Gastroesophageal Reflux Disease and Foregut Dysmotility in Children with Intestinal Failure
Abstract
1. Introduction
2. Foregut Manifestations and Their Pathophysiology in Intestinal Failure
2.1. Oral Aversion and Dysphagia
2.2. Regurgitation and GER in Children
2.2.1. Impact of the Distorted Anatomy on GERD
2.2.2. Complications Related to Necrotizing Enterocolitis
2.2.3. Impact of Small Bowel Resection on Gastric Acid Secretion
2.3. Delayed Gastric Emptying
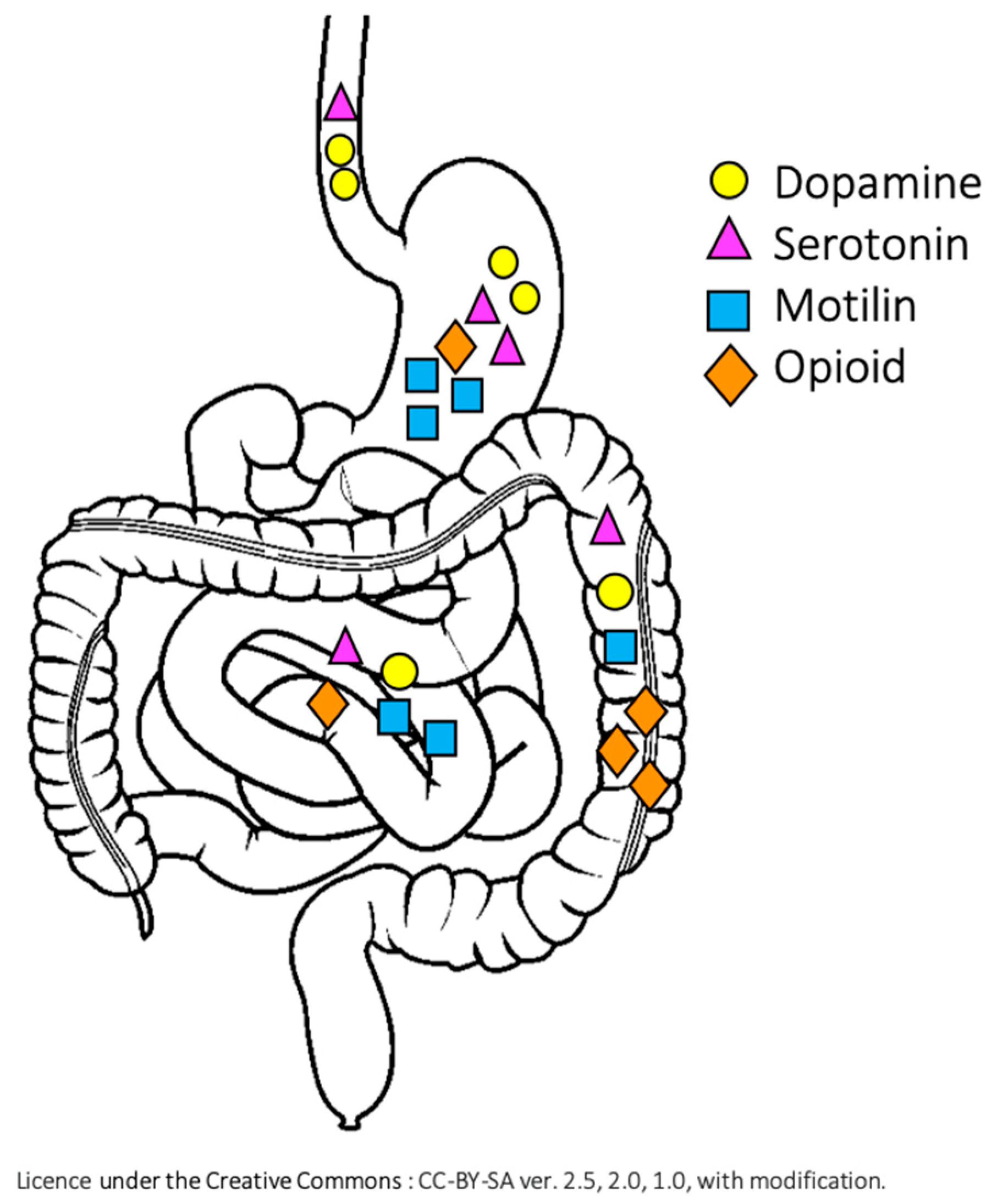
2.4. Impact of Small Bowel Resection on Motility
3. Impact of Feeding on GI Motility in IF
4. Tools in the Diagnostics of the Upper GI Dysmotility
4.1. Barium Contrast Study
4.2. Esophago-Gastro-Duodenoscopy
4.3. 24-Hour Esophageal pH-Impedance Study
4.4. High Resolution Esophageal Manometry
4.5. Antro-Duodenal Manometry
4.6. Nuclear Medicine Gastric Emptying Study
5. Management of GERD and Foregut Dysmotility in IF
5.1. Non-Pharmacological and Dietary Treatment
5.2. Pharmacological Treatment
5.3. Indication for Surgical Management
6. Summary and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gupte, G.L.; Beath, S.V.; Protheroe, S.; Murphy, M.S.; Davies, P.; Sharif, K.; McKiernan, P.J.; de Ville de Goyet, J.; Booth, I.W.; Kelly, D.A. Improved outcome of referrals for intestinal transplantation in the UK. Arch. Dis. Child. 2007, 92, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Jolley, S.G.; Lorenz, M.L.; Hendrickson, M.; Kurlinski, J.P. Esophageal pH monitoring abnormalities and gastroesophageal reflux disease in infants with intestinal malrotation. Arch. Surg. 1999, 134, 747–752, discussion 752–753. [Google Scholar] [CrossRef] [PubMed]
- Koivusalo, A.; Rintala, R.; Lindahl, H. Gastroesophageal reflux in children with a congenital abdominal wall defect. J. Pediatr. Surg. 1999, 34, 1127–1129. [Google Scholar] [CrossRef]
- Devane, S.P.; Coombes, R.; Smith, V.V.; Bisset, W.M.; Booth, I.W.; Lake, B.D.; Milla, P.J. Persistent gastrointestinal symptoms after correction of malrotation. Arch. Dis. Child. 1992, 67, 218–221. [Google Scholar] [CrossRef]
- Hussain, S.Z.; Di Lorenzo, C. Motility disorders: Diagnosis and treatment for the pediatric patient. Pediatr. Clin. N. Am. 2002, 49, 27–51. [Google Scholar] [CrossRef]
- Thapar, N.; Saliakellis, E.; Benninga, M.A.; Borrelli, O.; Curry, J.; Faure, C.; De Giorgio, R.; Gupte, G.; Knowles, C.H.; Staiano, A.; et al. Paediatric Intestinal Pseudo-obstruction: Evidence and Consensus-based Recommendations From an ESPGHAN-Led Expert Group. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 991–1019. [Google Scholar] [CrossRef]
- Bagwell, C.E.; Filler, R.M.; Cutz, E.; Stringer, D.; Ein, S.H.; Shandling, B.; Stephens, C.A.; Wesson, D.E. Neonatal intestinal pseudoobstruction. J. Pediatr. Surg. 1984, 19, 732–739. [Google Scholar] [CrossRef]
- Al-Shboul, O.A. The Importance of Interstitial Cells of Cajal in the Gastrointestinal Tract. Saudi J. Gastroenterol. 2013, 19, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Auber, F.; Danzer, E.; Noché-Monnery, M.-E.; Sarnacki, S.; Trugnan, G.; Boudjemaa, S.; Audry, G. Enteric nervous system impairment in gastroschisis. Eur. J. Pediatr. Surg. 2013, 23, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Radhika Krishna, O.H.; Aleem, M.A.; Kayla, G. Abnormalities of the intestinal pacemaker cells, enteric neurons, and smooth muscle in intestinal atresia. J. Lab Physicians 2019, 11, 180–185. [Google Scholar] [CrossRef]
- Zani-Ruttenstock, E.; Zani, A.; Paul, A.; Diaz-Cano, S.; Ade-Ajayi, N. Interstitial cells of Cajal are decreased in patients with gastroschisis associated intestinal dysmotility. J. Pediatr. Surg. 2015, 50, 750–754. [Google Scholar] [CrossRef] [PubMed]
- Molenaar, J.C.; Tibboel, D.; van der Kamp, A.W.; Meijers, J.H. Diagnosis of innervation-related motility disorders of the gut and basic aspects of enteric nervous system development. Prog. Pediatr. Surg. 1989, 24, 173–185. [Google Scholar] [CrossRef]
- Coombs, R.C.; Buick, R.G.; Gornall, P.G.; Corkery, J.J.; Booth, I.W. Intestinal malrotation: The role of small intestinal dysmotility in the cause of persistent symptoms. J. Pediatr. Surg. 1991, 26, 553–556. [Google Scholar] [CrossRef]
