1. Introduction
In developed countries, the increasing number of overweight and obese people is a major public health concern [
1], and dietary choices are viewed as a key factor in influencing the global burden of non-communicable diseases also known as chronic diseases [
2,
3]. The choice of diets that are not in keeping with dietary guidance is associated with various comorbidities such as type 2 diabetes, cardiovascular diseases and cancer [
4]. In addition, to the individual consequences of an unhealthy diet, its impact on the healthcare system is politically relevant. The annual direct costs of obesity in Germany amount for approximately €29.39 billion and the indirect costs (e.g., lower productivity, long-term nursing care and pain) to an additional €33.65 billion [
5]. A total of 102,000 subjects die prematurely each year because of obesity, and there is a significant excess of unemployment, long-term nursing care, pain and suffering due to obesity [
5]. From a lifetime perspective, every obese man is equal to an additional burden of €166,911 and each woman of €206,526 for total healthcare costs [
5]. From a more comprehensive perspective, the global economic costs caused by obesity account for 2.3% of the worlds’ gross domestic product which equals US
$2 trillion [
6].
To overcome this economic burden, it is necessary that overweight and obese citizens change their diet. Changing eating behaviour is a slow and long-lasting process [
7] and a significant challenge for most people. In recent years, several countries have adopted policy interventions to support a healthy diet of their citizens. These interventions can range from providing information to instruments with a greater level of intervention, e.g., taxes on unhealthy foods, bans of advertisement targeted at children (for a detailed explanation of the different policy instruments see
Table 1). Over the past few years, the debate on such policy instruments has gained international importance, as a result of increased efforts of the World Health Organization (WHO) [
8,
9,
10]. For example, some European countries have introduced health-related (“fat”) taxes. In 2011, Denmark was the first country to introduce a tax on saturated fatty acids [
11]. The UK established a tax on sugar-sweetened beverages in April 2018. The extra revenue is used for healthier school meals and improvements in physical education in schools. Research shows that the introduced tax in the UK was an incentive for companies to reduce the sugar content of their sugar-sweetened beverages and that it led to a reduction in sales volume of these drinks [
12]. This shows that such health taxes are effective as companies reduced the sugar content in their soft drinks and, at the same time, consumers bought less of them. However, such taxes are often highly controversial. For example, the tax on saturated fatty acids in Denmark was abolished again in January 2012, after a change of government. However, the importance of a suitable policy mix for a healthy diet is increasingly recognised in the literature [
9,
13,
14,
15].
With regard to such health-related taxes or other food-related interventions, the state is reluctant in Germany as such policy interventions in the field of personal diets might be very unpopular. For example, in the 2013 election campaign, the demand for an obligatory veggie day per week (meat-free day in canteens) was perceived as a public relations disaster for the Green party, which has deterred many other politicians from proposing health-oriented interventions. Nevertheless, discussions about policy instruments, which go beyond simple health information have intensified in recent times [
8]. However, some politicians and many companies have highly contested these instruments [
16,
17], drawing the picture of a nanny state. The results of an international comparison show great differences in terms of political intervention in the diet of consumers [
18]. In respective rankings, Germany is among the countries with particularly few nutrition policy interventions, whereas many Scandinavian countries go much further [
18,
19].
Research about consumer acceptance of various different nutrition policy interventions within one study is scarce in Germany. Reisch et al. [
20] focused on consumers’ preference for different nudges towards law and policy, most of them were designed to promote health, safety and clean energy. Their major finding was that consumers reject nudges that take their money without asking them, although the underlying reason for the nudge is attractive [
20]. The review by Niebylski et al. [
21] analysed healthy food subsidies and unhealthy food taxation. As a conclusion, they recommended the implementation and evaluation of healthy food subsidies and unhealthy food taxation. A tax on unhealthy food which results in a 20% price increase reduces unhealthy eating behaviour [
22]. One review examined the acceptability of government interventions to change health-related behaviours [
23]. The results show that the greatest public acceptability of government interventions is given for the least intrusive interventions that are often the least effective. Eykelenboom et al. [
24] recommend four strategies to increase public acceptability of a sugar-sweetened beverage tax. First, communicate the differences between the general belief and the scientific evidence of such a tax. Second, use the additional revenue for health initiatives. Third, tell the purpose of the tax to the consumer in a transparent way and fourth, give political priority to the problem of policy adoption and implementation [
24]. Moreover, interventions that do not affect one’s own behaviour are more accepted than interventions that target it [
23].
