The Efficacy of Squalene in Cardiovascular Disease Risk-A Systematic Review
Abstract
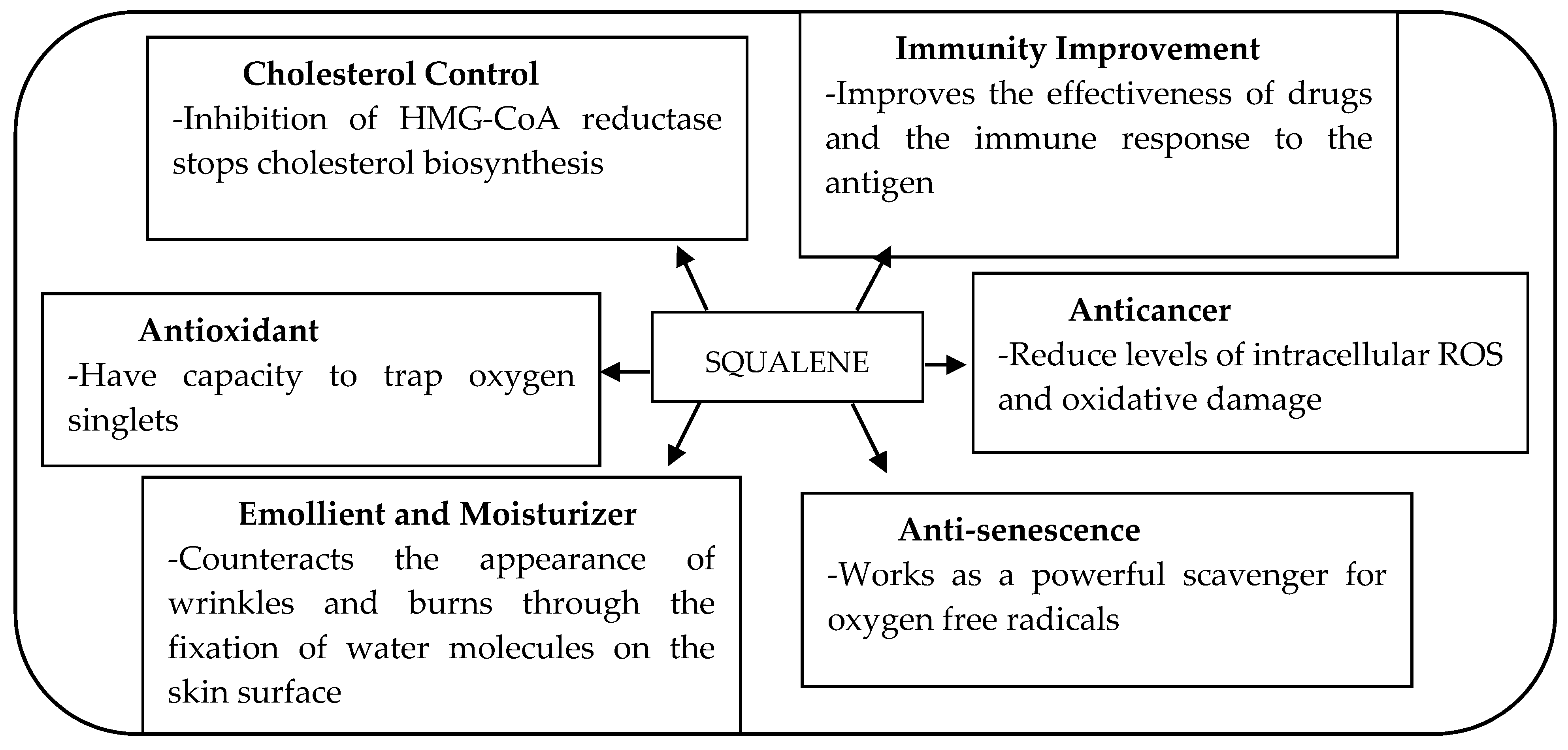
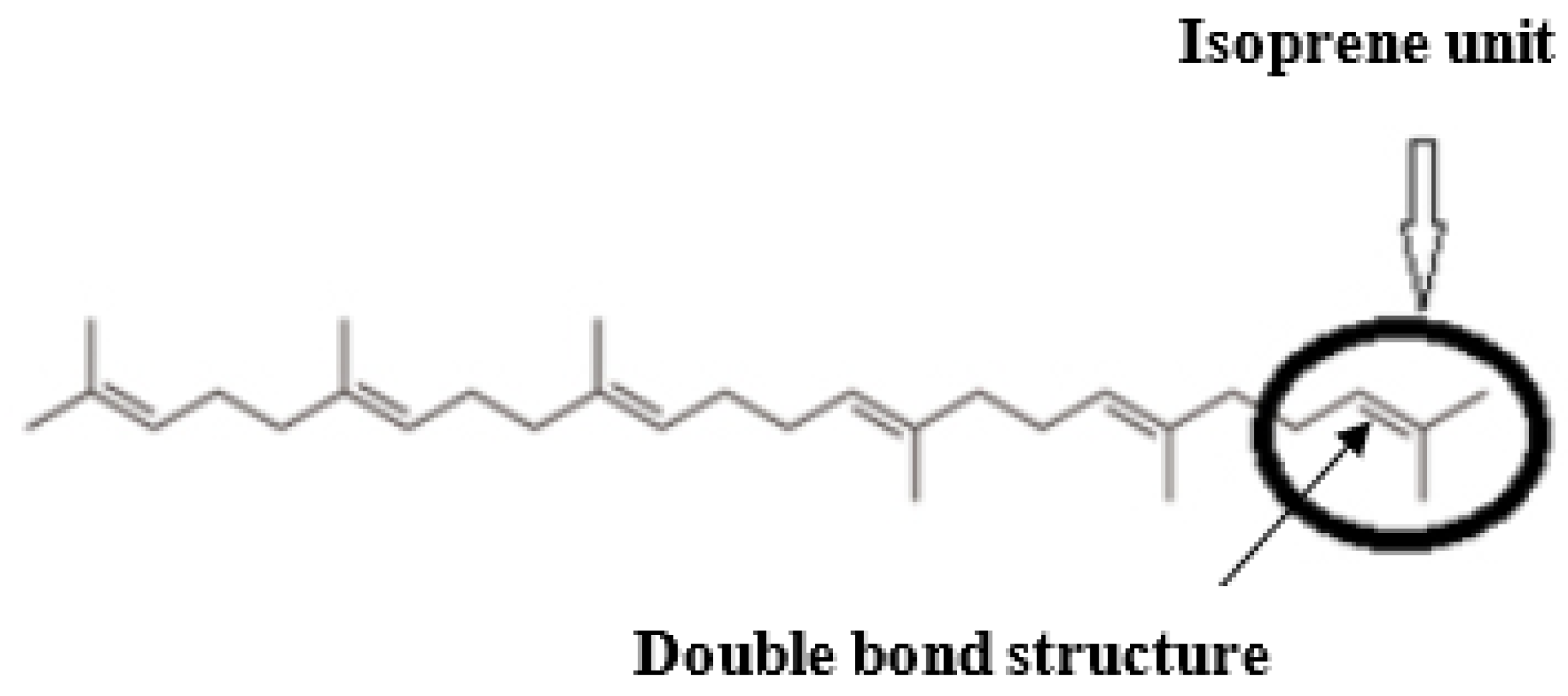
1. Introduction
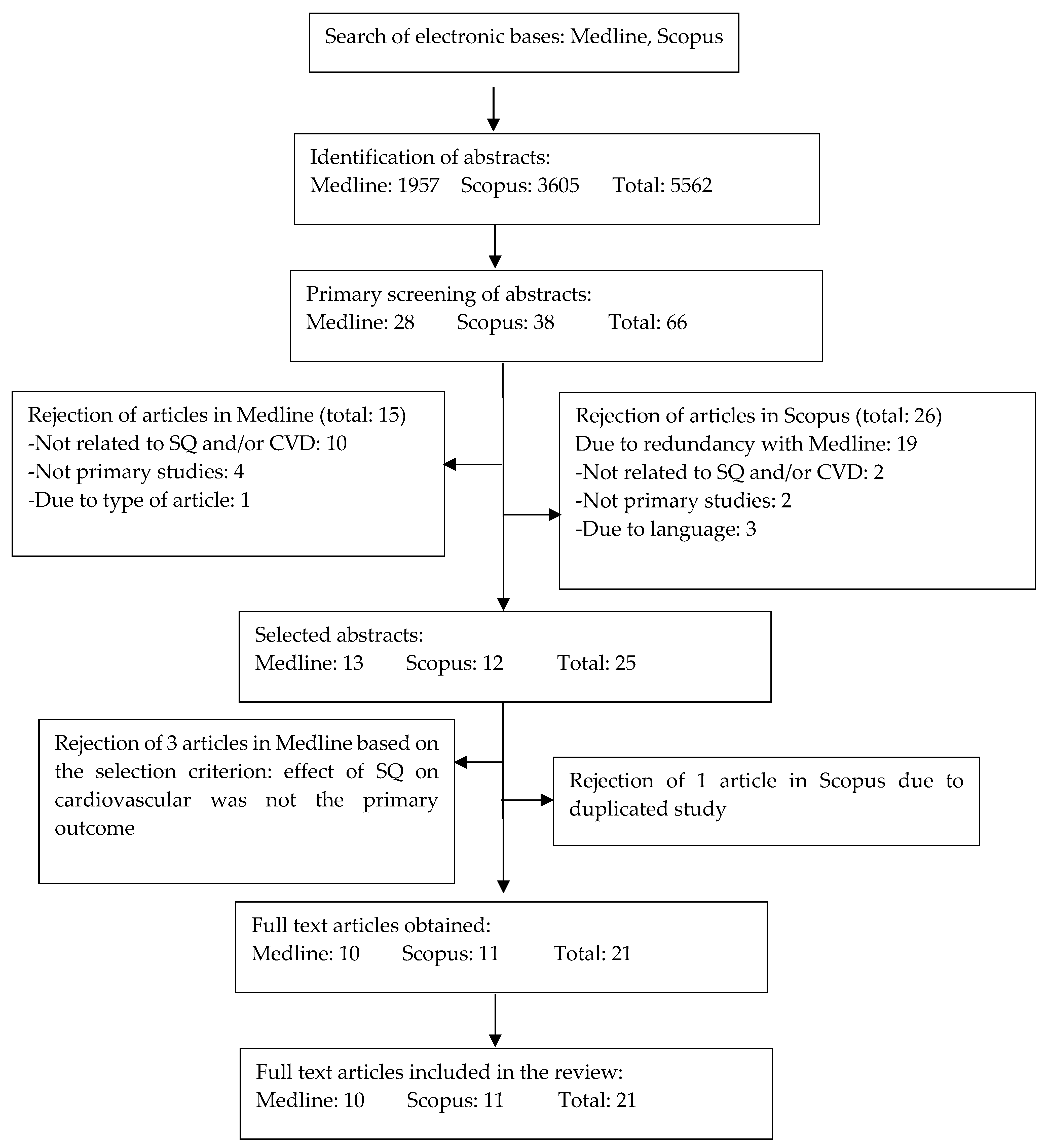
2. Methods
2.1. Literature Review
2.2. Selection of Research Articles
2.3. Data Extraction and Management
3. Results
3.1. Search Results
3.2. Study Characteristics
4. Effects of Squalene on CVD for Animal Studies
5. Effects of Squalene on CVD for Human Studies
6. Discussion
6.1. Diseases/Conditions included in the Review
6.2. Animal Studies
6.2.1. Animal Studies Related to Hyperlipidemia
6.2.2. Animal Studies Related to Atherosclerosis
6.2.3. Animal Studies Related to Myocardial Infarction (MI)
6.2.4. Animal Studies Related to Cardiotoxicity and Cardiomyopathy
6.3. Human Studies
Human Studies Related to Hypercholesterolemia
7. Strengths and Limitations of this Review
8. Recommendations
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| Apo A | apolipoprotein A |
| Apo E | apolipoprotein E |
| Apoa1 | apolipoprotein a-1 |
| Apoa5 | apolipoprotein a-5 |
| ALT | alanine aminotransferase |
| AST | aspartate transaminase |
| BW | body weight |
| Ca+2 | calcium ions |
| Ca2+ ATPase | calcium-dependent adenosine triphosphatase |
| CAT | catalase |
| CP | cyclophosphamide |
| CPK | creatine phosphokinase |
| CVD | cardiovascular disease |
| DHA | docosahexaenoic acid |
| EPA | eicosapentaenoic acid |
| FA | fatty acids |
| GPx | glutathione peroxidase |
| GR | glutathione reductase |
| GSH | reduced glutathione |
| GST | glutathione s-transferases |
| HDL-C | high-density lipoproteins cholesterols |
| HFD | high-fat diet |
| HMG-CoA | 3-hydroxy-3-methylglutarylcoenzyme A |
| i.p. | intraperitoneal |
| IDL | intermediate-density lipoproteins |
| KK-Ay | a cross between diabetic kk and lethal yellow |
| LDH | lactate dehydrogenase |
| LDL | low-density lipoproteins |
| LDL-C | low-density lipoprotein cholesterols |
| LPO | lipid peroxides |
| MDA | malondialdehyde |
| MI | myocardial infarction |
| mRNA | messenger RNA |
| N | normal diet |
| Na+ /K+ ATPase | sodium potassium-dependent adenosine triphosphatase |
| NO | nitric oxide |
| POTG | palm oil triacylglycerol |
| PUFA | polyunsaturated fatty acids |
| SOD | superoxide dismutase |
| SQ | squalene |
| TAC | total antioxidant capacity |
| TAG | triacylglycerol |
| TC | total cholesterol |
| TG | triglyceride |
| TL | total lipids |
| VLDL | very-low-density lipoproteins |
| WAT | white adipose tissue |
| WHO | World Health Organization |
References
- World Health Organization. Cardiovascular Disease. Available online: https://www.who.int/cardiovascular_diseases/en/ (accessed on 17 June 2019).
- Mendis, S.P.P.; Norrving, B. Global Atlas on Cardiovascular Disease Prevention and Control; WHO: Geneva, Switzerland, 2011; Available online: https://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/ (accessed on 17 June 2019).
- Torpy, J.M.; Lynm, C.; Glass, R.M. Risk Factors for Heart Disease. JAMA 2003, 290, 980. [Google Scholar] [CrossRef] [PubMed]
- Havranek, E.P.; Mujahid, M.S.; Barr, D.A.; Blair, I.V.; Cohen, M.S.; Cruz-Flores, S.; Davey-Smith, G.; Dennison-Himmelfarb, C.R.; Lauer, M.S.; Lockwood, D.W.; et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2015, 132, 873–898. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.; D’Agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of coronary heart disease using risk factor categories. Circulation 1998, 97, 1837–1847. [Google Scholar] [CrossRef] [PubMed]
- Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: The Scandinavian Simvastatin Survival Study (4S). Lancet 1994, 344, 1383–1389. [Google Scholar]
- Shepherd, J.; Cobbe, S.M.; Ford, I.; Isles, C.G.; Lorimer, A.R.; MacFarlane, P.W.; McKillop, J.H.; Packard, C.J. Prevention of Coronary Heart Disease with Pravastatin in Men with Hypercholesterolemia. N. Engl. J. Med. 1995, 333, 1301–1308. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Pfeffer, M.A.; Moye, L.A.; Rouleau, J.L.; Rutherford, J.D.; Cole, T.G.; Brown, L.; Warnica, J.W.; Arnold, J.M.; Wun, C.C.; et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N. Engl. J. Med. 1996, 335, 1001–1009. [Google Scholar] [CrossRef]
- Schachter, M. Chemical, pharmacokinetic and pharmacodynamic properties of statins: An update. Fundam. Clin. Pharm. 2005, 19, 117–125. [Google Scholar] [CrossRef]
- Dragos, D. High-Dose Statin Associated with Rhabdomyolysis, Acute Kidney Injury, Cholestatic Liver Injury, and Thrombocytopenia. J. Nephrol. Kidney 2017, 1, 1001. [Google Scholar] [CrossRef]
- Goldstein, J.L.; Brown, M.S. Regulation of the mevalonate pathway. Nature 1990, 343, 425–430. [Google Scholar] [CrossRef]
- Stancu, C.; Sima, A. Statins: Mechanism of action and effects. J. Cell. Mol. Med. 2001, 5, 378–387. [Google Scholar] [CrossRef]
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20, 536 high-risk individuals: A randomised placebo-controlled trial. Lancet 2002, 360, 7–22. [Google Scholar] [CrossRef]
- Waters, D.D. Medical therapy versus revascularization: The atorvastatin versus revascularization treatment AVERT trial. Can. J. Cardiol. 2000, 16, 11a–3a. [Google Scholar] [PubMed]
- Yokoyama, M.; Seo, T.; Park, T.; Yagyu, H.; Hu, Y.; Son, N.H.; Augustus, A.S.; Vikramadithyan, R.K.; Ramakrishnan, R.; Pulawa, L.K.; et al. Effects of lipoprotein lipase and statins on cholesterol uptake into heart and skeletal muscle. J. Lipid Res. 2007, 48, 646–655. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.H.; Lee, Y.C.; Chang, C.H.; Lin, M.S.; Lin, J.W.; Lai, M.S. Statins of high versus low cholesterol-lowering efficacy and the development of severe renal failure. Pharm. Drug Saf. 2013, 22, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Wang, Y.; Wu, N.; Zhu, C.; Guo, Y.; Qing, P.; Liu, G.; Dong, Q.; Li, J. Statins use and the risk of liver dysfunction: A Chinese cohort study in real world clinical practice. IJC Metab. Endocr. 2017, 16, 16–20. [Google Scholar] [CrossRef]
