Nutrition and Lifestyle Behavior Peer Support Program for Adults with Metabolic Syndrome: Outcomes and Lessons Learned from a Feasibility Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Development of PERSUADE Peer Support Module
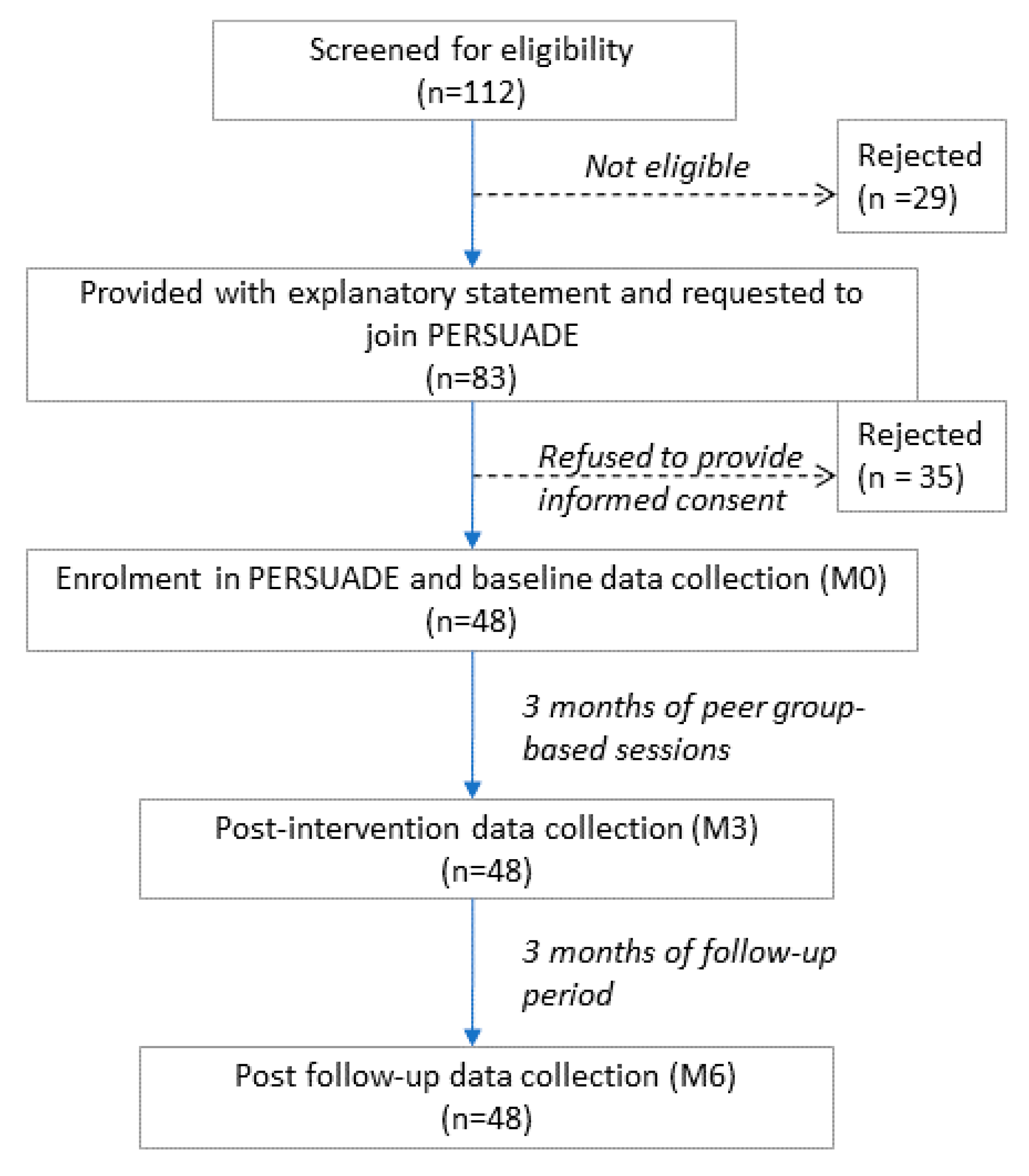
2.2. Feasibility Trial
2.2.1. Study Participants
2.2.2. Peer Leader Training Program
2.2.3. Peer Session by Peer Leaders
2.2.4. Data Collection and Measurements
2.2.5. Data Analysis
3. Results
3.1. Dietary Behaviors
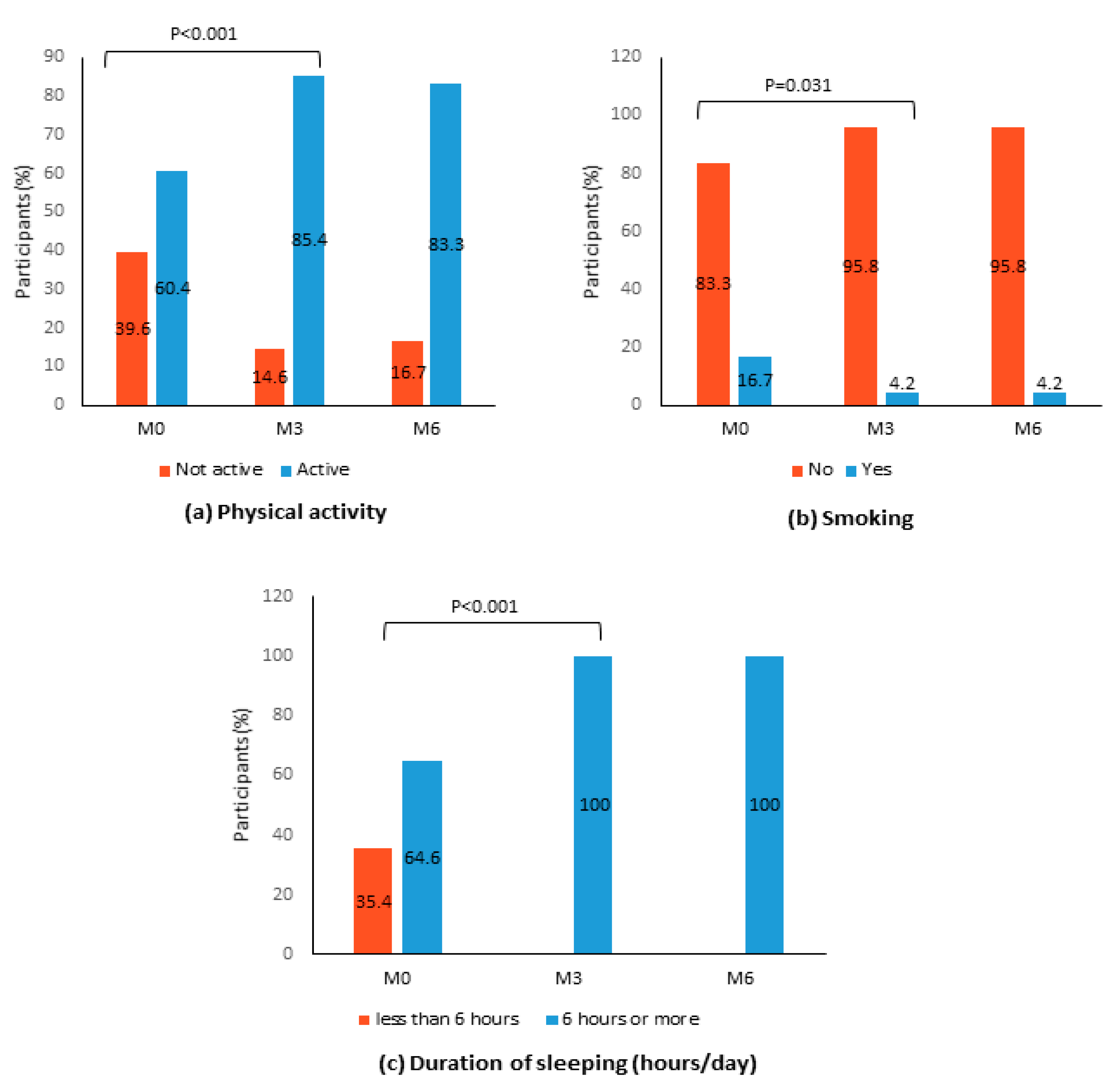
3.2. Lifestyle Behaviors
3.3. Anthropometry and Metabolic Parameters
4. Discussion
4.1. Lessons Learned from PERSUADE
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Ghee, L.K.; Kooi, C.W. A review of metabolic syndrome research in Malaysia. Med. J. Malays. 2016, 71, 20–28. [Google Scholar]
- Ramli, A.S.; Daher, A.M.; Nor-Ashikin, M.N.K.; Mat-Nasir, N.; Ng, K.K.; Miskan, M.; Ambigga, K.S.; Ariffin, F.; Mazapuspavina, M.Y.; Abdul-Razak, S.; et al. JIS definition identified more Malaysian adults with metabolic syndrome compared to the NCEP-ATP III and IDF Criteria. Biomed. Res. Int. 2013, 760963. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.A.; Gowda, U.; Smith, B.J.; Renzaho, A.M. Systematic review of the effect of lifestyle interventions on the components of the metabolic syndrome in South Asian migrants. J. Immigr. Minor. Health 2016, 20, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Rezaianzadeh, A.; Namayandeh, S.M.; Sadr, S.M. National Cholesterol Education Program Adult Treatment Panel III Versus International Diabetic Federation definition of metabolic syndrome, which one is associated with diabetes mellitus and coronary artery disease? Int. J. Prev. Med. 2012, 3, 552–558. [Google Scholar]
- Ministry of Health. National Strategic Plan for Non-Communicable Disease (NSP- NCD) 2010-2014; Ministry of Health: Kuala Lumpur, Malaysia, 2010.