In consumer research, many indications denote that attitudes influence behaviour, and vice versa [
25,
26]. In this direction, according to the current literature, the issue of whether the acceptance of health-oriented governmental interventions is related to one’s own struggle to eat healthily has not been investigated. As it is difficult for consumers to change their own eating behaviour [
7] some of them might require support e.g., through policy interventions. There are some indications that one’s own eating habits may influence attitudes towards nutrition policies [
27].
Thus, the main objective of this study is to explore the relationship between the general acceptance of policy interventions and the individual efforts to achieve a healthy diet. To this end, a principal component- and a cluster analysis were performed with the example of German consumers to identify different consumer segments and their attitude towards specific policy instruments.
4. Results
4.1. Sample Description
The sample consisted of 1035 German citizens. The quota setting for gender, age, education and region worked in a manner that effectively mimics these characteristics of the German population (
Table 2).
On average 63.4% of respondents agree with the general statements about nutrition policy interventions by the government (
Appendix A,
Table A1). However, the query of specific examples of policy instruments shows lower acceptance levels. The average acceptance rate of all instruments amounts to 50.9% (
Appendix A,
Table A2). Accordingly, the rejection of nutrition policy instruments increases when specific examples are given (general statements: 11.2% and specific nutrition policy instruments: 29.6%) (
Appendix A,
Table A1 and
Table A2).
4.2. Results of the Principal Component Analysis
The PCA revealed two factors (
Table 3). The KMO of 0.847 is acceptable [
69], and the Cronbach’s alpha value denotes that the items are reliably measured within one factor [
66]. Factor 1 that is named “general support of nutrition policy interventions” has a Cronbach’s alpha value of 0.860. The second factor is called “perceived struggle to eat healthily”.
The values of the extracted factors were used in the subsequent cluster analysis as cluster-building variables.
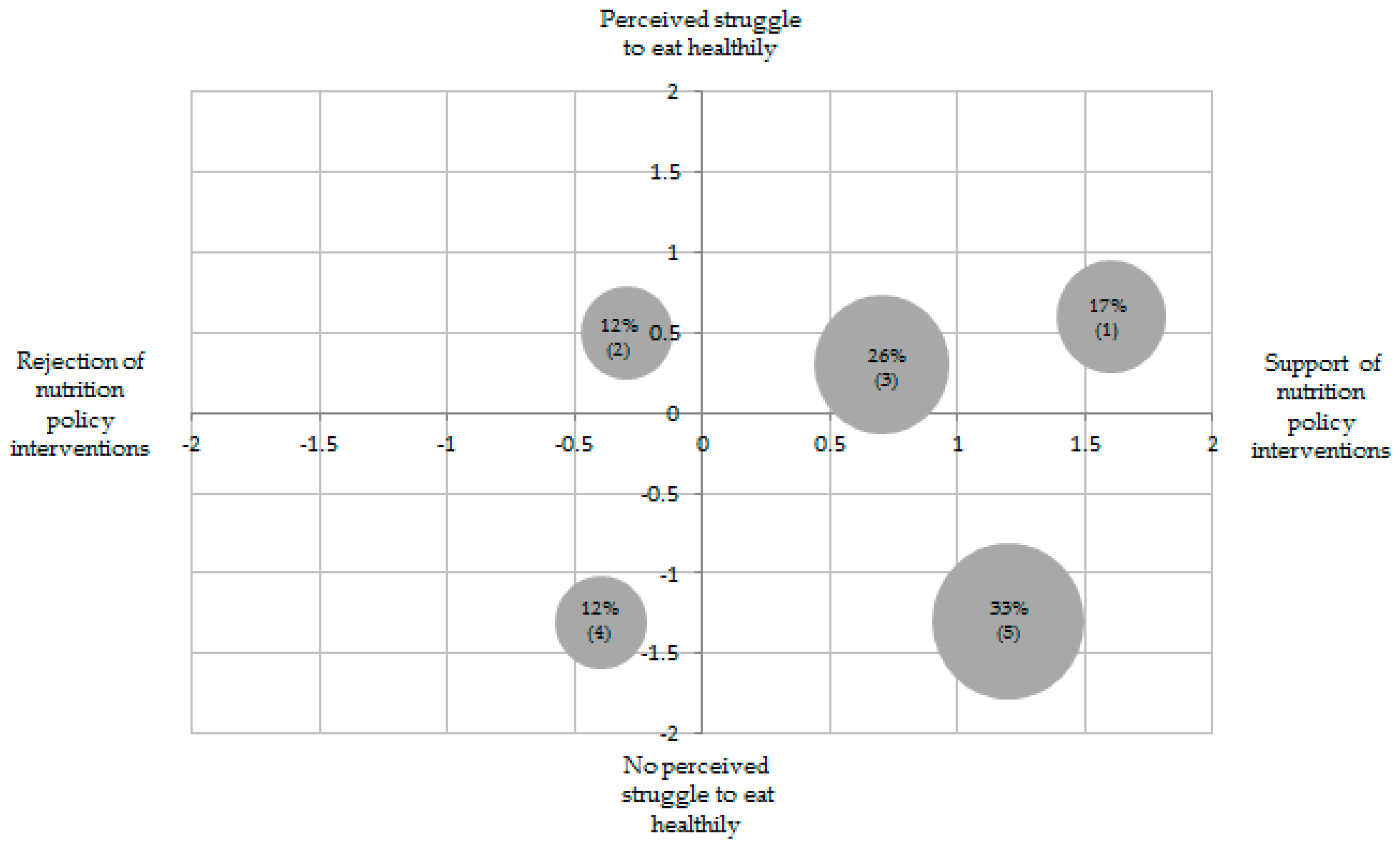
4.3. Results of the Cluster Analysis
