Predictive Ability of Waist Circumference and Waist-to-Height Ratio for Cardiometabolic Risk Screening among Spanish Children
Abstract
1. Background
2. Methods
2.1. Design and Study Participants
2.2. Measurements
2.2.1. Anthropometric Variables
2.2.2. Blood Pressure
2.2.3. Biochemical Assessments
2.2.4. Metabolic Syndrome (MetS)
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012, 307, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1246. [Google Scholar] [CrossRef] [PubMed]
- Lakshman, R.; Elks, C.E.; Ong, K.K. Childhood obesity. Circulation 2012, 126, 1770–1779. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Dietz, W.H.; Srinivasan, S.R.; Berenson, G.S. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics 1999, 103, 1175–1182. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.B.; Harro, M.; Sardinha, L.B.; Froberg, K.; Ekelund, U.; Brage, S.; Anderssen, S.A. Physical activity, and clustered cardiovascular risk in children: A cross-sectional study (The European Youth Heart Study). Lancet 2006, 368, 299–304. [Google Scholar] [CrossRef]
- Magnussen, C.G.; Koskinen, J.; Chen, W.; Thomson, R.; Schmidt, M.D.; Srinivasan, S.R.; Kivimaki, M.; Mattsson, N.; Kähönen, M.; Laitinen, T.; et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation 2010, 122, 1604–1611. [Google Scholar] [CrossRef]
- Magge, S.N.; Goodman, E.; Armstrong, S.C. The metabolic syndrome in children and adolescents: Shifting the focus to Cardiometabolic risk factor clustering. Pediatrics 2017, 140, e20171603. [Google Scholar] [CrossRef]
- Sardinha, L.B.; Santos, D.A.; Silva, A.M.; Grøntved, A.; Andersen, L.B.; Ekelund, U. A comparison between BMI, waist circumference, and waist-to-height ratio for identifying cardio-metabolic risk in children and adolescents. PLoS ONE 2016, 11, e0149351. [Google Scholar] [CrossRef]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S. 2000 CDC growth charts for the United States: Methods and development. Vital. Health Stat. 11 2002, 246, 1–190. [Google Scholar]
- World Health Organization. Growth Reference Data for 5–19 Years; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Freedman, D.S.; Wang, J.; Maynard, L.M.; Thornton, J.C.; Mei, Z.; Pierson, R.N., Jr.; Dietz, W.H.; Horlick, M. Relation of BMI to fat and fat-free mass among children and adolescents. Int. J. Obes. 2005, 29, 1. [Google Scholar] [CrossRef]
- Demerath, E.W.; Schubert, C.M.; Maynard, L.M.; Sun, S.S.; Chumlea, W.C.; Pickoff, A.; Czerwinski, S.A.; Towne, B.; Siervogel, R.M. Do changes in body mass index percentile reflect changes in body composition in children? Data from the Fels Longitudinal Study. Pediatrics 2006, 117, 487–495. [Google Scholar] [CrossRef] [PubMed]
