Survival and Nutritional Status of Male and Female Heart Transplant Patients Based on the Nutritional Risk Index
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Sample
2.3. Sample Size
2.4. Study Tools
2.4.1. Anthropometric Measurements
2.4.2. Malnutrition Assessment
2.4.3. The Length of Stay
2.4.4. Blood Biochemical Tests
2.5. Statistical Analysis
3. Results
3.1. Participants’ Basal Characteristics
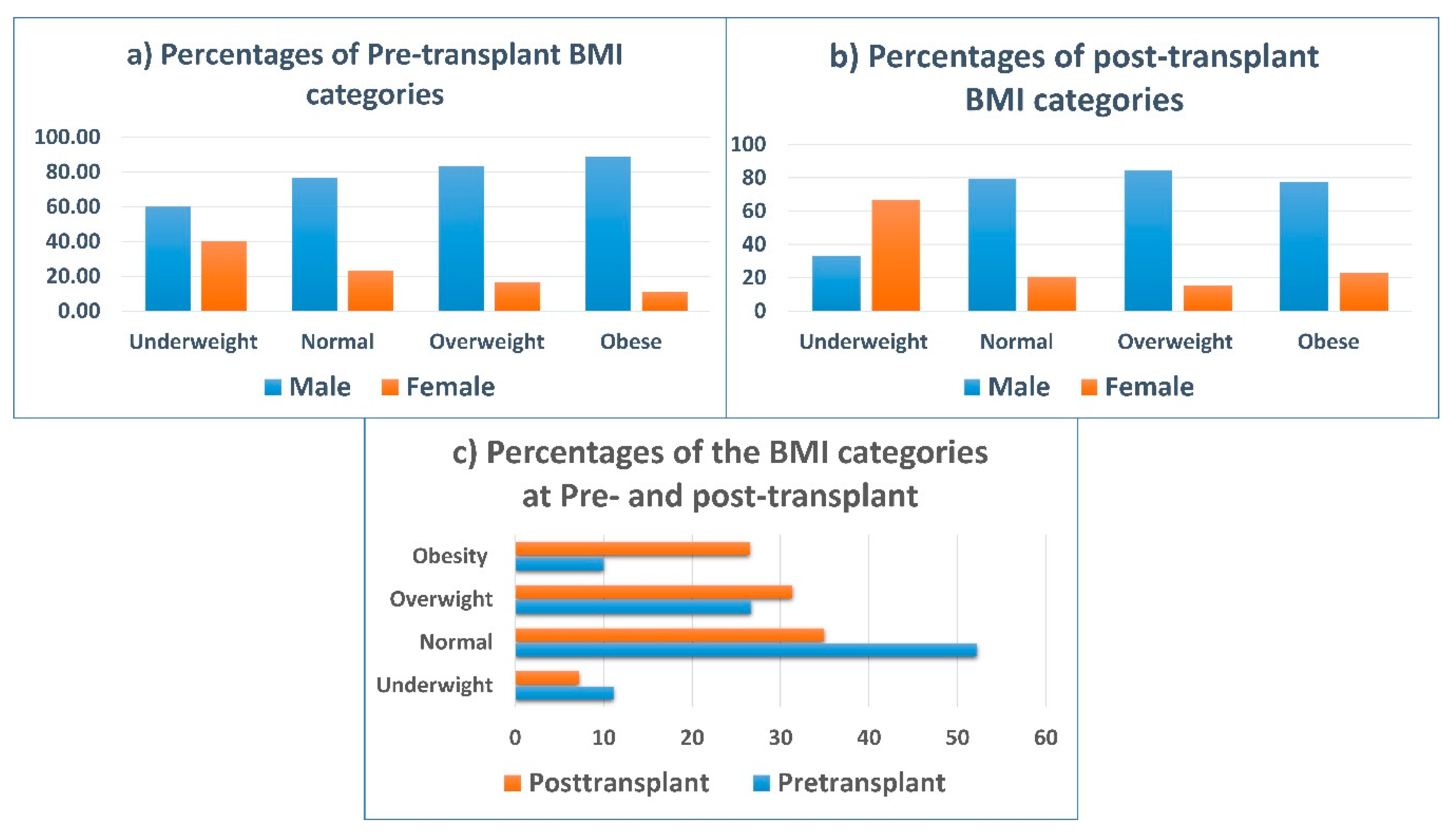
3.2. Anthropometric and NRI Comparison Pre- and Post-Transplantation
3.3. Comparison between Pre-Transplant and Post-Transplant Nutritional Assessment According to Gender
3.4. Survival Analysis
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Blackburn, G.L.; Gibbons, G.W.; Bothe, A.; Benotti, P.N.; Harken, D.E.; McEnany, T.M. Nutritional support in cardiac cachexia. J. Thorac. Cardiovasc. Surg. 1977, 73, 489–496. [Google Scholar] [CrossRef]
- Gastelurrutia, P.; Lupón, J.; Domingo, M.; Ribas, N.; Noguero, M.; Martinez, C.; Cortes, M.; Bayes-Genis, A. Usefulness of body mass index to characterize nutritional status in patients with heart failure. Am. J. Cardiol. 2011, 108, 1166–1170. [Google Scholar] [CrossRef]
- Rahman, A.; Jafry, S.; Jeejeebhoy, K.; Nagpal, A.D.; Pisani, B.; Agarwala, R. Malnutrition and cachexia in heart failure. JPEN J. Parenter. Enter. Nutr. 2016, 40, 475–486. [Google Scholar] [CrossRef]
- Carroa, A.; Panisellob, J.M.; Coats, S.A.J. Nutritional Status in Advanced Heart Failure and Heart Transplant Patients. Rev. Esp. Cardiol. 2017, 70, 626–628. [Google Scholar] [CrossRef]
- Jomphe, V.; Lands, L.C.; Mailhot, G. Nutritional Requirements of Lung Transplant Recipients: Challenges and Considerations. Nutrients 2018, 10, 790. [Google Scholar] [CrossRef] [Green Version]
- Hasse, J.M. Nutrition assessment and support of organ transplant recipients. JPEN J. Parenter. Enter. Nutr. 2001, 25, 120–131. [Google Scholar] [CrossRef]
- Thieme, R.D.; Cutchma, G.; Chieferdecker, M.E.M.; Campos, A.C.L. Nutritional risk index is predictor of postoperative complications in operations of digestive system or abdominal wall? ABCD Arq. Bras. Cir. Dig. 2013, 26, 286–292. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, C.M.; Hasselblad, V.; Mehta, R.H.; Tasissa, G.; Califf, R.M.; Fiuzat, M.; Rogers, J.G.; Leier, C.V.; Stevenson, L.W. Triage after hospitalization with advanced heart failure: The ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J. Am. Coll. Cardiol. 2010, 55, 872–878. [Google Scholar] [CrossRef] [Green Version]
