Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging according to Sex and Age: EVA Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Ethics Approval and Consent to Participate
2.4. Variables and Measuring Instruments
2.4.1. Assessment of Carotid Intima-Media Thickness
2.4.2. The Ankle Arm Index
2.4.3. Assessment of Carotid-Femoral Pulse Wave Velocity (cfPWV)
2.4.4. Definition of Healthy Vascular Aging, Normal Vascular Aging and Early Vascular Aging
2.4.5. Adherence to the Mediterranean Diet
2.4.6. Evaluation of Lifestyles
2.4.7. Measurement of Cardiovascular Risk Factors
2.5. Statistical Analysis
3. Results
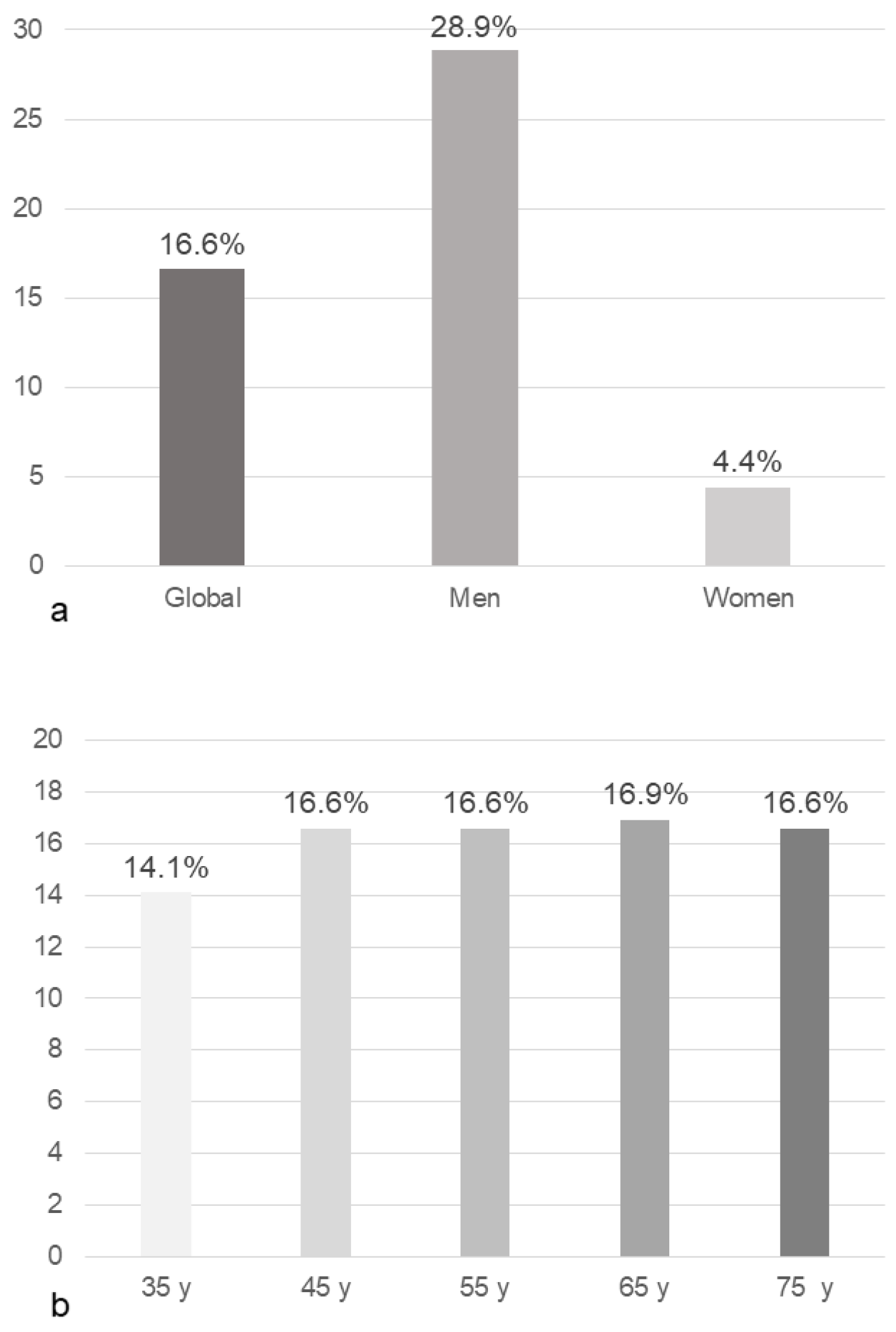
3.1. Clinical Characteristics and Vascular Aging
3.2. Adherence to the Mediterranean Diet and Its Components
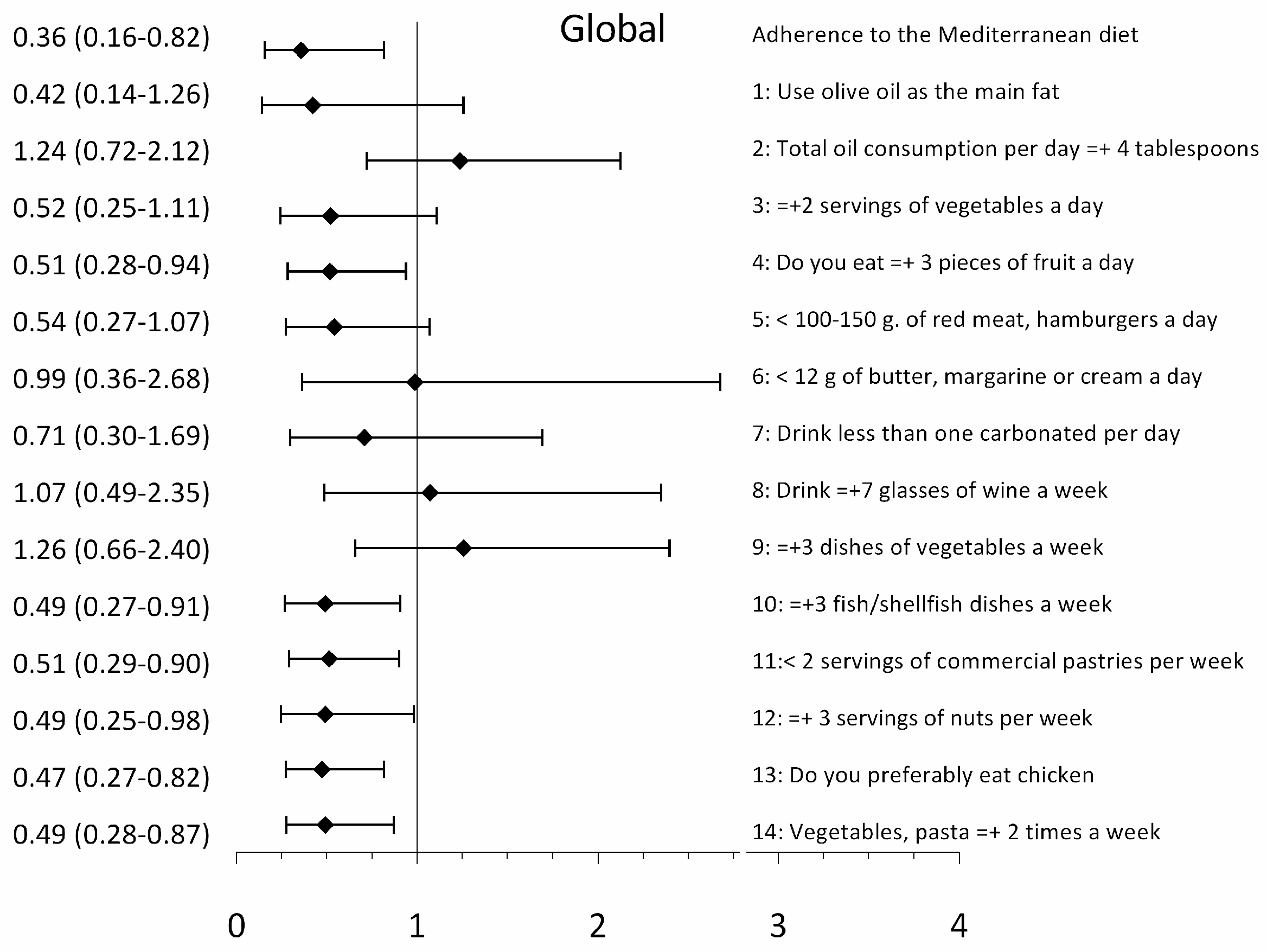
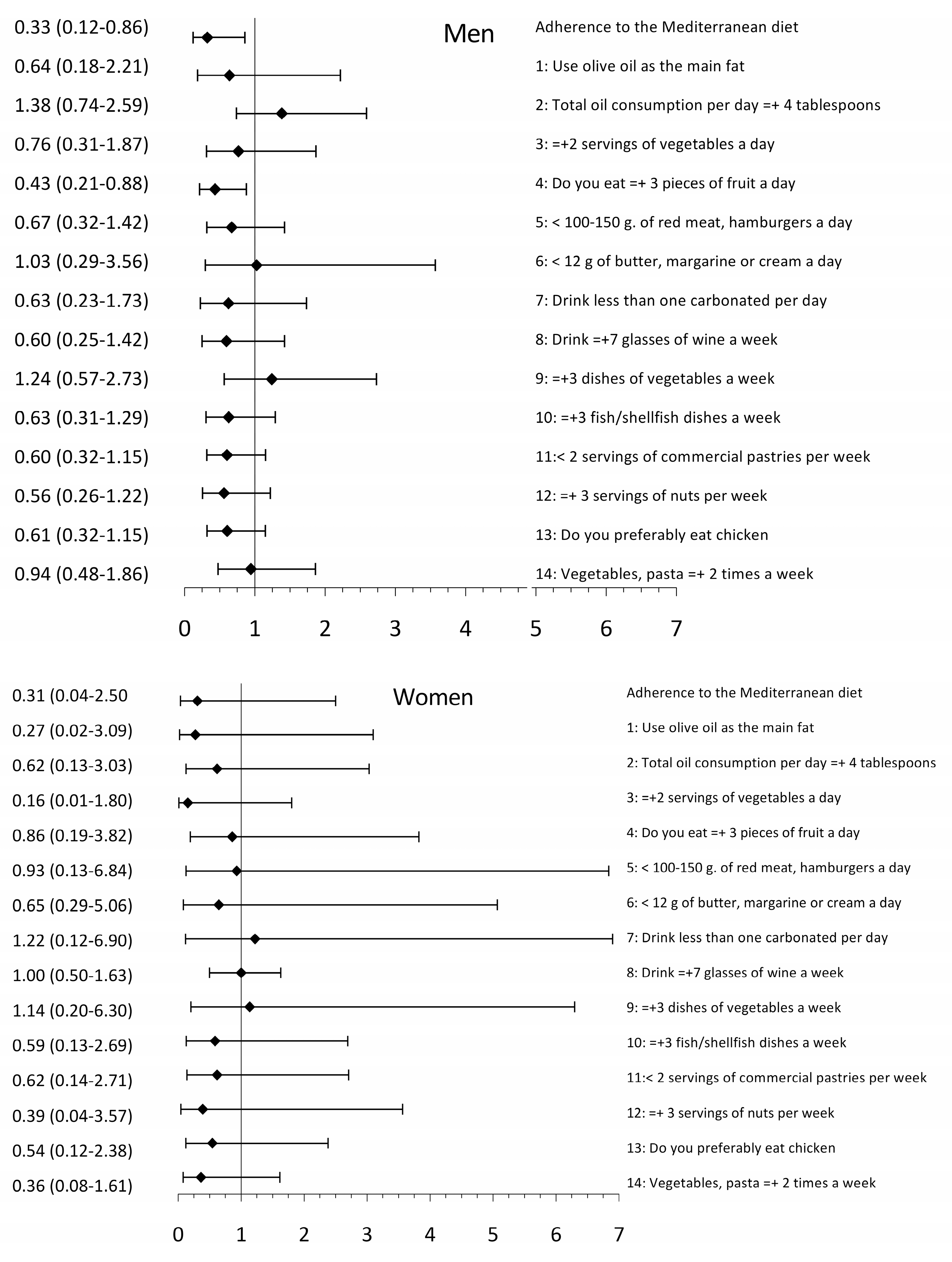
3.3. Association between EVA and Adherence to the Mediterranean Diet and Its Components
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Trichopoulou, A.; Martinez-Gonzalez, M.A.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 3, CD009825. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvado, J.; Covas, M.I.; Corella, D.; Aros, F.; Gomez-Gracia, E.; Ruiz-Gutierrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Serino, A.; Salazar, G. Protective Role of Polyphenols against Vascular Inflammation, Aging and Cardiovascular Disease. Nutrients 2018, 11, 53. [Google Scholar] [CrossRef] [PubMed]
- Cunha, P.G.; Boutouyrie, P.; Nilsson, P.M.; Laurent, S. Early Vascular Ageing (EVA): Definitions and Clinical Applicability. Curr. Hypertens. Rev. 2017, 13, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Cunha, P.G.; Cotter, J.; Oliveira, P.; Vila, I.; Boutouyrie, P.; Laurent, S.; Nilsson, P.M.; Scuteri, A.; Sousa, N. Pulse wave velocity distribution in a cohort study: From arterial stiffness to early vascular aging. J. Hypertens. 2015, 33, 1438–1445. [Google Scholar] [CrossRef]