- Toro-Ramos, T.; Lee, D.H.; Kim, Y.; Michaelides, A.; Oh, T.J.; Kim, K.M.; Jang, H.C.; Lim, S. Effectiveness of a smartphone application for the management of metabolic syndrome components focusing on weight loss: A preliminary study. Metab. Syndr. Relat. Disord. 2017, 15, 465–473. [Google Scholar] [CrossRef]
- Brown, T.; Avenell, A.; Edmunds, L.D.; Moore, H.; Whittaker, V.; Avery, L.; Summerbell, C. Systematic review of long-term lifestyle interventions to prevent weight gain and morbidity in adults. Obes. Rev. 2009, 10, 627–638. [Google Scholar] [CrossRef]
- Doull, M.; O’Connor, A.M.; Welch, V.; Tugwell, P.; Wells, G.A. Peer support strategies for improving the health and well-being of individuals with chronic diseases. Cochrane Database Syst. Rev. 2017, CD005352. [Google Scholar] [CrossRef]
- Sanee, A.; Somrongthong, R.; Plianbangchang, S. The positive effects of a peer-led intervention system for individuals with a risk of metabolic syndrome. J. Multidiscip. Healthc. 2017, 10, 293–300. [Google Scholar] [CrossRef]
- Ahmad Sharoni, S.K.; Abdul Rahman, H.; Minhat, H.S.; Shariff-Ghazali, S.; Azman Ong, M.H. The effects of self-efficacy enhancing program on foot self-care behaviour of older adults with diabetes: A randomised controlled trial in elderly care facility, Peninsular Malaysia. PLoS ONE 2018, 13, e0192417. [Google Scholar] [CrossRef]
- Nalliah, S. Strategic interventions in the management of gestational diabetes to reduce type 2 diabetes mellitus in women in Malaysia. Med. J. Malays. 2015, 70, 211–213. [Google Scholar]
- Yap, R.W.K.; Shidoji, Y.; Hon, W.M.; Masaki, M. Interaction between VEGF receptor-2 gene polymorphisms and dietary patterns on blood glucose and lipid levels in Chinese Malaysian adults. J. Nutrigenet. Nutrigenom. 2012, 4, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I.M. The Health Belief Model: Explaining health behavior through expectancies. In Health Behavior and Health Education: Theory, Research, and Practice; Glanz, K., Lewis, F.M., Rimer, B.K., Eds.; Jossey-Bass: San Francisco, CA, USA, 1990; pp. 39–62. [Google Scholar]
- Muhammad Daniel, A.M.; Quek, K.F.; Ramadas, A. Process evaluation of a nutrition and lifestyle and behavior peer support program for adults with metabolic syndrome. Int. J. Environ. Res. Public Health 2020, 17, 2641. [Google Scholar] [CrossRef]
- Billingham, S.A.M.; Whitehead, A.L.; Julious, S.A. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med. Res. Methodol. 2013, 13, 104. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report on a WHO Consultation on the Epidemiology of Obesity; World Health Organization: Warsaw, Poland, 1987. [Google Scholar]
- Suzara, S.; Noor Aini, M.Y.; Nik Shanita, S.; Rafidah, G.; Roslina, A. Atlas Makanan: Saiz Pertukaran & Porsi; MDC Publisher: Kuala Lumpur, Malaysia, 2009. [Google Scholar]
- Shyam, S.; Wai, T.N.; Arshad, F. Adding glycaemic index and glycaemic load functionality to DietPLUS, a Malaysian food composition database and diet intake calculator. Asia Pac. J. Clin. Nutr. 2012, 21, 201–208. [Google Scholar]