- Gouya, G.; Voithofer, P.; Neuhold, S.; Storka, A.; Vila, G.; Pacher, R.; Wolzt, M.; Hülsmann, M. Association of nutritional risk index with metabolic biomarkers, appetite-regulatory hormones and inflammatory biomarkers and outcome in patients with chronic heart failure. Int. J. Clin. Pract. 2014, 68, 1293–1300. [Google Scholar] [CrossRef]
- Russo, M.J.; Hong, K.N.; Davies, R.R.; Chen, J.M.; Mancini, D.M.; Oz, M.C.; Rose, E.A.; Gelijns, A.; Naka, Y. The effect of body mass index on survival following heart transplantation: Do outcomes support consensus guidelines? Ann. Surg. 2010, 251, 144–152. [Google Scholar] [CrossRef]
- Thourani, V.H.; Keeling, W.B.; Kilgo, P.D.; Puskas, J.D.; Lattouf, O.M.; Chen, E.P.; Guyton, R.A. The impact of body mass index on morbidity and short-and long-term mortality in cardiac valvular surgery. J. Thorac. Cardiovasc. Surg. 2011, 42, 1052–1061. [Google Scholar] [CrossRef] [Green Version]
- Oreopoulos, A.; Padwal, R.; Kalantar-Zadeh, K.; Fonarow, G.C.; Norris, C.M.; McAlister, F.A. Body mass index and mortality in heart failure: A meta-analysis. Am. Heart J. 2008, 156, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Rapp-Kesek, D.; Ståhle, E.; Karlsson, T. Body mass index and albumin in the preoperative evaluation of cardiac surgery patients. Clin. Nutr. 2004, 23, 1398–1404. [Google Scholar] [CrossRef]
- Gastelurrutia, P.; Lupón, J.; de Antonio, M.; Zamora, E.; Domingo, M.; Urrutia, A.; Altimir, S.; Coll, R.; Díez, C.; Bayes-Genis, A. Body mass index, body fat, and nutritional status of patients with heart failure: The PLICA study. Clin. Nutr. 2015, 34, 1233–1238. [Google Scholar] [CrossRef]
- Curtis, J.P.; Selter, J.G.; Wang, Y.; Rathore, S.S.; Jovin, I.S.; Jadbabaie, F.; Kosiborod, M.; Portnay, E.L.; Sokol, S.I.; Bader, F.; et al. The obesity paradox: Body mass index and outcomes in patients with heart failure. Arch. Intern. Med. 2005, 165, 55–61. [Google Scholar] [CrossRef]
- Galiuto, L.; Locorotondo, G. Gender differences in cardiovascular disease. J. Integr. Cardiol. 2015, 1, 20–22. [Google Scholar]
- Barge-Caballero, E.; García-López, F.; Marzoa-Rivas, R.; Barge-Caballero, G.; Couto-Mallón, D.; Paniagua-Martín, M.J.; Solla-Buceta, M.; Velasco-Sierra, C.; Pita-Gutiérrez, F.; Herrera-Noreña, J.M.; et al. Prognostic Value of the Nutritional Risk Index in Heart Transplant Recipients. Rev. Esp. Cardiol. (Engl. Ed.) 2017, 70, 639–645. [Google Scholar] [CrossRef]
- Pai, M.P.; Paloucek, F.P. The origin of the "ideal" body weight equations. Ann. Pharmacother. 2000, 34, 1066–1069. [Google Scholar] [CrossRef]
- Robinson, J.D.; Lupkiewicz, S.M.; Palenik, L.; Lopez, L.M.; Ariet, M. Determination of ideal body weight for drug dosage calculations. Am. J. Hosp. Pharm. 1983, 40, 1016–1019. [Google Scholar] [CrossRef]
