Influence of Alcohol and Red Meat Consumption on Life Expectancy: Results of 164 Countries from 1992 to 2013
Abstract
:1. Research in Context
1.1. Evidence before This Study
1.2. Added Value of This Study
1.3. Policy Implication
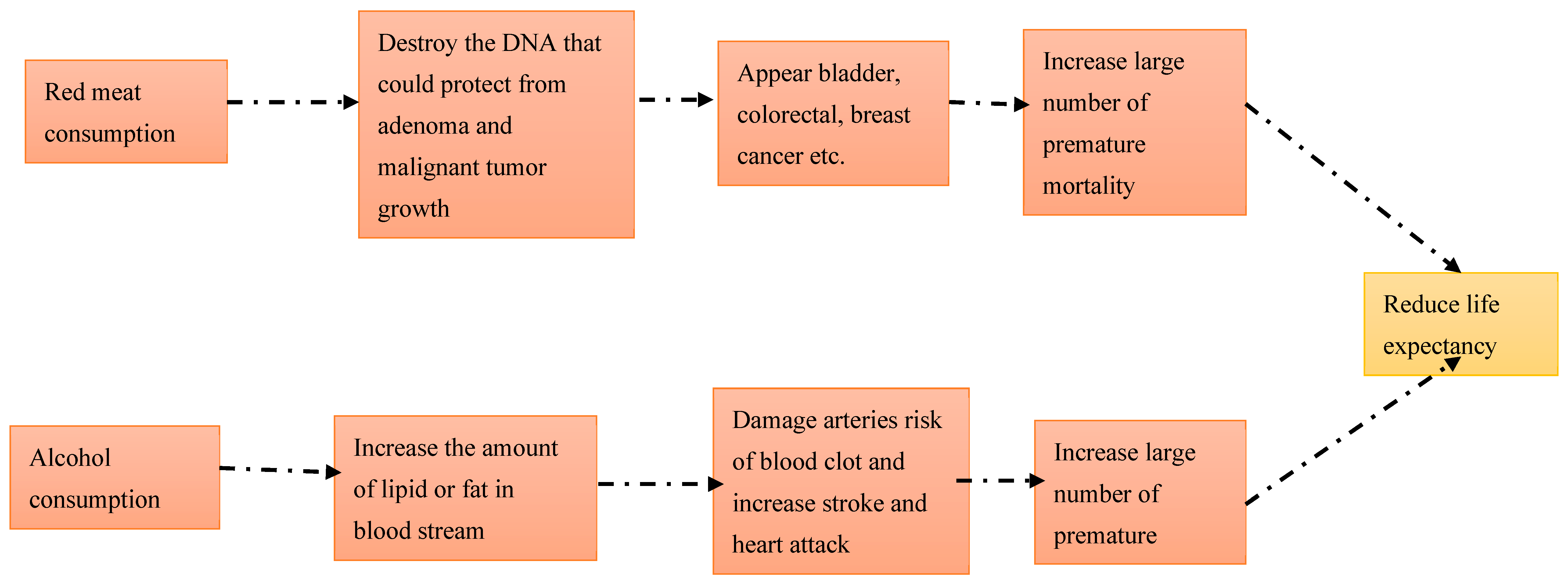
2. Introduction
3. Methods
3.1. Study Design
3.2. Source of Data
3.3. Variables
3.4. Measurement of Variables
lnCalorieit + β4 × lnAlcoholit + β5 × lnGNIit + Eit
3.5. Statistical Analysis
4. Results
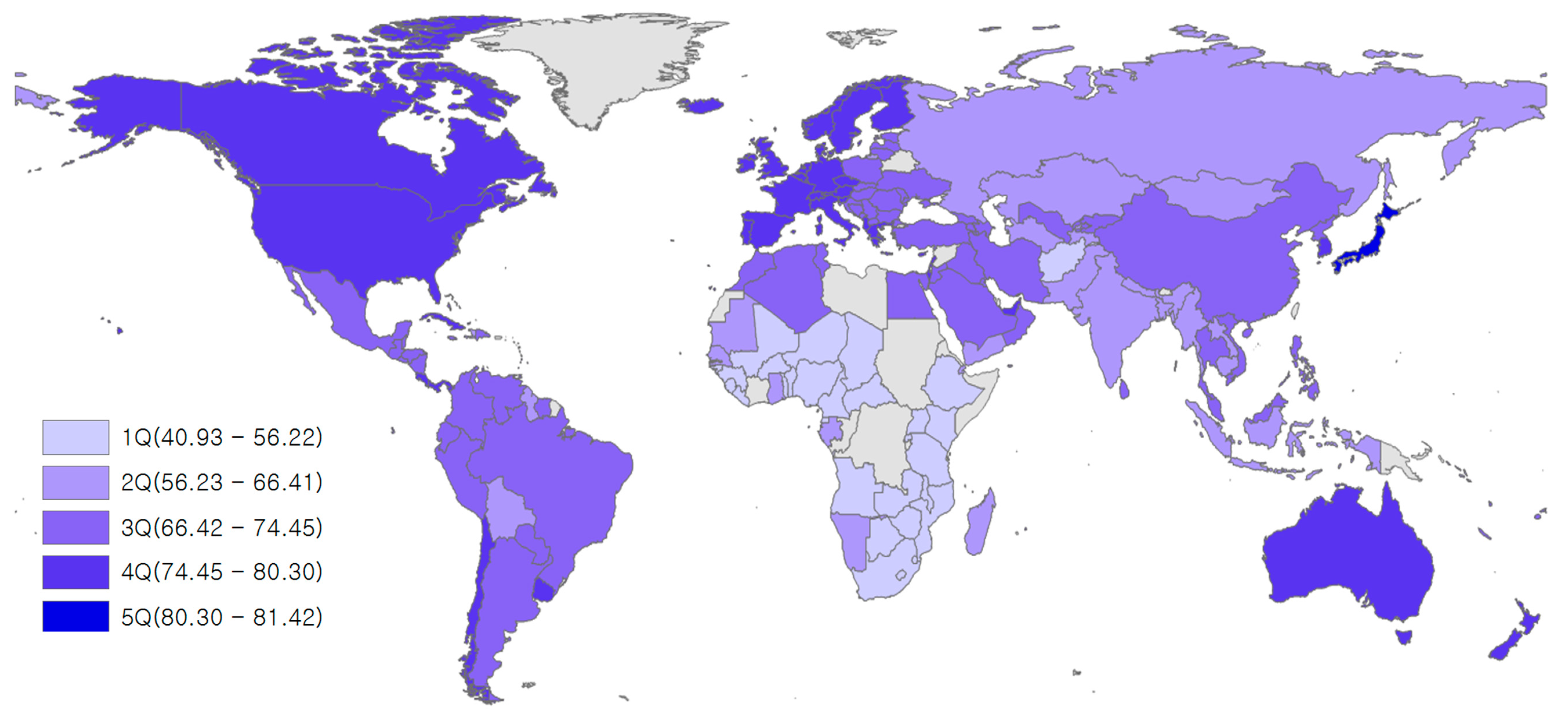
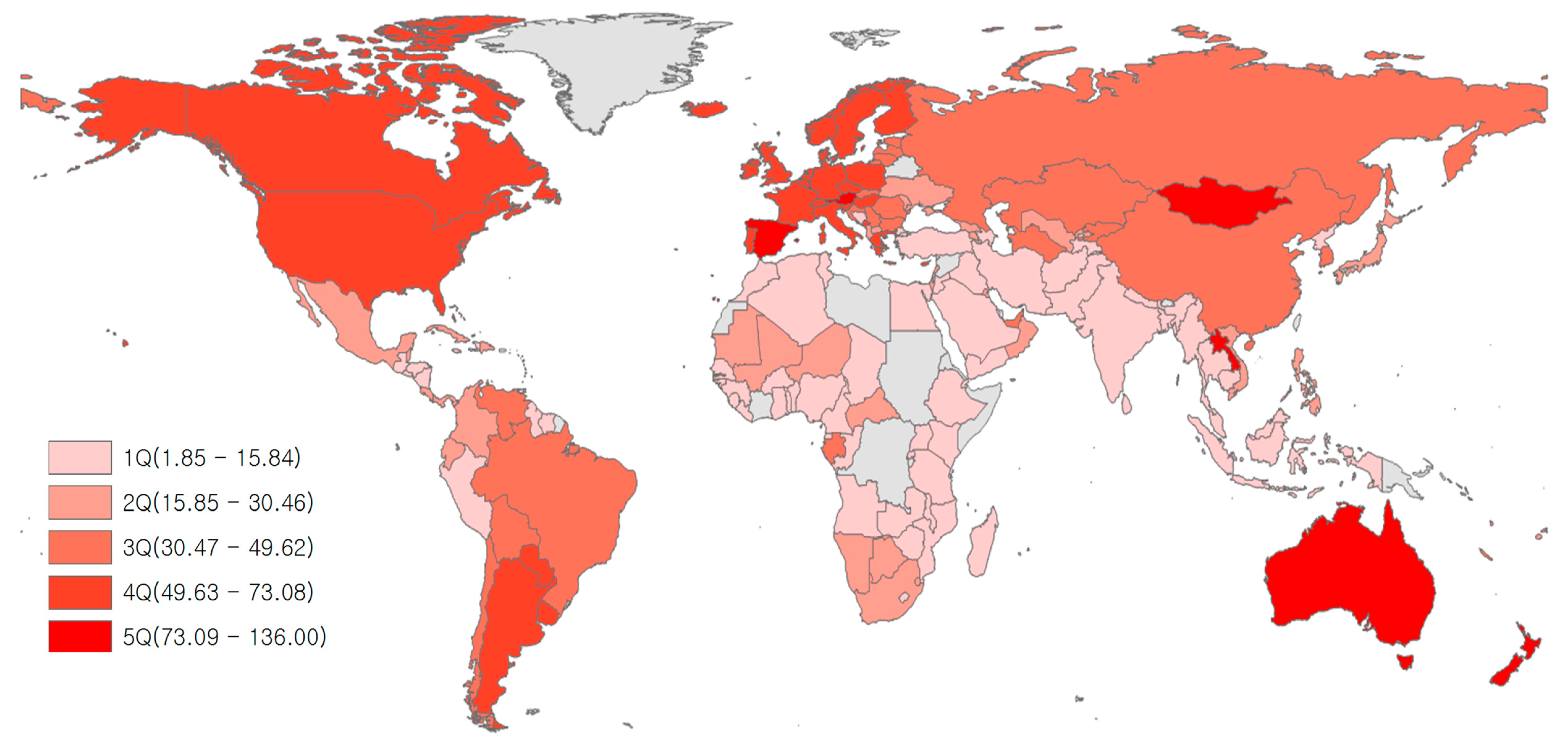
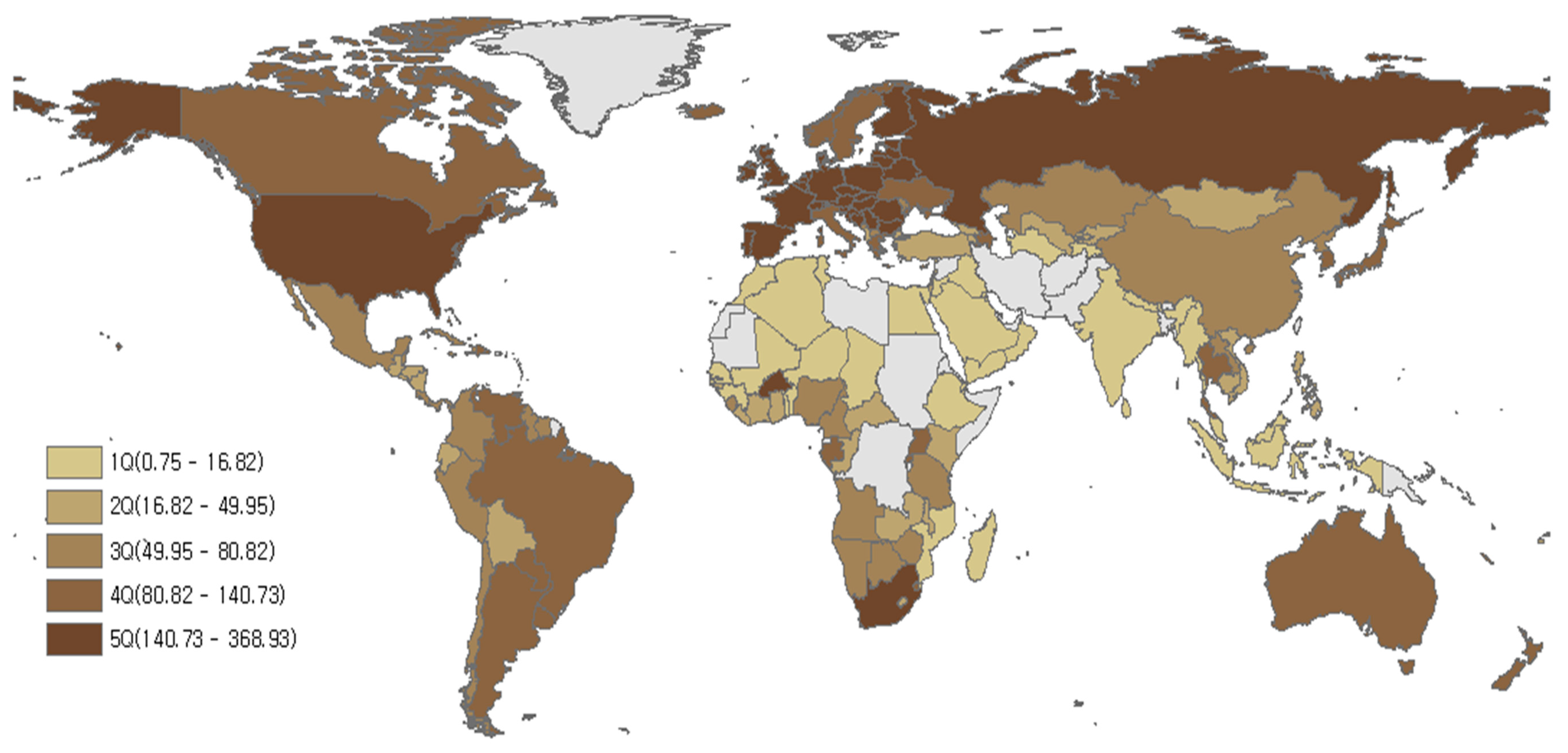
4.1. Situation of Red Meat Consumption and Life Expectancy
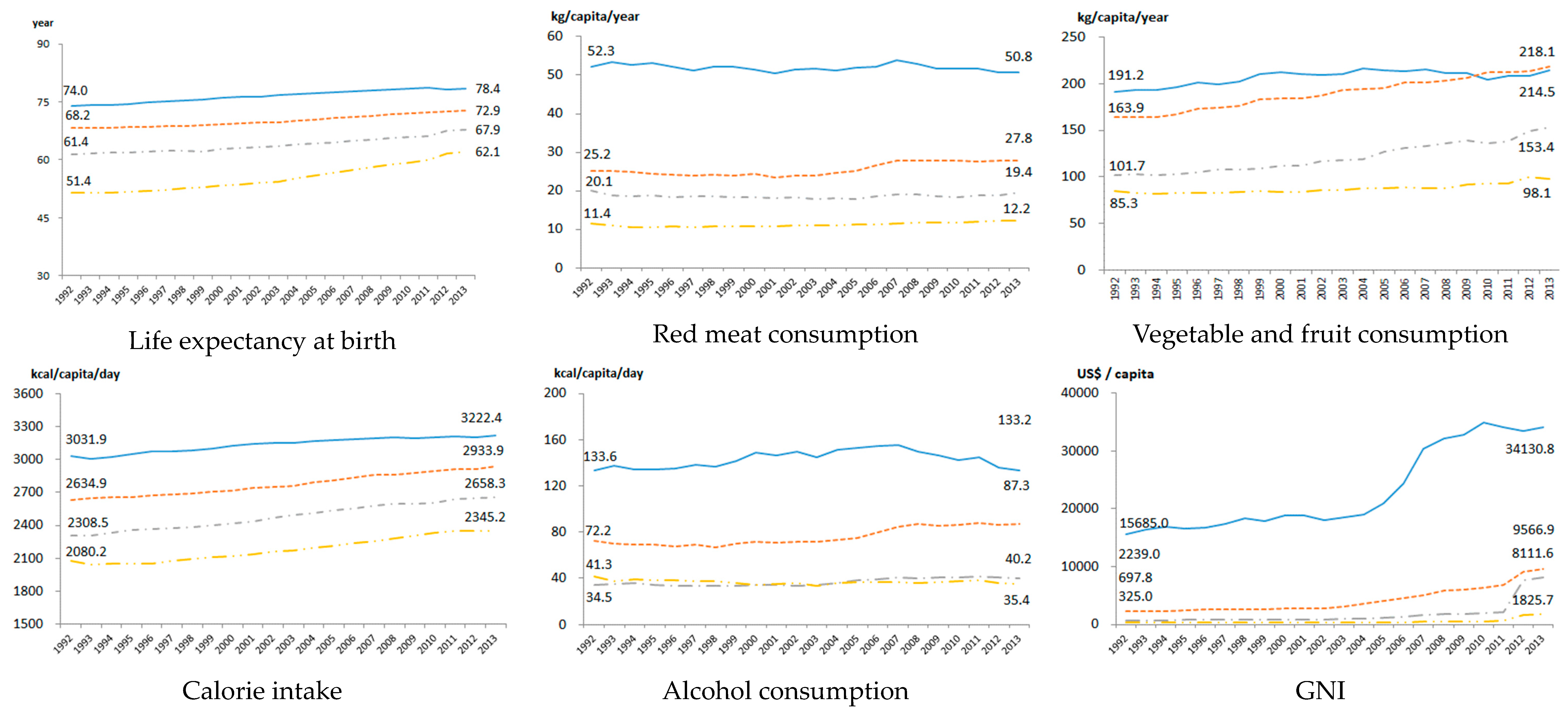
4.2. Descriptive Analysis
4.3. Estimates from Pooled OLS and Fixed Effect Regression Models
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Ethics Approval
References