- Tony Ng, K.W., Jr. DietPLUS- a User-friendly ‘2 in 1’ food composition database and calculator of nutrient intakes. Malays. J. Nutr. 2010, 16, 125–130. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Boothroyd, R.I.; Fisher, E.B. Peers for progress: Promoting peer support for health around the world. Fam. Pract. 2010, 27 (Suppl. 1), i62–i68. [Google Scholar] [CrossRef]
- Van Dam, H.A.; van der Horst, F.G.; Knoops, L.; Ryckman, R.M.; Crebolder, H.F.; van den Borne, B.H. Social support in diabetes: A systematic review of controlled intervention studies. Patient Educ. Couns. 2005, 59, 1–12. [Google Scholar] [CrossRef]
- Aziz, Z.; Riddell, M.A.; Absetz, P.; Brand, M.; Oldenburg, B. Peer support to improve diabetes care: An implementation evaluation of the Australasian Peers for Progress Diabetes Program. BMC Public Health 2018, 18, 262. [Google Scholar] [CrossRef]
- Adams, K.; Paasse, G.; Clinch, D. Peer-support preferences and readiness-to-change behaviour for chronic disease prevention in an urban indigenous population. Aust. Soc. Work 2011, 64, 55–67. [Google Scholar] [CrossRef]
- Funnell, M.M. Peer-based behavioural strategies to improve chronic disease self-management and clinical outcomes: Evidence, logistics, evaluation considerations and needs for future research. Fam. Prac. 2010, 27 (Suppl. 1), i17–i22. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, M.J.; Perez, A.; Scanlan, A.B.; Alos, V.A.; Whitaker, R.C.; Foster, G.D.; Ackermann, R.T.; Ciolino, J.D.; Homko, C. PREVENT-DM comparative effectiveness trial of lifestyle intervention and metformin. Am. J. Prev. Med. 2017, 52, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Megson, M.; Wing, R.; Leahey, T.M. Effects of breakfast eating and eating frequency on body mass index and weight loss outcomes in adults enrolled in an obesity treatment program. J. Behav. Med. 2017, 40, 595–601. [Google Scholar] [CrossRef]
- Aschbrenner, K.A.; Mueser, K.T.; Naslund, J.A.; Gorin, A.A.; Kinney, A.; Daniels, L.; Bartels, S.J. Feasibility study of increasing social support to enhance a healthy lifestyle intervention for individuals with serious mental illness. J. Soc. Soc. Work Res. 2016, 7, 289–313. [Google Scholar] [CrossRef]
- Stuckey, M.I.; Gill, D.P.; Petrella, R.J. Does systolic blood pressure response to lifestyle intervention indicate metabolic risk and health-related quality-of-life improvement over 1 year? J. Clin. Hypertens. 2015, 17, 375–380. [Google Scholar] [CrossRef]
- Pérez-Escamilla, R.; Hromi-Fiedler, A.; Vega-López, S.; Bermúdez-Millán, A.; Segura-Pérez, S. Impact of peer nutrition education on dietary behaviors and health outcomes among Latinos: A systematic literature review. J. Nutr. Educ. Behav. 2008, 40, 208–225. [Google Scholar] [CrossRef]
- Kasje, W.N.; Denig, P.; Stewart, R.E.; de Graeff, P.A.; Haaijer-Ruskamp, F.M. An educational programme for peer review groups to improve treatment of chronic heart failure and diabetes mellitus type 2 in general practice. J. Eval. Clin. Pract. 2006, 12, 613–621. [Google Scholar] [CrossRef]