The cluster analysis based on the two factors described above resulted in five consumer segments. The first group consisted of 17.3%, the second of 12.3%, the third of 25.5%, the fourth of 12.1% and the fifth of 32.8% of the sample. The discriminant function indicated that 97.3% of the cases were classified correctly.
Table 4 visualises the mean values of the items included in the two factors. Compared to the factor means, the mean values of the items are better for interpretation, as the direction of agreement or disagreement can be observed directly.
Cluster 1 demonstrates the strongest support of nutrition policy interventions. This cluster struggles to eat healthily. Compared to the other clusters, cluster 1 has the greatest struggle to eat healthily.
Cluster 3 slightly supports nutrition policy interventions. Its support is weaker than from clusters 1 and 5. Cluster 3 marginally struggles to eat healthily.
Cluster 5 supports nutrition policy interventions, the second strongest after cluster 1. However, cluster 5 does not struggle to eat healthily compared to cluster 1.
Two other smaller groups (namely, 2 and 4, make up a total of 24% of the respondents) are slightly opposed to nutrition policy interventions. On the one hand, cluster 2 includes respondents who struggle to eat healthily. On the other hand, cluster 4 comprises respondents who do not struggle to eat healthily.
Cluster 2 rejects nutrition policy interventions. The rejection is the second strongest among all clusters. The rejection is somewhat lower than that of cluster 4. Similar to cluster 1, cluster 2 struggles to eat a healthy diet. However, cluster 2’s struggle to eat healthily is somewhat smaller than that of cluster 1.
Cluster 4 rejects nutrition policy interventions. Its rejection is the strongest in comparison to the other four clusters. Furthermore, cluster 4 has no perceived struggle to eat healthily. Clusters 4 and 5 identically do not struggle to eat healthily.
Based on the above differences, the clusters are labelled as follows: “Help-seeking advocates” (1), “health-unconscious rejecters” (2), “differentiating supporters” (3), “health-conscious rejecters” (4) and “health-conscious advocates” (5). Furthermore, the authors analysed if the five clusters differ in their acceptance of specific nutrition policy instruments by conducting an ANOVA (
Table 5). The specific nutrition policy instruments are used as cluster-descriptive variables.
