Circulating Levels of Muscle-Related Metabolites Increase in Response to a Daily Moderately High Dose of a Vitamin D3 Supplement in Women with Vitamin D Insufficiency—Secondary Analysis of a Randomized Placebo-Controlled Trial
Abstract
1. Introduction
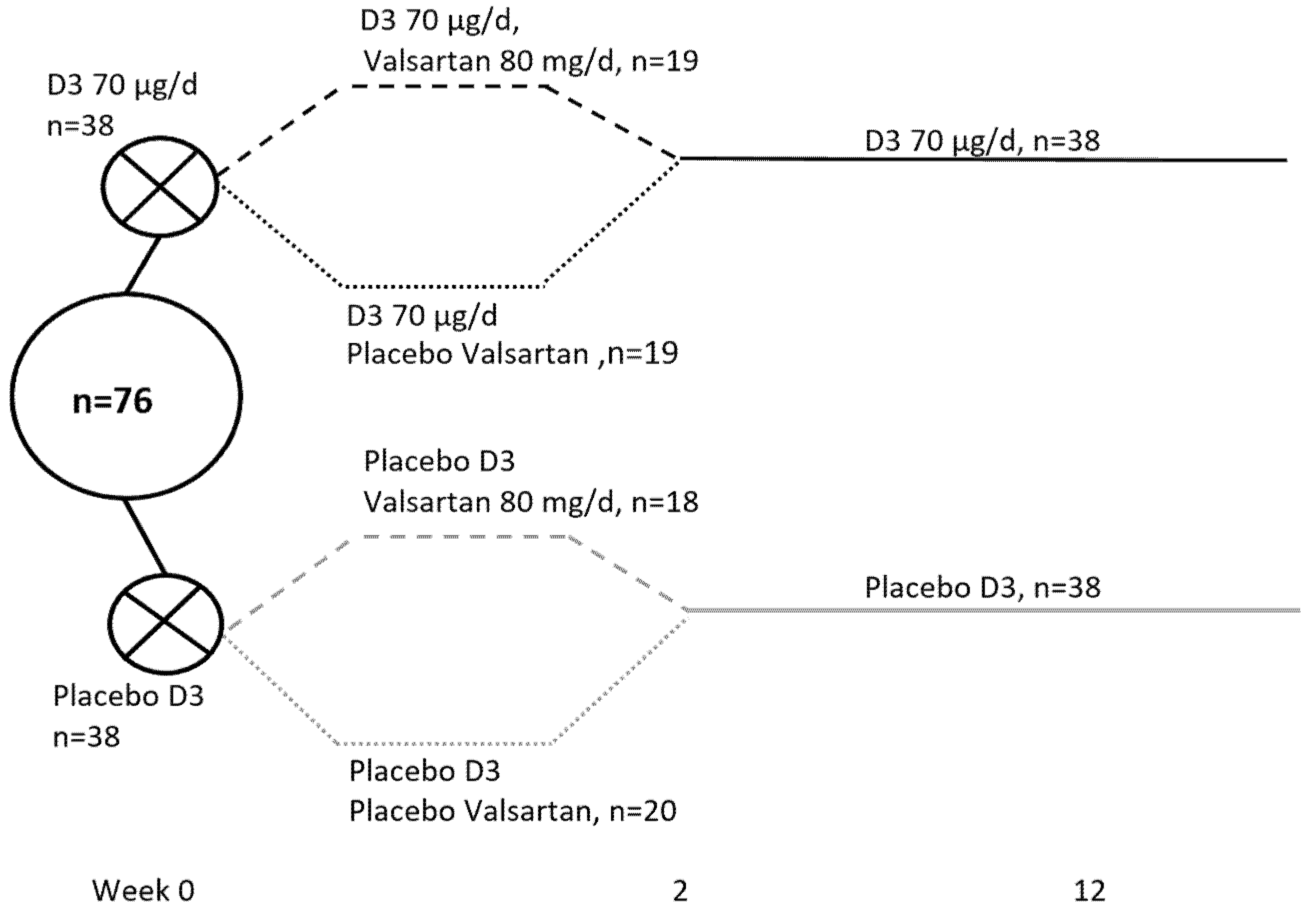
2. Materials and Methods
3. Results
3.1. Baseline Characteristics and Effects of Vitamin D Supplementation on 25(OH)D, 1,25(OH)2D, and PTH Levels
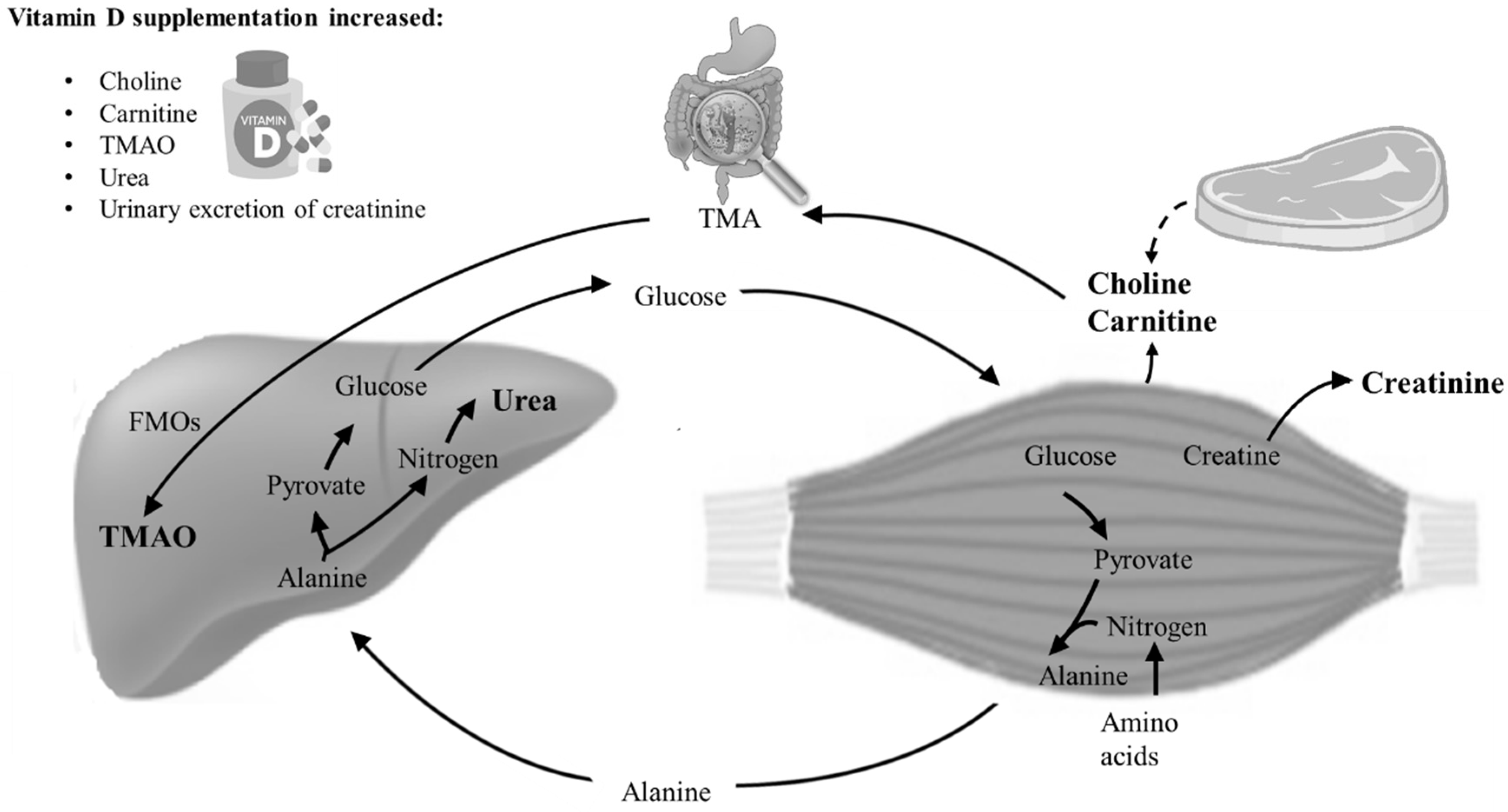
3.2. Changes in Muscle-Related Metabolites
3.3. The Effect of Valsartan on the Metabolome
3.4. Nutrient Intake and Physical Activity
3.5. Correlations between Muscle-Related Metabolites, Body Composision, Musle Strength, and Physical Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hansen, L.; Tjønneland, A.; Køster, B.; Brot, C.; Andersen, R.; Cohen, A.S.; Frederiksen, K.; Olsen, A. Vitamin D Status and Seasonal Variation among Danish Children and Adults: A Descriptive Study. Nutritients 2018, 10, 1801. [Google Scholar] [CrossRef] [PubMed]
- Lips, P. Vitamin D Deficiency and Secondary Hyperparathyroidism in the Elderly: Consequences for Bone Loss and Therapeutic Implications. Endocr. Rev. 2001, 22, 477–501. [Google Scholar] [CrossRef]
- Rødbro, L.L.; Bislev, L.S.; Sikjær, T.; Rejnmark, L. Bone metabolism, density, and geometry in postmenopausal women with vitamin D insufficiency: A cross-sectional comparison of the effects of elevated parathyroid levels. Osteoporos. Int. 2018, 29, 2211–2218. [Google Scholar] [CrossRef] [PubMed]
- Bislev, L.S.; Rødbro, L.L.; Sikjaer, T.; Rejnmark, L. Effects of elevated PTH levels on muscle health, postural stability and quality of life in vitamin D insufficient healthy women: A cross-sectional study. Calcif. Tissue Int. 2019, 105, 642–650. [Google Scholar] [CrossRef] [PubMed]
- Bouillon, R. Comparative analysis of nutritional guidelines for vitamin D. Nat. Rev. Endocrinol. 2017, 13, 466–479. [Google Scholar] [CrossRef] [PubMed]
- Sanders, K.M.; Seibel, M.J. Therapy: New findings on vitamin D3 supplementation and falls—When more is perhaps not better. Nat. Rev. Endocrinol. 2016, 12, 190–191. [Google Scholar] [CrossRef]
- Reid, I.R. High-Dose Vitamin D: Without Benefit but Not Without Risk. J. Intern. Med. 2018, 284, 694–696. [Google Scholar] [CrossRef]