- Ritchie, H.; Roser, M. Meat and Seafood Production & Consumption; Global Data Change Lab: University of Oxford, UK, 2018; Published online at Our World in Data; Available online: https://ourworldindata.org/seafood-production (accessed on 5 February 2020).
- World Health Organization. Universal Health Coverage. 2018. Available online: http://www.who.int/universal_health_coverage/en/ (accessed on 3 January 2020).
- IARC. List of Classifications; IARC: Lyon, France, 2018; Volume 1–120, Available online: http://monographs.iarc.fr/ENG/Classification/latest_classif.php (accessed on 15 March 2018).
- Cross, A.J.; Ferrucci, L.M.; Risch, A.; Graubard, B.I.; Ward, M.H.; Park, Y.; Hollenbeck, A.R.; Schatzkin, A.; Sinha, R. A large prospective study of meat consumption and colorectal cancer risk: An investigation of potential mechanisms underlying this association. Cancer Res. 2010, 70, 2406–2414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aune, D.; Chan, D.S.; Vieira, A.R.; Rosenblatt, D.A.N.; Vieira, R.; Greenwood, D.C.; Kampman, E.; Norat, T. Red and processed meat intake and risk of colorectal adenomas: A systematic review and meta-analysis of epidemiological studies. Cancer Causes Control 2013, 24, 611–627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avila Curiel, A. Food, nutrition and the prevention of cancer: A global perspective. Salud Pública Méx. 2004, 46, 368–369. [Google Scholar] [CrossRef] [Green Version]
- Taylor, E.; Burley, V.; Greenwood, D.; Cade, J. Meat consumption and risk of breast cancer in the UK Women’s Cohort Study. Br. J. Cancer 2007, 96, 1139–1146. [Google Scholar] [CrossRef] [Green Version]
- Larsen, C.S. Animal source foods and human health during evolution. J. Nutr. 2003, 133, 3893S–3897S. [Google Scholar] [CrossRef] [PubMed]
- Bouvard, V.; Loomis, D.; Guyton, K.Z.; Grosse, Y.; Ghissassi, F.E.; Benbrahim-Tallaa, L.; Guha, N.; Mattock, H.; Straif, K.; International Agency for Research on Cancer Monograph Working Group. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015, 16, 1599–1600. [Google Scholar] [CrossRef] [Green Version]
- McAfee, A.J.; McSorley, E.M.; Cuskelly, G.J.; Moss, B.W.; Wallace, J.M.; Bonham, M.P.; Fearon, A.M. Red meat consumption: An overview of the risks and benefits. Meat Sci. 2010, 84, 1–13. [Google Scholar] [CrossRef]
- Lichtenstein, A.H.; Appel, L.J.; Brands, M.; Carnethon, M.; Daniels, S.; Franch, H.A.; Franklin, B.; Kris-Etherton, P.; Harris, W.S.; Howard, B. Diet and lifestyle recommendations revision 2006 A scientific statement from the American Heart Association nutrition committee. Circulation 2006, 114, 82–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skerrett, P.J.; Willett, W.C. Essentials of healthy eating: A guide. J. Midwifery Women’s Health 2010, 55, 492–501. [Google Scholar] [CrossRef] [Green Version]
- National Institute for Health. What Is a Standard Drink? National Institute for Health: Bethesda, MD, USA, 2019. Available online: https://www.niaaa.nih.gov/what-standard-drink (accessed on 17 January 2020).