The help-seeking advocates (1) have the highest acceptance for the coloured traffic-light marking on the front of food packaging, followed by setting product limits and the lowest acceptance for a tax on foods with a high content of sugar, fat or salt without compensation. Notably, help-seeking advocates express higher support for setting product limits than imposing a ban on marketing to children.
The health-unconscious rejecters (2) only support the coloured traffic-light marking on the front of food packaging. They reject all other specific nutrition policy instruments. They demonstrate the weakest rejection for setting product limits. At the same time, this intervention is the most intrusive in this study. Furthermore, the health-unconscious rejecters (2) refuse nutrition policy instruments that include a tax with compensation to roughly the same extent. However, they most strongly reject a tax without compensation.
The differentiating supporters (3) reveal a high approval for the coloured traffic-light marking on the front of food packaging. They show a lower acceptance for setting product limits. The evaluation of the other specific nutrition instruments is indifferent (i.e., they neither support nor reject these nutrition instruments). The differentiating supporters (3) only clearly reject the tax without compensation.
The health-conscious rejecters (4) only support the coloured traffic-light marking on the front of food packaging. They most strongly reject a tax that is used to improve healthcare. Somewhat less strongly, they refuse a tax without compensation. Their rejection of the remaining specific policy instruments is moderately strong.
The health-conscious advocates (5) most strongly support the coloured traffic-light marking on the front of food packaging. They express the second highest support for setting product limits. Their support for other specific policy instruments is moderate. Their lowest level of support is for a tax without compensation.
Overall, all clusters show the highest acceptance values for a coloured traffic-light marking on the front of packaging. Four out of five clusters demonstrate the lowest acceptance or highest rejection of a tax on foods with a high content of sugar, fat or salt without compensation. Additionally, this is the only instrument that the entire sample rejects.
Descriptive statistics indicate that the clusters significantly differ in some sociodemographic characteristics (
Table 6).
The cluster of differentiating supporters (3) consists of the youngest consumers, with an average age of 45.1 years, whereas the cluster of health-conscious advocates (5) represents the oldest consumers, with an average age of 53.1 years. In terms of education, health-conscious rejecters (4) on average have the highest educational background. In this context, the cluster of health-conscious rejecters (4) has the highest amount of consumers with an income above €4500. At the same time, this cluster includes the lowest number of individuals with a salary below €1300.
5. Discussion
The study results show that the majority of the German population is open to nutritional policy interventions by the state. Of the German consumers, 63.4% support nutrition policy in general, 11.2% have a negative attitude and 25.4% are indifferent (
Appendix A Table A1). These findings are in line with the literature [
42,
70,
71]. The assessment of concrete instruments gives a more complex picture and shows approval ratings of between 34.2% and 78.7% depending on the instrument (50.9% on the average of all instruments,
Appendix A Table A2). This might be a consequence of the fact that the personal impact of a policy measure influences the evaluation of the instrument.
In the present study one’s perceived own struggle for a healthy diet has been analysed with regard to the hypothesis of a connection between personal vulnerability and the acceptance of nutritional policy measures. Overall the results depict that the extent of support for food policy instruments is not linearly related to one’s perceived own struggle for a healthy diet. The cluster analysis identifies both consumer groups who are themselves struggling for a healthy diet as supporter (or rejecter) of nutrition policy interventions, as well as consumers who do not have any difficulties themselves. In fact, only a minority of the population (size of cluster 2 and 4) clearly rejects nutrition policy interventions, whereas most of the population (size of cluster 1, 3 and 5) is more or less open-minded.
The results of the present study, which illustrates that consumers agree to nutrition policy instruments unrelated of their own efforts for a healthy diet, partly differ from previous literature. A past study has revealed that the acceptance of nutrition policy measures is higher among people who eat unhealthily than among individuals who eat healthily [
31]. However, the current study focuses on the personal struggle for a healthy diet, not on the individual eating behaviour as an outcome of the personal efforts.
Figure 1 visualises the non-linear results of the present study in a two-dimensional matrix.