- IDF. The IDF Consensus Definition of the Metabolic Syndrome in Children and Adolescents; IDF: Brussels, Belgium, 2007. [Google Scholar]
- Hirschler, V.; Aranda, C.; de Luján Calcagno, M.; Maccalini, G.; Jadzinsky, M. Can waist circumference identify children with the metabolic syndrome? Arch. Pediatr. Adolesc. Med. 2005, 159, 740–744. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kotlyarevska, K.; Wolfgram, P.; Lee, J.M. Is waist circumference a better predictor of insulin resistance than body mass index in US adolescents? J. Adolesc. Health 2011, 49, 330–333. [Google Scholar] [CrossRef] [PubMed]
- Bosy-Westphal, A.; Geisler, C.; Onur, S.; Korth, O.; Selberg, O.; Schrezenmeir, J.; Müller, M.J. Value of body fat mass vs anthropometric obesity indices in the assessment of metabolic risk factors. Int. J. Obes. 2006, 30, 475. [Google Scholar] [CrossRef]
- Fernandes, R.A.; Christofaro, D.G.D.; Codogno, J.S.; Buonani, C.; Bueno, D.R.; Oliveira, A.R.; Rosa, C.S.; Freitas, I.F., Jr. Cut-offs propose for abdominal obesity identification among adolescents. Arq. Bras. Cardiol. 2009, 93, 603–609. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012, 13, 275–286. [Google Scholar] [CrossRef]
- Schroder, H.; Ribas, L.; Koebnick, C.; Funtikova, A.; Gómez, S.F.; Fitó, M.; Perez-Rodrigo, C.; Serra-Majem, L. Prevalence of Abdominal Obesity in Spanish Children and Adolescents. Do We Need Waist Circumference Measurements in Pediatric Practice? PLoS ONE 2014, 9, e87549. [Google Scholar] [CrossRef]
- Ashwell, M.; Hsieh, S.D. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int. J. Food Sci. Nutr. 2005, 56, 303–307. [Google Scholar] [CrossRef]
- Ashwell, M.; Mayhew, L.; Richardson, J.; Rickayzen, B. Waist-to-height ratio is more predictive of years of life lost than body mass index. PLoS ONE 2014, 9, e103483. [Google Scholar] [CrossRef]
- Bauer, K.; Marcus, M.; Ogden, C.; Foster, G. Cardio-metabolic risk screening among adolescents: Understanding the utility of body mass index, waist circumference and waist to height ratio. Pediatr. Obes. 2015, 10, 329–337. [Google Scholar] [CrossRef]
- Kahn, H.S.; Imperatore, G.; Cheng, Y.J. A population-based comparison of BMI percentiles and waist-to-height ratio for identifying cardiovascular risk in youth. J. Pediatr. 2005, 146, 482–488. [Google Scholar] [CrossRef]
- Graves, L.; Garnett, S.P.; Cowell, C.T.; Baur, L.A.; Ness, A.; Sattar, N.; Lawlor, D.A. Waist-to-height ratio and cardiometabolic risk factors in adolescence: Findings from a prospective birth cohort. Pediatr. Obes. 2014, 9, 327–338. [Google Scholar] [CrossRef]