- Rocha, N.P.; Fortes, R.C. Total lymphocyte count and serum albumin as predictors of nutritional risk in surgical patients. Arq. Bras. Cir. Dig. 2015, 28, 193–196. [Google Scholar] [CrossRef] [Green Version]
- Chou, N.K.; Su, I.C.; Kuo, H.L.; Chen, Y.H.; Yang, R.S.; Wang, S.S. Bone mineral density in long-term Chinese heart transplant recipients: A cross-sectional study. Transpl. Proc. 2006, 38, 2141–2144. [Google Scholar] [CrossRef]
- Al-Najjar, Y.; Clark, A.L. Predicting outcome in patients with left ventricular systolic chronic heart failure using a nutritional risk index. Am. J. Cardiol. 2012, 109, 1315–1320. [Google Scholar] [CrossRef]
- Aziz, E.F.; Javed, F.; Pratap, B.; Musat, D.; Nader, A.; Pulimi, S.; Alivar, C.L.; Herzog, E.; Kukin, M.L. Malnutrition as assessed by nutritional risk index is associated with worse outcome in patients admitted with acute decompensated heart failure: An ACAP-HF data analysis. Heart Int. 2011, 6, e3–e8. [Google Scholar] [CrossRef]
- Kinugasa, Y.; Kato, M.; Sugihara, S.; Hirai, M.; Yamada, K.; Yanagihara, K.; Yamamoto, K. Geriatric nutritional risk index predicts functional dependency and mortality in patients with heart failure with preserved ejection fraction. Circulation 2013, 77, 705–711. [Google Scholar] [CrossRef] [Green Version]
- Kuzu, M.A.; Terzioğlu, H.; Genç, V.; Erkek, A.B.; Özban, M.; Sonyürek, P.; Elhan, A.H.; Torun, N. Preoperative nutritional risk assessment in predicting postoperative outcome in patients undergoing major surgery. World J. Surg. 2006, 30, 378–390. [Google Scholar] [CrossRef]
- Zhao, Y.; Ge, N.; Xie, D.; Gao, L.; Wang, Y.; Lio, Y.; Yue, J. The geriatric nutrition risk index versus the mini-nutritional assessment short form in predicting postoperative delirium and hospital length of stay among older non-cardiac surgical patients: A prospective cohort study. BMC Geriatr. 2020, 20, 107. [Google Scholar] [CrossRef]
- Zeltzer, S.M.; Taylor, D.O.; Tang, W.W. Long-term dietary habits and interventions in solid-organ transplantation. J. Heart Lung Transpl. 2015, 34, 1357–1365. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, L.G.; Santos, L.F.; Anastácio, L.R.; Lima, A.S.; Correia, M.I. Resting energy expenditure, body composition, and dietary intake: A longitudinal study before and after liver transplantation. Transplantation 2013, 96, 579–585. [Google Scholar] [CrossRef]
- Heaf, J.; Jakobsen, U.; Tvedegaard, E.; Kanstrup, I.L.; Fogh-Andersen, N. Dietary habits and nutritional status of renal transplant patients. J. Ren. Nutr. 2004, 14, 20–25. [Google Scholar] [CrossRef]