- Grübler, M.R.; März, W.; Pilz, S.; Grammer, T.B.; Trummer, C.; Müllner, C.; Schwetz, V.; Pandis, M.; Verheyen, N.; Tomaschitz, A.; et al. Vitamin-D concentrations, cardiovascular risk and events—A review of epidemiological evidence. Rev. Endocr. Metab. Disord. 2017, 18, 259–272. [Google Scholar] [CrossRef]
- Rejnmark, L.; Bislev, L.S.; Cashman, K.D.; Eiríksdottir, G.; Gaksch, M.; Grübler, M.; Grimnes, G.; Gudnason, V.; Lips, P.; Pilz, S.; et al. Non-skeletal health effects of vitamin D supplementation: A systematic review on findings from meta-analyses summarizing trial data. PLoS ONE 2017, 12, e0180512. [Google Scholar] [CrossRef]
- Jorde, R.; Grimnes, G. Vitamin D and health: The need for more randomized controlled trials. J. Steroid Biochem. Mol. Biol. 2015, 148, 269–274. [Google Scholar] [CrossRef]
- Tokarz, J.; Haid, M.; Cecil, A.; Prehn, C.; Artati, A.; Möller, G.; Adamski, J. Endocrinology Meets Metabolomics: Achievements, Pitfalls, and Challenges. Trends Endocrinol. Metab. 2017, 28, 705–721. [Google Scholar] [CrossRef] [PubMed]
- Kaddurah-Daouk, R.; Weinshilboum, R. Metabolomic signatures for drug response phenotypes: Pharmacometabolomics enables precision medicine. Clin. Pharmacol. Ther. 2015, 98, 71–75. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, A.; Gibney, M.J.; Connor, A.O.; Mion, B.; Kaluskar, S.; Cashman, K.D.; Flynn, A.; Shanahan, F.; Brennan, L. Biochemical and metabolomic phenotyping in the identification of a vitamin D responsive metabotype for markers of the metabolic syndrome. Mol. Nutr. Food Res. 2011, 55, 679–690. [Google Scholar] [CrossRef] [PubMed]
- Bislev, L.S.; Langagergaard Rødbro, L.; Bech, J.N.; Pedersen, E.B.; Kjaergaard, A.D.; Ladefoged, S.A.; Rolighed, L.; Sikjaer, T.; Rejnmark, L. The effect of vitamin D3 supplementation on markers of cardiovascular health in hyperparathyroid, vitamin D insufficient women: A randomized placebo-controlled trial. Endocrine 2018, 62, 82–194. [Google Scholar] [CrossRef]
- Bislev, L.S.; Langagergaard Rødbro, L.; Nørgaard Bech, J.; Bjerregaard Pedersen, E.; Rolighed, L.; Sikjaer, T.; Rejnmark, L. Effects of treatment with an angiotensin 2 receptor blocker and/or vitamin D3 on parathyroid hormone and aldosterone: A randomized, placebo-controlled trial. Clin. Endocrinol. 2018, 89, 656–666. [Google Scholar] [CrossRef]