- Gaist, D.; Jeppesen, U.; Andersen, M.; García Rodríguez, L.A.; Hallas, J.; Sindrup, S.H. Statins and risk of polyneuropathy: A case-control study. Neurology 2002, 58, 1333–1337. [Google Scholar] [CrossRef] [PubMed]
- Bove, M.; Fogacci, F. Pharmacokinetic drug evaluation of ezetimibe + simvastatin for the treatment of hypercholesterolemia. Expert. Opin. Drug Metab. Toxicol. 2017, 13, 1099–1104. [Google Scholar] [CrossRef]
- Slim, H.; Thompson, P.D. Ezetimibe-related myopathy: A systematic review. J. Clin. Lipidol. 2008, 2, 328–334. [Google Scholar] [CrossRef]
- Luo, L.; Yuan, X.; Huang, W.; Ren, F.; Zhu, H.; Zheng, Y.; Tang, L. Safety of coadministration of ezetimibe and statins in patients with hypercholesterolaemia: A meta-analysis. Intern. Med. J. 2015, 45, 546–557. [Google Scholar] [CrossRef]
- Patel, J.; Martin, S.; Banach, M. The Therapeutic Challenges Faced by Statin Intolerance. Expert Opin. Pharm. 2016, 17, 1497–1507. [Google Scholar] [CrossRef]
- Strilchuk, L.; Fogacci, F.; Cicero, A.F. Safety and tolerability of injectable lipid-lowering drugs: An update of clinical data. Expert Opin. Drug Saf. 2019, 18, 611–621. [Google Scholar] [CrossRef]
- Fogacci, F.; Banach, M.; Mikhailidis, D.P.; Bruckert, E.; Toth, P.P.; Watts, G.F.; Reiner, Ž.; Mancini, J.; Rizzo, M.; Mitchenko, O. Safety of red yeast rice supplementation: A systematic review and meta-analysis of randomized controlled trials. Pharm. Res. 2019, 143, 1–16. [Google Scholar] [CrossRef]
- Strandberg, T.E.; Tilvis, R.S.; Miettinen, T.A. Variations of hepatic cholesterol precursors during altered flows of endogenous and exogenous squalene in the rat. Biochim. Biophys. Acta 1989, 1001, 150–156. [Google Scholar] [CrossRef]
- Xu, R.B.; Liu, W.W.; Wang, M.Y. Progress of Preparation and Application in Squalene. Shandong J. Med. 2005, 45, 69–70. [Google Scholar]
- Fang, X.D.; Miao, H. A study on the anti-senescense effect of squalene compound in rats and Drosoph melanogasters. J. Navy Med. 2004, 25, 289–291. [Google Scholar]
- Popa, O.; Babeanu, N.E.; Popa, I.; Nita, S.; Dinu-Parvu, E. Methods for obtaining and determination of squalene from natural sources. Biomed. Res. Int. 2015, 2015, 367202. [Google Scholar] [CrossRef]
- Pham, D.M.; Boussouira, B.; Moyal, D.; Nguyen, Q.L. Oxidization of squalene, a human skin lipid: A new and reliable marker of environmental pollution studies. Int. J. Cosmet. Sci. 2015, 37, 357–365. [Google Scholar] [CrossRef]
- Wolosik, K.; Knaś, M.; Zalewska, A.; Niczyporuk, M.; Przystupa, A.W. The importance and perspective of plant-based squalene in cosmetology. J. Cosmet. Sci. 2013, 64, 59–66. [Google Scholar]
- Kelly, G.S. Squalene and its potential clinical uses. Altern. Med. Rev. 1999, 4, 29–36. [Google Scholar]
- Lozano-Grande, M.A.; Gorinstein, S.; Espitia-Rangel, E.; Dávila-Ortiz, G.; Martínez-Ayala, L. Plant Sources, Extraction Methods, and Uses of Squalene. Int. J. Agron. 2018, 2018, 13. [Google Scholar] [CrossRef]
- De Stefani, E.; Ronco, A. Squalene: A multi-task link in the crossroads of cancer and aging. Funct. Foods Health Dis. 2013, 3, 462–476. [Google Scholar]
- Turchini, G.M.; Tocher, D.R. Fish Oil Replacement and Alternative Lipid Sources in Aquaculture Feed; CRC Press: Boca Raton, FL, USA, 2010. [Google Scholar]
- Bhattacharjee, P.; Singhal, R.S. Extraction of Squalene from Yeast by Supercritical Carbon Dioxid. World J. Microbiol. Biotechnol. 2003, 19, 605–608. [Google Scholar] [CrossRef]
- Lau, H.L.; Puah, C.W.; Choo, Y.M.; Ma, A.N.; Chuah, C.H. Simultaneous quantification of free fatty acids, free sterols, squalene, and acylglycerol molecular species in palm oil by high-temperature gas chromatography--flame ionization detection. Lipids 2005, 40, 523–528. [Google Scholar]
- Schnetzler, K.A.B.W. Food uses and amaranth product research: A comprehensive review. In Amaranth Biology, Chemistry and Technology; CRC Press: Boca Raton, FL, USA, 1994. [Google Scholar]
- Pappas, A. Epidermal surface lipids. Dermato-Endocrinology 2009, 1, 72–76. [Google Scholar] [CrossRef]
- Kostyuk, V.; Potapovitch, A.I.; Stancato, A.; Luca, C.D.; Lulli, D.; Pastore, S.; Korkina, L.G. Photo-oxidation products of skin surface squalene mediate metabolic and inflammatory responses to solar UV in human keratinocytes. PLoS ONE 2012, 7, e44472. [Google Scholar] [CrossRef]
- Tilvis, S.R.; Miettinen, T.A. Absorption and metabolic fate of dietary 3H-squalene in the rat. Lipids 1983, 18, 233–238. [Google Scholar] [CrossRef]
- Gylling, H.; Miettinen, T.A. Postabsorptive metabolism of dietary squalene. Atherosclerosis 1994, 106, 169–178. [Google Scholar] [CrossRef]
- Rajaratnam, R.A.; Gylling, H.; Miettinen, T.A. Serum squalene in postmenopausal women without and with coronary artery disease. Atherosclerosis 1999, 146, 61–64. [Google Scholar] [CrossRef]
- Scolastici, C.; Ong, T.P.; Moreno, F.S. Squalene does not exhibit a chemopreventive activity and increases plasma cholesterol in a Wistar rat hepatocarcinogenesis model. Nutr. Cancer 2004, 50, 101–109. [Google Scholar] [CrossRef]
- Zhang, Z.; Yeung, W.K.; Huang, Y.; Chen, Z. Effect of squalene and shark liver oil on serum cholesterol level in hamsters. Int J. Food Sci. Nutr. 2002, 53, 411–418. [Google Scholar] [CrossRef]
- Strandberg, T.E.; Tilvis, R.S.; Miettinen, T.A. Metabolic variables of cholesterol during squalene feeding in humans: Comparison with cholestyramine treatment. J. Lipid Res. 1990, 31, 1637–1643. [Google Scholar]