- Adejumo, O.L.; Koelling, T.M.; Hummel, S.L. Nutritional Risk Index Predicts Mortality in Hospitalized Advanced Heart Failure Patients. J. Heart Lung Transpl. 2015, 34, 1385–1389. [Google Scholar] [CrossRef] [Green Version]
- Kenchaiah, S.; Pocock, S.J.; Wang, D.; Finn, P.V.; Zornoff, L.A.; Skali, H.; Pfeffer, M.A.; Yusuf, S.; Swedberg, K.; Michelson, E.L.; et al. Body mass index and prognosis in patients with chronic heart failure. Circulation 2007, 116, 627–636. [Google Scholar] [CrossRef] [Green Version]
- Gopal, D.M.; Kalogeropoulos, A.P.; Georgiopoulou, V.V.; Tang, W.W.; Methvin, A.; Smith, A.L.; Bauer, D.C.; Newman, A.B.; Kim, L.; Harris, T.B.; et al. Serum albumin concentration and heart failure risk: The Health, Aging, and Body Composition Study. Am. Heart J. 2010, 160, 279–285. [Google Scholar] [CrossRef] [Green Version]
- Horwich, T.B.; Kalantar-Zadeh, K.; MacLellan, R.W.; Fonarow, G.C. Albumin levels predict survival in patients with systolic heart failure. Am. Heart J. 2008, 155, 883–889. [Google Scholar] [CrossRef] [Green Version]
- Wang, T.K.M.; O’Sullivan, S.; Gamble, G.D.; Ruygrok, P.N. Bone Density in Heart or Lung Transplant Recipients-A Longitudinal Study. Transpl. Proc. 2013, 45, 2357–2365. [Google Scholar] [CrossRef]
- Stein, E.M.; Cohen, A.; Freeby, M.; Rogers, H.; Kokolus, S.; Scott, V.; Mancini, D.; Restaino, S.; Brown, R.; McMahon, D.J.; et al. Severe vitamin D deficiency among heart and liver transplant recipients. Clin. Transpl. 2009, 23, 861–865. [Google Scholar] [CrossRef] [Green Version]
- Oloruntoba, O.O.; Cynthia, A.; Moylan, C.A. Gender-based disparities in access to and outcomes of liver transplantation. World J. Hepatol. 2015, 7, 460–467. [Google Scholar] [CrossRef]
- Jindal, R.M.; Ryan, J.J.; Sajjad, I.; Murthy, M.H.; Baines, L.S. Kidney Transplantation and Gender Disparity. Am. J. Nephrol. 2005, 25, 474–483. [Google Scholar] [CrossRef]
- Dang, N.C.; Topkara, V.K.; Kim, B.T.; Mercando, M.L.; Kay, J.; Naka, Y. Clinical outcomes in patients with chronic congestive heart failure who undergo left ventricular assist device implantation. J. Thorac. Cardiovasc. Surg. 2005, 130, 1302–1309. [Google Scholar] [CrossRef] [Green Version]
- Almufleh, A.; Fazelpour, S.; Merdad, A.; Marbach, J.; Davies, R.; Mielniczuk, L.; Chih, S.; Stadnick, E. Gender Differences in Pre-Transplant Characteristics and Short-Term Clinical Outcomes Post Heart Transplantation. J. Heart Lung Transpl. 2019, 38, S397. [Google Scholar] [CrossRef]