- Masumoto, K.; Suita, S.; Nada, O.; Taguchi, T.; Guo, R. Abnormalities of enteric neurons, intestinal pacemaker cells, and smooth muscle in human intestinal atresia. J. Pediatr. Surg. 1999, 34, 1463–1468. [Google Scholar] [CrossRef]
- Alatas, F.S.; Masumoto, K.; Esumi, G.; Nagata, K.; Taguchi, T. Significance of abnormalities in systems proximal and distal to the obstructed site of duodenal atresia. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 242–247. [Google Scholar] [CrossRef]
- Rolle, U.; Piotrowska, A.P.; Nemeth, L.; Puri, P. Altered distribution of interstitial cells of Cajal in Hirschsprung disease. Arch. Pathol. Lab. Med. 2002, 126, 928–933. [Google Scholar] [CrossRef]
- Olieman, J.; Kastelijn, W. Nutritional Feeding Strategies in Pediatric Intestinal Failure. Nutrients 2020, 12, 177. [Google Scholar] [CrossRef]
- Hopkins, J.; Cermak, S.A.; Merritt, R.J. Oral Feeding Difficulties in Children with Short Bowel Syndrome: A Narrative Review. Nutr. Clin. Pract. 2018, 33, 99–106. [Google Scholar] [CrossRef]
- Olieman, J.F.; Penning, C.; Ijsselstijn, H.; Escher, J.C.; Joosten, K.F.; Hulst, J.M.; Tibboel, D. Enteral nutrition in children with short-bowel syndrome: Current evidence and recommendations for the clinician. J. Am. Diet. Assoc. 2010, 110, 420–426. [Google Scholar] [CrossRef]
- Crapnell, T.L.; Rogers, C.E.; Neil, J.J.; Inder, T.E.; Woodward, L.J.; Pineda, R.G. Factors associated with feeding difficulties in the very preterm infant. Acta Paediatr. 2013, 102, e539–e545. [Google Scholar] [CrossRef]
- Goulet, O.; Olieman, J.; Ksiazyk, J.; Spolidoro, J.; Tibboe, D.; Köhler, H.; Yagci, R.V.; Falconer, J.; Grimble, G.; Beattie, R.M. Neonatal short bowel syndrome as a model of intestinal failure: Physiological background for enteral feeding. Clin. Nutr. 2013, 32, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Mason, S.J.; Harris, G.; Blissett, J. Tube feeding in infancy: Implications for the development of normal eating and drinking skills. Dysphagia 2005, 20, 46–61. [Google Scholar] [CrossRef] [PubMed]
- Barlow, S.M.; Finan, D.S.; Lee, J.; Chu, S. Synthetic orocutaneous stimulation entrains preterm infants with feeding difficulties to suck. J. Perinatol. 2008, 28, 541–548. [Google Scholar] [CrossRef]
- Harris, G.; Blissett, J.; Johnson, R. Food Refusal Associated with Illness. Child Psychol. Psychiatry Rev. 2000, 5, 148–156. [Google Scholar] [CrossRef]
- Larson, R.W.; Branscomb, K.R.; Wiley, A.R. Forms and functions of family mealtimes: Multidisciplinary perspectives. New Dir. Child Adolesc. Dev. 2006, 2006, 1–15. [Google Scholar] [CrossRef]
- Rommel, N.; De Meyer, A.-M.; Feenstra, L.; Veereman-Wauters, G. The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. J. Pediatr. Gastroenterol. Nutr. 2003, 37, 75–84. [Google Scholar] [CrossRef]
- Singendonk, M.M.J.; Rexwinkel, R.; Steutel, N.F.; Gottrand, F.; McCall, L.; Orsagh-Yentis, D.K.; Rosen, R.; Strisciuglio, C.; Thapar, N.; Vandenplas, Y.; et al. Development of a Core Outcome Set for Infant Gastroesophageal Reflux Disease. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 655–661. [Google Scholar] [CrossRef]
- Jadcherla, S. Dysphagia in the high-risk infant: Potential factors and mechanisms123. Am. J. Clin. Nutr. 2016, 103, 622S–628S. [Google Scholar] [CrossRef]
- Jadcherla, S.R.; Gupta, A.; Stoner, E.; Fernandez, S.; Caniano, D.; Rudolph, C.D. Neuromotor Markers of Esophageal Motility in Feeding Intolerant Infants with Gastroschisis. J. Pediatric Gastroenterol. Nutr. 2008, 47, 158–164. [Google Scholar] [CrossRef]
- De Oliveira, A.C.M.; de Lima Friche, A.A.; Salomão, M.S.; Bougo, G.C.; Vicente, L.C.C. Predictive factors for oropharyngeal dysphagia after prolonged orotracheal intubation. Braz. J. Otorhinolaryngol. 2018, 84, 722–728. [Google Scholar] [CrossRef]
- Kahrilas, P.J.; Boeckxstaens, G.; Smout, A.J.P.M. Management of the patient with incomplete response to PPI therapy. Best Pract. Res. Clin. Gastroenterol. 2013, 27, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Demirbilek, S.; Karaman, A.; Gürünlüoğlu, K.; Akin, M.; Taş, E.; Aksoy, R.T.; Kekilli, E. Delayed gastric emptying in gastroesophageal reflux disease: The role of malrotation. Pediatr. Surg. Int. 2005, 21, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Koppen, I.J.N.; Benninga, M.A.; Singendonk, M.M.J. Motility disorders in infants. Early Hum. Dev. 2017, 114, 1–6. [Google Scholar] [CrossRef]
