The Mediating Effects of Eating Disorder, Food Addiction, and Insomnia in the Association between Psychological Distress and Being Overweight among Iranian Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Instruments
2.2.1. Measures at Baseline
2.2.2. Measures at One-Year Follow-Up
2.3. Data Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Wabitsch, M.; Moss, A.; Kromeyer-Hauschild, K. Unexpected plateauing of childhood obesity rates in developed countries. BMC Med. 2014, 12, 17. [Google Scholar] [CrossRef]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief 2017, 288, 1–8. [Google Scholar]
- Wang, J.J.; Gao, Y.; Lau, P.W.C. Prevalence of overweight in Hong Kong Chinese children: Its associations with family, early-life development and behaviors-related factors. J. Exerc. Sci. Fit 2017, 15, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Mottaghi, A.; Mirmiran, P.; Pourvali, K.; Tahmasbpour, Z.; Azizi, F. Incidence and prevalence of childhood obesity in Tehran, Iran in 2011. Iran. J. Public Health 2017, 46, 1395–1403. [Google Scholar] [PubMed]
- Kumar, S.; Kelly, A.S. Review of childhood obesity: From epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin. Proc. 2017, 92, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.Y.; Wang, S.-M.; Lam, Y.Y.; Luk, H.T.; Man, Y.C.; Lin, C.-Y. The relationships between weight bias, perceived weight stigma, eating behavior and psychological distress among undergraduate students in Hong Kong. J. Nerv. Ment. Dis. 2018, 206, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.; Suh, Y. Health consequences of weight stigma: Implications for obesity prevention and treatment. Curr. Obes. Rep. 2015, 4, 182–190. [Google Scholar] [CrossRef]
- Wong, P.C.; Hsieh, Y.P.; Ng, H.H.; Kong, S.F.; Chan, K.L.; Au, T.Y.A.; Lin, C.-Y. Investigating the self-stigma and quality of life for overweight/obese children in Hong Kong: A preliminary study. Child Indic. Res. 2018, 12, 1065–1082. [Google Scholar] [CrossRef]
- Lin, C.-Y. Comparing quality of life instruments: Sizing Them Up versus Pediatric Quality of Life and Kid-KINDL. Soc. Health Behav. 2018, 1, 42–47. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Su, C.-T.; Wang, J.-D.; Ma, H.-I. Self-rated and parent-rated quality of life (QoL) for community-based obese and overweight children. Acta Paediatr. 2013, 102, e114–e119. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-C.; Strong, C.; Tsai, M.-C.; Lin, C.-Y.; Fung, X.C.C. Validating Sizing Them Up: A parent-proxy weight-related quality-of-life measure, with community-based children. Int. J. Clin. Health Psychol. 2018, 18, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Pakpour, A.H.; Chen, C.-Y.; Lin, C.-Y.; Strong, C.; Tsai, M.-C.; Lin, Y.-C. The relationship between children’s overweight and quality of life: A comparison of Sizing Me Up, PedsQL, and Kid-KINDL. Int. J. Clin. Health Psychol. 2019, 19, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Strong, C.; Lin, Y.-C.; Tsai, M.-C.; Lin, C.-Y. Factor structure of Sizing Me Up, a self-reported weight-related quality of life instrument, in community children across weight status. Child Obes. 2017, 13, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Su, C.-T.; Wang, J.-D.; Lin, C.-Y. Child-rated versus parent-rated quality of life of community-based obese children across gender and grade. Health Qual. Life Outcomes 2013, 11, 206. [Google Scholar] [CrossRef] [PubMed]