- García-Cosío, M.D.; González-Vilchez, F.; López-Vilella, R.; Barge-Caballero, E.; Gómez-Bueno, M.-S.M.; Arizón, J.M.; Sousa, D.R.; González-Costello, J.; Mirabet, S.; Pérez-Villa, F.; et al. Gender differences in heart transplantation: Twenty-five year trends in the nationwide Spanish heart transplant registry. Clin. Transpl. 2020. [Google Scholar] [CrossRef]
- Prasad, N.; Sinha, A.; Gupta, A.; Bhadauria, D.; Manjunath, R.; Kaul, A.; Sharma, R.K. Validity of nutrition risk index as a malnutrition screening tool compared with subjective global assessment in end-stage renal disease patients on peritoneal dialysis. Indian J. Nephrol. 2016, 26, 27–32. [Google Scholar] [CrossRef]





| Variables | Males (n = 70) Mean ± SD | Females (n = 20) Mean ± SD | p-Value |
|---|---|---|---|
| Length of stay | 28.81 ± 27.06 | 28.75 ± 23.97 | NS |
| Age | 39.84 ± 12.22 | 32.35 ± 9.31 | <0.05 |
| Height (cm) | 169.30 ± 6.68 | 157.60 ± 4.31 | <0.001 |
| Ideal weight (kg) | 65.21 ± 6.01 | 52.35 ± 2.80 | <0.001 |
| Weight (kg) | 70.19 ± 15.44 | 55.43 ± 13.50 | <0.001 |
| Body mass index (kg/m2) | 24.48 ± 5.06 | 22.20 ± 5.02 | NS |
| Nutritional risk index | 96.97 ± 8.52 | 95.29 ± 8.56 | NS |
| Variables | Pre-Transplant (n = 90) | Post-Transplant (n = 90) | p-Value | ||
|---|---|---|---|---|---|
| Range | Mean ± SD | Range | Mean ± SD | ||
| Weight (kg) | 32.70–117.00 | 66.91 ± 16.18 | 31.00–139.40 | 73.50 ± 17.88 | <0.001 |
| BMI (kg/m2) | 13.27–39.09 | 23.98 ± 5.11 | 12.74–43.02 | 26.40 ± 5.68 | <0.001 |
| NRI | 69.10–114.60 | 96.60 ± 8.50 | 72.10–120.70 | 105.50 ± 8.10 | <0.001 |
| Albumin (g/L) | 23.00–48.00 | 37.61 ± 5.23 | 20.00–52.00 | 41.99 ± 5.86 | <0.001 |
| Variables | Pre-Transplant | p-Value | Post-Transplant | p-Value | ||
|---|---|---|---|---|---|---|
| Male (n = 70) Mean ± SD | Female (n = 20) Mean ± SD | Male (n = 70) Mean ± SD | Female (n = 20) Mean ± SD | |||
| Hemoglobin (g/L) | 119.30 ± 22.91 | 105.00 ± 18.52 | <0.05 | 129.80 ± 23.05 | 105.90 ± 17.76 | <0.001 |
| Hematocrit (%) | 36.00 ± 7.00 | 32.00 ± 5.00 | <0.05 | 39.00 ± 7.00 | 33.00 ± 5.00 | <0.001 |
| Lymphocyte count (%) | 18.74 ± 15.98 | 23.28 ± 15.53 | NS | 20.29 ± 11.17 | 22.49 ± 14.27 | NS |
| Red blood cells (1012/L) | 4.52 ± 00.95 | 3.97 ± 0.69 | <0.05 | 4.85 ± 00.92 | 3.89 ± 0.65 | <0.001 |
| Iron (µmol/L) | 11.53 ± 6.43 | 12.67 ± 14.14 | NS | 12.02 ± 5.28 | 8.86 ± 5.46 | NS |
| TIBC (µmol/L) | 63.29 ± 12.09 | 61.46 ± 13.21 | NS | 45.20 ± 10.73 | 46.90 ± 9.18 | NS |
| UIBC (µmol/L) | 51.55 ± 12.76 | 50.11 ± 16.18 | NS | 33.31 ± 12.39 | 37.94 ± 10.39 | NS |
| Ferritin (µg/L) | 183.80 ± 183.20 | 145.60 ± 178.20 | NS | 379.50 ± 331.10 | 323.90 ± 407.00 | NS |
| Alkaline phosphatase (u/L) | 111.90 ± 72.35 | 102.30 ± 69.03 | NS | 104.10 ± 70.89 | 110.00 ± 80.33 | NS |