- Gilger, M.A.; El-Serag, H.B.; Gold, B.D.; Dietrich, C.L.; Tsou, V.; McDuffie, A.; Shub, M.D. Prevalence of endoscopic findings of erosive esophagitis in children: A population-based study. J. Pediatr. Gastroenterol. Nutr. 2008, 47, 141–146. [Google Scholar] [CrossRef]
- Busch, A.; Sturm, E. Screening Endoscopy Contributes to Relevant Modifications of Therapeutic Regimen in Children with Intestinal Failure. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 478–482. [Google Scholar] [CrossRef]
- Kawahara, H.; Nakajima, K.; Yagi, M.; Okuyama, H.; Kubota, A.; Okada, A. Mechanisms responsible for recurrent gastroesophageal reflux in neurologically impaired children who underwent laparoscopic Nissen fundoplication. Surg. Endosc. 2002, 16, 767–771. [Google Scholar] [CrossRef]
- Laje, P.; Fraga, M.V.; Peranteau, W.H.; Hedrick, H.L.; Khalek, N.; Gebb, J.S.; Moldenhauer, J.S.; Johnson, M.P.; Flake, A.W.; Adzick, N.S. Complex gastroschisis: Clinical spectrum and neonatal outcomes at a referral center. J. Pediatr. Surg. 2018, 53, 1904–1907. [Google Scholar] [CrossRef]
- Scarpato, E.; D’Armiento, M.; Martinelli, M.; Mancusi, V.; Campione, S.; Alessandrella, A.; Staiano, A.; Miele, E. Impact of hiatal hernia on pediatric dyspeptic symptoms. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 795–798. [Google Scholar] [CrossRef]
- Marseglia, L.; Manti, S.; D’Angelo, G.; Gitto, E.; Salpietro, C.; Centorrino, A.; Scalfari, G.; Santoro, G.; Impellizzeri, P.; Romeo, C. Gastroesophageal reflux and congenital gastrointestinal malformations. World J. Gastroenterol. 2015, 21, 8508–8515. [Google Scholar] [CrossRef]
- Contractor, Q.Q.; Akhtar, S.S.; Contractor, T.Q. Endoscopic esophagitis and gastroesophageal flap valve. J. Clin. Gastroenterol. 1999, 28, 233–237. [Google Scholar] [CrossRef]
- Vannucchi, M.G.; Midrio, P.; Flake, A.W.; Faussone-Pellegrini, M.S. Neuronal differentiation and myenteric plexus organization are delayed in gastroschisis: An immunohistochemical study in a rat model. Neurosci. Lett. 2003, 339, 77–81. [Google Scholar] [CrossRef]
- Kocoshis, S.A.; Goldschmidt, M.L.; Nathan, J.D.; El-Chammas, K.I.; Bondoc, A.J.; Tiao, G.M.; Alonso, M.H.; Ubesie, A.C.; Cole, C.R.; Kaul, A. Esophageal dysmotility: An intrinsic feature of megacystis, microcolon, hypoperistalsis syndrome (MMIHS). J. Pediatr. Surg. 2019, 54, 1303–1307. [Google Scholar] [CrossRef]
- Kumar, D.; Brereton, R.J.; Spitz, L.; Hall, C.M. Gastro-oesophageal reflux and intestinal malrotation in children. Br. J. Surg. 1988, 75, 533–535. [Google Scholar] [CrossRef]
- Tiboni, S.G.; Patel, Y.; Lander, A.D.; Parikh, D.H.; Jawaheer, G.; Arul, G.S. Management of gastroesophageal reflux associated with malrotation in children. J. Pediatr. Surg. 2011, 46, 289–291. [Google Scholar] [CrossRef]
- Nehra, D.; Goldstein, A.M. Intestinal malrotation: Varied clinical presentation from infancy through adulthood. Surgery 2011, 149, 386–393. [Google Scholar] [CrossRef]
- Ballance, W.A.; Dahms, B.B.; Shenker, N.; Kliegman, R.M. Pathology of neonatal necrotizing enterocolitis: A ten-year experience. J. Pediatr. 1990, 117, S6–S13. [Google Scholar] [CrossRef]
- Koike, Y.; Li, B.; Lee, C.; Cheng, S.; Miyake, H.; Welsh, C.; Hock, A.; Belik, J.; Zani, A.; Pierro, A. Gastric emptying is reduced in experimental NEC and correlates with the severity of intestinal damage. J. Pediatr. Surg. 2017, 52, 744–748. [Google Scholar] [CrossRef]
- Williams, N.S.; Evans, P.; King, R.F. Gastric acid secretion and gastrin production in the short bowel syndrome. Gut 1985, 26, 914–919. [Google Scholar] [CrossRef]
- Phan, J.; Benhammou, J.N.; Pisegna, J.R. Gastric Hypersecretory States: Investigation and Management. Curr. Treat. Options Gastroenterol. 2015, 13, 386–397. [Google Scholar] [CrossRef]
- Hyman, P.E.; Everett, S.L.; Harada, T. Gastric acid hypersecretion in short bowel syndrome in infants: Association with extent of resection and enteral feeding. J. Pediatr. Gastroenterol. Nutr. 1986, 5, 191–197. [Google Scholar] [CrossRef]
- Richter, C.; Tanaka, T.; Yada, R.Y. Mechanism of activation of the gastric aspartic proteinases: Pepsinogen, progastricsin and prochymosin. Biochem. J. 1998, 335 Pt 3, 481–490. [Google Scholar] [CrossRef]
