Reference Values of Thyroid Hormones During the First Trimester of Pregnancy in Valencian Community (Spain) and Their Relationship with Iodine Intake
Abstract
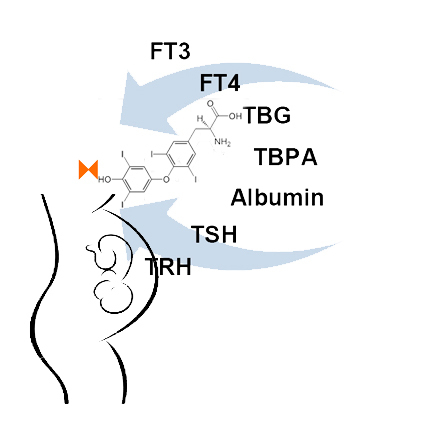
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Variables
2.3. Laboratory Methods
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Velasco, I.; Sánchez-Gila, M.; Manzanares, S.; Taylor, P.; García-Fuentes, E. Iodine Status, Thyroid Function, and Birthweight: A Complex Relationship in High-Risk Pregnancies. J. Clin. Med. 2020, 9, 177. [Google Scholar] [CrossRef]
- Vila, L.; Velasco, I.; González, S.; Morales, F.; Sánchez, E.; Lailla, J.M.; Txanton, M.-A.; Manel, P.-D. Detección de la disfunción tiroidea en la población gestante: Está justificado el cribado universal. Conferencia de consenso. Med. Clin. 2012, 139, 509.e1–509.e11. [Google Scholar] [CrossRef] [PubMed]
- Alexander, E.K.; Pearce, E.N.; Brent, G.A.; Brown, R.S.; Chen, H.; Dosiou, C.; Grobman, W.A.; Laurberg, P.; Lazarus, J.H.; Mandel, S.J.; et al. Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 2017, 27, 315–389. [Google Scholar] [CrossRef] [PubMed]
- Capel, I.; Corcoy Pla, R. Enfermedades Tiroideas y Gestación. In Obstetricia y Medicina Materno-Fetal; Cabrero, L., Saldivar, D., Cabrillo, E., Eds.; Panamericana: Buenos Aires-Madrid, Spain, 2010; pp. 867–874. [Google Scholar]
- Endocrine Society; American Association Clinical Endocrinologists; Asia & Oceania Thyroid Association; American Thyroid Association; European Thyroid Association; Latin American Thyroid Association. Management of thyroid dysfunction during pregnancy and postpartum: An Endocrine Society Clinical Practice Guideline. Thyroid 2007, 17, 1159–1167. [Google Scholar]
- Bocos-Terraz, J.; Izquierdo-Álvarez, S.; Banzalero-Flores, J.; Álvarez-Lahuerta, R.; Aznar-Sauca, A.; Real-López, E.; Ibáñez-Marco, R.; Bocanegra-García, V.; Rivera-Sánchez, G. Thyroid hormones according to gestational age in pregnant Spanish women. BMC Res. Notes. 2009, 26, 237. [Google Scholar] [CrossRef]
- Vila, L.; Serra-Prat, M.; Palomera, E.; Casamitjana, R.; De Castro, A.; Legaz, G.; Barrionuevo, C.; Garcia, A.-J.; Lal-Trehan, S.; Muñoz, J.A.; et al. Reference values for thyroid function tests in pregnant women living in Catalonia, Spain. Thyroid 2010, 20, 221–225. [Google Scholar] [CrossRef]
- García de Guadiana, L.; González Morales, M.; Martín-Ondarza González, M.C.; Martín García, E.; Martínez Uriarte, J.; Blázquez Abellán, A.; Nuevo-García, J. Valoración de la función tiroidea durante la gestación: Intervalos de referencia de tirotropina y tiroxina no unida a proteína durante el primer trimestre. Endocrinol Nutr. 2010, 57, 290–295. [Google Scholar] [CrossRef]
- Santiago, P.; Berrio, M.; Olmedo, P.; Velasco, I.; Sánchez, B.; García, E.; Martínez, J.; Soriguer, F. Reference values for thyroid hormones in the population of pregnant women in Jaen (Spain). Endocrinol Nutr. 2011, 58, 62–67. [Google Scholar] [CrossRef]
- Aller Granda, J.; Rabal Artal, A. Valores de referencia de tirotropina en el primer trimestre del embarazo. Endocrinol Nutr. 2013, 60, 405–406. [Google Scholar] [CrossRef]
- Grifol, M.L.; Gutierrez Menendez, M.L.; García Menéndez, L.; Valdazo Revenga, M.V. Valores de referencia y estudio de la variabilidad de hormonas tiroideas en gestantes de El Bierzo. Endocrinol Nutr. 2013, 60, 549–554. [Google Scholar] [CrossRef]