- IARC. Consumption of Red Meat and Processed Meat; International Agency for Research on Cancer: Lyon, France, 2015; pp. 6–13. [Google Scholar]
- Tappel, A. Heme of consumed red meat can act as a catalyst of oxidative damage and could initiate colon, breast and prostate cancers, heart disease and other diseases. Med. Hypotheses 2007, 68, 562–564. [Google Scholar] [CrossRef]
- Halliwell, B. Oxidative stress and cancer: Have we moved forward? Biochem. J. 2007, 401, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Pan, A.; Sun, Q.; Bernstein, A.M.; Schulze, M.B.; Manson, J.E.; Stampfer, M.J.; Willett, W.C.; Hu, F.B. Red meat consumption and mortality: Results from 2 prospective cohort studies. Arch. Intern. Med. 2012, 172, 555–563. [Google Scholar] [PubMed] [Green Version]
- Sinha, R.; Cross, A.J.; Graubard, B.I.; Leitzmann, M.F.; Schatzkin, A. Meat intake and mortality: A prospective study of over half a million people. Arch. Intern. Med. 2009, 169, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Manson, J.E.; Buring, J.E.; Liu, S. A Prospective Study of Red Meat Consumption and Type 2 Diabetes in Middle-Aged and Elderly Women The Women’s Health Study. Diabetes Care 2004, 27, 2108–2115. [Google Scholar] [CrossRef] [Green Version]
- Kaluza, J.; Åkesson, A.; Wolk, A. Processed and Unprocessed Red Meat Consumption and Risk of Heart Failure Prospective Study of Men. Circ. Heart Fail. 2014, 7, 552–557. [Google Scholar] [CrossRef] [Green Version]
- Kaluza, J.; Wolk, A.; Larsson, S.C. Red Meat Consumption and Risk of Stroke A Meta-Analysis of Prospective Studies. Stroke 2012, 43, 2556–2560. [Google Scholar] [CrossRef] [Green Version]
- Micha, R.; Wallace, S.K.; Mozaffarian, D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus a systematic review and meta-analysis. Circulation 2010, 121, 2271–2283. [Google Scholar] [CrossRef] [Green Version]
- Azadbakht, L.; Esmaillzadeh, A. Red meat intake is associated with metabolic syndrome and the plasma C-reactive protein concentration in women. J. Nutr. 2009, 139, 335–339. [Google Scholar] [CrossRef]
- Pattison, D.J.; Symmons, D.P.; Lunt, M.; Welch, A.; Luben, R.; Bingham, S.A.; Khaw, K.T.; Day, N.E.; Silman, A.J. Dietary risk factors for the development of inflammatory polyarthritis: Evidence for a role of high level of red meat consumption. Arthritis Rheum. 2004, 50, 3804–3812. [Google Scholar] [CrossRef]
- Koeth, R.A.; Wang, Z.; Levison, B.S.; Buffa, J.A.; Org, E.; Sheehy, B.T.; Britt, E.B.; Fu, X.; Wu, Y.; Li, L. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013, 19, 576–585. [Google Scholar] [CrossRef] [Green Version]
- Friedman, L.A.; Kimball, A. Coronary heart disease mortality and alcohol consumption in Framingham. Am. J. Epidemiol. 1986, 124, 481–489. [Google Scholar] [CrossRef] [Green Version]
- Petti, S.; Scully, C. Oral cancer: The association between nation-based alcohol-drinking profiles and oral cancer mortality. Oral Oncol. 2005, 41, 828–834. [Google Scholar] [CrossRef] [PubMed]
- Leon, D.A.; Saburova, L.; Tomkins, S.; Andreev, E.; Kiryanov, N.; McKee, M.; Shkolnikov, V.M. Hazardous alcohol drinking and premature mortality in Russia: A population based case-control study. Lancet 2007, 369, 2001–2009. [Google Scholar] [CrossRef]
- Kono, S.; Ikeda, M.; Tokudome, S.; Nishizumi, M.; Kuratsune, M. Alcohol and mortality: A cohort study of male Japanese physicians. Int. J. Epidemiol. 1986, 15, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Maltby, J.; Wright, S.; Bird, G.; Sheron, N. Chemokine levels in human liver homogenates: Associations between GRO α and histopathological evidence of alcoholic hepatitis. Hepatology 1996, 24, 1156–1160. [Google Scholar]
- Dominguez, M.; Miquel, R.; Colmenero, J.; Moreno, M.; García–Pagán, J.C.; Bosch, J.; Arroyo, V.; Ginès, P.; Caballería, J.; Bataller, R. Hepatic expression of CXC chemokines predicts portal hypertension and survival in patients with alcoholic hepatitis. Gastroenterology 2009, 136, 1639–1650. [Google Scholar] [CrossRef]
- Fisher, N.D.L.; Orav, E.J.; Chang, G. Effects of alcohol consumption on blood pressure in hypertensive women. Am. J. Drug Alcohol Abus. 2018, 44, 200–205. [Google Scholar] [CrossRef]
- Stewart, D.; Han, L.; Doran, T.; McCambridge, J. Alcohol consumption and all-cause mortality: An analysis of general practice database records for patients with long-term conditions. J. Epidemiol. Community Health 2017, 71, 729–735. [Google Scholar] [CrossRef]
- Östergren, O.; Martikainen, P.; Lundberg, O. The contribution of alcohol consumption and smoking to educational inequalities in life expectancy among Swedish men and women during 1991–2008. Int. J. Public Health 2018, 63, 41–48. [Google Scholar] [CrossRef] [Green Version]
- Wood, A.M.; Kaptoge, S.; Butterworth, A.S.; Willeit, P.; Warnakula, S.; Bolton, T.; Paige, E.; Paul, D.S.; Sweeting, M.; Burgess, S.; et al. Risk thresholds for alcohol consumption: Combined analysis of individual-participant data for 599,912 current drinkers in 83 prospective studies. Lancet 2018, 391, 1513–1523. [Google Scholar] [CrossRef] [Green Version]
- Rehm, J.; Probst, C. Decreases of Life Expectancy Despite Decreases in Non-Communicable Disease Mortality: The Role of Substance Use and Socioeconomic Status. Eur. Addict. Res. 2018, 24, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Barrio, E.; Tome, S.; Rodriguez, I.; Gude, F.; Sanchez-Leira, J.; Perez-Becerra, E.; Gonzalez-Quintela, A. Liver disease in heavy drinkers with and without alcohol withdrawal syndrome. Alcohol. Clin. Exp. Res. 2004, 28, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Harper, C. The neuropathology of alcohol-related brain damage. Alcohol Alcohol. 2009, 44, 136–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, V.V.; Stewart, S.H.; Mohr, C.D. Coping-anxiety and coping-depression motives predict different daily mood-drinking relationships. Psychol. Addict. Behav. J. Soc. Psychol. Addict. Behav. 2009, 23, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Lee, I.M.; Manson, J.E.; Buring, J.E.; Sesso, H.D. Alcohol consumption, weight gain, and risk of becoming overweight in middle-aged and older women. Arch. Intern. Med. 2010, 170, 453–461. [Google Scholar] [CrossRef] [Green Version]
- An American Addiction Center Resource (AADCR). High Blood Pressure from Alcohol Consumption; An American Addiction Center Resource: Brentwood, TN, USA, 2018; Available online: https://www.alcohol.org/effects/blood-pressure/ (accessed on 7 July 2019).