- Gabas-Rivera, C.; Barranquero, C.; Martínez-Beamonte, R.; Navarro, M.A.; Surra, J.C.; Osada, J. Dietary squalene increases high density lipoprotein-cholesterol and paraoxonase 1 and decreases oxidative stress in mice. PLoS ONE 2014, 9, e104224. [Google Scholar] [CrossRef]
- Shin, D.H.; Heo, H.J.; Lee, Y.J.; Kim, H.K. Amaranth squalene reduces serum and liver lipid levels in rats fed a cholesterol diet. Br. J. Biomed. Sci. 2004, 61, 11–14. [Google Scholar] [CrossRef]
- Khor, H.T.; Chieng, D.Y. Effect of squalene, tocotrienols and α-tocopherol supplementations in the diet on serum and liver lipids in the hamster. Nutr. Res. 1997, 17, 475–483. [Google Scholar] [CrossRef]
- Chan, P.; Tomlinson, B.; Lee, C.B.; Lee, Y.S. Effectiveness and safety of low-dose pravastatin and squalene, alone and in combination, in elderly patients with hypercholesterolemia. J. Clin. Pharm. 1996, 36, 422–427. [Google Scholar] [CrossRef]
- Miettinen, T.A.; Vanhanen, H. Serum concentration and metabolism of cholesterol during rapeseed oil and squalene feeding. Am. J. Clin. Nutr. 1994, 59, 356–363. [Google Scholar] [CrossRef]
- Liu, Y.; Xu, X.; Bi, D.; Wang, X.; Zhang, X.; Dai, H.; Chen, S.; Zhang, W. Influence of squalene feeding on plasma leptin, testosterone & blood pressure in rats. Indian J. Med. Res. 2009, 129, 150–153. [Google Scholar]
- Ravi Kumar, S.; Yamauchi, I.; Narayan, B.; Katsuki, A.; Hosokawa, M.; Miyashita, K. Squalene modulates fatty acid metabolism: Enhanced EPA/DHA in obese/diabetic mice (KK-Ay) model. Eur. J. Lipid Sci. Technol. 2016, 118, 1935–1941. [Google Scholar] [CrossRef]
- Smith, D.; Espino-Montoro, A.; Perez-Jimenez, F.; Pedro-Botet, J.; Perepez, J.J.; Ordovas, J.M. Effect of a high saturated fat and cholesterol diet supplemented with squalene or β-sitosterol on lipoprotein profile in fib hamsters. Nutr. Res. 2000, 20, 1309–1318. [Google Scholar] [CrossRef]
- de Castro, L.I.; Soares, R.A.; Saldiva, P.H.; Ferrari, R.A.; Miguel, A.M.; Almeida, C.A.; Arêas, J.A. Amaranth oil increased fecal excretion of bile Acid but had no effect in reducing plasma cholesterol in hamsters. Lipids 2013, 48, 609–618. [Google Scholar] [CrossRef]
- Kritchevsky, D.; Moyer, A.W.; Tesar, W.C.; Logan, J.B.; Brown, R.A.; Richmond, G. Squalene feeding in experimental atherosclerosis. Circ. Res. 1954, 2, 340–343. [Google Scholar] [CrossRef]
- Guillen, N.; Acín, S.; Navarro, M.A.; Perona, J.S.; Arbonés-Mainar, J.M.; Arnal, C.; Sarría, A.J.; Surra, J.C.; Carnicer, R.; Orman, I.; et al. Squalene in a sex-dependent manner modulates atherosclerotic lesion which correlates with hepatic fat content in apoE-knockout male mice. Atherosclerosis 2008, 197, 72–83. [Google Scholar] [CrossRef]
- Sabeena Farvin, K.H.; Anandan, R.; Kumar, S.H.S.; Shiny, K.S.; Sankar, T.V.; Kurumpan, T.T. Effect of squalene on tissue defense system in isoproterenol-induced myocardial infarction in rats. Pharm. Res. 2004, 50, 231–236. [Google Scholar] [CrossRef]
- Farvin, S.; Anandan, R.; Sankar, T.V.; Nair, V. Protective Effect of Squalene against Isoproterenol-Induced Myocardial Infarction in Rats. J. Clin. Biochem. Nutr. 2005, 37, 55–60. [Google Scholar] [CrossRef]
- Farvin, K.H.; Anandan, R.; Kumar, S.H.S.; Shiny, K.S.; Mathew, S.; Sankar, T.V.; Nair, P.G.V. Cardioprotective effect of squalene on lipid profile in isoprenaline-induced myocardial infarction in rats. J. Med. Food 2006, 9, 531–536. [Google Scholar] [CrossRef]
- Farvin, K.H.S.; Kumar, S.H.S.; Anandan, D.R.; Mathew, S.; Sankar, T.V.; Nair, P.G.V. Supplementation of squalene attenuates experimentally induced myocardial infarction in rats. Food Chem. 2007, 105, 1390–1395. [Google Scholar] [CrossRef]
- Dhandapani, N.; Ganesan, B.; Anandan, R.; Jeyakumar, R.; Rajaprabhu, D.; Ezhilan, R.A. Synergistic effects of squalene and polyunsaturated fatty acid concentrate on lipid peroxidation and antioxidant status in isoprenaline-induced myocardial infarction in rats. Afr. J. Biotechnol. 2007, 6, 1021–1027. [Google Scholar]
- Farvin, K.H.S.; Surendraraj, A.; Anandan, R. Protective Effect of Squalene on Endogenous Antioxidant Vitamins in Experimentally Induced Myocardial Infarction in Rats. Asian J. Biochem. 2009, 4, 133–139. [Google Scholar] [CrossRef]
- Motawi, T.M.; Sadik, N.A.; Refaat, A. Cytoprotective effects of DL-alpha-lipoic acid or squalene on cyclophosphamide-induced oxidative injury: An experimental study on rat myocardium, testicles and urinary bladder. Food Chem. Toxicol. 2010, 48, 2326–2336. [Google Scholar] [CrossRef]
- Preobrazhenskaya, N.S.; Pokrovskij, M.V.; Berezhnova, T.A.; Levchenko, Y.A. Hypolipidemic effects of Amaranth oil in Experimental Doxorubicine Cardiomyopathy. Res. J. Pharm. Biol. Chem. Sci. 2016, 7, 1017–1021. [Google Scholar]
- Meir, S.K.; Leitersdorf, E. Atherosclerosis in the apolipoprotein-E-deficient mouse: A decade of progress. Arter. Thromb. Vasc. Biol. 2004, 24, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Nelson, R.H. Hyperlipidemia as a risk factor for cardiovascular disease. Prim. Care 2013, 40, 195–211. [Google Scholar] [CrossRef] [PubMed]
- Trevor Huff, I.J. Physiology, Cholesterol [Updated 2019 Mar 13]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Frangogiannis, N.G. Pathophysiology of Myocardial Infarction. Compr. Physiol. 2015, 5, 1841–1875. [Google Scholar]
- Ramirez, A.; Hu, P.P. Low High-Density Lipoprotein and Risk of Myocardial Infarction. Clin. Med. Insights. Cardiol. 2015, 9, 113–117. [Google Scholar] [CrossRef]
- Cardiotoxicity and Cardiomyopathy. Available online: http://chemocare.com/chemotherapy/side-effects/cardiotoxicity-and-cardiomyopathy.aspx (accessed on 22 December 2019).