The idea that nutrition policy interventions are not solely aimed at one target group is important to recognise. According to the present study results, German citizens may be divided into five target audiences with different policy intervention preferences. Thus, target group specific political communication strategies (i.e., the different segments should be targeted separately with individual communication strategies) are advised [
72]. For example, a communication campaign targeting health-unconscious rejecters (2) should explain how policy interventions might help them to follow a healthier diet. They could take the given health information into account which might help them to shift their food purchase towards a healthier choice.
Overall, our results reveal a relatively positive attitude towards the acceptance of nutrition policy instruments in Germany. As expected, information tools are more readily accepted than taxes or bans [
23]. All five clusters support traffic-light labelling on the front of packaging. This finding is consistent with earlier research [
37]. It leads to the following clear conclusion that politicians can be confident to introduce e.g., the traffic-light label as a mandatory label on food packaging.
In contrast to our results, Effertz [
31] argued that both, taxes with and without compensation are more likely to be rejected by the population. The current results reveal that consumers accept food taxes on unhealthy products when combined with a tax reduction for healthy products. Thus, food taxes including compensation are favourable. A clear communication on which products would be affected by a higher price due to a tax increase and which product prices would in turn decrease due to a tax reduction is recommended. Only if the consumers have this knowledge they might be able to adapt their behaviour accordingly and to understand the mechanism behind the tax introduction.
Other studies revealed that a ban on marketing targeted at children is the instrument that the population is most likely to support [
23,
31]. On the one hand, this finding is consistent with Effertz [
31] as about 2/3 of his and our sample accept a ban on marketing addressed to children. On the other hand, Effertz [
31] result is inconsistent with our results, as in the present study the traffic-light labelling exhibits a higher support than the ban targeted at children. Overall, a ban on marketing to children depicts high acceptance rates. Since it has been shown in several studies that a ban is supported by a large part of the population [
23,
31]. Politicians could take a closer look at this measure and use marketing restrictions to children as a tool to protect children in particular from a too strong influence through marketing. Further considerations in this regard could also include social media marketing.
The complex results achieved here could be explained from an economic, sociological or psychological perspective. Neo-classical economic theory [
73] maintains that consumers behave according to their own preferences and reject any restrictions of their own choices [
74] which is not the case in the present study. Especially cluster 1 seeks governmental support. From a neoclassical viewpoint, consumers also have a desire to maximise their utilities (own preferences). Therefore, one would expect consumers who follow these principles to evaluate the interventions according to whether or not they benefit financially from them. A fat tax makes unhealthy eating behaviour more expensive and healthy eating behaviour cheaper. According to this hypothesis, consumers with an unhealthy behaviour (i.e., cluster 1, 2, 3) should be against health taxes whereas consumers with a healthy behaviour should support them. In fact, health-unconscious rejecters (2) and health-conscious advocates (5) behave exactly as expected from neo-classical economic theory, while the health-conscious rejecters (4), differentiating supporters (3), and help-seeking advocates (1) do not behave according to this economic hypothesis. Without changing their current behaviour, health-unconscious rejecters (2) struggle to eat healthily, which is why a tax on unhealthy food would lead to higher expenses for them while the health-conscious advocates (5) would benefit financially as healthy food gets cheaper. Help-seeking advocates (1) highly accept interventions but struggle to follow a healthy diet. As members of this cluster follow an unhealthy diet, a rejection of interventions would have been expected because a health tax would affect this cluster financially—at least if they do not fundamentally change their eating behaviour.
One option to convince health-unconscious rejecters (2) of policy interventions is to communicate personal benefits of healthy behaviour. For example, if health-unconscious rejecters (2) will lose weight, they will save money in the future due to lower healthcare costs caused by their current overweight. Research shows that political interventions can change consumer behaviour [
75,
76]. Sharma et al. [
77] estimated through panel data that a 20% price increase of sugar-sweetened beverages would lead to a reduction of consumption which results in a lower calorie intake of 10,000 kj per year. This is equivalent to 0.93 kg body weight at an average cost per household of €17. Furthermore, in countries such as Germany where health insurance is compulsorily deducted from income [
78], economic costs are another factor. Consumers who follow a healthy diet should be interested in the fact that the remaining consumers eat healthily as well, so that they do not have to co-finance their healthcare costs. This aspect might additionally explain the high acceptance of political interventions by the health-conscious advocates (5). However, the explanations from an economical viewpoint depict that not all clusters can be explained accordingly and that other perspectives have to be taken into account.