- Alshahrani, S.M.; Fraser, G.E.; Sabaté, J.; Knutsen, R.; Shavlik, D.; Mashchak, A.; Lloren, J.I.; Orlich, M.J. Red and Processed Meat and Mortality in a Low Meat Intake Population. Nutrients 2019, 11, 622. [Google Scholar] [CrossRef] [Green Version]
- Crippa, A.; Larsson, S.C.; Discacciati, A.; Wolk, A.; Orsini, N. Red and processed meat consumption and risk of bladder cancer: A dose–response meta-analysis of epidemiological studies. Eur. J. Nutr. 2018, 57, 689–701. [Google Scholar] [CrossRef] [Green Version]
- Quintana Pacheco, D.A.; Sookthai, D.; Wittenbecher, C.; Graf, M.E.; Schübel, R.; Johnson, T.; Katzke, V.; Jakszyn, P.; Kaaks, R.; Kühn, T. Red meat consumption and risk of cardiovascular diseases—Is increased iron load a possible link? Am. J. Clin. Nutr. 2018, 107, 113–119. [Google Scholar] [CrossRef] [Green Version]
- Pelucchi, C.; Tramacere, I.; Boffetta, P.; Negri, E.; La Vecchia, C. Alcohol consumption and cancer risk. Nutr. Cancer 2011, 63, 983–990. [Google Scholar] [CrossRef]
- Turati, F.; Garavello, W.; Tramacere, I.; Pelucchi, C.; Galeone, C.; Bagnardi, V.; Corrao, G.; Islami, F.; Fedirko, V.; Boffetta, P.; et al. A meta-analysis of alcohol drinking and oral and pharyngeal cancers: Results from subgroup analyses. Alcohol Alcohol. 2013, 48, 107–118. [Google Scholar] [CrossRef] [Green Version]
- Fedirko, V.; Tramacere, I.; Bagnardi, V.; Rota, M.; Scotti, L.; Islami, F.; Negri, E.; Straif, K.; Romieu, I.; La Vecchia, C.; et al. Alcohol drinking and colorectal cancer risk: An overall and dose-response meta-analysis of published studies. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2011, 22, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Life Expectancy at Birth; World Health Organization: Geneva, Switzerland, 2005; Available online: https://www.who.int/whosis/whostat2006DefinitionsAndMetadata.pdf (accessed on 18 June 2019).
- Murray, C.J.L.; Lopez, A.D. Production and analysis of health indicators: The role of academia. PLoS Med. 2010, 7, e1001004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mwatsama, M.K.; Wong, S.; Ettehad, D.; Watt, N.F. Global health impacts of policies: Lessons from the UK. Glob. Health 2014, 10, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, C.M.; Clavier, C.; Potvin, L. Are national policies on global health in fact national policies on global health governance? A comparison of policy designs from Norway and Switzerland. BMJ Glob. Health 2017, 2, e000120. [Google Scholar] [CrossRef] [Green Version]
- Ohlhorst, S.D.; Russell, R.; Bier, D.; Klurfeld, D.M.; Li, Z.; Mein, J.R.; Milner, J.; Ross, A.C.; Stover, P.; Konopka, E. Nutrition research to affect food and a healthy life span. J. Nutr. 2013, 143, 1349–1354. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Pan, A.; Wang, D.D.; Liu, X.; Dhana, K.; Franco, O.H.; Kaptoge, S.; Angelantonio, E.D.; Stampfer, M.; Willett, W.C.; et al. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation 2018, 138, 345–355. [Google Scholar] [CrossRef]
- Zali, H.; Rezaei-Tavirani, M.; Azodi, M. Gastric cancer: Prevention, risk factors and treatment. Gastroenterol. Hepatol. Bed Bench 2011, 4, 175–185. [Google Scholar]
- Oyebode, O.; Gordon-Dseagu, V.; Walker, A.; Mindell, J.S. Fruit and vegetable consumption and all-cause, cancer and CVD mortality: Analysis of Health Survey for England data. J. Epidemiol. Community Health 2014, 68, 856–862. [Google Scholar] [CrossRef]
- Torres-Reyna, O. Panel data analysis fixed and random effects using Stata (v. 4.2). Data Stat. Serv. Priceton Univ. 2007, 112, 1–40. [Google Scholar]
- Bank, W. 2016. Available online: http://data.worldbank.org/country (accessed on 5 June 2016).