- Zaragoza, C.; Gomez-Guerrero, C.; Martin-Ventura, J.L.; Blanco-Colio, L.; Lavin, B.; Mallavia, B.; Tarin, C.; Mas, S.; Ortiz, A.; Egido, J. Animal Models of Cardiovascular Diseases. J. Biomed. Biotechnol. 2011, 2011, 13. [Google Scholar] [CrossRef]
- Dhesi, S.; Chu, M.P.; Blevins, G.; Paterson, I.; Larratt, L.; Oudit, G.Y.; Kim, D.H. Cyclophosphamide-Induced Cardiomyopathy: A Case Report, Review, and Recommendations for Management. J. Investig. Med. High. Impact Case Rep. 2013, 1, 2324709613480346. [Google Scholar] [CrossRef]
- Takemura, G.; Fujiwara, H. Doxorubicin-Induced Cardiomyopathy: From the Cardiotoxic Mechanisms to Management. Prog. Cardiovasc. Dis. 2007, 49, 330–352. [Google Scholar] [CrossRef]
- O’Connell, J.L.; Romano, M.M.; Campos Pulici, E.C.; Carvalho, E.E.; de Souza, F.R.; Tanaka, D.M.; Maciel, B.C.; Salgado, H.C.; Fazan-Júnior, R.; Rossi, M.A.; et al. Short-term and long-term models of doxorubicin-induced cardiomyopathy in rats: A comparison of functional and histopathological changes. Exp. Toxicol. Pathol. 2017, 69, 213–219. [Google Scholar] [CrossRef]
- Bartoli, C.R.; Brittian, K.R.; Giridharan, G.; Koenig, S.C.; Hamid, T.; Prabhu, S.D. Bovine model of doxorubicin-induced cardiomyopathy. J. Biomed. Biotechnol. 2011, 2011, 758736. [Google Scholar] [CrossRef]
- Omole, J.G.; Ayoka, O.A.; Alabi, Q.K.; Adefisayo, M.A.; Asafa, M.A.; Olubunmi, B.O.; Fadeyi, B.A. Protective Effect of Kolaviron on Cyclophosphamide-Induced Cardiac Toxicity in Rats. JEBIM. 2018, 23, 1–11. [Google Scholar] [CrossRef]
- Günes, S.; Sahinturk, V.; Karasati, P.; Sahin, I.K.; Ayhanci, A. Cardioprotective Effect of Selenium Against Cyclophosphamide-Induced Cardiotoxicity in Rats. Biol. Trace Elem. Res. 2015, 177, 107–144. [Google Scholar] [CrossRef] [PubMed]
- Leite Matos, S.; Paula, H.D.; Pedrosa, M.L.; Santos, R.C.D.; Oliveira, E.L.D.; Chianca Júnior, D.A.; Silva, M.E. Dietary models for inducing hypercholesterolemia in rats. Braz. Arch. Biol. Technol. 2005, 48, 203–209. [Google Scholar] [CrossRef]
- Dillard, A.; Matthan, N.R.; Lichtenstein, A.H. Use of hamster as a model to study diet-induced atherosclerosis. Nutr. Metab. 2010, 7, 89. [Google Scholar] [CrossRef] [PubMed]
- Russell, C.J.; Proctor, S.D. Small animal models of cardiovascular disease: Tools for the study of the roles of metabolic syndrome, dyslipidemia, and atherosclerosis. Cardiovasc. Pathol. 2006, 15, 318–330. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, K.; Hagi, A.; Inoue, Y. The relationship between plasma high density lipoprotein cholesterol levels and cholesteryl ester transfer protein activity in six species of healthy experimental animals. Biol. Pharm. Bull. 2001, 24, 579–581. [Google Scholar] [CrossRef]
- Dalboge, L.S.; Pedersen, P.J.; Hansen, G.; Fabricius, K.; Hansen, H.H.; Jelsing, J.; Vrang, N. A Hamster Model of Diet-Induced Obesity for Preclinical Evaluation of Anti-Obesity, Anti-Diabetic and Lipid Modulating Agents. PLoS ONE 2015, 10, e0135634. [Google Scholar] [CrossRef]
- Ferdowsian, R.H.; Barnard, N.D. Effects of plant-based diets on plasma lipids. Am. J. Cardiol. 2009, 104, 947–956. [Google Scholar] [CrossRef]
- Kokubo, Y. Prevention of Hypertension and Cardiovascular Diseases. Hypertension 2014, 63, 655–660. [Google Scholar] [CrossRef]
- Kontush, A.; Chapman, M.J. Antiatherogenic function of HDL particle subpopulations: Focus on antioxidative activities. Curr. Opin. Lipidol. 2010, 21, 312–318. [Google Scholar] [CrossRef]
- Breslow, J.L. n-3 fatty acids and cardiovascular disease. Am. J. Clin. Nutr. 2006, 83, 1477s–1482s. [Google Scholar] [CrossRef]
- Burr, M.L.; Fehily, A.M.; Gilbert, J.F.; Rogers, S.; Holliday, R.M.; Sweetnam, P.M.; Elwood, P.C.; Deadman, N.M. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: Diet and reinfarction trial (DART). Lancet 1989, 2, 757–761. [Google Scholar] [CrossRef]
- Singh, R.B.; Niaz, M.A.; Sharma, J.P.; Kumar, R.; Rastogi, V.; Moshiri, M. Randomized, double-blind, placebo-controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: The Indian experiment of infarct survival-4. Cardiovasc Drugs 1997, 11, 485–491. [Google Scholar] [CrossRef] [PubMed]
- GISSI-Prevenzione Investigators. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: Results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. Lancet 1999, 354, 447–455. [Google Scholar] [CrossRef]
- Takeuchi, N.; Yamamura, Y. Cholesterol esterification and cholesterol ester hydrolysis by liver homogenates in rats with accelerated cholesterol metabolism. Atherosclerosis 1973, 17, 211–224. [Google Scholar] [CrossRef]
- Insull, W., Jr. The pathology of atherosclerosis: Plaque development and plaque responses to medical treatment. Am. J. Med. 2009, 122, S3–S14. [Google Scholar] [CrossRef]
- Garelnabi, M.; Lor, K.; Jin, J.; Chai, F.; Santanam, N. The paradox of ApoA5 modulation of triglycerides: Evidence from clinical and basic research. Clin. Biochem. 2013, 46, 12–19. [Google Scholar] [CrossRef]
- Patil, N.; Chavan, V.; Karnik, N.D. Antioxidant status in patients with acute myocardial infarction. Indian J. Clin. Biochem. IJCB 2007, 22, 45–51. [Google Scholar] [CrossRef]
- Srinivas, K.; Bhaskar, M.V.; Aruna Kumari, R.; Nagaraj, K.; Reddy, K.K. Antioxidants, lipid peroxidation and lipoproteins in primary hypertension. Indian Heart J. 2000, 52, 285–288. [Google Scholar]
- Bernard, R. Nomenclature and criteria for diagnosis of ischemic heart disease. Report of the Joint International Society and Federation of Cardiology/World Health Organization task force on standardization of clinical nomenclature. Circulation 1979, 59, 607–609. [Google Scholar]
- Dolci, A.; Panteghini, M. The exciting story of cardiac biomarkers: From retrospective detection to gold diagnostic standard for acute myocardial infarction and more. Clin. Chim. Acta 2006, 369, 179–187. [Google Scholar] [CrossRef]
- Ladenson, J.H. A personal history of markers of myocyte injury [myocardial infarction]. Clin. Chim. Acta 2007, 381, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Mythili, S.; Malathi, N. Diagnostic markers of acute myocardial infarction. Biomed. Rep. 2015, 3, 743–748. [Google Scholar] [CrossRef] [PubMed]
- Ramana, K.V.; Srivastava, S.; Singhal, S.S. Lipid Peroxidation Products in Human Health and Disease. Oxidative Med. Cell. Longev. 2013, 2013, 3. [Google Scholar] [CrossRef] [PubMed]
- Brindha, E.; Rajasekapandiyan, M. Preventive Effect of Phytic Acid on Isoproterenol-Induced Cardiotoxicity in Wistar Rats. Int. J. Biomed. Sci. IJBS 2015, 11, 35–41. [Google Scholar]
- Kumar, N.; Kumar, S.; Kumar, A.; Shakoor, T.; Rizwan, A. Lipid Profile of Patients with Acute Myocardial Infarction (AMI). Cureus 2019, 11, e4265. [Google Scholar] [CrossRef]
- Syed Nauman Ali, M.B.; Mubasher, S. Pattern of Dyslipidemia in Young Patients with ST Elevation Myocardial Infarction. JSZMC 2016, 7, 998–1001. [Google Scholar]
- Kumar, P.S.S.; Prasad, S.; Yadav, U.P.; Agrawal, P.K. Study of Lipid Profile in Acute Myocardial Infarction within 24 Hours. AABS 2018, 5, A1–A7. [Google Scholar] [CrossRef]
- Brooks, W.W.; Conrad, C.H. Isoproterenol-induced myocardial injury and diastolic dysfunction in mice: Structural and functional correlates. Comp. Med. 2009, 59, 339–343. [Google Scholar]
- Culav, M.E.; Clark, C.H.; Merrilees, M.J. Connective Tissues: Matrix Composition and Its Relevance to Physical Therapy. Phys. Ther. 1999, 79, 308–319. [Google Scholar] [CrossRef]
- Montpetit, M.L.; Stocker, P.J.; Schwetz, T.A.; Harper, J.M.; Norring, S.A.; Schaffer, L.; North, S.J.; Jang-Lee, J.; Gilmartin, T.; Head, S.R. Regulated and aberrant glycosylation modulate cardiac electrical signaling. Proc. Natl. Acad. Sci. USA 2009, 106, 16517–16522. [Google Scholar] [CrossRef]
- Viswanatha Swamy, A.H.M.; Patel, U.M.; Koti, B.C.; Gadad, P.C.; Patel, N.L.; Thippeswamy, A.H. Cardioprotective effect of Saraca indica against cyclophosphamide induced cardiotoxicity in rats: A biochemical, electrocardiographic and histopathological study. Indian J. Pharmacol. 2013, 45, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Rajakannu, S.; Ragavendran, B.; Gnanapragasam, A.; Yogeeta, S.K.; Devaki, T. Biochemical study on the protective potential of Nardostachys jatamansi extract on lipid profile and lipid metabolizing enzymes in doxorubicin intoxicated rats. Die Pharm. 2007, 62, 382–387. [Google Scholar]
- Pound, P.; Ebrahim, S.; Sandercock, P.; Bracken, M.B.; Roberts, I. Where is the evidence that animal research benefits humans? BMJ 2004, 328, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Boren, J.; Williams, K.J. The central role of arterial retention of cholesterol-rich apolipoprotein-B-containing lipoproteins in the pathogenesis of atherosclerosis: A triumph of simplicity. Curr. Opin. Lipidol. 2016, 27, 473–483. [Google Scholar] [CrossRef]
- Shapiro, D.M.; Fazio, S. Apolipoprotein B-containing lipoproteins and atherosclerotic cardiovascular disease. F1000Research 2017, 6, 134. [Google Scholar] [CrossRef]
- Relas, H.; Gylling, H.; Miettinen, T.A. Dietary squalene increases cholesterol synthesis measured with serum non-cholesterol sterols after a single oral dose in humans. Atherosclerosis 2000, 152, 377–383. [Google Scholar] [CrossRef]
- Lindsey, C.A., Jr.; Wilson, J.D. Evidence for A Contribution By The Intestinal Wall To The Serum Cholesterol Of The Rat. J. Lipid Res. 1965, 6, 173–181. [Google Scholar]
- AbuMweis, S.S.; Jew, S.; Jones, P.J. Optimizing clinical trial design for assessing the efficacy of functional foods. Nutr Rev. 2010, 68, 485–499. [Google Scholar] [CrossRef]
- Lucey, A.; Heneghan, C.; Kiely, M.E. Guidance for the design and implementation of human dietary intervention studies for health claim submissions. Nutr. Bull. 2016, 41, 378–394. [Google Scholar] [CrossRef]