- Bislev, L.S.; Langagergaard Rødbro, L.; Rolighed, L.; Sikjaer, T.; Rejnmark, L. Effects of Vitamin D3 Supplementation on Muscle Strength, Mass, and Physical Performance in Women with Vitamin D Insufficiency: A Randomized Placebo-Controlled Trial. Calcif. Tissue Int. 2018, 103, 483–493. [Google Scholar] [CrossRef]
- Bislev, L.S.; Langagergaard Rødbro, L.; Rolighed, L.; Sikjaer, T.; Rejnmark, L. Bone Microstructure in Response to Vitamin D3 Supplementation: A Randomized Placebo-Controlled Trial. Calcif. Tissue Int. 2018, 104, 160–170. [Google Scholar] [CrossRef]
- Roth, H.J.; Schmidt-Gayk, H.; Weber, H.; Niederau, C. Accuracy and clinical implications of seven 25-hydroxyvitamin D methods compared with liquid chromatography-tandem mass spectrometry as a reference. Ann. Clin. Biochem. 2008, 45, 153–159. [Google Scholar] [CrossRef]
- Fielding, R.; Riede, L.; Lugo, J.P.; Bellamine, A. L-carnitine supplementation in recovery after exercise. Nutrients 2018, 10, 349. [Google Scholar] [CrossRef]
- Wiedeman, A.M.; Barr, S.I.; Green, T.J.; Xu, Z.; Innis, S.M.; Kitts, D.D. Dietary choline intake: Current state of knowledge across the life cycle. Nutrients 2018, 10, 1513. [Google Scholar] [CrossRef]
- Peeling, P.; Binnie, M.J.; Goods, P.S.R.; Sim, M.; Burke, L.M. Evidence-based supplements for the enhancement of athletic performance. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Consolo, S.; Romano, H.; Scozzesi, C.; Bonetti, A.; Ladinsky, H. Acetylcholine and Choline Contents of Rat Skeletal Muscle Determined by a Radioenzymatic Microassay: Effects of Drugs. Dyn. Cholinergic Funct. 1986, 30, 583–592. [Google Scholar]
- Fayad, L.M.; Salibi, N.; Wang, X.; Machado, A.J.; Jacobs, M.A.; Ouwerkerk, R.; Okollie, B.; David, A.; Eng, J.; Barker, P.B. Quantification of Muscle Choline Concentration by Proton MR Spectroscopy at 3 Tesla: Technical Feasibility. 2010, 194, W73–W79. Am. J. Roentgenol. 2010, 194, W73–W79. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Felig, P. The glucose-alanine cycle. Metabolism 1973, 22, 179–207. [Google Scholar] [CrossRef]
- Ufnal, M.; Anna, Z.; Ryszard, O. TMAO: A small molecule of great expectations. Nutrition 2015, 31, 1317–1323. [Google Scholar] [CrossRef]
