolic Parameters and Predict Liver Fibrosis Progression in Subjects with Fatty Liver Disease: A 7-Year Longitudinal Study. Nutrients. 2020; 12(6):1770. https://doi.org/10.3390/nu12061770
Chicago/Turabian StyleKamada, Yoshihiro, Koichi Morishita, Masahiro Koseki, Mayu Nishida, Tatsuya Asuka, Yukiko Naito, Makoto Yamada, Shinji Takamatsu, Yasushi Sakata, Tetsuo Takehara, and et al. 2020. "Serum Mac-2 Binding Protein Levels Associate with Metabolic Parameters and Predict Liver Fibrosis Progression in Subjects with Fatty Liver Disease: A 7-Year Longitudinal Study" Nutrients 12, no. 6: 1770. https://doi.org/10.3390/nu12061770
APA StyleKamada, Y., Morishita, K., Koseki, M., Nishida, M., Asuka, T., Naito, Y., Yamada, M., Takamatsu, S., Sakata, Y., Takehara, T., & Miyoshi, E. (2020). Serum Mac-2 Binding Protein Levels Associate with Metabolic Parameters and Predict Liver Fibrosis Progression in Subjects with Fatty Liver Disease: A 7-Year Longitudinal Study. Nutrients, 12(6), 1770. https://doi.org/10.3390/nu12061770