- Bongaerts, G.P.; Severijnen, R.S.; Tangerman, A.; Verrips, A.; Tolboom, J.J. Bile acid deconjugation by Lactobacilli and its effects in patients with a short small bowel. J. Gastroenterol. 2000, 35, 801–804. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, A.F. Biliary secretion and excretion in health and disease: Current concepts. Ann. Hepatol. 2007, 6, 15–27. [Google Scholar] [CrossRef]
- Koek, G.H.; Vos, R.; Sifrim, D.; Cuomo, R.; Janssens, J.; Tack, J. Mechanisms underlying duodeno-gastric reflux in man. Neurogastroenterol. Motil. 2005, 17, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Dixon, M.F.; Neville, P.M.; Mapstone, N.P.; Moayyedi, P.; Axon, A.T. Bile reflux gastritis and Barrett’s oesophagus: Further evidence of a role for duodenogastro-oesophageal reflux? Gut 2001, 49, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, L.; Irani, K.; Jiang, H.; Goldstein, A.M. Clinical presentation, response to therapy, and outcome of gastroparesis in children. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 185–190. [Google Scholar] [CrossRef]
- Waseem, S.; Islam, S.; Kahn, G.; Moshiree, B.; Talley, N.J. Spectrum of gastroparesis in children. J. Pediatric Gastroenterol. Nutr. 2012, 55, 166–172. [Google Scholar] [CrossRef]
- Franken, J.; Mauritz, F.A.; Stellato, R.K.; Van der Zee, D.C.; Van Herwaarden-Lindeboom, M.Y.A. The Effect of Gastrostomy Placement on Gastric Function in Children: A Prospective Cohort Study. J. Gastrointest. Surg. 2017, 21, 1105–1111. [Google Scholar] [CrossRef]
- Parkman, H.P.; Hasler, W.L.; Fisher, R.S. American Gastroenterological Association American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Gastroenterology 2004, 127, 1592–1622. [Google Scholar] [CrossRef]
- Nguyen, N.Q.; Fraser, R.J.; Bryant, L.K.; Holloway, R.H. Functional association between proximal and distal gastric motility during fasting and duodenal nutrient stimulation in humans. Neurogastroenterol. Motil. 2007, 19, 638–645. [Google Scholar] [CrossRef]
- Smith, D.S.; Williams, C.S.; Ferris, C.D. Diagnosis and treatment of chronic gastroparesis and chronic intestinal pseudo-obstruction. Gastroenterol. Clin. N. Am. 2003, 32, 619–658. [Google Scholar] [CrossRef]
- Braden, B.; Peterknecht, A.; Piepho, T.; Schneider, A.; Caspary, W.F.; Hamscho, N.; Ahrens, P. Measuring gastric emptying of semisolids in children using the 13C-acetate breath test: A validation study. Dig. Liver Dis. 2004, 36, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Wessel, J.J.; Kocoshis, S.A. Nutritional management of infants with short bowel syndrome. Semin. Perinatol. 2007, 31, 104–111. [Google Scholar] [CrossRef]
- Spencer, A.U.; Neaga, A.; West, B.; Safran, J.; Brown, P.; Btaiche, I.; Kuzma-O’Reilly, B.; Teitelbaum, D.H. Pediatric short bowel syndrome: Redefining predictors of success. Ann. Surg. 2005, 242, 403–409, discussion 409–412. [Google Scholar] [CrossRef]
- Phillips, J.D.; Raval, M.V.; Redden, C.; Weiner, T.M. Gastroschisis, atresia, dysmotility: Surgical treatment strategies for a distinct clinical entity. J. Pediatr. Surg. 2008, 43, 2208–2212. [Google Scholar] [CrossRef]
- Tunell, W.P.; Puffinbarger, N.K.; Tuggle, D.W.; Taylor, D.V.; Mantor, P.C. Abdominal wall defects in infants. Survival and implications for adult life. Ann. Surg. 1995, 221, 525–528, discussion 528–530. [Google Scholar] [CrossRef]
- Dicken, B.J.; Sergi, C.; Rescorla, F.J.; Breckler, F.; Sigalet, D. Medical management of motility disorders in patients with intestinal failure: A focus on necrotizing enterocolitis, gastroschisis, and intestinal atresia. J. Pediatr. Surg. 2011, 46, 1618–1630. [Google Scholar] [CrossRef]
- Masumoto, K.; Suita, S.; Taguchi, T. The occurrence of unusual smooth muscle bundles expressing alpha-smooth muscle actin in human intestinal atresia. J. Pediatr. Surg. 2003, 38, 161–166. [Google Scholar] [CrossRef]
- Husebye, E. The patterns of small bowel motility: Physiology and implications in organic disease and functional disorders. Neurogastroenterol. Motil. 1999, 11, 141–161. [Google Scholar] [CrossRef]
- Nygaard, K. Gastro-intestinal motility after resections and bypass-operations on the small intestine in rats. The effect of different types of anastomosis. Acta Chir. Scand. 1967, 133, 653–663. [Google Scholar]
- Spiller, R.C. Intestinal absorptive function. Gut 1994, 35, S5–S9. [Google Scholar] [CrossRef] [PubMed]