- Koeth, R.A.; Wang, Z.; Levison, B.S.; Buffa, J.A.; Org, E.; Sheehy, B.T.; Britt, E.B.; Fu, X.; Wu, Y.; Li, L.; et al. Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013, 19, 576–585. [Google Scholar] [CrossRef]
- Aldana-Hernández, P.; Leonard, K.A.; Zhao, Y.Y.; Curtis, J.M.; Field, C.J.; Jacobs, R.L. Dietary Choline or Trimethylamine N-oxide Supplementation Does Not Influence Atherosclerosis Development in Ldlr-/- and Apoe-/- Male Mice. J. Nutr. 2020, 150, 249–255. [Google Scholar] [CrossRef]
- Zhou, T.; Heianza, Y.; Chen, Y.; Li, X.; Sun, D.; DiDonato, J.A.; Pei, X.; LeBoff, M.S.; Bray, G.A.; Sacks, F.M.; et al. Circulating gut microbiota metabolite trimethylamine N-oxide (TMAO) and changes in bone density in response to weight loss diets: The Pounds lost trial. Diabetes Care 2019, 42, 1365–1371. [Google Scholar] [CrossRef]
- Salazar, J.H. Overview of Urea and Creatinine. Lab. Med. 2014, 45, e19–e20. [Google Scholar] [CrossRef]
- Grove-Laugesen, D.; Cramon, P.K.; Malmstroem, S.; Ebbehoj, E.; Watt, T.; Hansen, K.W.; Rejnmark, L. Effects of supplemental vitamin D on muscle performance and quality of life in Graves’ disease. A randomized clinical trial. Thyroid 2020, 30, 661–671. [Google Scholar] [CrossRef]
- Ginde, A.A.; Blatchford, P.; Breese, K.; Zarrabi, L.; Linnebur, S.A.; Wallace, J.I.; Schwartz, R.S. High-Dose Monthly Vitamin D for Prevention of Acute Respiratory Infection in Older Long-Term Care Residents: A Randomized Clinical Trial. J. Am. Geriatr. Soc. 2017, 65, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.M.; Gallagher, J.C.; Suiter, C. Medium doses of daily vitamin D decrease falls and higher doses of daily vitamin D3 increase falls: A randomized clinical trial. J. Steroid Biochem. Mol. Biol. 2017, 173, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Bischoff-Ferrari, H.A.; Dawson-Hughes, B.; John Orav, E.; Staehelin, H.B.; Meyer, O.W.; Theiler, R.; Dick, W.; Willett, W.C.; Egli, A. Monthly high-dose Vitamin D treatment for the prevention of functional decline a randomized clinical trial. JAMA Intern. Med. 2016, 176, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Mason, C.; Tapsoba, J.D.; Duggan, C.; Imayama, I.; Wang, C.-Y.; Korde, L.; McTiernan, A. Effects of Vitamin D 3 Supplementation on Lean Mass, Muscle Strength, and Bone Mineral Density During Weight Loss: A Double-Blind Randomized Controlled Trial. J. Am. Geriatr. Soc. 2016, 64, 769–778. [Google Scholar] [CrossRef] [PubMed]