- Jakovljevic, M.B.; Vukovic, M.; Fontanesi, J. Life expectancy and health expenditure evolution in Eastern Europe—DiD and DEA analysis. Expert Rev. Pharm. Outcomes Res. 2016, 16, 537–546. [Google Scholar] [CrossRef]
- Han, M.A.; Zeraatkar, D.; Guyatt, G.H.; Vernooij, R.W.M.; El Dib, R.; Zhang, Y.; Algarni, A.; Leung, G.; Storman, D.; Valli, C.; et al. Reduction of Red and Processed Meat Intake and Cancer Mortality and Incidence: A Systematic Review and Meta-analysis of Cohort Studies. Ann. Intern. Med. 2019, 171, 711–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- USDA. Fresh Pork from Farm to Table; USDA: Washington, DC, USA, 2016. Available online: http://www.fsis.usda.gov/wps/portal/fsis/topics/food-safety-education/get-answers/food-safety-fact-sheets/meat-preparation/fresh-pork-from-farm-to-table/CT_Index (accessed on 8 August 2017).
- Grant, W.B. The role of meat in the expression of rheumatoid arthritis. Br. J. Nutr. 2000, 84, 589–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benito-Garcia, E.; Feskanich, D.; Hu, F.B.; Mandl, L.A.; Karlson, E.W. Protein, iron, and meat consumption and risk for rheumatoid arthritis: A prospective cohort study. Arthritis Res. Ther. 2007, 9, R16. [Google Scholar] [CrossRef] [Green Version]
- IFRI. Taxing Red Meat May Cut Emissions and Disease: Carbon Taxes on Food Could Help the World Control Global Warming and Improve Public Health; IFRI-blog: Washington, DC, USA, 2016; Available online: http://www.ifpri.org/blog/taxing-red-meat-may-cut-emissions-and-disease (accessed on 15 March 2018).
- FAO. Meat and Meat Products in Human Nutrition in Developing Countries; Food and Agtriculture Organization of the United Nations: Rome, Italy, 1992. [Google Scholar]
- Walker, P.; Rhubart-Berg, P.; McKenzie, S.; Kelling, K.; Lawrence, R.S. Public health implications of meat production and consumption. Public Health Nutr. 2005, 8, 348–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popkin, B.M. Reducing meat consumption has multiple benefits for the world’s health. Arch. Intern. Med. 2009, 169, 543–545. [Google Scholar] [CrossRef]
- Fanzo, J.; Hawkes, C.; Udomkesmalee, E.; Afshin, A.; Allemandi, L.; Assery, O.; Baker, P.; Battersby, J.; Bhutta, Z.; Chen, K. 2018 Global Nutrition Report: Shining a Light to Spur Action on Nutrition; Development Innitiative: Bristol, UK, 2018. [Google Scholar]
- Ranabhat, C.L.; Jakovljevic, M.; Dhimal, M.; Kim, C.-B. Structural Factors Responsible for Universal Health Coverage in Low- and Middle-Income Countries: Results From 118 Countries. Front. Public Health 2020, 7, 414. [Google Scholar] [CrossRef] [Green Version]
- Delgado, C.L. Rising consumption of meat and milk in developing countries has created a new food revolution. J. Nutr. 2003, 133, 3907S–3910S. [Google Scholar] [CrossRef] [Green Version]
- Chemnitz, C.; Becheva, S. Meat Atlas: Facts and Figures about the Animals We Eat; Heinrich Böll Foundation: Berlin, Germany, 2014. [Google Scholar]
- Takata, Y.; Shu, X.-O.; Gao, Y.-T.; Li, H.; Zhang, X.; Gao, J.; Cai, H.; Yang, G.; Xiang, Y.-B.; Zheng, W. Red meat and poultry intakes and risk of total and cause-specific mortality: Results from cohort studies of Chinese adults in Shanghai. PLoS ONE 2013, 8, e56963. [Google Scholar] [CrossRef] [Green Version]
- Fund, W.C.R.; American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective; American Institute for Cancer Research: Washington, DC, USA, 2007; Volume 1. [Google Scholar]
- Griswold, M.G.; Fullman, N.; Ranabhat, C.L.; Hawley, C.; Arian, N.; Zimsen, S.R.; Tymeson, H.D.; Venkateswaran, V.; Salama, J.S. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar] [CrossRef] [Green Version]
- Tomkins, S.; Collier, T.; Oralov, A.; Saburova, L.; McKee, M.; Shkolnikov, V.; Kiryanov, N.; Leon, D.A. Hazardous alcohol consumption is a major factor in male premature mortality in a typical Russian city: Prospective cohort study 2003–2009. PLoS ONE 2012, 7, e30274. [Google Scholar] [CrossRef] [Green Version]
- Ranabhat, C.L.; Atkinson, J.; Park, M.-B.; Kim, C.-B.; Jakovljevic, M. The influence of universal health coverage on life expectancy at birth (LEAB) and healthy life expectancy (HALE): A multi-country cross-sectional study. Front. Pharmacol. 2018, 9, 960. [Google Scholar] [CrossRef] [Green Version]
- Gulis, G. Life expectancy as an indicator of environmental health. Eur. J. Epidemiol. 2000, 16, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Nixon, J.; Ulmann, P. The relationship between health care expenditure and health outcomes. Eur. J. Health Econ. 2006, 7, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Kabir, M. Determinants of life expectancy in developing countries. J. Dev. Areas 2008, 41, 185–204. [Google Scholar] [CrossRef]
- Jakovljevic, M.; Riegler, A.; Jovanovic, M.; Djordjevic, N.; Patek, K.; Lesch, O.; Walter, H. Serbian and Austrian alcohol-dependent patients: A comparison of two samples regarding therapeutically relevant clinical features. Alcohol Alcohol. 2013, 48, 505–508. [Google Scholar] [CrossRef] [Green Version]
- U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 7th ed.; USDA: Washington, DC, USA, 2010.