- Tanofsky-Kraff, M.; Cohen, M.L.; Yanovski, S.Z.; Cox, C.; Theim, K.R.; Keil, M.; Reynolds, J.C.; Yanovski, J.A. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics 2006, 117, 1203–1209. [Google Scholar] [CrossRef] [PubMed]
- Tanofsky-Kraff, M.; Yanovski, S.Z.; Schvey, N.A.; Olsen, C.H.; Gustafson, J.; Yanovski, J.A. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. Int. J. Eat. Disord. 2009, 42, 26–30. [Google Scholar] [CrossRef]
- Goldschmidt, A.B.; Wall, M.M.; Zhang, J.; Loth, K.A.; Neumark-Sztainer, D. Overeating and binge eating in emerging adulthood: 10-year stability and risk factors. Dev. Psychol. 2016, 52, 475–483. [Google Scholar] [CrossRef]
- Avena, N.M.; Hoebel, B.G. A diet promoting sugar dependency causes behavioral cross-sensitization to a low dose of amphetamine. Neuroscience 2003, 122, 17–20. [Google Scholar] [CrossRef]
- Johnson, P.M.; Kenny, P.J. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nat. NeuroSci. 2010, 13, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Pursey, K.M.; Collins, C.E.; Stanwell, P.; Burrows, T.L. Foods and dietary profiles associated with ‘food addiction’ in young adults. Addict Behav. Rep. 2015, 2, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.; Skinner, J.; Joyner, M.A.; Palmieri, J.; Vaughan, K.; Gearhardt, A.N. Food addiction in children: Associations with obesity, parental food addiction and feeding practices. Eat. Behav. 2017, 26, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; Roberto, C.A.; Seamans, M.J.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the Yale Food Addiction Scale for Children. Eat. Behav. 2013, 14, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Gopnik, A.; O’Grady, S.; Lucas, C.G.; Griffiths, T.L.; Wente, A.; Bridgers, S.; Aboody, R.; Fung, H.; Dahl, R.E. Changes in cognitive flexibility and hypothesis search across human life history from childhood to adolescence to adulthood. Proc. Natl. Acad. Sci. USA 2017, 114, 7892–7899. [Google Scholar] [CrossRef]
- Barry, C.L.; Brescoll, V.L.; Brownell, K.D.; Schlesinger, M. Obesity metaphors: How beliefs about the causes of obesity affect support for public policy. Milbank Q. 2009, 87, 7–47. [Google Scholar] [CrossRef] [PubMed]
- Hargens, T.A.; Kaleth, A.S.; Edwards, E.S.; Butner, K.L. Association between sleep disorders, obesity, and exercise: A review. Nat. Sci. Sleep 2013, 5, 27–35. [Google Scholar] [CrossRef]
- Hsieh, S.D.; Muto, T.; Murase, T.; Tsuji, H.; Arase, Y. Association of short sleep duration with obesity, diabetes, fatty liver and behavioral factors in Japanese men. Intern Med. 2011, 50, 2499–2502. [Google Scholar] [CrossRef][Green Version]