- Uusi-Rasi, K.; Patil, R.; Karinkanta, S.; Kannus, P.; Tokola, K.; Lamberg-Allardt, C.; Sievänen, H. Exercise and vitamin din fall prevention among older women a randomized clinical trial. JAMA Intern. Med. 2015, 175, 703–711. [Google Scholar] [CrossRef]
- Sanders, K.M.; Stuart, A.L.; Williamson, E.J.; Simpson, J.A.; Kotowicz, M.A.; Young, D.; Nicholson, G.C. Annual high-dose oral vitamin D and falls and fractures in older women: A randomized controlled trial. JAMA 2010, 303, 1815–1822. [Google Scholar] [CrossRef]
- Burt, L.A.; Gabel, L.; Billington, E.O.; Hanley, D.A.; Boyd, S.K. Postural Balance Effects Associated with 400, 4000 or 10,000 IU Vitamin D3 Daily for Three Years: A Secondary Analysis of a Randomized Clinical Trial. Nutrients 2020, 12, 527. [Google Scholar] [CrossRef]
- Grimnes, G.; Emaus, N.; Cashman, K.D.; Jorde, R. The effect of high-dose vitamin D supplementation on muscular function and quality of life in postmenopausal women—A randomized controlled trial. Clin. Endocrinol. 2017, 87, 20–28. [Google Scholar] [CrossRef]
- Camperi, A.; Pin, F.; Costamagna, D.; Penna, F.; Menduina, M.L.; Aversa, Z.; Zimmers, T.; Verzaro, R.; Fittipaldi, R.; Caretti, G.; et al. Vitamin D and VDR in cancer cachexia and muscle regeneration. Oncotarget 2017, 8, 21778–21793. [Google Scholar] [CrossRef]
- Owens, D.J.; Sharples, A.P.; Polydorou, I.; Alwan, N.; Donovan, T.; Tang, J.; Fraser, W.D.; Cooper, R.G.; Morton, J.P.; Stewart, C.; et al. A systems-based investigation into vitamin D and skeletal muscle repair, regeneration, and hypertrophy. Am. J. Physiol.-Endocrinol. Metab. 2015, 309, E1019–E1031. [Google Scholar] [CrossRef]
- Debruin, D.A.; Timpani, C.A.; Lalunio, H.; Rybalka, E.; Goodman, C.A.; Hayes, A. Exercise May Ameliorate the Detrimental Side Effects of High Vitamin D Supplementation on Muscle Function in Mice. J. Bone Miner. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Dina, R.; Jafari, M. Angiotensin II-receptor antagonists: An overview. Am. J. Health Pharm. 2000, 57, 1231–1241. [Google Scholar] [CrossRef] [PubMed]
| Vitamin D (n = 38) | Placebo (n = 38) | p-Value | |
|---|---|---|---|
| Age and body composition | |||