- Ashwell, M.; Gibson, S. A proposal for a primary screening tool: Keep your waist circumference to less than half your height. BMC Med. 2014, 12, 207. [Google Scholar] [CrossRef] [PubMed]
- Khoury, M.; Manlhiot, C.; McCrindle, B.W. Role of the Waist/Height Ratio in the Cardiometabolic Risk Assessment of Children Classified by Body Mass Index. J. Am. Coll. Cardiol. 2013, 62, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Kruger, H.S.; Faber, M.; Schutte, A.E.; Ellis, S.M. A proposed cutoff point of waist-to-height ratio for metabolic risk in African township adolescents. Nutrition 2013, 29, 502–507. [Google Scholar] [CrossRef]
- Sangrador, C.O.; Ochoa-Brezmes, J. Waist-to-height ratio as a risk marker for metabolic syndrome in childhood. A meta-analysis. Pediatr. Obes. 2018, 13, 421–432. [Google Scholar] [CrossRef]
- Vizcaíno, V.M.; Aguilar, F.S.; Gutiérrez, R.F.; Martínez, M.S.; López, M.S.; Martínez, S.S.; García, E.L.; Artalejo, F.R. Assessment of an after-school physical activity program to prevent obesity among 9-to 10-year-old children: A cluster randomized trial. Int. J. Obes. 2008, 32, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Vizcaino, V.; Sánchez-López, M.; Salcedo-Aguilar, F.; Notario-Pacheco, B.; Solera-Martínez, M.; Moya-Martínez, P.; Franquelo-Morales, P.; López-Martínez, S.; Rodríguez-Artalejo, F. Protocolo de un ensayo aleatorizado de clusters para evaluar la efectividad del programa MOVI-2 en la prevención del sobrepeso en escolares. Rev. Esp. Cardiol. 2012, 65, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Marfell-Jones, M.; Olds, T.; Stewart, A. International standards for anthropometric assessment; International Society for the Advancement of Kinanthropometry: Wellington, New Zealand, 2011. [Google Scholar]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation and treatment or high blood pressure in children and adolescents. Pediatrics 2004, 114, S2. [Google Scholar]
- National Heart, Lung and Blood Institute. Expert on Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in children and adolescents (full reported). Pediatrics 2012, 128, 213–256. [Google Scholar]
- National Diabetes Data Group. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 1979, 28, 1039–1057. [Google Scholar] [CrossRef] [PubMed]