A sociological perspective may also contribute to the explanation of the results. Thus, a slim appearance can be interpreted as a characteristic of social differentiation [
61]. A healthy, slim appearance tends to be associated with social success, whereas weight problems are perceived as a lower-class problem [
79]. Previous research indicated that higher-quality diets including regular fruit and vegetable intake are more often consumed by better-educated people [
61,
62,
80]. According to the sociological construct of conspicuous consumption [
81], upper-class citizens are interested in keeping such differences (e.g., the image of poor and fat). Therefore, they might be rather reluctant in advocating nutrition interventions. The health-conscious rejecters (4) and the health-conscious advocates (5) are the best-educated consumer segments (see
Table 6). Thereby, it is expected that both reject policy interventions to keep appearance differences (slim versus fat) of social classes. However, the results show that only the health-conscious rejecters (4) judge policy interventions negatively and behave as expected from a conspicuous consumption perspective. Against the background that studies reveal different class patterns in the food consumption of healthy and unhealthy products [
61], the persistent tendency of class-specific eating habits [
79] may prevent the acceptance of food policy interventions at least for this cluster.
From a psychological viewpoint, reactance effects [
82] can play a crucial role. Psychological reactance is a complex defensive reaction that can be understood as resistance to external or internal restrictions. Reactance is usually triggered by psychological pressure or the restriction of freedom [
82]. Reactance as an acceptance barrier would result in the fact that the more health-conscious a cluster is, the higher the acceptance of policy interventions. In this context, the help-seeking advocates (1) do not behave as expected as they highly accept policy interventions, although they struggle to follow a healthy diet and thereby would experience restrictions of their own behaviour. In contrast, the attitude of cluster 2 could perhaps be explained by reactance.
Another explanation from a psychological viewpoint could be that the individual motivation [
83] to change one’s habitual behaviour to follow a healthier diet is important. Therefore, the help-seeking advocates (1) may lack motivation of their own and need motivation and/or restrictions by a third party to be able to change their eating behaviour. One possible reason why consumers need support is self-commitment [
84]. One reason for this could be that consumers are unable to resist the temptations of an obesogenic environment and realise their own weaknesses.
Moreover, the effect of short-term versus long-term preferences could help to explain consumers’ attitude towards nutrition policy instruments. Consumers who are aware of their short-term weaknesses should strive for self-commitment by supporting nutrition policy interventions, i.e., a healthy nutrition environment, and vice versa. The health-conscious rejecters (4) and health-unconscious rejecters (2) may exhibit a rejection due to the underestimation of the long-term consequences of an unbalanced diet. When these segments would be more aware of the future benefits (e.g., lower risk for developing type 2 diabetes, cardiovascular diseases or cancer), their members might rethink their behaviour and support policy interventions. One way to increase acceptability would be to target the health-unconscious rejecters (2) by a communication strategy which explains them that in the short-term the tax might increase their food expenditure but in the long run they could benefit. If they change their diet, they will not experience higher food expenses and they will safe health-care expenditure due to no occurrence of comorbidities related to obesity. Thus, in the long-term, they will benefit both, from a financial and health-related point of view. Communication between politicians and consumers is crucial. Only if consumers understand that these health taxes are introduced for their own benefit and not for the state to raise money, there is a chance for a change in their opinion about nutrition policy interventions.
One limitation of this research is that nutritional problems were only recorded on the basis of self-declarations about the own struggle to follow a healthy diet, the nutritional status was not measured. Similarly, the stated preferences may be biased by social desirability effects. A third limitation is that the second factor consists of only one item; therefore, the perceived own struggle to eat healthily needs to be better understood in a further study. One option would be to measure the actual health status, e.g., the body mass index.