- Santiago Fernández, P.; González-Romero, S.; Martín Hernández, T.; Navarro González, E.; Velasco López, I.; Millón Ramírez, M.C. Abordaje del manejo de la disfunción tiroidea en la gestación. Documento de consenso de la Sociedad Andaluza de Endocrinología y Nutrición (SAEN). Semergen–Med. de. fam. 2015, 41, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Pombar-Pérez, M.; Penín-Álvarez, M.; Vélez-Castillo, M.; Trigo-Barros, C.; Álvarez-García, E.; Rodríguez-Ferro, R. Impacto de la aplicación de los criterios de la Asociación Americana de tiroides en el diagnóstico de hipotiroidismo en gestantes de Vigo, España. Rev. Peru. Med. Exp. Salud. Pública. 2013, 30, 428–431. [Google Scholar]
- Diaz-Cadórniga, F.J.; Delgado-Álvarez, E. Déficit de Yodo en España. Endocrinol Nutr. 2004, 51, 2–13. [Google Scholar] [CrossRef]
- Fundación Española de Dietistas y Nutricionistas. Revisión Científica sobre la alimentación en la mujer embarazada. Evidencia Científica. Pamplona: Centro de Análisis de Evidencia Científica (CAEC-FEDN), Consejo General de Dietistas-Nutricionistas: Author. 2014. Available online: http://www.fedn.es/docs/alimentacionyembarazoFEDN.pdf (accessed on 16 March 2020).
- Wu, T.; Liu, G.J.; Li, P.; Clar, C. Iodized salt for preventing iodine deficiency disorders. CDSR 2002. No.: CD003204. [Google Scholar] [CrossRef]
- De Luís, D.A.; Aller, R.; Izaola, O. Problemática de la deficiencia de yodo durante la gestación. Ann. Med. Interna. 2005, 22, 445–448. [Google Scholar]
- Suárez Rodríguez, M.; Azcona San Julián, C.; Alzina de Aguilar, V. Ingesta de yodo durante el embarazo: Efectos en la función tiroidea materna y neonatal. Endocrinol. Nutr. 2013, 60, 352–357. [Google Scholar] [CrossRef]
- Soriguer, F.; García-Fuentes, E.; Gutiérrez-Repiso, C.; Rojo-Martínez, G.; Velasco, I.; Goday, A. Iodine intake in the adult population. Di@bet.es study. Clin. Nutr. 2012, 31, 882–888. [Google Scholar] [CrossRef]
- Dunn, J.T.; Crutchfield, H.E.; Gutekunst, R.; Dunn, A.D. Two simple methods for measuring iodine in urine. Thyroid 1993, 3, 119–123. [Google Scholar] [CrossRef]
- Reed, A.H.; Henry, R.J.; Mason, W.B. Influence of statistical method used on the resulting estimate of normal range. Clin. Chem. 1971, 17, 275–284. [Google Scholar] [CrossRef]
- Karakosta, P.; Chatzi, L.; Bagkeris, E.; Daraki, V.; Alegakis, D.; Castanas, E.; Manolis, K.; Marilena, K. First and second-trimester reference intervals for thyroid hormones during pregnancy in "Rhea" Mother-Child Cohort, Crete, Greece. J. Thyroid Res 2011, 490783. [Google Scholar] [CrossRef]
- Lazarus, J.H.; Bestwick, J.P.; Channon, S.; Paradice, R.; Maina, A.; Rees, R.; Chiusano, E.; John, R.; Guaraldo, V.; George, L.M. Antenatal thyroid screening and childhood cognitive function. N. Engl. J. Med. 2012, 366, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Amouzegar, A.; Khazan, M.; Hedayati, M.; Azizi, F. An assessment of the iodine status and the correlation between iodine nutrition and thyroid function during pregnancy in an iodine sufficient area. Eur. J. Clin. Nutr. 2014, 68, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Soldin, O.P. Thyroid function in pregnancy and thyroid disease: Trimester-specific reference intervals. Therap. Drug. Monit. 2006, 28, 8–11. [Google Scholar] [CrossRef] [PubMed]
- International Council For Control of Iodine Deficiency Disorders-ICCIDD. Iodine requirements in pregnancy and infancy. IDD Newsletter. 2007, 23. [Google Scholar]