- Parry, M.; Watt-Watson, J. Peer support intervention trials for individuals with heart disease: A systematic review. Eur. J. Cardiovasc. Nurs. 2010, 9, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Greer, D.; Hill, D.C. Implementing an evidence-based metabolic syndrome prevention and treatment program utilizing group visits. J. Am. Acad. Nurse Pract. 2011, 23, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Ash, G.I.; Joiner, K.L.; Savoye, M.; Baker, J.S.; Gerosa, J.; Kleck, E.; Patel, N.S.; Sadler, L.S.; Stults-Kolehmainen, M.; Weinzimer, S.A.; et al. Feasibility and safety of a group physical activity program for youth with type 1 diabetes. Pediatr. Diabetes 2019, 20, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Cooper, K.; Schofield, P.; Smith, B.H.; Klien, S. PALS: Peer support for community dwelling older people with chronic low back pain: A feasibility and acceptability study. Physiotherapy 2020, 106, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Allen, C.; Vassilev, I.; Kennedy, A.; Rogers, A. Long-term condition self-management support in online communities: A meta-synthesis of qualitative papers. J. Med. Internet Res. 2016, 18, e61. [Google Scholar] [CrossRef] [PubMed]
- Gatenby, S.J.; Aaron, J.I.; Morton, G.M.; Mela, D.J. Nutritional implications of reduced-fat food use by free-living consumers. Appetite 1995, 25, 241–252. [Google Scholar] [CrossRef]
- Stubbs, R.J.; Mazlan, N.; Whygrow, S. Carbohydrates, Appetite and Feeding Behavior in Humans. J. Nutr. 2001, 131, 2775S–2781S. [Google Scholar] [CrossRef]

| Characteristics | All (N = 48) | PG1 (n = 14) | PG2 (n = 10) | PG3 (n = 15) | PG4 (n = 9) | p | |
|---|---|---|---|---|---|---|---|
| Age (Years) | Median (IQR) | 46 (11) | 43.5 (11) | 47 (6) | 44 (17) | 46 (7) | 0.563 |
| Gender | Female | 25 (52.1) | 6 (42.9) | 6 (60.0) | 6 (40.0) | 7 (77.8) | 0.292 |
| Male | 23 (47.9) | 8 (57.1) | 4 (40.0) | 9 (60.0) | 2 (22.2) | ||
| Ethnicity | Malay | 41 (85.4) | 12 (85.7) | 9 (90.0) | 13 (86.7) | 7 (77.8) | 0.515 |
| Chinese | 3 (6.3) | 1 (7.1) | 0 (0.0) | 2 (13.3) | 0 (0.0) | ||
| Indian | 4 (8.3) | 1 (7.1) | 1 (10.0) | 0 (0.0) | 2 (22.2) | ||
| Marital status | Single | 2 (4.2) | 1 (7.1) | 0 (0.0) | 1 (6.7) | 0 (0.0) | 0.967 |
| Married | 44 (91.7) | 13 (92.9) | 9 (90.0) | 13 (86.7) | 9 (100.0) | ||
| Widowed | 2 (4.2) | 0 (0.0) | 1 (10.0) | 1 (6.7) | 0 (0.0) | ||
| Education | Primary | 5 (10.4) | 1 (7.1) | 1 (10.0) | 1 (6.7) | 2 (22.2) | 0.658 |
| Lower secondary | 13 (27.1) | 2 (14.3) | 4 (40.0) | 3 (20.0) | 4 (44.4) | ||
| Upper secondary | 16 (33.3) | 6 (42.9) | 3 (30.0) | 5 (33.3) | 2 (22.2) | ||
| Tertiary | 14 (29.2) | 5 (35.7) | 2 (20.0) | 6 (40.0) | 1 (11.1) | ||
| Occupation | Working | 47 (97.9) | 13 (92.9) | 10 (100.0) | 15 (100.0) | 9 (100.0) | 0.687 |
| Not working | 1 (2.1) | 1 (7.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Baseline (M0) | Post-Intervention (M3) | Post-Follow-Up (M6) | pa | Pairwise Comparison | Change (%) | pb | |
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Energy (kcal) | 1685.42 (421.04) | 1613.82 (331.50) | 1453.24 (296.61) | 0.001 | M0 vs. M3 | −4.25 | 0.045 |
| M3 vs. M6 | −9.90 | 0.015 | |||||