- Capriati, T.; Nobili, V.; Stronati, L.; Cucchiara, S.; Laureti, F.; Liguori, A.; Tyndall, E.; Diamanti, A. Enteral nutrition in pediatric intestinal failure: Does initial feeding impact on intestinal adaptation? Expert Rev. Gastroenterol. Hepatol. 2017, 11, 741–748. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.K.; Davies, N.; Smyth, E.; Heather, N.; Cole, C.; Keys, S.C.; Beattie, R.M.; Batra, A. Intestinal failure: The evolving demographic and patient outcomes on home parenteral nutrition. Acta Paediatr. 2018, 107, 2207–2211. [Google Scholar] [CrossRef] [PubMed]
- Cole, C.R.; Kocoshis, S.A. Nutrition management of infants with surgical short bowel syndrome and intestinal failure. Nutr. Clin. Pract. 2013, 28, 421–428. [Google Scholar] [CrossRef]
- Homko, C.J.; Duffy, F.; Friedenberg, F.K.; Boden, G.; Parkman, H.P. Effect of dietary fat and food consistency on gastroparesis symptoms in patients with gastroparesis. Neurogastroenterol. Motil. 2015, 27, 501–508. [Google Scholar] [CrossRef]
- Camilleri, M.; Shin, A. Novel and Validated Approaches for Gastric Emptying Scintigraphy in Patients with Suspected Gastroparesis. Dig. Dis. Sci. 2013, 58, 1813–1815. [Google Scholar] [CrossRef]
- Van Den Driessche, M.; Peeters, K.; Marien, P.; Ghoos, Y.; Devlieger, H.; Veereman-Wauters, G. Gastric Emptying in Formula-Fed and Breast-Fed Infants Measured with the 13C-Octanoic Acid Breath Test. J. Pediatr. Gastroenterol. Nutr. 1999, 29, 46–51. [Google Scholar] [CrossRef]
- Meyer, R.; Foong, R.-X.M.; Thapar, N.; Kritas, S.; Shah, N. Systematic review of the impact of feed protein type and degree of hydrolysis on gastric emptying in children. BMC Gastroenterol. 2015, 15, 137. [Google Scholar] [CrossRef]
- Kelly, K.A. Gastric emptying of liquids and solids: Roles of proximal and distal stomach. Am. J. Physiol. Gastrointest. Liver Physiol. 1980, 239, G71–G76. [Google Scholar] [CrossRef]
- Camilleri, M.; Parkman, H.P.; Shafi, M.A.; Abell, T.L.; Gerson, L. Clinical Guideline: Management of Gastroparesis. Am. J. Gastroenterol. 2013, 108, 18–38. [Google Scholar] [CrossRef]
- Di Lorenzo, C.; Flores, A.F.; Buie, T.; Hyman, P.E. Intestinal motility and jejunal feeding in children with chronic intestinal pseudo-obstruction. Gastroenterology 1995, 108, 1379–1385. [Google Scholar] [CrossRef]
- Duggan, C.P.; Jaksic, T. Pediatric Intestinal Failure. N. Engl. J. Med. 2017, 377, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, K.; Flint, A.; Mouzaki, M.; Carpenter, A.; Haliburton, B.; Bannister, L.; Norgrove, H.; Hoffman, L.; Mack, D.; Stintzi, A.; et al. Blenderized Enteral Nutrition Diet Study: Feasibility, Clinical, and Microbiome Outcomes of Providing Blenderized Feeds Through a Gastric Tube in a Medically Complex Pediatric Population. JPEN J. Parenter Enter. Nutr. 2018, 42, 1046–1060. [Google Scholar] [CrossRef] [PubMed]
- Gu, L.; Ding, C.; Tian, H.; Yang, B.; Zhang, X.; Hua, Y.; Zhu, Y.; Gong, J.; Zhu, W.; Li, J.; et al. Serial Frozen Fecal Microbiota Transplantation in the Treatment of Chronic Intestinal Pseudo-obstruction: A Preliminary Study. J. Neurogastroenterol. Motil. 2017, 23, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Pentiuk, S.; O’Flaherty, T.; Santoro, K.; Willging, P.; Kaul, A. Pureed by gastrostomy tube diet improves gagging and retching in children with fundoplication. JPEN J. Parenter Enter. Nutr. 2011, 35, 375–379. [Google Scholar] [CrossRef]
- Samela, K.; Mokha, J.; Emerick, K.; Davidovics, Z.H. Transition to a Tube Feeding Formula with Real Food Ingredients in Pediatric Patients with Intestinal Failure. Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr. 2017, 32, 277–281. [Google Scholar] [CrossRef]
- Lambe, C.; Goulet, O.; Norsa, L. Colon importance in short bowel syndrome. Aging (Albany N. Y.) 2019, 11, 9961–9962. [Google Scholar] [CrossRef]
- Pironi, L.; Goulet, O.; Buchman, A.; Messing, B.; Gabe, S.; Candusso, M.; Bond, G.; Gupte, G.; Pertkiewicz, M.; Steiger, E.; et al. Outcome on home parenteral nutrition for benign intestinal failure: A review of the literature and benchmarking with the European prospective survey of ESPEN. Clin. Nutr. 2012, 31, 831–845. [Google Scholar] [CrossRef]
- Han, S.M.; Knell, J.; Henry, O.; Hong, C.R.; Han, G.Y.; Staffa, S.J.; Modi, B.P.; Jaksic, T. Long-Term Outcomes and Disease Burden of Neonatal Onset Short Bowel Syndrome. J. Pediatr. Surg. 2020, 55, 164–168. [Google Scholar] [CrossRef]