- Saravanan, P.; Dayan, C.M. Thyroid autoantibodies. Endocrinol. Metab. Clin. North Am. 2001, 30, 315–337. [Google Scholar] [CrossRef]
- Plouvier, E.; Alliot, L.; Bigorie, B.; Kowalski, C.; Medeau, V.; Thuillier, F. De la nécessité de bien définir les valeurs de référence des hormones thyroïdiennes pour une meilleure interprétation clinique. Ann. Biol. Clin. 2011, 69, 77–83. [Google Scholar] [CrossRef]
- Donnay, S.; Arena, J.; Lucas, A. Suplementación con yodo durante el embarazo y la lactancia. Toma de posición del Grupo de Trabajo de Trastornos relacionados con la Deficiencia de Yodo y Disfunción Tiroidea de la Sociedad Española de Endocrinología y Nutrición. Endocrinol. Nutr. 2014, 61, 27–34. [Google Scholar] [CrossRef]
- Harding, K.B.; Peña-Rosas, J.P.; Webster, A.C.; Yap, C.M.; Payne, B.A.; Ota, E.; De-Regil, L.M. Iodine supplementation for women during the preconception, pregnancy and postpartum period. Cochrane Database Syst. Rev. 2017, 3, CD011761. [Google Scholar] [CrossRef]
- Arrizabalaga, J.J.; Jalón, M.; Espada, M.; Cañas, M.; Latorre, P.M. Concentración de yodo en la leche ultrapasteurizada de vaca. Aplicaciones en la práctica clínica y en la nutrición comunitaria. Med. Clin. 2015, 145, 55–61. [Google Scholar] [CrossRef]
- Monckeberg, F. La sal es indispensable para la vida, pero cuánta? Rev. Chil. Nutr. 2012, 39, 192–195. [Google Scholar]
- Bechtler, G.; Haeckel, R.; Horder, M.; Küffer, H.; Porth, A.J. Guidelines (1987) for Classification, Calculation and Validation of Conversion Rates in Clinical Chemistry. Clinical Chemistry and Laboratory Medicine 1987, 25, 315–342. [Google Scholar] [CrossRef]

| Area in Spain | TSH (mIU/L) P2.5 to P97.5+ | n^ | Method |
|---|---|---|---|
| Aragón (Center) (Bocos-Terraz J et al., 2009 [6]) | 0.41–2.63 (WG ** 14) | 330 | Chemiluminescence immunoassay Abbott Diagnostics |
| Cataluña (Northeast) (Vila L et al., 2010 [7]) | 0.12–4.5 (WG 9) | 178 | Chemiluminescence immunoassay Advia Centaur Bayer |
| Cartagena (Southeast) (García de Guadiana L et al., 2010 [8]) | 0.047–3.466 (WG 11) 0.13–3.706 (WG 12) | 117 151 | Chemiluminescence immunoassay Roche Diagnostics |
| Jaén (Southeast) (Santiago P et al., 2011 [9]) | 0.23–4.18 (WG 7–10) | 279 | Chemiluminescence immunoassay Beckman Access |
| Oviedo, Asturias (North) (Aller Granda et al, 2013 [10]) | 0.17–4.15 (WG 6–12) | 264 | Chemiluminescence immunoassay Roche Diagnostic |
| El Bierzo (North) (Grifol ML et al., 2013 [11]) | 0.497–3.595 (WG < 12) | 412 | Chemiluminescence immunoassay ADVIA Centaur XP |
| Sevilla (Southwest) (Santiago P et al., 2015 [12]) | 0.36–4.49 (WG NI *) | NI * | Electrochemiluminescence immunoassay |
| Vigo (Northwest) (Pombar-Pérez et al., 2013 [13]) | 0.33–4.59 (WG < 12) | 2410 | Electrochemiluminescent immunometric analysis |
| . | Mean ± SD or n (%) | p-Value |
|---|---|---|
| Maternal age (years) | 30.8 ± 5.1 | |
| BMI first trimester (kg/m2) | 23.9 ± 4.4 | |
| Milk consumption | ||
| No | 36 (13.8%) | <0.001 * |
| Yes | 225 (86.21%) | |
| Use of iodine supplements | ||
| No | 77 (29.5%) | <0.001 * |
| Yes | 184 (70.5%) | |
| Use of iodized salt | ||
| No | 133 (51%) | 0.757 * |
| Yes | 128 (49%) | |
| Use of table salt | ||
| No | 166 (63.6%) | <0.001 * |
| Yes | 95 (36.4%) | |
| Use of sea salt | ||
| No | 210 (80.5%) | <0.001 * |
| Yes | 51 (19.5%) | |
| Smoking | ||