| Study | Disease/ Condition | Study Type / SQ Source | Sample/ Population | Methodology | Results (SQ and CVD Only) | Comments/Outcomes |
|---|---|---|---|---|---|---|
| Study 1 Khor and Chieng 1997 [48] | Hyperlipidemia | Animal study Obtained from Sigma, St. Louis, MO, USA | Male Syrian hamsters (123 ± 2 g) The animals were randomly assigned into four groups. | The hamsters were fed with semi-synthetic diet containing 20% (w/w) of fat and a palm oil triacylglycerol (POTG) fraction isolated from commercial palm olein. They were divided into 4 groups: a) POTG b) POTG + SQ (POTG-SQ) c)POTG + SQ + pure tocotrienols (POTG-SQ-T3) d) POTG+ SQ and α-tocopherol (POTG-SQ- αT). The animals were fed accordingly for 45 days. SQ, T3, and α-T were supplemented at concentrations of 0.1%, 162 ppm, and 72 ppm, respectively. At the end of the treatment period, fasting blood samples were taken for the measurement of serum TC, HDL-C, TAG, and LDL-C. The livers were excised for measurement of liver lipids. | Serum: SQ-alone supplementation had significantly lowered (p < 0.05) serum TC levels as compared to the POTG group SQ-alone supplementation also lowers HDL-C, LDL-C, and TAG levels, but the reduction was not significant (p > 0.05) as compared to the POTG group. Liver: SQ-alone supplementation had significantly increased liver total lipids (p < 0.0l) and TC levels (p < 0.05). SQ-alone supplemented group had elevated the liver TAG level, while other liver lipids such as diacylglycerols (DAG), monoacylglycerols (MAG), free fatty acids (FFA), and phospholipids (PL) were not affected. | Squalene supplemented in short-term period (45 days) at a low level (0.1%) reduced serum TC. The ability of squalene to lower serum TC might be enhanced by cholesterol esterification activity in the liver. |
| Study 2 Shin et al. 2004 [47] | Hyperlipidemia | Animal study Amaranth SQ (in-house extraction) Shark liver SQ (obtained from Sigma, St. Louis, MO) | Male Sprague Dawley rats (110–130 g) Randomly divided into three groups | All rats were fed with 1% cholesterol diet for four weeks to induce hypercholesterolemia and were assigned into i) group 1: injected with saline (control) ii) group 2: injected with amaranth SQ (AS) iii) group 3: injected with shark liver SQ (SS) Both treatment groups, AS and SS, were injected at 200 mg/kg via intraperitoneal route for seven days prior to the sacrifice. Fecal samples were collected for the last 3 days for analysis of steroid excretion. Blood samples were analyzed for serum and liver lipids. The liver was excised to obtain liver microsomes for HMG-CoA reductase activity. | AS injection to the rats caused significant(p < 0.05) decrease in serum (TC and TG) and hepatic (cholesterol and TG) profiles compared to control and SS groups. Serum HDL-C levels in the AS group were significantly increased, resulting in a 45% reduction in atherogenic index. The AS group also significantly (p< 0.05) increased in fecal excretions of cholesterol and bile acid and slightly inhibited HMG-CoA reductase activity. However, these effects were not observed in SS-injected group. | Amaranth SQ (AS), which represents a plant source of SQ, exerts better hypolipidemic effects compared to the shark liver SQ (animal source of SQ). The authors concluded that the cholesterol-lowering effect of amaranth SQ might be mediated by the following:
|
| Study 3 Liu et al. 2009 [51] | Hyperlipidemia | Animal study Obtained from Healthy Nature Resource Inc | 40 male Wistar rats (22 days old) Randomly divided into two groups (20 rats per group) | The two groups were fed with the following diet for four weeks:
When the rats were 51 days old (day 0 after the SQ withdrawal) and 75 days old (day 24 after the SQ withdrawal), ten rats from each SQ and control group were sacrificed. Blood samples were collected for measurements of leptin, glucose, cholesterol, and triglycerides. Tail arterial blood pressure (BP) and body weight were monitored weekly. | Following SQ feeding, BP and body weight gain were lower in the SQ group. BP was significantly lower from 47 days of age in the squalene-fed group compared to controls (p < 0.01). Plasma leptin, glucose, cholesterol, and triglycerides in SQ fed rats group were significantly lower compared to the control group at 51 and 75 days of age (p < 0.05). | Squalene may counteract the increase in body fat, BP, and levels of plasma leptin, glucose, cholesterol, and triglycerides. Squalene may act as an alternative treatment for clinical management of high blood pressure (BP) and obesity. |
| Study 4 Gabas-Rivera et al. 2014 [46] | Hyperlipidemia | Animal study The source was not disclosed. | Male wild-type (WT), Apo E-deficient and Apoa1-deficient mice on C57BL/6J genetic background Following baseline blood samples, groups with similar initial plasma cholesterol were established. | All mice were fed chow semi-purified diets and divided into
The animals were fed the experimental diets for 11 weeks. Following the intervention, blood was sampled for measurement: a) plasma parameters TC, TG, HDL-C, nonesterified fatty acids, and aryl esterase; b) lipoprotein profiles VLDL, LDL, and HDL; and c) oxidative stress variable ROS levels in lipoprotein fractions. | Plasma parameters WT mice: The supplementation of SQ at 1 g/kg BW significantly increased HDL-C, nonesterified fatty acids, and aryl esterase activity when compared to the control group (p < 0.05). Apoa1-deficient mice: The supplementation of SQ at 1 g/kg BW significantly increased HDL-C and aryl esterase activity when compared to the control group (p < 0.05). Apo E-deficient mice: The supplementation of SQ at 1 g/kg BW significantly increased HDL-C when compared to the control and 0.25 g/kg BW SQ-treated groups (p < 0.05). The supplementation of SQ at 0.25 g/kg BW significantly increased total cholesterol when compared to the control and 1 g/kg SQ-treated groups (p < 0.01). Lipoprotein profiles WT mice: The administration of SQ at 1 g/kg BW induced an increase in HDL cholesterol that was accompanied by increased HDL phosphatidylcholine, whilst no changes in sphingomyelin and Apoa1 and redistribution of Apoa4 towards smaller HDL particles were observed. Apoa1-deficient mice: The administration of SQ at 1 g/kg BW did not have any effect on cholesterol distribution, decreased phosphatidylcholine, and increased Apoa4 in HDL particles and did not modify HDL sphingomyelin but decreased this phospholipid in LDL. Apo E-deficient mice: The SQ administration at either studied dose had little effect on cholesterol, esterified cholesterol, phosphatidylcholine, and sphingomyelin. However, it increased the presence of Apoa4 in HDL and decreased LDL Apoa4. Oxidative stress WT mice: The supplementation of SQ at 1 g/kg BW significantly reduced levels of ROS in isolated VLDL, LDL (p < 0.01), and HDL(p < 0.05) as well as plasma malondialdehyde (MDA) levels (p < 0.01) compared to the control group. Apoa1-deficient mice: The supplementation of SQ at 1 g/kg BW significantly reduced levels of ROS in isolated LDL (p < 0.01) and HDL (p < 0.05) compared to the control group. Apo E-deficient mice: The supplementation of SQ at 1 g/kg BW significantly reduced levels of ROS in isolated VLDL (p < 0.01) and HDL (p < 0.05) as well as plasma malondialdehyde (p < 0.01) compared to the control group. The supplementation of SQ at 0.25 g/kg BW significantly reduced levels of ROS in isolated VLDL (p < 0.01), HDL (p < 0.01), and LDL + HDL (p < 0.05) as well as plasma malondialdehyde (p < 0.01) compared to the control group. | SQ supplemented at a high dose (1 g/kg) for a long-term administration (11 weeks) significantly increased HDL-C level with independence of the genetic background without elevating TC level. SQ supplementation can modify HDL composition depending on the presence of Apo E and Apoa1. SQ supplementation can elicit an antioxidant action by decreasing oxidative stress level in lipoprotein fractions. |
| Study 5 Kumar et al. 2016 [52] | Hyperlipidemia | Animal study Obtained from Wako Pure Chemicals, Ltd., Osaka, JP | Obese/diabetic model KK-Ay mice (male, four weeks age) The mice were randomly divided into control and experimental groups (n = 7). | The groups were as follows:
At the end of the experiment (4 weeks), all animals were sacrificed to collect blood and other organs. Measurement involved
| There was a significant decrease in the liver and epididymal WAT TG of SQ fed experimental groups as compared to control (p < 0.05). TG levels in serum and cholesterol levels in serum, liver, and epididymal WAT were not significantly different from control(p > 0.05). There was a significant increment in proportions of the long-chain n-3 fatty acid, DHA, in the squalene-fed group when compared to control (p < 0.05). | SQ influenced the lipid metabolism as seen by the TG levels and fatty acid profiles in the test diet fed to KK-Ay mice. SQ potentially exhibits a hypotriglyceridemic effect. |
| Study 6 Smith et al. (2000) [53] | Hyperlipidemia | Animal study Obtained from Sigma, St. Louis, MO | Thirty-six male adult F1B hamsters (170 to 250 g) During phase three, the animals were randomly assigned to three different diet groups (12 animals each). | This study was divided into three phases: phase 1 (acclimatization): the animals were fed with a normal chow diet; phase 2: the animals were fed with a high-fat diet for four weeks; and phase 3: the animals were randomly assigned to the following three groups for four weeks: i) group 1 continued with the same high-fat diet, ii) group 2 was fed a high-fat diet supplemented with 1% SQ, and iii) group 3 was fed a high-fat diet plus 0.5% β-sitosterol. At the end of each phase, major lipoproteins, namely chylomicrons, VLDL + IDL, and HDL were isolated and their concentrations were measured. | Cholesterol: During phase 3, both un-supplemented and SQ-supplemented groups (groups 1 and 2) showed significant increases in cholesterol content in VLDL + IDL (p< 0.01) compared with their phase 2 values. There were no significant changes observed in any of the groups on LDL-C and HDL-C levels. Triglycerides/ HDL and LDL-C ratios: During phase 3, group 1 and group 2 had comparable plasma triglyceride levels. The SQ-supplemented group (Group 2) significantly increased plasma triglyceride and LDL-C/HDL-C ratio in comparison to the level at phase 1. | Under this experimental condition, SQ supplementation at 1% of the total diet did not produce hypocholesterolemic and hypotriglyceridemic effects in the high-fat diet hamsters. |