- Anderssen, S.A.; Cooper, A.R.; Riddoch, C.; Sardinha, L.B.; Harro, M.; Brage, S.; Andersen, L.B. Low cardiorespiratory fitness is a strong predictor for clustering of cardiovascular disease risk factors in children independent of country, age, and sex. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Hanley, J.A.; McNeil, B.J. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983, 148, 839–843. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Glas, A.S.; Lijmer, J.G.; Prins, M.H.; Bonsel, G.J.; Bossuyt, P.M. The diagnostic odds ratio: A single indicator of test performance. J. Clin. Epidemiol. 2003, 56, 1129–1135. [Google Scholar] [CrossRef]
- Berenson, G.S.; Srinivasan, S.R.; Bao, W.; Newman, W.P., 3rd; Tracy, R.E.; Wattigney, W.A. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N. Eng. J. Med. 1998, 338, 1650–1656. [Google Scholar] [CrossRef]
- Kuba, V.M.; Leone, C.; Damiani, D. Is waist-to-height ratio a useful indicator of cardio-metabolic risk in 6-10-year-old children? BMC Pediatr. 2013, 13, 91. [Google Scholar] [CrossRef]
- Hirschler, V.; Ruiz, A.; Romero, T.; Dalamón, R.; Molinari, C. Comparison of Different Anthropometric Indices for Identifying Insulin Resistance in Schoolchildren. Diabetes Technol. Ther. 2009, 11, 615–621. [Google Scholar] [CrossRef]
- Quadros, T.M.; Gordia, A.P.; Silva, R.C.; Silva, L.R. Predictive capacity of anthropometric indicators for dyslipidemia screening in children and adolescents. J. Pediatr. 2015, 91, 455–463. [Google Scholar] [CrossRef]
- Zhang, Y.X.; Wang, Z.X.; Chu, Z.H.; Zhao, J.S. Blood pressure profiles of children and adolescents categorized by waist-to-height ratio cutoffs: Study in a large sample in Shandong, China. Blood Press Monit. 2017, 22, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Goran, M.I.; Ball, G.D.C.; Cruz, M.L. Obesity and Risk of Type 2 Diabetes and Cardiovascular Disease in Children and Adolescents. J. Clin. Endocrinol. Metab. 2003, 88, 1417–1427. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.; Wong, M.; Khalechelvam, P.; Tam, W. Waist-to-height ratio, body mass index and waist circumference for screening paediatric cardio-metabolic risk factors: A meta-analysis. Obes. Rev. 2016, 17, 1258–1275. [Google Scholar] [CrossRef] [PubMed]

| Total (n = 848) | Boys (n = 408) | Girls (n = 440) | p | |
|---|---|---|---|---|
| Age | 9.5 ± 0.7 | 9.5 ± 0.7 | 9.5 ± 0.7 | 0.986 |
| Anthropometric measures | ||||
| Weight (kg) | 37.3 ± 9.1 | 37.6 ± 9.3 | 37.0 ± 8.9 | 0.331 |
| Height (cm) | 139.6 ± 7.0 | 139.5 ± 6.8 | 139.7 ± 7.2 | 0.713 |
| BMI (kg/m2) | 19.0 ± 3.6 | 19.1 ± 3.7 | 18.8 ± 3.6 | 0.183 |
| WC (cm) | 67.5 ± 9.2 | 68.2 ± 9.5 | 66.8 ± 8.8 | 0.025 |
| WtHR | 0.5 ± 0.06 | 0.5 ± 0.06 | 0.5 ± 0.06 | 0.011 |
| Biochemical measurements | ||||
| Glucose (mg/dL) | 83.1 ± 6.3 | 84.3 ± 6.3 | 82.0 ± 6.1 | <0.001 |
| Insulin (µU/mL) * | 6.9 (5.1, 9.4) | 6.3 (4.8, 8.5) | 7.5 (5.6, 10.2) | <0.001 |
| TG (mg/dL) * | 58 (44, 81) | 55 (41, 77) | 62 (47.3, 84) | <0.001 |