- Macharia, E.W. Comparison of upper gastrointestinal contrast studies and pH/impedance tests for the diagnosis of childhood gastro-oesophageal reflux. Pediatr. Radiol. 2012, 42, 946–951. [Google Scholar] [CrossRef]
- Katzka, D.A. A gastroenterologist’s perspective on the role of barium esophagography in gastroesophageal reflux disease. Abdom. Radiol. (N. Y.) 2018, 43, 1319–1322. [Google Scholar] [CrossRef] [PubMed]
- Lundell, L.R.; Dent, J.; Bennett, J.R.; Blum, A.L.; Armstrong, D.; Galmiche, J.P.; Johnson, F.; Hongo, M.; Richter, J.E.; Spechler, S.J.; et al. Endoscopic assessment of oesophagitis: Clinical and functional correlates and further validation of the Los Angeles classification. Gut 1999, 45, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Johnsson, F.; Joelsson, B.; Gudmundsson, K.; Greiff, L. Symptoms and endoscopic findings in the diagnosis of gastroesophageal reflux disease. Scand. J. Gastroenterol. 1987, 22, 714–718. [Google Scholar] [CrossRef] [PubMed]
- Ching, Y.A.; Modi, B.P.; Jaksic, T.; Duggan, C. High diagnostic yield of gastrointestinal endoscopy in children with intestinal failure. J. Pediatr. Surg. 2008, 43, 906–910. [Google Scholar] [CrossRef] [PubMed]
- Nikaki, K.; Woodland, P.; Sifrim, D. Adult and paediatric GERD: Diagnosis, phenotypes and avoidance of excess treatments. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 529–542. [Google Scholar] [CrossRef]
- Gyawali, C.P.; Kahrilas, P.J.; Savarino, E.; Zerbib, F.; Mion, F.; Smout, A.J.P.M.; Vaezi, M.; Sifrim, D.; Fox, M.R.; Vela, M.F.; et al. Modern diagnosis of GERD: The Lyon Consensus. Gut 2018, 67, 1351–1362. [Google Scholar] [CrossRef]
- Mahoney, L.B.; Nurko, S.; Rosen, R. The Prevalence of Rome IV Nonerosive Esophageal Phenotypes in Children. J. Pediatr. 2017, 189, 86–91. [Google Scholar] [CrossRef]
- Rosen, R.; Garza, J.M.; Tipnis, N.; Nurko, S. An ANMS-NASPGHAN consensus document on esophageal and antroduodenal manometry in children. Neurogastroenterol. Motil. 2018, 30. [Google Scholar] [CrossRef]
- Ferris, L.; King, S.; McCall, L.; Rommel, N.; Scholten, I.; Teague, W.; Doeltgen, S.; Omari, T. Piecemeal Deglutition and the Implications for Pressure Impedance Dysphagia Assessment in Pediatrics. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 713–719. [Google Scholar] [CrossRef]
- Patcharatrakul, T.; Gonlachanvit, S. Technique of functional and motility test: How to perform antroduodenal manometry. J. Neurogastroenterol. Motil. 2013, 19, 395–404. [Google Scholar] [CrossRef]
- Faure, C.; Goulet, O.; Ategbo, S.; Breton, A.; Tounian, P.; Ginies, J.L.; Roquelaure, B.; Despres, C.; Scaillon, M.; Maurage, C.; et al. Chronic intestinal pseudoobstruction syndrome: Clinical analysis, outcome, and prognosis in 105 children. French-Speaking Group of Pediatric Gastroenterology. Dig. Dis. Sci. 1999, 44, 953–959. [Google Scholar] [CrossRef] [PubMed]
- Fell, J.M.; Smith, V.V.; Milla, P.J. Infantile chronic idiopathic intestinal pseudo-obstruction: The role of small intestinal manometry as a diagnostic tool and prognostic indicator. Gut 1996, 39, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Knowles, C.H.; Lindberg, G.; Panza, E.; De Giorgio, R. New perspectives in the diagnosis and management of enteric neuropathies. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 206–218. [Google Scholar] [CrossRef] [PubMed]
- Sigurdsson, L.; Reyes, J.; Kocoshis, S.A.; Mazariegos, G.; Abu-Elmagd, K.M.; Bueno, J.; Di Lorenzo, C. Intestinal transplantation in children with chronic intestinal pseudo-obstruction. Gut 1999, 45, 570–574. [Google Scholar] [CrossRef]
- Abell, T.L.; Camilleri, M.; Donohoe, K.; Hasler, W.L.; Lin, H.C.; Maurer, A.H.; McCallum, R.W.; Nowak, T.; Nusynowitz, M.L.; Parkman, H.P.; et al. Consensus recommendations for gastric emptying scintigraphy: A joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am. J. Gastroenterol. 2008, 103, 753–763. [Google Scholar] [CrossRef]
- Szarka, L.A.; Camilleri, M. Methods for measurement of gastric motility. Am. J. Physiol. Gastrointest. Liver Physiol. 2009, 296, G461–G475. [Google Scholar] [CrossRef]
- Degen, L.P.; Phillips, S.F. Variability of gastrointestinal transit in healthy women and men. Gut 1996, 39, 299–305. [Google Scholar] [CrossRef]