| Study 7 Zhang (2002) [44] | Hyperlipidemia | Animal study Obtained from Sigma, St. Louis, MO | Thirty male Golden Syrian hamsters (95 ± 5 g) Divided into five groups (n = 6) | Each group was fed with one of the following diets for 4 weeks: 1. high-fat diet (HFD); 2. HFD + 0.05% pure SQ; 3. HFD + 0.1% pure SQ; 4. HFD + 0.5% pure SQ; and 5. HFD + 0.05% SQ-containing shark liver oil (SLO). At the end of the treatment, blood was sampled for serum lipid measurements. Livers, heart, and adipose tissue were collected for cholesterol measurement. | Elevation in serum TC in all groups supplemented with SQ (groups 2 to 5) In comparison to the control, serum TC was significantly (p < 0.05) increased in groups 2 and 4. A similar trend was observed for serum TG. Significant elevation in serum HDL-C in the 0.1% SQ and 0.5% SQ groups but not in the 0.05% SQ group as compared with the control hamsters No significant differences in serum non-HDL-C were observed among the five groups. SQ supplemented at 0.5% had significantly increased the cholesterol level in the liver and adipose tissue compared to the control. No differences in the cholesterol levels in the heart were observed among the five groups. | The investigators had concluded that SQ exerts a hypercholesterolemic effect at least in hamsters. Thus, caution must be exercised when SQ is routinely consumed as supplements. |
| Study 8 Castro et al. 2013 [54] | Hyperlipidemia | Animal study Amaranth oil (in-house extraction) | Forty-six male Golden Syrian strain hamsters, weanling (approximately 21 days), of sanitary standard type The animals were randomly divided into five groups. | Following seven days of adaptation, the rats were fed with commercial diet. Prior to further dietary regimen, six animals were randomly selected and fasted for 8 h before blood collection. The remaining 40 animals were divided into groups according to different diets and were fed for four weeks: i) control was fed a balanced diet containing 20% corn oil as the lipid source; ii) hypercholesterolemic was identical to the control group but contained 12% coconut oil, 8% corn oil, and 0.1% cholesterol as the lipid source; iii) Amaranth oil was identical to the hypercholesterolemic group but substitute corn oil with amaranth oil; and iv) squalene was identical to the hypercholesterolemic group but admixed with SQ in the ratio found in amaranth oil. At the end of the experiment, the animals were sacrificed for blood and liver collection. The following parameters were included: a) analyses in plasma (TC, TG, and HDL-C) and non-HDL-C (LDL-C + VLDL-C), b) analyses in the liver: liver weight and hepatic cholesterol concentration, c) histological analysis: haematoxylin and eosin, and d) analyses in the feces: cholesterol and bile acids. | There was a significant increase in all lipid profile parameters in the amaranth oil and SQ groups when compared to the control group (p < 0.05). Fecal excretion of bile acids was significantly greater in the amaranth oil and SQ groups as compared to the control group (p < 0.05). The liver weight was significantly increased in the SQ group compared to the control group (p < 0.05). | The consumption of amaranth oil and its SQ component did not exert a hypocholesterolemic effect in hamsters fed on a high-fat diet but promoted an increase in fecal excretion of bile acids. |
| Study | Disease/ Condition | Study Type/ SQ Source | Sample/ Population | Methodology | Results (SQ and CVD only) | Comments/Outcomes |
|---|---|---|---|---|---|---|
| Study 1 Kritchevsky et al. (1954) [55] | Atherosclerosis | Animal study Purchased from Distillation Products Inc, Rochester, NY, USA. | Male rabbits (1.5 to 2 kg) Divided into five groups | Rabbits were randomly divided into five groups as follows: group I: normal diet (N), group II: N + SQ, group III: N + SQ (14 weeks), group IV: N + cholesterol, and group V: N + SQ + cholesterol. The treatments were prepared at 3% of the total diet and were mixed with corn oil. All groups were maintained on the diets for seven weeks, except for group III (14 weeks duration). After the treatment, the livers were weighed and assayed for total non-saponifiable material, cholesterol, and SQ. The aortas were visually examined for atherosclerotic lesions and were graded on a 0 to 4 plus scale (in the order of increasing severity). Ultra-centrifugal examination of the serum for β-lipoproteins was also performed. | a) Atheromatous lesions: SQ-alone-supplemented groups (II and III) did not develop lesion and corresponded to those seen in group I. The cholesterol- alone (group IV) and SQ + cholesterol feeding (group V) showed the highest degrees of average atheroma. b) Liver weight and total non-saponifiable material: The liver weight of seven-week squalene supplementation (group II) increased markedly when compared to the normal group (group I). There was an increase in total non-saponifiable material in all groups (II–V) compared to the normal group, with a much greater increase in groups IV and V. c) Serum β-lipoproteins: The animals on the seven-week squalene diet showed no increase in their serum lipoproteins. As squalene feeding continued, there was an increase in the serum levels. | Supplementation of SQ may be regarded as a source of endogenous cholesterol and did not cause atherosclerosis. Exogenous cholesterol played a more important role in the development of atherosclerosis than endogenous cholesterol. SQ might increase liver weight and total non-saponifiable material; however, no development of atheroma was observed. |
| Study 2 Guill´en et al. 2008 [56] | Atherosclerosis | Animal study Source of SQ was not disclosed. | Homozygous ApoE knockout mice (aged 2 months) Divided according to sex (17 males, 15 females) | Both groups (male and female) were fed on a standard chow diet and were assigned into two groups with different beverages: i) SQ group, 1% (v/v) glycerol solution supplemented in squalene to provide a dose of 1 g/kg/day and ii) control group, glycerol solution (vehicle). Duration of treatment: Ten weeks At the end of the treatment, the mice were sacrificed for blood collection and heart excision. Measurement involved a) plasma lipid and lipoprotein, b) liver parameters, c) area of atherosclerotic lesion, d) antioxidant defenses (paraoxonase activity and isoprostane levels), and e) hepatic apolipoprotein. | One% SQ supplemented in beverage significantly decreased plasma cholesterol, triglycerides, and Apoa1 in females (p < 0.05), while there was no change in males. The liver weight was significantly decreased in males consuming SQ (p < 0.05), while this effect was not evident in females. Male mice receiving SQ showed a significant decrease in fat in the liver (p < 0.05). Males receiving SQ showed a significant decrease in the lesion (p < 0.01), while female mice showed no change in their lesion area. In males, there was a high statistically significant direct correlation (rs = 0.81; p < 0.000) between hepatic weight and plasma triglycerides. A statistically significant direct association (rs = 0.64; p < 0.02) was also observed between the lesion area and hepatic fat accumulation. SQ intake significantly decreased plasma levels of 8-isoprostaglandin F2 in both sexes (p < 0.05). No significant change in hepatic Apoa1 mRNA levels in both sexes Male mice receiving SQ showed significantly increased Apoa5 expression (p < 0.01). | The administration of SQ modulates lesion development in a sex-specific manner. The accumulation of hepatic fat by the liver is highly correlated with lesion progression in males. SQ administration could be used as a safe alternative to alleviate atherosclerosis and hepatic steatosis, particularly in males. |
| Study | Disease/ Condition | Study Type/ SQ Source | Sample/ Population | Methodology | Results (SQ and CVD only) | Comments/Outcomes |
|---|---|---|---|---|---|---|
| Study 1 Farvin et al. 2004 [57] | Myocardial infarction | Animal study Isolated from fresh shark liver | Wistar strain male albino rats (100–120 g) Divided into four groups (six rats per group) | Following 7-day acclimatization, the rats were divided according to groups, were fed on a standard diet with added oils for 45 days, and were injected with saline or isoproterenol for 2 days. Isoproterenol was used to induce myocardial infarction in rats. Group I (control): 2% coconut oil and injected with saline Group II (control): 2% SQ and injected with saline Group III: 2% Coconut oil and injected with isoproterenol Group IV: 2% SQ and injected with isoproterenol At the end of the experiment (24 h after last isoproterenol injection), the rats were sacrificed for blood collection and heart excision. Measurement involved a) antioxidant enzymes GPx and GST, and b) anti-peroxidative enzymes CAT and SOD. | The prior treatment with SQ had significantly increased the activities of antioxidant enzymes (GPx and GST) and anti-peroxidative enzymes (CAT and SOD) in the heart tissue of group IV as compared to group III isoproterenol-induced myocardial infarcted rats (p < 0.001). The normal rats receiving SQ alone (group II) did not show any significant change in comparison to the control (group I). | SQ supplementation possesses a cardioprotective effect due to their antioxidant property. No adverse effect following a low dose of SQ supplementation (at 2%) |