- Botto, F.; Obregon, S.; Rubinstein, F.; Scuteri, A.; Nilsson, P.M.; Kotliar, C. Frequency of early vascular aging and associated risk factors among an adult population in Latin America: The OPTIMO study. J. Hum. Hypertens. 2018, 32, 219–227. [Google Scholar] [CrossRef]
- Laurent, S. Defining vascular aging and cardiovascular risk. J. Hypertens. 2012, 30, S3–S8. [Google Scholar] [CrossRef]
- Nilsson Wadstrom, B.; Fatehali, A.H.; Engstrom, G.; Nilsson, P.M. A Vascular Aging Index as Independent Predictor of Cardiovascular Events and Total Mortality in an Elderly Urban Population. Angiology 2019, 70, 929–937. [Google Scholar] [CrossRef]
- Gomez-Marcos, M.A.; Martinez-Salgado, C.; Gonzalez-Sarmiento, R.; Hernandez-Rivas, J.M.; Sanchez-Fernandez, P.L.; Recio-Rodriguez, J.I.; Rodriguez-Sanchez, E.; Garcia-Ortiz, L. Association between different risk factors and vascular accelerated ageing (EVA study): Study protocol for a cross-sectional, descriptive observational study. BMJ Open 2016, 6, e011031. [Google Scholar] [CrossRef]
- Gomez-Sanchez, M.; Patino-Alonso, M.C.; Gomez-Sanchez, L.; Recio-Rodriguez, J.I.; Rodriguez-Sanchez, E.; Maderuelo-Fernandez, J.A.; Garcia-Ortiz, L.; Gomez-Marcos, M.A. Reference values of arterial stiffness parameters and their association with cardiovascular risk factors in the Spanish population. The EVA Study. Rev. Esp. Cardiol. (Engl. Ed.) 2020, 73, 43–52. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [CrossRef]
- Gomez-Marcos, M.A.; Recio-Rodriguez, J.I.; Patino-Alonso, M.C.; Agudo-Conde, C.; Gomez-Sanchez, L.; Gomez-Sanchez, M.; Rodriguez-Sanchez, E.; Garcia-Ortiz, L. Protocol for measuring carotid intima-media thickness that best correlates with cardiovascular risk and target organ damage. Am. J. Hypertens. 2012, 25, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J. Hypertens. 2018, 36, 2284–2309. [Google Scholar] [CrossRef] [PubMed]