- Liu, J.; Hay, J.; Joshi, D.; Faught, B.E.; Wade, T.; Cairney, J. Sleep difficulties and obesity among preadolescents. Can. J. Public Health 2011, 102, 139–143. [Google Scholar] [CrossRef]
- Al-Disi, D.; Al-Daghri, N.; Khanam, L.; Al-Othman, A.; Al-Saif, M.; Sabico, S.; Chrousos, G. Subjective sleep duration and quality influence diet composition and circulating adipocytokines and ghrelin levels in teen-age girls. Endocr. J. 2010, 57, 915–923. [Google Scholar] [CrossRef]
- Moreira, P.; Santos, S.; Padrão, P.; Cordeiro, T.; Bessa, M.; Valente, H.; Barros, R.; Teixeira, V.; Lopes, C.; Moreira, A. Food patterns according to sociodemographics, physical activity, sleeping and obesity in Portuguese children. Int. J. Environ. Res. Public Health 2010, 7, 1121–1138. [Google Scholar] [CrossRef]
- Seixas, A.A.; Nunes, J.V.; Airhihenbuwa, C.O.; Williams, N.J.; Pandi-Perumal, S.R.; James, C.C.; Jean-Louis, G. Linking emotional distress to unhealthy sleep duration: Analysis of the 2009 National Health Interview Survey. Neuropsychiatr Dis. Treat 2015, 11, 2425–2430. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.S.; Levsen, M.P.; McCrae, C.S. A meta-analysis of associations between obesity and insomnia diagnosis and symptoms. Sleep Med. Rev. 2018, 40, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.-C.; Hsieh, Y.-P.; Strong, C.; Lin, C.-Y. Effects of pubertal timing on alcohol and tobacco use in the early adulthood: A longitudinal cohort study in Taiwan. Res. Dev. Disabil. 2015, 36, 376–383. [Google Scholar] [CrossRef]
- Tsai, M.-C.; Strong, C.; Lin, C.-Y. Effects of pubertal timing on deviant behaviors in Taiwan: A longitudinal analysis of 7th- to 12th-grade adolescents. J. Adolesc. 2015, 42, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-Y.; Imani, V.; Broström, A.; Huus, K.; Björk, M.; Hodges, E.A.; Pakpour, A.H. Psychological distress and quality of life in Iranian adolescents with overweight/obesity: Mediating roles of weight bias internalization and insomnia. Eat. Weight Disord. 2019. [Google Scholar] [CrossRef] [PubMed]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Griffiths, M.D.; Su, J.-A.; Latner, J.D.; Marshall, R.D.; Pakpour, A.H. A prospective study on the link between weight-related self-stigma and binge eating: Role of food addiction and psychological distress. Int. J. Eat. Disord. 2020, 53, 442–450. [Google Scholar] [CrossRef]
- Mies, G.W.; Treur, J.L.; Larsen, J.K.; Halberstadt, J.; Pasman, J.A.; Vink, J.M. The prevalence of food addiction in a large sample of adolescents and its association with addictive substances. Appetite 2017, 118, 97–105. [Google Scholar] [CrossRef]
- World Health Organization. Growth Reference 5–19 Years|Application Tools|WHO AnthroPlus Software. 2016. Available online: https://www.who.int/growthref/en/ (accessed on 1 March 2020).
- Asghari, A.; Saed, F.; Dibajnia, P. Psychometric properties of the Depression Anxiety Stress Scales-21 (DASS-21) in a non-clinical Iranian sample. Int. J. Psychol. 2008, 2, 82–102. [Google Scholar]