| Age (years) | 64.5 [61.0; 68.25] | 65.5 [62.0; 68.25] | 0.56 |
| Body weight (Kg) | 75.3 [67.3; 90.3] | 70.4 [65.0; 78.2] | 0.17 |
| Height (cm) | 166.2 ± 4.7 | 165.1 ± 6.0 | 0.39 |
| Body mass index (Kg/m2) | 27.3 [23.3; 32.0] | 26.8 [23.6; 28.8] | 0.42 |
| Appendicular lean mass index (Kg/m2) | 10.8 [10.0; 12.1] | 10.7 [10.1; 11.5] | 0.56 |
| Fat mass index (Kg/m2) | 18.7 [14.1; 23.8] | 17.9 [12.5; 20.2] | 0.16 |
| Indices of bone health | |||
| Calcium intake (mg/day) | 850 [700; 950] | 700 [650; 1075] | 0.87 |
| History of fracture in adulthood n (%) | 13 (34) | 7 (20) | 0.12 |
| Smoking statusn(%) | 0.22 | ||
| Never | 23 (61) | 22 (68) | |
| Current | 1 (3) | 5 (13) | |
| Former | 14 (37) | 11 (29) | |
| Use of medication | |||
| Any n (%) | 13 (34) | 13 (34) | 0.60 |
| Indices of cardiovascular health | |||
| Systolic 24 h blood pressure (mmHg) | 129 [125; 146] | 128 [118; 135] | 0.14 |
| Diastolic 24 h blood pressure (mmHg) | 75 [68; 83] | 74 [68; 79] | 0.31 |
| Total cholesterol (mmol/L) | 5.2 [4.8; 5.9] | 5.5 [5.0; 6.4] | 0.12 |
| HDL (mmol/L) | 1.8 ± 0.4 | 1.8 ± 0.4 | 0.76 |
| LDL (mmol/L) | 3.0 ± 0.8 | 3.3 ± 1.0 | 0.14 |
| Triglycerides (mmol/L) | 1.1 [0.7; 1.3] | 0.9 [0.7; 1.3] | 0.65 |
| Arterial stiffness (m2/s) | 9.7 ± 1.7 | 9.1 ± 1.3 | 0.10 |
| Changes (Δ) | |||||
|---|---|---|---|---|---|
| Ref.Range | Baseline, n = 76 | Vitamin D, n = 38 | Placebo, n = 38 | p-Value | |
| Plasma | |||||
| 25(OH)D (nmol/L) | 50–160 | 33 ± 9 | 58.5 ± 16.3 | −4.5 ± 6.3 | <0.00001 |
| 1.25(OH)2D (pmol/L) | 60–180 | 53 ± 14 | 18.5 ± 15.2 | −9.6 ± 9.9 | <0.00001 |
| PTH (pmol/L) | 1.6–6.9 | 6.1 ± 1.3 | -0.69 ± 0.79 | 0.28 ± 0.80 | <0.00001 |
| Ca2+ (mmol/L) | 1.18–1.32 | 1.25 ± 0.04 | 0.00 ± 0.04 | −0.01 ± 0.03 | 0.20 |
| Magnesium (mmol/L) | 0.7–1.1 | 0.88 ± 0.06 | -0.01 ± 0.04 | 0.01 ± 0.04 | 0.24 |
| Phosphate (mmol/L) | 0.76–1.41 | 1.00 ± 0.14 | 0.06 ± 0.11 | 0.04 ± 0.12 | 0.52 |
| eGRF | >60 mL/min | 82.4 [73.1; 90.7] | −2.18 [−5.45; 4.21] | −1.15 [−5.30; 1.76] | 0.94 |
| Urine | |||||
| Creatinine (mmol/24 h) | 6–15 | 10.3 ± 1.9 | 0.33 ± 1.53 | −0.37 ± 1.67 | 0.06 |
| Metabolites | Baseline, µmol/L, n = 76 | Changes (Δ), µmol/L | p-Value | |
|---|---|---|---|---|
| Vitamin D, n = 38 | Placebo n = 38 | |||
| Hydroxybutyrate | 38 [22; 90] | −0.34 [−55; 25] | 2.1 [−34; 29] | 0.58 |