| Study 2 Farvin et al. 2005 [58] | Myocardial infarction | Animal study Shark liver oil of Centrophorus sp. caught in Andaman waters | Wistar male albino rats (100–120 g) Divided into four groups (six rats per group) | All rats were fed on a standard diet with added oils for 45 days and were injected with saline or isoproterenol for 2 days according to the groups. Isoproterenol was used to induce myocardial infarction in rats. Group I (control): 2% coconut oil and injected with saline Group II (control): 2% SQ and injected with saline Group III: 2% coconut oil and injected with isoproterenol Group IV: 2% SQ and injected with isoproterenol At the end of the experiment, (24 h after last isoproterenol injection), the rats were sacrificed for blood collection and heart excision. Measurement involved a) diagnostic marker enzymes, b) membrane-bound ATPase (Na+, K+ ATPase, and Ca2+ ATPase) activities and mineral status (sodium, potassium, and calcium), and c) lipid peroxidation and GSH | The pretreatment of 2% SQ in the diet had significantly reduced the release of diagnostic marker enzymes (ALT, AST, LDH, and CPK) into the systemic circulation as compared to group III rats (p < 0.001). The pretreatment of 2% SQ in the diet also had significantly counteracted the isoproterenol-induced lipid peroxidation and maintained the level of GSH at near normalcy in group IV rats as compared to group III animals (p < 0.001). SQ supplementation exerted membrane-stabilizing action against isoproterenol-induced myocardial infarction by maintaining the activities of membrane-bound ATPase (Na+, K+ ATPase, and Ca2+ ATPase) activity in the heart tissue and the mineral status (sodium, potassium, and calcium) in plasma and heart tissue at near-normal levels. | The cardioprotective effect of SQ might be contributed by the antioxidant property and membrane-stabilizing action. |
| Study 3 Farvin et al. 2006 [59] | Myocardial infarction | Animal study Isolated from fresh shark liver | Male Wistar strain albino rats (120–150 g) Divided into four groups (six rats per group) | All animals were fed on a standard diet with added oils for 45 days and injected with saline/isoproterenol for 2 days according to the groups. Isoproterenol was used to induce myocardial infarction (MI) in rats. Group I (control): 2% coconut oil and injected with saline Group II (control): 2% SQ and injected with saline Group III: 2% coconut oil and injected with isoproterenol Group IV: 2% SQ and injected with isoproterenol At the end of the experiment, (24 h after last isoproterenol injection), the rats were sacrificed for blood collection and heart tissue excision Measurement involved
| For normal rats (group I vs group II), SQ supplementation to the normal rats (group II) had significantly increased plasma HDL-C levels compared to the group I normal control rats (p < 0.01). Plasma lipid peroxidation in group II (normal squalene-fed rats) showed a slight decline as compared with group I normal control animals (p < 0.05). For MI-induced rats (group III vs group IV), both plasma and heart tissue levels of cholesterol, TG, free fatty acids, phospholipids, and LDL-C in MI-induced rats in group IV were significantly decreased in comparison to that of group III (p < 0.001). In contrast, the HDL-C level in group IV had also significantly increased compared to Group III. Both plasma and heart tissue lipid peroxidation in group IV MI-squalene fed were significantly decreased when compared with group III MI-control rats (p < 0.001). | The pre-administration of 2% SQ for 45 days prevents the symptoms of isoprenaline-induced myocardial infarction in rats. The cardioprotective effect of SQ might be related to its ability to inhibit lipid accumulation by
|
| Study 4 Farvin et al. 2007 [60] | Myocardial infarction | Animal study Isolated from fresh shark liver | Twenty-four Wistar strain male albino rats (120–150 g) Divided into four groups of six rats per group | All rats were fed on a standard diet with added oils for 45 days and were injected with saline or isoproterenol for 2 days according to the groups. Isoproterenol was used to induce myocardial infarction in rats. Group I (control): 2% coconut oil and injected with saline Group II (control): 2% SQ and injected with saline Group III: 2% coconut oil and injected with isoproterenol Group IV: 2% SQ and injected with isoproterenol At the end of the experiment, (24 h after last isoproterenol injection), the rats were sacrificed for blood collection and heart tissue excision. Measurement involved a) protein content, b) hexose and hexosamine content, c) lipid peroxidation in the presence of promoters (ascorbic acid, ferrous sulphate, and tert-butyl hydroperoxide), and d) GSH | The pretreatment of 2% SQ (group IV) had significantly decreased the level of protein, hexose, and hexosamine in both plasma and heart tissue (p < 0.05). The group had also significantly increased in the level of GSH and maintained it to near normalcy (p < 0.05). In the presence of promoters (ascorbic acid, ferrous sulphate, and tert-butyl hydroperoxide) in the heart tissue, group IV (MI-SQ) had significantly decreased (p < 0.05) lipid peroxidation levels when compared to the control group (group III MI-control rats). The normal rats receiving squalene (group II) showed a significant change (p < 0.05) for the level of protein and hexose in the heart tissue when compared with normal control rats (group I). | The pretreatment of SQ might exert cardioprotective effects by preventing isoprenaline-induced necrotic damage to the myocardial cell membrane by its membrane-stabilizing and antioxidant properties. |
| Study 5 Dhandapani et al. 2007 [61] | Myocardial infarction | Animal study Shark liver oil Centrophorus sp. caught in the Andaman waters | Forty-eight Wistar strain male albino rats (120–150 g) Divided into four groups of 12 rats per group | The rats were fed on commercial feed added with the following oils at a 2% level for 60 days: group 1: coconut oil, group 2: SQ, group 3: PUFA concentrate, and group 4: SQ + PUFA concentrate. After 60 days, each group was further subdivided into eight groups of six rats per group: 1) groups 1a and 1b; 2a and 2b; 3a and 3b; and 4a and 4b, were i.p. injected with only saline for two days (control animals) and 2) groups 1b, 2b, 3b, and 4b rats were i.p. injected with isoprenaline for two days to induce myocardial infarction. At the end of the experimental period, the rats were sacrificed for blood collection and heart excision. Measurement involved 1) diagnostic marker enzymes (ALT, AST, LDH, and CPK) and 2) lipid peroxides (LPO), reduced glutathione (GSH), and antioxidant enzymes. | Pre-supplementation with SQ alone (Group 2b) had significantly reduced the release of these enzymes (ALT, AST, LDH, and CPK) from the myocardium into the systemic circulation as compared to group 1b isoprenaline-administered rats (p < 0.001). Pre-supplementation with SQ alone (group 2b) had significantly reduced the LPO (p < 0.001) and significantly elevated GSH and antioxidant enzymes when compared to group 1b isoprenaline-administered rats (p < 0.001). Th normal SQ-fed rats (group 2a) showed no significant changes when compared to normal control rats (group 1a) rats. | Supplementation of SQ significantly counteracts the isoprenaline-induced elevations in the levels of diagnostic marker enzymes and LPO and is able to maintain the level of antioxidant enzymes at near normalcy. The administration of SQ may exert significant cardioprotection against isoprenaline intoxication. |
| Study 6 Farvin et al. 2009 [62] | Myocardial infarction | Animal study Shark liver oil Centrophorus sp. caught in the Andaman waters | Male Wistar strain albino rats (120–150 g) Divided into four groups of six rats per group. | All animals were fed on a standard diet with added oils for 45 days and injected with saline/isoproterenol for 2 days according to the groups. Isoproterenol was used to induce myocardial infarction in rats. Group I (control): 2% coconut oil and injected with saline Group II (control): 2% SQ and injected with saline Group III: 2% coconut oil and injected with isoproterenol Group IV: 2% SQ and injected with isoproterenol At the end of the experimental period (24 h after the last isoproterenol injection), the animals were sacrificed for blood collection and heart tissue excision. Measurement involved 1) ascorbic acid, 2) alpha tocopherol, and 3) endogenous squalene content. | Prior administration of 2% SQ in the diet (group IV) significantly increased the endogenous antioxidants (vitamin C and vitamin E) compared to MI-control rats (group III) (p < 0.001). The administration of 2% SQ in the diet also significantly restored the membrane-bound SQ content in the heart tissue compared to MI-control rats (group III) (p < 0.001). | SQ supplementation potentially exerts a deleterious effect of isoprenaline-induced aberration in endogenous antioxidant vitamins in experimental rats. SQ may exert cardioprotective effect via the ability to counteract free radicals by its antioxidant nature or membrane-stabilizing action. |
| Study | Disease/ Condition | Study Type/ SQ Source | Sample/ Population | Methodology | Results (SQ and CVD only) | Comments/Outcomes |
|---|---|---|---|---|---|---|