- Lin, C.-Y.; Broström, A.; Nilsen, P.; Griffiths, M.D.; Pakpour, A.H. Psychometric validation of the Persian Bergen Social Media Addiction Scale using classic test theory and Rasch models. J. Behav. Addict. 2017, 6, 620–629. [Google Scholar] [CrossRef]
- Shaw, T.; Campbell, M.A.; Runions, K.C.; Zubrick, S.R. Properties of the DASS-21 in an Australian community adolescent population. J. Clin. Psychol. 2017, 73, 879–892. [Google Scholar] [CrossRef]
- Ahmadi, S.; Moloodi, R.; Zarbaksh, M.R.; Ghaderi, A. Psychometric properties of the Eating Attitude Test-26 for female Iranian students. Eat. Weight. Disord. 2014, 19, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Preliminary validation of the Yale Food Addiction Scale. Appetite 2009, 52, 430–436. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Magyar, É.E.; Tényi, D.; Gearhardt, A.; Jeges, S.; Abaligeti, G.; Tóth, Á.L.; Janszky, J.; Molnár, D.; Tényi, Y.; Csábi, G. Adaptation and validation of the Hungarian version of the Yale Food Addiction Scale for Children. J. Behav. Addict. 2018, 7, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef]
- Yazdi, Z.; Sadeghniiat-Haghighi, K.; Zohal, M.A.; Elmizadeh, K. Validity and reliability of the Iranian version of the Insomnia Severity Index. Malays J. Med. Sci. 2012, 19, 31–36. [Google Scholar]
- Chung, K.F.; Kan, K.K.; Yeung, W.F. Assessing insomnia in adolescents: Comparison of Insomnia Severity Index, Athens Insomnia Scale and Sleep Quality Index. Sleep Med. 2011, 12, 463–470. [Google Scholar] [CrossRef]
- Muthuri, S.K.; Onywera, V.O.; Tremblay, M.S.; Broyles, S.T.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Kuriyan, R.; Kurpad, A.; Lambert, E.; et al. Relationships between parental education and overweight with childhood overweight and physical activity in 9–11 year old children: Results from a 12-country study. PLoS ONE 2016, 11, e0147746. [Google Scholar] [CrossRef]
- Mehryar, A.H.; Tashakkori, A. A father’s education as a determinant of socioeconomic and cultural characteristics of families in a sample of Iranian adolescents. Sociol. Inq. 1984, 54, 62–71. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- MacCallum, R.C.; Austin, J.T. Applications of structural equation modeling in psychological research. Ann. Rev. Psychol. 2000, 51, 201–226. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Cheung, M.K.T.; Hung, A.T.F.; Poon, P.K.K.; Chan, S.C.C.; Chan, C.C.H. Can a modified theory of planned behavior explain the effects of empowerment education for people with type 2 diabetes? Ther. Adv. Endocrinol. Metab. 2020, 11. [Google Scholar] [CrossRef]
- Rucker, D.D.; Preacher, K.J.; Tormala, Z.L.; Petty, R.E. Mediation analysis in social psychology: Current practices and new recommendations. Soc. Pers. Psychol. Compass 2011, 5, 359–371. [Google Scholar] [CrossRef]
- Cole, D.A.; Maxwell, S.E. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. J. Abnorm. Psychol. 2003, 112, 558–577. [Google Scholar] [CrossRef] [PubMed]