- Van Bortel, L.M.; Laurent, S.; Boutouyrie, P.; Chowienczyk, P.; Cruickshank, J.K.; De Backer, T.; Filipovsky, J.; Huybrechts, S.; Mattace-Raso, F.U.; Protogerou, A.D.; et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J. Hypertens. 2012, 30, 445–448. [Google Scholar] [CrossRef] [PubMed]
- Schroder, H.; Fito, M.; Estruch, R.; Martinez-Gonzalez, M.A.; Corella, D.; Salas-Salvado, J.; Lamuela-Raventos, R.; Ros, E.; Salaverria, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Marshall, A.L.; Miller, Y.D.; Burton, N.W.; Brown, W.J. Measuring total and domain-specific sitting: A study of reliability and validity. Med. Sci. Sports Exerc. 2010, 42, 1094–1102. [Google Scholar] [CrossRef]
- Caparello, G.; Galluccio, A.; Giordano, C.; Lofaro, D.; Barone, I.; Morelli, C.; Sisci, D.; Catalano, S.; Ando, S.; Bonofiglio, D. Adherence to the Mediterranean diet pattern among university staff: A cross-sectional web-based epidemiological study in Southern Italy. Int. J. Food Sci. Nutr. 2019, 1–12. [Google Scholar] [CrossRef]
- Jennings, A.; Berendsen, A.M.; de Groot, L.; Feskens, E.J.M.; Brzozowska, A.; Sicinska, E.; Pietruszka, B.; Meunier, N.; Caumon, E.; Malpuech-Brugere, C.; et al. Mediterranean-Style Diet Improves Systolic Blood Pressure and Arterial Stiffness in Older Adults. Hypertension 2019, 73, 578–586. [Google Scholar] [CrossRef]
- Davis, C.R.; Hodgson, J.M.; Woodman, R.; Bryan, J.; Wilson, C.; Murphy, K.J. A Mediterranean diet lowers blood pressure and improves endothelial function: Results from the MedLey randomized intervention trial. Am. J. Clin. Nutr. 2017, 105, 1305–1313. [Google Scholar] [CrossRef] [PubMed]