| Study 1 Motawi et al. 2010 [63] | Cardiotoxicity | Animal study Purchased from Sigma Chemicals Company, St. Louis, MO, USA | Male Wistar albino rats (170–200 g) Randomly divided into four groups: group I (n = 18), group II (n = 20), group III (n = 20), and group IV (n = 17). | Group I acted as the vehicle-treated control. The remaining three groups received a single intraperitoneal injection of 200 mg/kg BW cyclophosphamide (CP) to induce toxicity. Two of these groups received either DL-alpha-lipoic acid (LA) (35 mg/kg BW) or SQ (0.4 mL/rat) orally seven days before and seven days after CP injection. At the end of the experiment, the rats were sacrificed for blood collection and heart excision. Measurement involved 1) cardiac markers CPK, LDH, and AST; 2) serum TAC level; and 3) GPx and GR activities, levels of GSH, MDA, NO, and Ca2+ in the heart of CP-administered rats. | SQ treatment caused normalization of the levels of NO and Ca+2, a significant increase in the activity of GPx (p < 0.01), and decreases in the levels of cardiac GSH (p < 0.01) and serum uric acid (p < 0.001) when compared with the CP group. Hearts from SQ-treated rats showed nearly normal architecture of the heart with mild focal hemorrhage between myocardial bundles. The SQ-treated group had a significant decrease in all cardiac markers compared to the control group | SQ was able to attenuate the pathological alterations in the heart of CP-induced cardiotoxicity. This may highlight the efficacy of SQ as cytoprotectants in CP-induced cardiotoxicity. |
| Study 2 Preobrazhenskaya et al. 2015 [64] | Cardiomyopathy | Animal study Amaranth oil | Male albino rats (180–200 g) Randomly divided into six groups (seven rats per group) | All rats received daily gavage according to the groups for three weeks. Group 1: amaranth oil at 0.25 mL/kg Group 2: SQ 6% in corn oil Group 3: vehicle only (refined corn oil) Group 4: amaranth oil at 0.25 mL/kg Group 5: SQ 6% in corn oil Group 6: vehicle only (refined corn oil) Groups 4–6 were intraperitoneally (i.p) injected with 15 mg/kg doxorubicin in six injections over two weeks for cardiomyopathy induction, while control animals in groups 1–3 were injected with physiological saline solely. At the end of the experiment, animals were sacrificed and blood was sampled for the determination of plasma lipid profile: LDL-C, HDL-C, TC, TG, free FA, and phospholipids levels. | SQ supplementation to the cardiomyopathy-induced group (group 5) significantly reduced the TC, LDL-C, TG, and free FA profiles in plasma (p < 0.05) compared to the control group induced with the cardiomyopathy group (group 6). The level of HDL-C was significantly higher in group 5 compared to group 6(p < 0.05). All changes of plasma lipid profiles had a tendency for normalization but did not revert them to the normal level. | SQ supplementation at a low dose exerts a protective role against doxorubicin-induced cardiomyopathy in rats but did not revert them to the normal level. |
| Study | Disease/Condition | Study Type/ SQ Source | Sample/ Population | Methodology | Results (SQ and CVD Only) | Comments/Outcomes |
|---|---|---|---|---|---|---|
| Study 1 Strandberg et al. 1990 [45] | Cerebrovascular and cardiovascular disorders with different degrees of hypercholesterolemia | Human study SQ capsule The source was not disclosed | Fifteen patients (8 males and 7 females) of cerebrovascular and cardiovascular disorders Prior to the study, the patients were on a standard hospital diet for several weeks with the mean cholesterol and SQ intakes as 300 and 7 mg/day, respectively. | The patients were divided into two groups: i) SQ (n = 9), administered in capsules (300 mg) three times daily with meals, in which three subjects were fed for a minimum period (one-week) and six subjects were fed for an extended period (30 days), and ii) cholestyramine group (n = 6), administered 8 g of cholestyramine resin four times daily with meals. Blood was measured in intervals: basal, 7 days, and 30 days: i) cholesterol, SQ, and non-cholesterol sterol in serum and ii) cholesterol, SQ, and precursor sterol concentrations in different lipoproteins. | Fecal analysis showed that approximately 60% of dietary squalene was absorbed. Serum triglyceride and cholesterol contents were unchanged. Serum SQ levels were increased 17 times. The SQ feeding significantly increased serum levels of free and esterified methyl sterol contents (p < 0.05), while elevations of free and esterified cholesterol and lathosterol levels were inconsistent. The SQ feeding had no consistent effect on absorption efficiency of cholesterol yet significantly increased the fecal excretions of cholesterol, its nonpolar derivatives, and bile acids (p < 0.05). | SQ supplementation can increase cholesterol synthesis; however, no association was found with the consistency increment of serum cholesterol level. |
| Study 2 Miettinen and Vanhanen 1994 [50] | Hypercholesterolemia | Human study Source of SQ was not disclosed | Eighteen male subjects mean (± SE) age: 50 ± 3 y, with basal serum concentrations of cholesterol > 6 mmol/L and triglycerides < 2.5 mmol/L. | This study had four periods as follows: 1) baseline: home diet (n = 18); 2) rapeseed oil (n = 18), 6 weeks: 50 g of daily dietary fat intake was replaced with 50 g of a rapeseed oil mayonnaise per day for six weeks; 3) rapeseed oil (n = 8) or rapeseed oil + 1 g SQ/d (n = 10), 9 weeks (at week 15): ten subjects consumed rapeseed oil mayonnaise with 1 g SQ while the control group consumed rapeseed oil without SQ for nine weeks; and 4) rapeseed oil (n = 8) or rapeseed oil plus 0.5 g SQ/d (n = 10), 6 weeks (at week 21): ten subjects consumed rapeseed oil mayonnaise with 0.5 g SQ while the control group consumed rapeseed oil without SQ for six weeks. Fasting blood samples were collected for serum lipid (cholesterol, TG, phospholipids, apolipoprotein B, and HDL lipoprotein). Serum precursor sterols were also measured. | The addition of 1 g SQ to the diet at week 15 showed a significant increase in total cholesterol when compared to rapeseed oil-consuming only at week 6 and control rapeseed oil at week 15 and week 21 (p ≤ 0.05). The addition of 1 g SQ to the diet at week 15 showed significant increments (p ≤ 0.05) in LDL-C, total TG, and VLDL when compared at week 6 (rapeseed-given only). The addition of 0.5 g SQ to the diet at the 4th period showed a significant reduction in IDL cholesterol, triglycerides, and phospholipids (p ≤ 0.05). The reduction of SQ intake to only 0.5 g/d decreased the serum lipid concentrations to the rapeseed oil control and pre-squalene concentrations. Serum precursor sterols were significantly increased (p < 0.05) when compared at week 6 (rapeseed-given only). | A long-term (9 weeks) and large-amount SQ intake (1 g/d) might cause increased total cholesterol in serum due to augmented number of LDL particles with low surface lipids (free cholesterol and phospholipids) Small SQ doses (0.5 g/d) did not increase total cholesterol, which might be related to inhibition of endogenous pre-SQ cholesterol synthesis, which does not affect the LDL receptors or serum cholesterol. Long-term use of SQ resulted in the adaptation of cholesterol metabolism. |
| Study 3 Chan et al. 1996 [49] | Hypercholesterolemia | Human study, double-blind, randomized, placebo- controlled trial SQ capsule (Goldian Co., Singapore) | One hundred and two elderly (age > 65) patients with primary hypercholesterole-mia (TC > 250 mg/dL, TG < 300 mg/dL) were randomly assigned. The patients were enrolled after a three-month dietary intervention with the American Heart Association (AHA) Step I Diet. Patients with homozygous familial hypercholesterolemia, types I or III–V; hyperlipoproteinemia; cardiovascular; renal; hepatic; gastrointestinal; or metabolic diseases and malignancies were excluded. | Prior to randomization, any previous treatment with lipid-lowering drugs was discontinued for two months and a single-blind placebo lead-in period of four weeks was administered along with the dietary treatment. All patients then start consuming one of the following treatments with evening meal for a 20-week period: 1) 10 mg pravastatin; 2) two capsules (430 mg each) of SQ; 3) a combination of pravastatin and SQ; or 4) matching placebo. Levels of TC, HDL-C, and TG were determined at baseline after the fourth week lead-in placebo treatment and again after 4, 8, 12, and 20 weeks of the active treatment. LDL-C levels were determined by calculation. During each visit, blood was measured for concentrations of lipids and lipoproteins and for liver function and creatine kinase. | Supplementation of SQ 860 mg/day for 20 weeks had significantly decreased TC and LDL-C levels when compared to the baseline level and placebo group (p < 0.05). Supplementation of squalene 860 mg/day for 20 weeks had decreased TG levels by 5.3% while increased the HDL-C level by 1.8%. | Dietary squalene appeared to exert hypocholesterolemic activity. The authors proposed that this effect was due to the downregulation of HMG-CoA reductase activity by the enhanced squalene-derived synthesis of cholesterol. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, N.‘I.; Fairus, S.; Zulfarina, M.S.; Naina Mohamed, I. The Efficacy of Squalene in Cardiovascular Disease Risk-A Systematic Review. Nutrients 2020, 12, 414. https://doi.org/10.3390/nu12020414
Ibrahim N‘I, Fairus S, Zulfarina MS, Naina Mohamed I. The Efficacy of Squalene in Cardiovascular Disease Risk-A Systematic Review. Nutrients. 2020; 12(2):414. https://doi.org/10.3390/nu12020414
Chicago/Turabian StyleIbrahim, Nurul ‘Izzah, Syed Fairus, Mohamed S. Zulfarina, and Isa Naina Mohamed. 2020. "The Efficacy of Squalene in Cardiovascular Disease Risk-A Systematic Review" Nutrients 12, no. 2: 414. https://doi.org/10.3390/nu12020414
APA StyleIbrahim, N. ‘I., Fairus, S., Zulfarina, M. S., & Naina Mohamed, I. (2020). The Efficacy of Squalene in Cardiovascular Disease Risk-A Systematic Review. Nutrients, 12(2), 414. https://doi.org/10.3390/nu12020414