- Isomaa, R.; Isomaa, A.L.; Marttunen, M.; Kaltiala-Heino, R.; Björkqvist, K. Psychological distress and risk for eating disorders in subgroups of dieters. Eur. Eat. Disord. Rev. 2010, 18, 296–303. [Google Scholar] [PubMed]
- Roohafza, H.; Kabir, A.; Sadeghi, M.; Shokouh, P.; Aalaei-Andabili, S.H.; Mehrabi, Y.; Sarrafzadegan, N. Effect of psychological distress on weight concern and weight control behaviors. Arch. Iran Med. 2014, 17, 608–612. [Google Scholar]
- Cai, G.H.; Janson, C.; Theorell-Haglöw, J.; Benedict, C.; Elmståhl, S.; Lind, L.; Lindberg, E. Both weight at age 20 and weight gain have an impact on sleep disturbances later in life: Results of the EpiHealth Study. Sleep 2018, 41, zsx176. [Google Scholar] [CrossRef]
- Palm, A.; Janson, C.; Lindberg, E. The impact of obesity and weight gain on development of sleep problems in a population-based sample. Sleep Med. 2015, 16, 597. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Strong, C.; Scott, A.J.; Broström, A.; Pakpour, A.H.; Webb, T.L. A cluster randomized controlled trial of a theory-based sleep hygiene intervention for adolescents. Sleep 2018, 41, zsy170. [Google Scholar] [CrossRef]
- Strong, C.; Lin, C.-Y.; Jalilolghadr, S.; Updegraff, J.A.; Broström, A.; Pakpour, A.H. Sleep hygiene behaviors in Iranian adolescents: An application of the Theory of Planned Behavior. J. Sleep Res. 2018, 27, 23–31. [Google Scholar] [CrossRef]
| Mean ± SD or n (%) | |
|---|---|
| Age (Year) | 15.9 ± 3.2 |
| Gender (Male) | 372 (43.2) |
| Number of years education (father) | 8.6 ± 4.8 |
| Number of years education (mother) | 6.8 ± 3.9 |
| z-BMI at baseline | 2.4 ± 0.6 |
| z-BMI at one year follow-up | 2.4 ± 0.7 |
| Mothers’ BMI (kg/m2) | 40.2 ± 5.6 |
| Fathers’ BMI (kg/m2) | 37.8 ± 5.7 |
| Psychological distress a | 31.1 ± 15.9 |
| Eating Attitude Test-26 | 23.2 ± 10.4 |
| Food addiction b | 2.8 ± 1.3 |
| Insomnia Severity Index | 9.4 ± 4.3 |
| Time 2 z-BMI | Time 1 z-BMI | Psychological Distress 1 | Eating Disorder Attitudes 2 | Food Addiction 3 | Insomnia 4 | Mothers’ BMI | Fathers’ BMI | Age | Gender | Fathers’ Education | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| z-BMI at time 2 | 1 | 0.466 ** | 0.278 ** | 0.201 ** | 0.305 ** | 0.300 ** | 0.111 * | 0.129 * | 0.095 * | 0.045 | 0.136 ** |
| z-BMI at time 1 | 1 | 0.126 ** | 0.186 ** | 0.152 ** | 0.197 ** | 0.105 ** | 0.087 | 0.073 | 0.035 | ||
| Psychological distress 1 | 1 | 0.395 ** | 0.410 ** | 0.348 ** | 0.060 | 0.66 | 0.015 | 0.022 | 0.031 | ||
| Eating disorder attitudes 2 | 1 | 0.295 ** | 0.219 ** | 0.093 * | 0.089 * | 0.033 | 0.005 | 0.049 | |||
| Food addiction 3 | 1 | 0.303 ** | 0.081 * | 0.070 | 0.247 ** | 0.171 ** | 0.039 | ||||
| Insomnia 4 | 1 | 0.010 | 0.015 | 0.090 ** | 0.159 ** | 0.085 * | |||||
| Mothers’ BMI | 1 | 0.96 ** | 0.038 | 0.032 | 0.125 ** | ||||||
| Fathers’ BMI | 1 | 0.036 | 0.034 | 0.134 ** | |||||||
| Age | 1 | 0.014 | 0.021 | ||||||||
| Gender | 1 | −0.042 | |||||||||
| Fathers’ education | 1 |
| Unstand. Coeff. | SE or (Bootstrapping SE) | t-Value (p-Value) | Bootstrapping LLCI, ULCI | |
|---|---|---|---|---|