| Total protein (g/dL) | 72.72 ± 11.49 | 68.17 ± 11.86 | NS | 70.39 ± 7.96 | 64.54 ± 7.93 | <0.05 |
| Albumin (g/L) | 37.72 ± 5.18 | 37.20 ± 5.53 | NS | 42.52 ± 6.02 | 39.05 ± 4.93 | NS |
| Prealbumin (mg/dL) | 187.80 ± 59.36 | 116.30 ± 56.07 | <0.05 | 293.10 ± 68.01 | 167.80 ± 108.10 | <0.05 |
| Total cholesterol (mmol/L) | 2.98 ± 1.06 | 3.08 ± 1.02 | NS | 3.72 ± 1.49 | 3.80 ± 0.79 | NS |
| Low Density Lipoprotein (mmol/L) | 1.98 ± 0.76 | 2.05 ± 0.69 | NS | 2.23 ± 1.06 | 1.96 ± 0.49 | NS |
| High Density Lipoprotein (mmol/L) | 0.88 ± 0.38 | 0.99 ± 0.41 | NS | 1.20 ± 0.39 | 1.46 ± 0.49 | NS |
| Triglycerides (mmol/L) | 0.85 ± 0.36 | 0.86 ± 0.43 | NS | 1.35 ± 0.60 | 1.32 ± 0.63 | NS |
| Triiodothyronine (mmol/L) | 1.35 ± 0.46 | 1.35 ± 0.39 | NS | 1.61 ± 0.41 | 1.24 ± 0.65 | NS |
| Free thyroxine (pmol/L) | 20.09 ± 5.22 | 19.81 ± 5.58 | NS | 17.80 ± 4.22 | 18.01 ± 5.66 | NS |
| Thyroid stimulating hormone (mU/L) | 4.71 ± 3.90 | 4.53 ± 2.72 | NS | 3.01 ± 2.50 | 2.45 ± 2.21 | NS |
| Fasting blood glucose (mmol/L) | 6.23 ± 2.85 | 6.73 ± 3.85 | NS | 6.47 ± 2.73 | 6.61 ± 3.92 | NS |
| HbA1C (%) | 6.90 ± 2.01 | 6.09 ± 1.71 | NS | 6.87 ± 1.80 | 6.18 ± 2.12 | NS |
| Variables | Hazard Ratio | 95% CI | p-Value |
|---|---|---|---|
| Pre-transplant NRI | 0.79 | 0.92–1.02 | 0.20 |
| Post-transplant NRI | 0.82 | 0.75–0.89 | <0.001 |
| BMI | 1.54 | 0–3669.1 | 0.91 |
| Lymphocytes | 0.98 | 0.83–1.15 | 0.78 |
| Total cholesterol | 0.79 | 0.02–31.79 | 0.91 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almutawa, D.A.; Almuammar, M.; Elshafie, M.M.; Aljuraiban, G.S.; Alnafisah, A.; Abulmeaty, M.M.A. Survival and Nutritional Status of Male and Female Heart Transplant Patients Based on the Nutritional Risk Index. Nutrients 2020, 12, 3868. https://doi.org/10.3390/nu12123868
Almutawa DA, Almuammar M, Elshafie MM, Aljuraiban GS, Alnafisah A, Abulmeaty MMA. Survival and Nutritional Status of Male and Female Heart Transplant Patients Based on the Nutritional Risk Index. Nutrients. 2020; 12(12):3868. https://doi.org/10.3390/nu12123868
Chicago/Turabian StyleAlmutawa, Deema A., May Almuammar, Mona Mohamed Elshafie, Ghadeer S. Aljuraiban, Alaa Alnafisah, and Mahmoud M. A. Abulmeaty. 2020. "Survival and Nutritional Status of Male and Female Heart Transplant Patients Based on the Nutritional Risk Index" Nutrients 12, no. 12: 3868. https://doi.org/10.3390/nu12123868
APA StyleAlmutawa, D. A., Almuammar, M., Elshafie, M. M., Aljuraiban, G. S., Alnafisah, A., & Abulmeaty, M. M. A. (2020). Survival and Nutritional Status of Male and Female Heart Transplant Patients Based on the Nutritional Risk Index. Nutrients, 12(12), 3868. https://doi.org/10.3390/nu12123868