- Lahoz, C.; Castillo, E.; Mostaza, J.M.; de Dios, O.; Salinero-Fort, M.A.; Gonzalez-Alegre, T.; Garcia-Iglesias, F.; Estirado, E.; Laguna, F.; Sanchez, V.; et al. Relationship of the Adherence to a Mediterranean Diet and Its Main Components with CRP Levels in the Spanish Population. Nutrients 2018, 10, 379. [Google Scholar] [CrossRef] [PubMed]
- Casado-Diaz, A.; Dorado, G.; Quesada-Gomez, J.M. Influence of olive oil and its components on mesenchymal stem cell biology. World J. Stem Cells 2019, 11, 1045–1064. [Google Scholar] [CrossRef] [PubMed]
- Cesari, F.; Sofi, F.; Molino Lova, R.; Vannetti, F.; Pasquini, G.; Cecchi, F.; Marcucci, R.; Gori, A.M.; Macchi, C. Aging process, adherence to Mediterranean diet and nutritional status in a large cohort of nonagenarians: Effects on endothelial progenitor cells. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 84–90. [Google Scholar] [CrossRef]
- Bando, M.; Masumoto, S.; Kuroda, M.; Tsutsumi, R.; Sakaue, H. Effect of olive oil consumption on aging in a senescence-accelerated mice-prone 8 (SAMP8) model. J. Med. Investig. 2019, 66, 241–247. [Google Scholar] [CrossRef]
- van de Laar, R.J.; Stehouwer, C.D.; van Bussel, B.C.; Prins, M.H.; Twisk, J.W.; Ferreira, I. Adherence to a Mediterranean dietary pattern in early life is associated with lower arterial stiffness in adulthood: The Amsterdam Growth and Health Longitudinal Study. J. Intern. Med. 2013, 273, 79–93. [Google Scholar] [CrossRef]
| Global (501) | NVA (418) | EVA (83) | p Value | |
|---|---|---|---|---|
| Lifestyles | ||||
| Alcohol, (gr/W) | 46.12 ± 78.25 | 38.89 ± 70.38 | 82.53 ± 102.65 | <0.001 |
| Adequate alcohol use, n (%) | 451 (90) | 383 (92) | 68 (82) | 0.010 |
| Smoking index, year packages | 8.88 ± 17.52 | 8.42 ± 17.69 | 11.22 ± 16.53 | 0.009 |