| Acetate | 16 [9; 23] | −2.0 [−11; 2.8] | −0.33 [−12; 2.7] | 0.92 |
| Acetoacetate | 18 [10; 29] | 1.4 [−14; 14] | 2.4 [−7.8; 10] | 0.93 |
| Acetone | 7.1 [5.6; 11] | −1.3 [−7.4; 1.3] | −1.0 [−3.1; 1.8] | 0.33 |
| Alanine | 210 ± 57 | 8.3 [−15; 47] | 7.1 [−30; 38] | 0.26 |
| Betaine | 16 [9; 23] | 3.3 (−0.9 to 5.5) | 0.3 (−2.7 to 3.3) | 0.36 |
| Carnitine | 77 [65; 86] | 6.0 (−1.1 to 13) | −5.5 (−13 to 2.0) | 0.03 |
| Choline | 15 ± 6 | −0.00 (−2.2 to 2.1) | −4.1 (−6.7 to −1.6) | 0.02 |
| Citrate | 93 [82; 108] | −0.42 (−8.9 to 8.0) | −1.1 (−7.8 to 5.7) | 0.91 |
| Creatine | 23 [18; 31] | 3.5 (−0.44 to 7.5) | 4.2 (−0.76 to 9.1) | 0.84 |
| Creatinine | 49 ± 11 | 8.6 (3.4 to 14) | 5.3 (1.7 to 8.9) | 0.30 |
| Dimethylamine | 1.5 [1.0; 4.3] | 0.3 [0.0; 0.8] | 0.1 [−0.30; 0.5] | 0.25 |
| Formate | 1.3 [0.8; 2.1] | 0.0 (−0.24 to 0.3) | −0.01 (−0.29 to 0.3) | 0.91 |
| Glucose | 5500 [5125; 6000] | 0.0 [−225; 300] | −100 [−325; 100] | 0.31 |
| Glutamate | 48 [35; 73] | −2.1 [−23; 18] | −14 [−28; 7.0] | 0.15 |
| Glutamine | 470 [410; 520] | 64 [14; 130] | 60 [15; 127] | 0.82 |
| Glycerol | 390 [320; 530] | 0.0 [−180; 80] | −34 [−160; 71] | 0.65 |
| Glycine | 69 ± 22 | 6.4 (−0.30 to 13) | 2.9 (−5.7 to 11) | 0.52 |
| Isoleucine | 67 [59; 80] | 4.6 [−6.1; 19] | 4.4 [−10; 12] | 0.19 |
| Lactate | 750 [650; 970] | 77 (−31 to 180) | 10.7 (−92 to 110) | 0.37 |
| Leucine | 150 [140; 170] | 12 [−8.2; 36] | −2.5 [−20; 24] | 0.17 |
| Lysine | 260 [240; 280] | 13 [−30; 60] | 6.2 [−8.3; 46] | 0.83 |
| Methionine | 19 [17; 26] | −1.8 [−8.6; 2.1] | −2.7 [−7.6; 0.8] | 0.58 |
| OPhosphocholine | 19 [16; 24] | −1.2 (−2.7 to 0.4) | −1.2 (−2.9 to 0.5) | 0.98 |
| Ornithine | 83 [61; 110] | 5.9 (−11 to 23) | 5.0 (−8.0 to 18) | 0.93 |
| Phenylalanine | 57 [51; 65] | 4.7 (−0.1 to 9.6) | 0.4 (−3.5 to 4.4) | 0.17 |
| Proline | 150 [110; 280] | 52 (27 to 77) | 25 (2 to 47) | 0.11 |
| Pyruvate | 12 [7; 18] | 4.5 (1.7 to 7.4) | 4.9 (1.9 to 7.9) | 0.87 |
| Succinate | 3.6 [2.6; 6.6] | −0.25 [−2.9; 0.6] | −0.9 [−4.7; 1.4] | 0.87 |
| Threonine | 83 [74; 91] | 8.2 [−8.3; 17] | 6.8 [−2.6; 18] | 0.89 |
| TMAO | 36 [31; 42] | 6.3 (1.5 to 11) | 0.6 (−2.7 to 4.0) | 0.05 |
| Tyrosine | 59 ± 15 | 3.0 [−5.5; 12] | 1.0 [−4.2; 9.0] | 0.32 |
| Urea | 180 [150; 220] | 45 (24 to 66) | 13 (−7.0 to 34) | 0.03 |