| HDL-C (mg/dL) | 59.9 ± 13.4 | 61.6 ± 14.0 | 58.3 ± 12.7 | <0.001 |
| SBP (mmHg) | 100.6 ± 9.0 | 101.9 ± 9.1 | 99.4 ± 8.8 | <0.001 |
| DBP (mmHg) | 62.0 ± 7.3 | 61.9 ± 7.3 | 62.1 ± 7.2 | 0.767 |
| MetS | 0.01 ± 2.4 | 0.04 ± 2.4 | −0.02 ± 2.4 | 0.692 |
| Frequency of metabolic abnormalities | % (n) | |||
| HDL-C (<40mg/dL) | 11.8 (100) | 9.1 (37) | 14.3 (63) | 0.018 |
| TG (>130mg/dL) | 14 (119) | 10.8 (44) | 17 (75) | 0.009 |
| Elevated BP (P> 95) | 3.2 (27) | 3.7 (15) | 2.7 (12) | 0.432 |
| Insulin (>15.05 µU/mL) | 6.8 (58) | 4.9 (20) | 8.6 (38) | 0.030 |
| MetS (>+1SD) | 33.3 (282) | 35.5 (145) | 31.2 (137) | 0.174 |
| Independent Variable: WtHR | Independent Variable: WC | |||||
|---|---|---|---|---|---|---|
| Dependent Variable | B (SE) | Partial ŋ2 | p | B (SE) | Partial ŋ2 | p |
| HDL-C (mg/dL) | −0.86 (0.07) | 0.144 | <0.001 | −0.57(0.05) | 0.152 | <0.001 |
| TG (mg/dL) | 0.01 (0.001) | 0.178 | <0.001 | 0.01 (0.001) | 0.169 | <0.001 |
| Insulin (µU/mL) | 0.20 (0.001) | 0.258 | <0.001 | 0.01(0.001) | 0.309 | <0.001 |
| SBP (mmHg) | 0.39 (0.05) | 0.068 | <0.001 | 0.33 (0.03) | 0.112 | <0.001 |
| DBP (mmHg) | 0.32 (0.04) | 0.065 | <0.001 | 0.23 (0.03) | 0.087 | <0.001 |
| MetS | 0.24 (0.01) | 0.344 | <0.001 | 0.16 (0.01) | 0.367 | <0.001 |
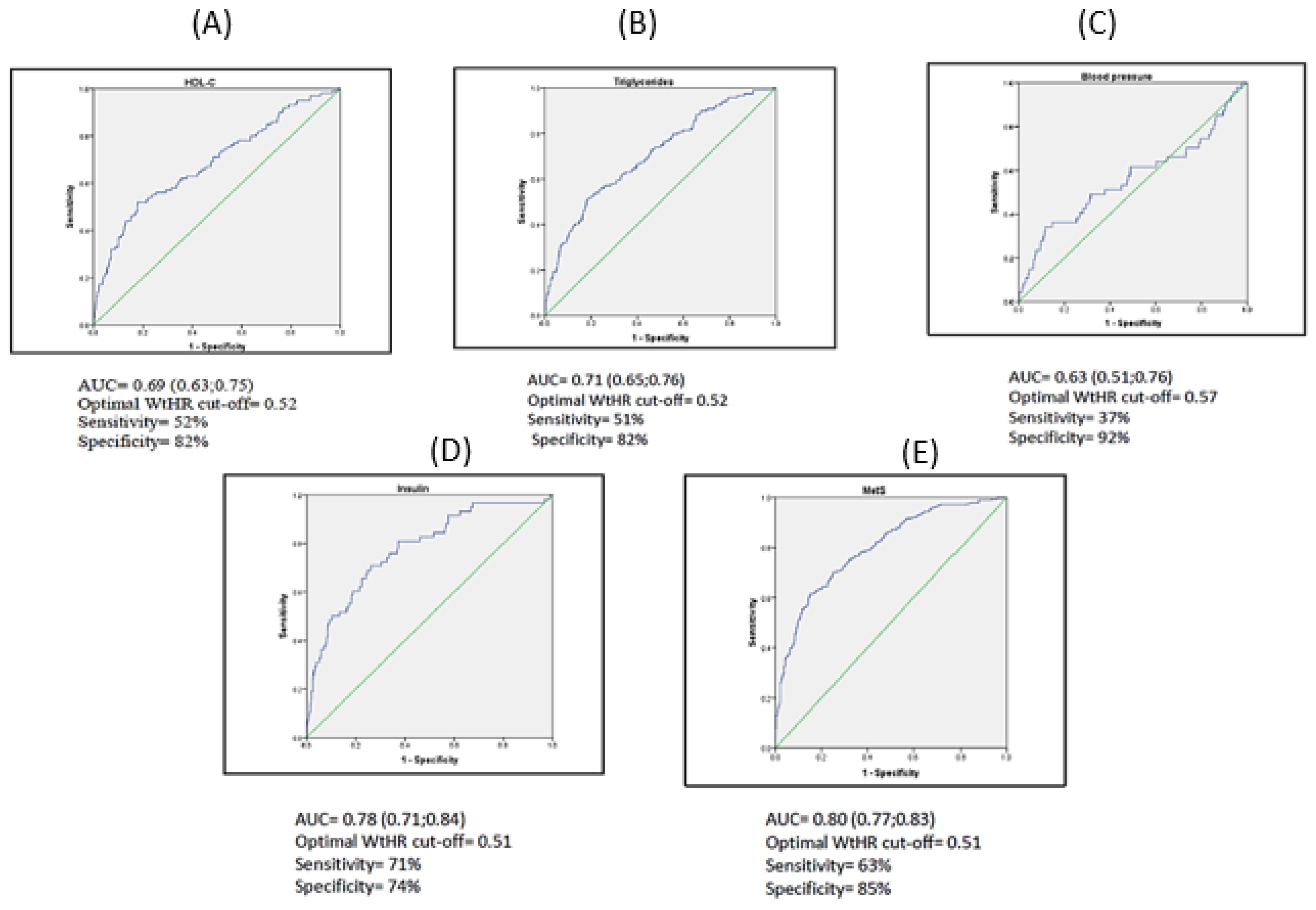
| WtHR and WC calculated | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| AUC | 95% CI | WtHR | Sens. | Spec. | AUC | 95% CI | WC (P90) | Sens. | Spec. | AUC Difference (SE) | |
| HDL-C | 0.69 | (0.63; 0.75) | 0.52 | 52 | 82 | 0.69 | (0.64; 0.75) | 80.2 | 30 | 93 | 0.01 (0.01) |
| TG | 0.71 | (0.65;0.76) | 0.52 | 51 | 82 | 0.70 | (0.65; 0.76) | 80.2 | 28 | 93 | 0.01 (0.01) |
| BP | 0.63 | (0.51;0.76) | 0.57 | 37 | 92 | 0.61 | (0.48; 0.74) | 80.2 | 30 | 91 | 0.02 (0.02) |
| Insulin | 0.78 | (0.71;0.84) | 0.51 | 71 | 74 | 0.80 | (0.74; 0.86) | 80.2 | 41 | 92 | 0.02 (0.01) |
| MetS | 0.80 | (0.77;0.83) | 0.51 | 63 | 85 | 0.81 | (0.77; 0.84) | 80.2 | 28 | 99 | 0.01 (0.01) |
| HDL-C | 0.69 | (0.63;0.75) | 0.50 | 57 | 69 | 0.69 | (0.64; 0.75) | 80.2 | 30 | 93 | 0.01 (0.01) |
| TG | 0.71 | (0.65;0.76) | 0.50 | 58 | 70 | 0.70 | (0.65; 0.76) | 80.2 | 28 | 93 | 0.01 (0.01) |
| BP | 0.63 | (0.51;0.76) | 0.50 | 56 | 67 | 0.61 | (0.48; 0.74) | 80.2 | 30 | 91 | 0.02 (0.02) |
| Insulin | 0.78 | (0.71;0.84) | 0.50 | 72 | 69 | 0.80 | (0.74; 0.86) | 80.2 | 41 | 92 | 0.02 (0.01) |
| MetS | 0.80 | (0.77;0.83) | 0.50 | 64 | 81 | 0.81 | (0.77; 0.84) | 80.2 | 28 | 99 | 0.01 (0.01) |
| WtHR | TP | TN | FP | FN | Sens. | Spec. | PPV | NPV | Accuracy | dOR | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HDL-C | 0.52 | 52 | 597 | 151 | 48 | 52 | 82 | 26 | 93 | 78 | 4.28 | (2.78; 6.59) |