| Carbohydrate (g/1000 kcal) | 139.71 (32.35) | 149.04 (42.91) | 165.19 (33.21) | 0.001 | M0 vs. M3 | −6.68 | 0.483 |
| M3 vs. M6 | 10.84 | 0.049 | |||||
| Protein (g/1000 kcal) | 32.91 (9.53) | 33.33 (14.54) | 39.93 (13.71) | 0.004 | M0 vs. M3 | −1.19 | 1.000 |
| M3 vs. M6 | +19.80 | 0.041 | |||||
| Fat (g/1000 kcal) | 29.03 (11.89) | 21.89 (12.44) | 22.96 (9.81) | 0.001 | M0 vs. M3 | −24.60 | <0.001 |
| M3 vs. M6 | +4.89 | 1.000 | |||||
| Total fiber c (g/1000 kcal) | 6.71 (2.05) | 6.95 (6.60) | 9.06 (3.41) | <0.001 | M0 vs. M3 | +3.58 | 0.508 |
| M3 vs. M6 | +30.36 | <0.001 | |||||
| Total sugar (g/1000 kcal) | 40.02 (18.64) | 32.05 (17.00) | 44.57 (20.42) | 0.001 | M0 vs. M3 | −24.87 | 0.056 |
| M3 vs. M6 | +39.06 | 0.002 | |||||
| Glycemic load (g/%) | 135.34 (30.05) | 157.54 (47.22) | 156.43 (44.16) | <0.001 | M0 vs. M3 | +14.93 | <0.001 |
| M3 vs. M6 | −0.70 | 1.000 |
| Baseline (M0) | Post-Intervention (M3) | Post Follow-Up (M6) | pa | Pairwise Comparison | Change (%) | pb | |
|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |||||
| SBP (mmHg) | 135.29 (19.65) | 130.50 (17.36) | 130.42 (18.36) | 0.001 | M0 vs. M3 | −3.54 | 0.001 |
| M3 vs. M6 | −0.06 | 1.000 | |||||
| DBP (mmHg) | 82.58 (11.67) | 81.00 (9.28) | 81.75 (9.67) | 0.566 | |||
| FBG (mmol/L) | 8.60 (3.48) | 7.57 (1.98) | 7.57 (2.16) | <0.001 | M0 vs. M3 | −11.98 | <0.001 |
| M3 vs. M6 | 0 | 1.000 | |||||
| BMI (kg/m2) | 25.84 (3.91) | 25.42 (3.93) | 25.50 (4.07) | 0.001 | M0 vs. M3 | −1.63 | <0.001 |
| M3 vs. M6 | +0.31 | 1.000 | |||||
| WC (cm) | 91.72 (11.53) | 91.07 (11.36) | 91.29 (11.43) | <0.001 | M0 vs. M3 | −0.71 | <0.001 |
| M3 vs. M6 | +0.24 | 0.018 | |||||
| BF (%) | 29.88 (6.57) | 29.42 (6.43) | 29.37 (6.36) | 0.060 | |||
| TG (mmol/L) | 2.89 (1.73) | 2.19 (2.06) | 2.19 (2.09) | <0.001 | M0 vs. M3 | −24.22 | <0.001 |
| M3 vs. M6 | 0 | 1.000 | |||||
| HDL (mmol/L) | 1.12 (0.35) | 1.41 (0.32) | 1.13 (0.33) | <0.001 | M0 vs. M3 | 25.89 | 0.001 |
| M3 vs. M6 | −19.86 | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahadzir, M.D.A.; Quek, K.F.; Ramadas, A. Nutrition and Lifestyle Behavior Peer Support Program for Adults with Metabolic Syndrome: Outcomes and Lessons Learned from a Feasibility Trial. Nutrients 2020, 12, 1091. https://doi.org/10.3390/nu12041091
Mahadzir MDA, Quek KF, Ramadas A. Nutrition and Lifestyle Behavior Peer Support Program for Adults with Metabolic Syndrome: Outcomes and Lessons Learned from a Feasibility Trial. Nutrients. 2020; 12(4):1091. https://doi.org/10.3390/nu12041091
Chicago/Turabian StyleMahadzir, Muhammad Daniel Azlan, Kia Fatt Quek, and Amutha Ramadas. 2020. "Nutrition and Lifestyle Behavior Peer Support Program for Adults with Metabolic Syndrome: Outcomes and Lessons Learned from a Feasibility Trial" Nutrients 12, no. 4: 1091. https://doi.org/10.3390/nu12041091
APA StyleMahadzir, M. D. A., Quek, K. F., & Ramadas, A. (2020). Nutrition and Lifestyle Behavior Peer Support Program for Adults with Metabolic Syndrome: Outcomes and Lessons Learned from a Feasibility Trial. Nutrients, 12(4), 1091. https://doi.org/10.3390/nu12041091