- Talley, N.J.; Locke, G.R.; Lahr, B.D.; Zinsmeister, A.R.; Tougas, G.; Ligozio, G.; Rojavin, M.A.; Tack, J. Functional dyspepsia, delayed gastric emptying, and impaired quality of life. Gut 2006, 55, 933–939. [Google Scholar] [CrossRef]
- Farmer, A.D.; Scott, S.M.; Hobson, A.R. Gastrointestinal motility revisited: The wireless motility capsule. United Eur. Gastroenterol. J. 2013, 1, 413–421. [Google Scholar] [CrossRef]
- Stanger, J.D.; Oliveira, C.; Blackmore, C.; Avitzur, Y.; Wales, P.W. The impact of multi-disciplinary intestinal rehabilitation programs on the outcome of pediatric patients with intestinal failure: A systematic review and meta-analysis. J. Pediatr. Surg. 2013, 48, 983–992. [Google Scholar] [CrossRef]
- Medoff-Cooper, B.; Rankin, K.; Li, Z.; Liu, L.; White-Traut, R. Multisensory intervention for preterm infants improves sucking organization. Adv. Neonatal. Care 2015, 15, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R.; Vandenplas, Y.; Singendonk, M.; Cabana, M.; DiLorenzo, C.; Gottrand, F.; Gupta, S.; Langendam, M.; Staiano, A.; Thapar, N.; et al. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 516–554. [Google Scholar] [CrossRef] [PubMed]
- Billeaud, C.; Guillet, J.; Sandler, B. Gastric emptying in infants with or without gastro-oesophageal reflux according to the type of milk. Eur. J. Clin. Nutr. 1990, 44, 577–583. [Google Scholar] [PubMed]
- Simeone, D.; Caria, M.C.; Miele, E.; Staiano, A. Treatment of childhood peptic esophagitis: A double-blind placebo-controlled trial of nizatidine. J. Pediatr. Gastroenterol. Nutr. 1997, 25, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Becker, H.D.; Reeder, D.D.; Thompson, J.C. Extraction of circulating endogenous gastrin by the small bowel. Gastroenterology 1973, 65, 903–906. [Google Scholar] [CrossRef]
- Squires, R.H.; Duggan, C.; Teitelbaum, D.H.; Wales, P.W.; Balint, J.; Venick, R.; Rhee, S.; Sudan, D.; Mercer, D.; Martinez, J.A.; et al. Natural history of pediatric intestinal failure: Initial report from the Pediatric Intestinal Failure Consortium. J. Pediatr. 2012, 161, 723–728.e2. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Rudolph, C.D.; Di Lorenzo, C.; Hassall, E.; Liptak, G.; Mazur, L.; Sondheimer, J.; Staiano, A.; Thomson, M.; Veereman-Wauters, G.; et al. Pediatric gastroesophageal reflux clinical practice guidelines: Joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J. Pediatr. Gastroenterol. Nutr. 2009, 49, 498–547. [Google Scholar] [CrossRef]
- Mt-Isa, S.; Tomlin, S.; Sutcliffe, A.; Underwood, M.; Williamson, P.; Croft, N.M.; Ashby, D. Prokinetics Prescribing in Paediatrics: Evidence on Cisapride, Domperidone, and Metoclopramide. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 508–514. [Google Scholar] [CrossRef]
- Pritchard, D.S.; Baber, N.; Stephenson, T. Should domperidone be used for the treatment of gastro-oesophageal reflux in children? Systematic review of randomized controlled trials in children aged 1 month to 11 years old. Br. J. Clin. Pharm. 2005, 59, 725–729. [Google Scholar] [CrossRef]
- Rao, A.S.; Camilleri, M. Review article: Metoclopramide and tardive dyskinesia. Aliment. Pharmacol. Ther. 2010, 31, 11–19. [Google Scholar] [CrossRef]
- Hibbs, A.M.; Lorch, S.A. Metoclopramide for the treatment of gastroesophageal reflux disease in infants: A systematic review. Pediatrics 2006, 118, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Djeddi, D.; Kongolo, G.; Lefaix, C.; Mounard, J.; Léké, A. Effect of domperidone on QT interval in neonates. J. Pediatr. 2008, 153, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Bines, J.E.; Quinlan, J.E.; Treves, S.; Kleinman, R.E.; Winter, H.S. Efficacy of domperidone in infants and children with gastroesophageal reflux. J. Pediatr. Gastroenterol. Nutr. 1992, 14, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Franzese, A.; Borrelli, O.; Corrado, G.; Rea, P.; Di Nardo, G.; Grandinetti, A.L.; Dito, L.; Cucchiara, S. Domperidone is more effective than cisapride in children with diabetic gastroparesis. Aliment. Pharmacol. Ther. 2002, 16, 951–957. [Google Scholar] [CrossRef]
- Hegar, B.; Alatas, S.; Advani, N.; Firmansyah, A.; Vandenplas, Y. Domperidone versus cisapride in the treatment of infant regurgitation and increased acid gastro-oesophageal reflux: A pilot study. Acta Paediatr. 2009, 98, 750–755. [Google Scholar] [CrossRef]