| TG | 0.52 | 61 | 587 | 142 | 58 | 51 | 82 | 30 | 91 | 78 | 4.35 | (2.90; 6.51) |
| BP | 0.57 | 9 | 754 | 67 | 18 | 37 | 92 | 12 | 98 | 90 | 5.63 | (2.43; 13.01) |
| Insulin | 0.51 | 40 | 588 | 202 | 18 | 71 | 74 | 17 | 97 | 74 | 6.47 | (3.63; 11.54) |
| MetS | 0.51 | 164 | 492 | 78 | 114 | 63 | 85 | 68 | 81 | 78 | 9.07 | (6.47; 12.72) |
| HDL-C | 0.5 | 57 | 516 | 232 | 43 | 57 | 69 | 20 | 92 | 67 | 2.95 | (1.93; 4.51) |
| TG | 0.5 | 69 | 509 | 220 | 50 | 58 | 70 | 24 | 91 | 68 | 3.19 | (2.15; 4.75) |
| BP | 0.5 | 15 | 547 | 274 | 12 | 56 | 67 | 1 | 98 | 67 | 2.50 | (1.15; 5.41) |
| Insulin | 0.5 | 42 | 543 | 247 | 16 | 72 | 69 | 15 | 97 | 69 | 5.77 | (3.18; 10.46) |
| MetS | 0.5 | 178 | 459 | 111 | 110 | 64 | 81 | 62 | 82 | 75 | 7.36 | (5.34; 10.15) |
| HDL-C | 80.2 | 30 | 692 | 56 | 70 | 30 | 93 | 35 | 91 | 85 | 5.30 | (3.19-8.79) |
| TG | 80.2 | 33 | 676 | 53 | 86 | 28 | 93 | 38 | 89 | 84 | 4.89 | (3.00; 7.98) |
| BP | 80.2 | 8 | 743 | 78 | 19 | 30 | 91 | 9 | 98 | 89 | 4.01 | (1.7; 9.40) |
| Insulin | 80.2 | 24 | 728 | 62 | 34 | 41 | 92 | 28 | 96 | 88 | 8.29 | (4.63; 14.85) |
| MetS | 80.2 | 78 | 562 | 8 | 200 | 28 | 99 | 91 | 74 | 76 | 27.40 | (13.00; 57.73) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arellano-Ruiz, P.; García-Hermoso, A.; García-Prieto, J.C.; Sánchez-López, M.; Martínez Vizcaíno, V.; Solera-Martínez, M. Predictive Ability of Waist Circumference and Waist-to-Height Ratio for Cardiometabolic Risk Screening among Spanish Children. Nutrients 2020, 12, 415. https://doi.org/10.3390/nu12020415
Arellano-Ruiz P, García-Hermoso A, García-Prieto JC, Sánchez-López M, Martínez Vizcaíno V, Solera-Martínez M. Predictive Ability of Waist Circumference and Waist-to-Height Ratio for Cardiometabolic Risk Screening among Spanish Children. Nutrients. 2020; 12(2):415. https://doi.org/10.3390/nu12020415
Chicago/Turabian StyleArellano-Ruiz, Paola, Antonio García-Hermoso, Jorge C. García-Prieto, Mairena Sánchez-López, Vicente Martínez Vizcaíno, and Montserrat Solera-Martínez. 2020. "Predictive Ability of Waist Circumference and Waist-to-Height Ratio for Cardiometabolic Risk Screening among Spanish Children" Nutrients 12, no. 2: 415. https://doi.org/10.3390/nu12020415
APA StyleArellano-Ruiz, P., García-Hermoso, A., García-Prieto, J. C., Sánchez-López, M., Martínez Vizcaíno, V., & Solera-Martínez, M. (2020). Predictive Ability of Waist Circumference and Waist-to-Height Ratio for Cardiometabolic Risk Screening among Spanish Children. Nutrients, 12(2), 415. https://doi.org/10.3390/nu12020415