| Smoking, n (%) | 90 (18) | 68 (14) | 22 (27) | 0.030 |
| Total physical activity, (METs/ min/week) | 2528 ± 1006 | 2439 ± 3260 | 2973 ± 3353 | 0.175 |
| Physically Active, n (%) | 414 (83) | 340 (81) | 74 (89) | 0.041 |
| Sedentary time, (h/ /week) | 42.15 ± 17.57 | 41.22 ± 17.85 | 46.85 ± 16.69 | 0.006 |
| Mediterranean diet | 7.15 ± 2.07 | 7.28 ± 2.05 | 6.49 ± 2.09 | 0.002 |
| Adherence to the MD, n (%) | 127 (25) | 115 (28) | 12 (15) | 0.013 |
| Conventional risk factors | ||||
| Age, (years) | 55.90 ± 14.24 | 55.59 ± 14.19 | 57.48 ± 14.44 | 0.270 |
| SBP, (mmHg) | 120.69 ± 3.13 | 118.85 ± 3.50 | 129.97 ± 18.65 | <0.001 |
| DBP, (mmHg) | 75.53 ± 10.10 | 74.50 ± 9.88 | 80.68 ± 9.64 | <0.001 |
| Hypertension, n (%) | 147 (29.34) | 108 (26) | 39 (47) | <0.001 |
| Antihypertensive drugs, n (%) | 96 (19) | 72 (17) | 24 (29) | <0.001 |
| Total cholesterol, (mg/dl) | 194.76 ± 32.50 | 193.69 ± 3.10 | 200.18 ± 28.81 | 0.096 |
| LDL-cholesterol, (mg/dl) | 115.51 ± 9.37 | 114.45 ± 9.89 | 120.85 ± 26.11 | 0.052 |
| HDL-cholesterol, (mg/dl) | 58.75 ± 16.16 | 59.58 ± 16.00 | 54.57 ± 16.41 | 0.010 |
| Triglycerides, (mg/dl) | 103.06 ± 53.19 | 98.18 ± 49.64 | 127.42 ± 63.13 | <0.001 |
| Atherogenic index | 3.54 ± 1.07 | 3.41 ± 1.04 | 3.93 ± 1.12 | <0.001 |
| Dyslipidaemia, n (%) | 191 (38) | 75 (18) | 19 (23) | 0.355 |
| Lipid–lowering drugs, n (%) | 102 (20) | 88 (21) | 14 (17) | 0.457 |
| Fasting plasma glucose, (mg/dl) | 88.21 ± 17.37 | 86.92 ± 14.73 | 94.70 ± 26.16 | <0.001 |
| HbA1c, (%) | 5.49 ± 0.56 | 5.44 ± 0.47 | 5.74 ± 0.83 | <0.001 |
| Diabetes mellitus, n (%) | 38 (8) | 23 (5) | 15 (18) | <0.001 |
| Hypoglycaemic drugs, n (%) | 35 (7) | 21 (5) | 14 (17) | 0.001 |
| Body mass index, (kg/m2) | 26.52 ± 4.23 | 26.26 ± 4.23 | 27.81 ± 3.99 | <0.001 |
| Obesity, n (%) | 94 (19) | 75 (18) | 19 (23) | <0.001 |