- MOHW. Dietary Reference Intakes for Koreans 2015; Ministry of Health and Welfare, Republic of Korea Sejong: Seoul, Korea, 2015.
| Variable | VIF | Tolerance |
|---|---|---|
| Red meat consumption | 3.12 | 0.320 |
| Vegetable and fruit consumption | 3.06 | 0.327 |
| Calorie intake | 2.48 | 0.403 |
| Alcohol consumption | 1.89 | 0.528 |
| GNI | 1.64 | 0.611 |
| Mean VIF | 2.44 | |
| LIC (n1 = 27) | LMIC (n2 = 38) | UMIC (n3 = 47) | HIC (n4 = 52) | |
|---|---|---|---|---|
| LE (years) | 55.3 | 63.9 | 70.1 | 76.5 |
| Red meat consumption (kg/capita/year) | 11.2 | 18.6 | 25.6 | 51.9 |
| Vegetable and fruit consumption (kg/capita/year) | 87.4 | 120.9 | 189.9 | 206.5 |
| Calorie intake (kcal/capita/day) | 2181.2 | 2480.0 | 2774.6 | 3136.0 |
| Alcohol consumption (kcal/capita/day) | 36.8 | 36.9 | 76.0 | 143.0 |
| GNI (US$/capita) | 499.44 | 1775.1 | 4238.3 | 23,325.33 |
| Pooled OLS | Fixed-Effect Model | Lag 5 Years | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LIC | LMIC | UMIC | HIC | LIC | LMIC | UMIC | HIC | LIC | LMIC | UMIC | HIC | |
| Red meat consumption (kg/capita/year) | 2.069 (0.000) | 1.365 (0.001) | 0.211 (0.545) | 1.831 (0.000) | −0.560 (0.490) | −0.013 (0.977) | 0.208 (0.548) | −2.039 (0.000) | −1.525 (0.077) | −0.536 (0.353) | −1.384 (0.001) | −1.616 (0.000) |
| Vegetable and fruit consumption (kg/capita/year) | 1.63 (0.000) | 4.109 (0.000) | 5.546 (0.000) | 1.789 (0.000) | 0.914 (0.231) | 1.766 (0.000) | −0.094 (0.752) | 1.258 (0.000) | −0.120 (0.881) | 0.245 (0.622) | −0.312 (0.396) | 0.519 (0.878) |
| Calories intake (kcal/capita/day) | 13.894 (0.000) | −0.839 (0.725) | 5.258 (0.001) | 3.059 (0.000) | 28.437 (0.000) | 2.126 (0.159) | 4.079 (0.003) | 3.324 (0.152) | 35.199 (0.000) | 8.269 (0.001) | 8.818 (0.000) | 11.531 (0.000) |
| Alcohol consumption (kcal/capita/day) | −1.124 (0.000) | −1.691 (0.000) | −0.594 (0.001) | −0.240 (0.017) | −1.909 (0.000) | −0.291 (0.217) | −0.259 (0.127) | −0.216 (0.272) | −1.562 (0.003) | 0.368 (0.190) | −0.299 (0.226) | −0.615 (0.003) |
| GNI (US$/capita) | 3.983 (0.000) | 3.580 (0.000) | 2.236 (0.000) | 2.644 (0.000) | 4.355 (0.000) | 2.058 (0.000) | 2.103 (0.000) | 2.397 (0.000) | 1.798 (0.000) | 1.184 (0.000) | 1.439 (0.000) | 2.079 (0.000) |
| Cons | −84.592 (0.000) | 16.455 (0.089) | −16.042 (0.122) | 10.925 (0.061) | −187.375 (0.000) | 25.758 (0.000) | 21.847 (0.023) | −60.705 (0.000) | −221.033 (0.000) | −10.657 (0.527) | −4.941 (0.700) | −28.225 (0.000) |
| Adj. R-squared | 0.325 | 0.296 | 0.411 | 0.586 | 0.591 | 0.395 | 0.428 | 0.420 | 0.486 | 0.248 | 0.291 | 0.495 |
| Observation | 551 | 794 | 934 | 992 | 551 | 794 | 934 | 992 | 434 | 622 | 723 | 768 |
| Number of countries | 27 | 38 | 47 | 52 | 27 | 38 | 47 | 52 | 26 | 38 | 47 | 52 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ranabhat, C.L.; Park, M.-B.; Kim, C.-B. Influence of Alcohol and Red Meat Consumption on Life Expectancy: Results of 164 Countries from 1992 to 2013. Nutrients 2020, 12, 459. https://doi.org/10.3390/nu12020459
Ranabhat CL, Park M-B, Kim C-B. Influence of Alcohol and Red Meat Consumption on Life Expectancy: Results of 164 Countries from 1992 to 2013. Nutrients. 2020; 12(2):459. https://doi.org/10.3390/nu12020459
Chicago/Turabian StyleRanabhat, Chhabi Lal, Myung-Bae Park, and Chun-Bae Kim. 2020. "Influence of Alcohol and Red Meat Consumption on Life Expectancy: Results of 164 Countries from 1992 to 2013" Nutrients 12, no. 2: 459. https://doi.org/10.3390/nu12020459
APA StyleRanabhat, C. L., Park, M.-B., & Kim, C.-B. (2020). Influence of Alcohol and Red Meat Consumption on Life Expectancy: Results of 164 Countries from 1992 to 2013. Nutrients, 12(2), 459. https://doi.org/10.3390/nu12020459