| No | 152 (58.24%) | 0.008 * |
| Yes | 109 (41.76%) |
| All | YES | NO | p-Value | |
|---|---|---|---|---|
| TSH (mIU/L) | 1.90 ± 1.05 | |||
| Milk consumption | 1.92 ± 1.03 | 1.75 ± 1.13 | 0.39 * | |
| Iodine supplements | 1.94 ± 1.05 | 1.78 ± 1.05 | 0.25 * | |
| Use of iodized salt | 1.98 ± 1.06 | 1.81 ± 1.03 | 0.21 * | |
| Use of table salt | 1.64 ± 0.82 | 2.04 ± 1.13 | 0.003 * | |
| Use of sea salt | 2.03 ± 1.18 | 1.86 ± 1.01 | 0.29 * | |
| Smoking | 1.51 ± 0.72 | 2.06 ± 1.13 | 0.05 * | |
| FT4 (ng/dL) | 1.19 ± 0.20 | |||
| Milk consumption | 1.19 ± 0.20 | 1.19 ± 0.16 | 0.95 * | |
| Iodine supplements | 1.19 ± 0.21 | 1.19 ± 0.17 | 0.94 * | |
| Use of iodized salt | 1.19 ± 0.21 | 1.19 ± 0.18 | 0.96 * | |
| Use of table salt | 1.17 ± 0.18 | 1.20 ± 0.21 | 0.40 * | |
| Use of sea salt | 1.22 ± 0.25 | 1.19 ± 0.18 | 0.27 * | |
| Smoking | 1.11 ± 0.30 | 1.18 ± 0.25 | 0.14 * | |
| Ioduria (μg/L) | 57 (33.3–101.3) | |||
| Milk consumption | 58.2 (33.5–103.3) | 51.7 (30.2–98.4) | 0.68 ** | |
| Iodine supplements | 69.6 (44.9–109.9) | 37.2 (25.6–80.5) | <0.001 ** | |
| Use of iodized salt | 65.4 (37.6–100.6) | 50.7 (28.1–102.7) | 0.03 ** | |
| Use of table salt | 48.3 (26.7–103.6) | 61.1 (36.7–101.6) | 0.03 ** | |
| Use of sea salt | 51.6 (30.9–102.7) | 59.0 (33.8–100.6) | 0.36 ** | |
| Smoking | 63.0 (39.2–109.7) | 51.7 (29.1–100.6) | 0.37 ** |
| Confidence Interval 95% | Lower Value P2.5 | Upper Value P97.5 | Lower Limit P2.5 | Lower Limit P97.5 | Upper Limit P2.5 | Upper Limit P97.5 |
|---|---|---|---|---|---|---|
| General | ||||||
| TSH | 0.128 | 4.455 | 0.054 | 4.272 | 0.310 | 4.637 |
| FT4 | 0.9 | 1.56 | 0.87 | 1.528 | 0.935 | 1.592 |
| Use of iodized salt | ||||||
| TSH | ||||||
| No | 0.10 | 4.13 | 0.026 | 3.947 | 0.282 | 4.312 |
| Yes | 0.18 | 4.70 | 0.106 | 4.517 | 0.362 | 4.883 |
| FT4 | ||||||
| No | 0.90 | 1.60 | 0.87 | 1.57 | 0.93 | 1.63 |
| Yes | 0.90 | 1.58 | 0.87 | 1.55 | 0.93 | 1.61 |
| Smoking | ||||||
| TSH | ||||||
| No | 0.14 | 4.61 | 0.066 | 4.418 | 0.322 | 4.802 |
| Yes | 0.10 | 3.66 | 0.026 | 3.586 | 0.2822 | 3.842 |
| FT4 | ||||||
| No | 0.80 | 1.60 | 0.77 | 1.57 | 0.83 | 1.63 |
| Yes | 0.80 | 1.50 | 0.77 | 1.47 | 0.83 | 1.53 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murillo-Llorente, M.T.; Fajardo-Montañana, C.; Pérez-Bermejo, M. Reference Values of Thyroid Hormones During the First Trimester of Pregnancy in Valencian Community (Spain) and Their Relationship with Iodine Intake. Nutrients 2020, 12, 1433. https://doi.org/10.3390/nu12051433
Murillo-Llorente MT, Fajardo-Montañana C, Pérez-Bermejo M. Reference Values of Thyroid Hormones During the First Trimester of Pregnancy in Valencian Community (Spain) and Their Relationship with Iodine Intake. Nutrients. 2020; 12(5):1433. https://doi.org/10.3390/nu12051433
Chicago/Turabian StyleMurillo-Llorente, María Teresa, Carmen Fajardo-Montañana, and Marcelino Pérez-Bermejo. 2020. "Reference Values of Thyroid Hormones During the First Trimester of Pregnancy in Valencian Community (Spain) and Their Relationship with Iodine Intake" Nutrients 12, no. 5: 1433. https://doi.org/10.3390/nu12051433
APA StyleMurillo-Llorente, M. T., Fajardo-Montañana, C., & Pérez-Bermejo, M. (2020). Reference Values of Thyroid Hormones During the First Trimester of Pregnancy in Valencian Community (Spain) and Their Relationship with Iodine Intake. Nutrients, 12(5), 1433. https://doi.org/10.3390/nu12051433