| Antiplatelet drugs, n (%) | 15 (19) | 10 (2) | 5 (5) | <0.041 |
| Vascular structure and function | ||||
| cfPWV, (m/s) | 6.53 ± 2.03 | 7.69 ± 2.00 | 10.76 ± 3.44 | <0.001 |
| cIMT | 0.68 ± 0.11 | 0.67 ± 0.11 | 0.73 ± 0.11 | <0.001 |
| NVA (418) | EVA (83) | p | |
|---|---|---|---|
| Adherence to the MD, n (%) | 115 (23) | 12 (2) | 0.013 |
| 1. Do you use olive oil as the principal source of fat for cooking? n (%) | 401 (96) | 77 (93) | 0.209 |
| 2. Does the total oil consumption per day ≥ 4 tablespoon? n (%) | 156 (37) | 37 (45) | 0.215 |
| 3. Do you eat ≥ 2 servings of vegetables a day? n (%) | 96 (23) | 10 (12) | 0.026 |
| 4. Do you eat ≥3 pieces of fruit a day (including natural juice)? n (%) | 185 (43) | 23 (28) | 0.005 |
| 5. Do you eat <100–150 g of red meat, hamburgers, sausages and a day? n (%) | 354 (85) | 63 (76) | 0.050 |
| 6. Do you eat <12 g of butter, margarine or cream a day? n (%) | 387 (93) | 77 (93) | 0.952 |
| 7. Do you drink less than one carbonated and/or sugary drink (soft drinks, colas, tonics, bitter) per day? n (%) | 382 (91) | 74 (89) | 0.512 |
| 8. Do you drink ≥ 7 glasses of wine (100 ml) a week? n (%) | 58 (14) | 26 (31) | 0.001 |
| 9 Do you consume ≥ 3 dishes of vegetables a week? (1 plate or serving of 150 g), n (%) | 74 (18) | 19 (23) | 0.267 |
| 10. Do you eat ≥ 3 fish-shellfish dishes a week? (1 piece, dish or portion: 100-150 g of fish or 4–5 pieces or 200 g of seafood), n (%) | 149 (36) | 23 (28) | 0.081 |
| 11. Do you consume <2 servings of commercial (non-homemade) pastries such as cookies, custards, sweets or cakes per week? n (%) | 197 (41) | 28 (34) | 0.025 |
| 12. Do you eat ≥ 3 servings of nuts per week? (serving = 30 g.), n (%) | 124 (30) | 14 (17) | 0.017 |
| 13. Do you preferably eat chicken, turkey or rabbit meat instead of beef, pork, hamburgers or sausages? (chicken meat: 1 piece or serving of 100-150 g), n (%) | 275 (66) | 41 (49) | 0.005 |