| Total effect of psychological distress on z-BMI | 3.40 | 0.45 | 7.62 (<0.001) | |
| Direct effect of psychological distress on z-BMI | 1.26 | 0.42 | 2.67 (0.003) | |
| Direct effect of psychological distress on mediators | ||||
| Eating disorder attitudes | 2.01 | 0.37 | 5.44 (<0.001) | |
| Food addiction | 0.31 | 0.04 | 8.82 (<0.001) | |
| Insomnia | 0.87 | 0.14 | 5.87 (<0.001) | |
| Indirect effect of psychological distress on z-BMI | ||||
| Total indirect effect | 2.14 | (0.37) | 5.78 (<0.001) | 1.43, 2.87 |
| Through eating disorder attitudes | 0.78 | (0.20) | 3.90 (<0.001) | 0.41, 1.20 |
| Through food addiction | 0.96 | (0.23) | 4.17 (<0.001) | 0.54, 1.43 |
| Through insomnia | 0.40 | (0.17) | 0.10, 0.78 |
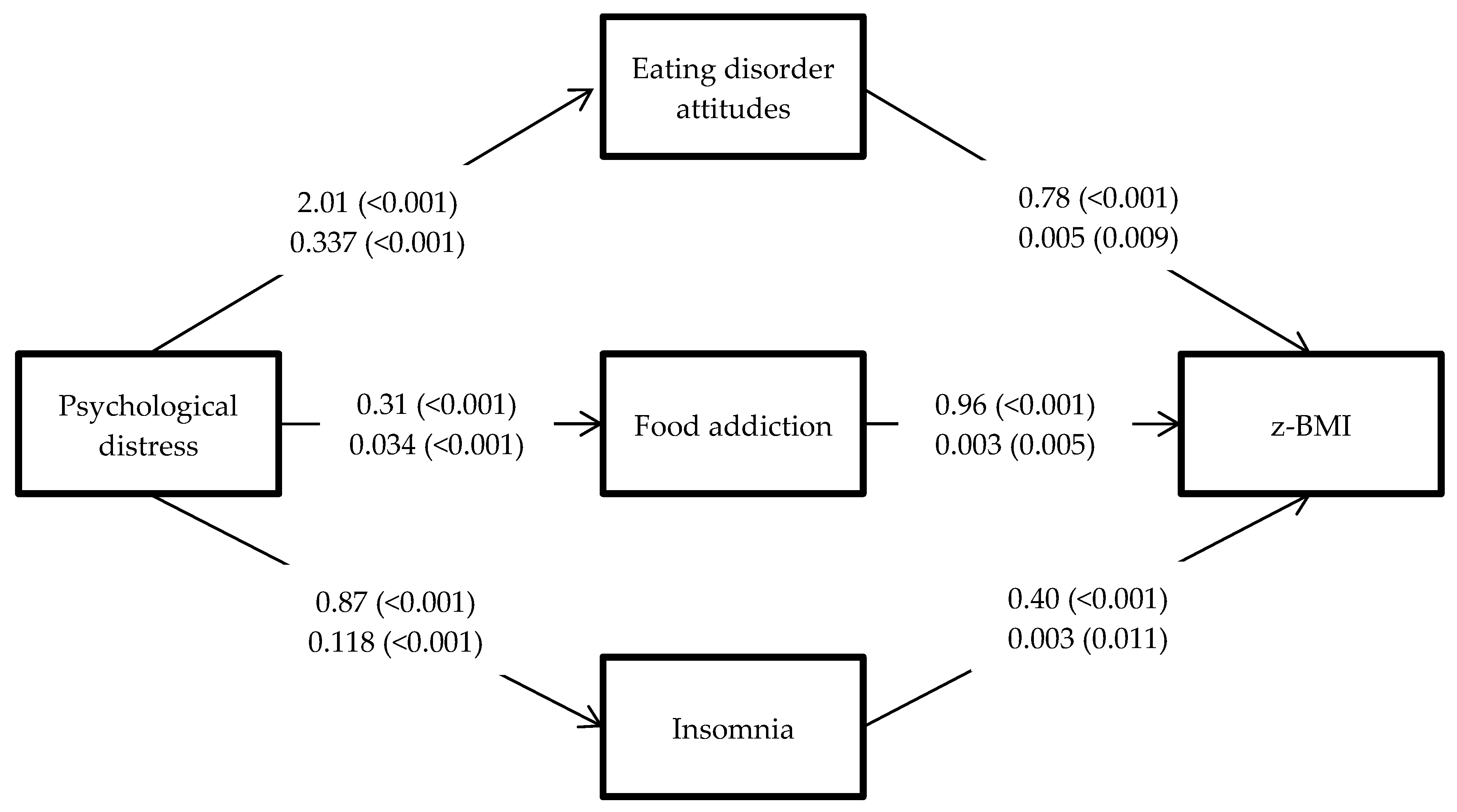
| Path | B (Bootstrapping SE) | β | LL | UL |
|---|---|---|---|---|
| Direct effects | ||||
| Psychological distress → z-BMI | 0.005 (0.001) | 0.054 ** | 0.001 | 0.009 |
| Psychological distress → food addiction | 0.034 (0.003) | 0.405 *** | 0.028 | 0.040 |
| Psychological distress → eating disorder attitudes | 0.337 (0.043) | 0.400 *** | 0.275 | 0.420 |
| Psychological distress →insomnia | 0.118 (0.021) | 0.331 *** | 0.079 | 0.149 |
| Indirect effects | ||||
| Psychological distress → food addiction →z-BMI | 0.003 (0.001) | 0.036 ** | 0.002 | 0.005 |
| Psychological distress → eating disorder attitudes →z-BMI | 0.005 (0.001) | 0.058 ** | 0.003 | 0.007 |
| Psychological distress → insomnia z-BMI | 0.003 (0.001) | 0.032 * | 0.001 | 0.004 |
| Psychological distress → food addiction, eating disorder attitudes, and insomnia→z-BMI | 0.011 (0.002) | 0.041 ** | 0.008 | 0.014 |
| Total effects | ||||
| Psychological distress →z-BMI | 0.015 (0.003) | 0.172 * | 0.010 | 0.019 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-Y.; Cheung, P.; Imani, V.; Griffiths, M.D.; Pakpour, A.H. The Mediating Effects of Eating Disorder, Food Addiction, and Insomnia in the Association between Psychological Distress and Being Overweight among Iranian Adolescents. Nutrients 2020, 12, 1371. https://doi.org/10.3390/nu12051371
Lin C-Y, Cheung P, Imani V, Griffiths MD, Pakpour AH. The Mediating Effects of Eating Disorder, Food Addiction, and Insomnia in the Association between Psychological Distress and Being Overweight among Iranian Adolescents. Nutrients. 2020; 12(5):1371. https://doi.org/10.3390/nu12051371
Chicago/Turabian StyleLin, Chung-Ying, Pauline Cheung, Vida Imani, Mark D. Griffiths, and Amir H. Pakpour. 2020. "The Mediating Effects of Eating Disorder, Food Addiction, and Insomnia in the Association between Psychological Distress and Being Overweight among Iranian Adolescents" Nutrients 12, no. 5: 1371. https://doi.org/10.3390/nu12051371
APA StyleLin, C.-Y., Cheung, P., Imani, V., Griffiths, M. D., & Pakpour, A. H. (2020). The Mediating Effects of Eating Disorder, Food Addiction, and Insomnia in the Association between Psychological Distress and Being Overweight among Iranian Adolescents. Nutrients, 12(5), 1371. https://doi.org/10.3390/nu12051371