| Valine | 240 [200; 280] | 14 [−5.0; 46] | 0.9 [−21; 31] | 0.11 |
| τMethylhistidine | 110 [100; 120] | 3.6 [−13; 30] | 4.8 [−13; 30] | 0.34 |
| Changes (Δ) | Total Fat Mass | TUG | Handgrip Strength | Knee Flexion 60° | ||||
|---|---|---|---|---|---|---|---|---|
| r | p-Value | r | p-Value | r | p-Value | R | p-Value | |
| 25(OH)D, nmol/L | - | - | - | - | −0.27 | 0.03 | −0.29 | 0.02 |
| Carnitine, mmol/L | 0.29 | 0.01 | 0.29 | 0.01 | - | - | - | - |
| Choline, mmol/L | - | - | 0.23 | 0.04 | −0.25 | 0.04 | - | - |
| Urea, mmol/L | 0.25 | 0.03 | 0.26 | 0.02 | - | - | - | - |
| Urine creatinine, mmol/day | - | - | - | - | −0.26 | 0.04 | - | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bislev, L.S.; Sundekilde, U.K.; Kilic, E.; Dalsgaard, T.K.; Rejnmark, L.; Bertram, H.C. Circulating Levels of Muscle-Related Metabolites Increase in Response to a Daily Moderately High Dose of a Vitamin D3 Supplement in Women with Vitamin D Insufficiency—Secondary Analysis of a Randomized Placebo-Controlled Trial. Nutrients 2020, 12, 1310. https://doi.org/10.3390/nu12051310
Bislev LS, Sundekilde UK, Kilic E, Dalsgaard TK, Rejnmark L, Bertram HC. Circulating Levels of Muscle-Related Metabolites Increase in Response to a Daily Moderately High Dose of a Vitamin D3 Supplement in Women with Vitamin D Insufficiency—Secondary Analysis of a Randomized Placebo-Controlled Trial. Nutrients. 2020; 12(5):1310. https://doi.org/10.3390/nu12051310
Chicago/Turabian StyleBislev, Lise Sofie, Ulrik Kræmer Sundekilde, Ece Kilic, Trine Kastrup Dalsgaard, Lars Rejnmark, and Hanne Christine Bertram. 2020. "Circulating Levels of Muscle-Related Metabolites Increase in Response to a Daily Moderately High Dose of a Vitamin D3 Supplement in Women with Vitamin D Insufficiency—Secondary Analysis of a Randomized Placebo-Controlled Trial" Nutrients 12, no. 5: 1310. https://doi.org/10.3390/nu12051310
APA StyleBislev, L. S., Sundekilde, U. K., Kilic, E., Dalsgaard, T. K., Rejnmark, L., & Bertram, H. C. (2020). Circulating Levels of Muscle-Related Metabolites Increase in Response to a Daily Moderately High Dose of a Vitamin D3 Supplement in Women with Vitamin D Insufficiency—Secondary Analysis of a Randomized Placebo-Controlled Trial. Nutrients, 12(5), 1310. https://doi.org/10.3390/nu12051310