| 14. Do you eat cooked vegetables, pasta, rice, or other dishes seasoned with tomato, garlic, onion, or leek sauce cooked over low heat with olive oil (sofrito) ≥2 times a week? n (%) | 203 (49) | 27 (32) | 0.007 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez Sánchez, M.; Gómez Sánchez, L.; Patino-Alonso, M.C.; Alonso-Domínguez, R.; Sánchez-Aguadero, N.; Lugones-Sánchez, C.; Rodríguez Sánchez, E.; García Ortiz, L.; Gómez-Marcos, M.A. Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging according to Sex and Age: EVA Study. Nutrients 2020, 12, 1025. https://doi.org/10.3390/nu12041025
Gómez Sánchez M, Gómez Sánchez L, Patino-Alonso MC, Alonso-Domínguez R, Sánchez-Aguadero N, Lugones-Sánchez C, Rodríguez Sánchez E, García Ortiz L, Gómez-Marcos MA. Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging according to Sex and Age: EVA Study. Nutrients. 2020; 12(4):1025. https://doi.org/10.3390/nu12041025
Chicago/Turabian StyleGómez Sánchez, Marta, Leticia Gómez Sánchez, Maria C Patino-Alonso, Rosario Alonso-Domínguez, Natalia Sánchez-Aguadero, Cristina Lugones-Sánchez, Emiliano Rodríguez Sánchez, Luis García Ortiz, and Manuel A Gómez-Marcos. 2020. "Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging according to Sex and Age: EVA Study" Nutrients 12, no. 4: 1025. https://doi.org/10.3390/nu12041025
APA StyleGómez Sánchez, M., Gómez Sánchez, L., Patino-Alonso, M. C., Alonso-Domínguez, R., Sánchez-Aguadero, N., Lugones-Sánchez, C., Rodríguez Sánchez, E., García Ortiz, L., & Gómez-Marcos, M. A. (2020). Adherence to the Mediterranean Diet in Spanish Population and Its Relationship with Early Vascular Aging according to Sex and Age: EVA Study. Nutrients, 12(4), 1025. https://doi.org/10.3390/nu12041025