- Raphael, B.P.; Nurko, S.; Jiang, H.; Hart, K.; Kamin, D.S.; Jaksic, T.; Duggan, C. Cisapride improves enteral tolerance in pediatric short-bowel syndrome with dysmotility. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 590–594. [Google Scholar] [CrossRef]
- Ng, S.C.-Y.; Gomez, J.M.; Rajadurai, V.S.; Saw, S.-M.; Quak, S.-H. Establishing enteral feeding in preterm infants with feeding intolerance: A randomized controlled study of low-dose erythromycin. J. Pediatr. Gastroenterol. Nutr. 2003, 37, 554–558. [Google Scholar] [CrossRef]
- Ng, P.C.; So, K.W.; Fung, K.S.; Lee, C.H.; Fok, T.F.; Wong, E.; Wong, W.; Cheung, K.L.; Cheng, A.F. Randomised controlled study of oral erythromycin for treatment of gastrointestinal dysmotility in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 2001, 84, F177–F182. [Google Scholar] [CrossRef]
- Di Lorenzo, C.; Flores, A.F.; Tomomasa, T.; Hyman, P.E. Effect of erythromycin on antroduodenal motility in children with chronic functional gastrointestinal symptoms. Dig. Dis. Sci. 1994, 39, 1399–1404. [Google Scholar] [CrossRef]
- Caron, F.; Ducrotte, P.; Lerebours, E.; Colin, R.; Humbert, G.; Denis, P. Effects of amoxicillin-clavulanate combination on the motility of the small intestine in human beings. Antimicrob. Agents Chemother. 1991, 35, 1085–1088. [Google Scholar] [CrossRef]
- Gomez, R.; Fernandez, S.; Aspirot, A.; Punati, J.; Skaggs, B.; Mousa, H.; Di Lorenzo, C. Effect of amoxicillin/clavulanate on gastrointestinal motility in children. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 780–784. [Google Scholar] [CrossRef] [PubMed]
- Omari, T.I.; Benninga, M.A.; Sansom, L.; Butler, R.N.; Dent, J.; Davidson, G.P. Effect of baclofen on esophagogastric motility and gastroesophageal reflux in children with gastroesophageal reflux disease: A randomized controlled trial. J. Pediatr. 2006, 149, 468–474. [Google Scholar] [CrossRef] [PubMed]
- Lidums, I.; Lehmann, A.; Checklin, H.; Dent, J.; Holloway, R.H. Control of transient lower esophageal sphincter relaxations and reflux by the GABA(B) agonist baclofen in normal subjects. Gastroenterology 2000, 118, 7–13. [Google Scholar] [CrossRef]
- Law, N.M.; Bharucha, A.E.; Undale, A.S.; Zinsmeister, A.R. Cholinergic stimulation enhances colonic motor activity, transit, and sensation in humans. Am. J. Physiol. Gastrointest. Liver Physiol. 2001, 281, G1228–G1237. [Google Scholar] [CrossRef] [PubMed]
- Manini, M.L.; Camilleri, M.; Grothe, R.; Di Lorenzo, C. Application of Pyridostigmine in Pediatric Gastrointestinal Motility Disorders: A Case Series. Paediatr. Drugs 2018, 20, 173–180. [Google Scholar] [CrossRef]
- Gmora, S.; Poenaru, D.; Tsai, E. Neostigmine for the treatment of pediatric acute colonic pseudo-obstruction. J. Pediatr. Surg. 2002, 37, E28. [Google Scholar] [CrossRef]
- Choudhury, A.; Rahyead, A.; Kammermeier, J.; Mutalib, M. The Use of Pyridostigmine in a Child with Chronic Intestinal Pseudo-Obstruction. Pediatrics 2018, 141, S404–S407. [Google Scholar] [CrossRef]
- Di Lorenzo, C.; Lucanto, C.; Flores, A.F.; Idries, S.; Hyman, P.E. Effect of Octreotide on Gastrointestinal Motility in Children with Functional Gastrointestinal Symptoms. J. Pediatr. Gastroenterol. Nutr. 1998, 27, 508–512. [Google Scholar] [CrossRef]
- Emmanuel, A.V.; Kamm, M.A.; Roy, A.J.; Kerstens, R.; Vandeplassche, L. Randomised clinical trial: The efficacy of prucalopride in patients with chronic intestinal pseudo-obstruction—A double-blind, placebo-controlled, cross-over, multiple n = 1 study. Aliment. Pharm. 2012, 35, 48–55. [Google Scholar] [CrossRef]
- Foglia, R.P.; Fonkalsrud, E.W.; Ament, M.E.; Byrne, W.J.; Berquist, W.; Siegel, S.C.; Katz, R.M.; Rachelefsky, G.S. Gastroesophageal fundoplication for the management of chronic pulmonary disease in children. Am. J. Surg. 1980, 140, 72–79. [Google Scholar] [CrossRef]
- Rothenberg, S.S. Two decades of experience with laparoscopic nissen fundoplication in infants and children: A critical evaluation of indications, technique, and results. J. Laparoendosc. Adv. Surg. Tech. A 2013, 23, 791–794. [Google Scholar] [CrossRef] [PubMed]
- Fonkalsrud, E.W.; Pitt, H.A.; Berquist, W.E.; Ament, M.E. Surgical management of chronic intestinal pseudo-obstruction in infancy and childhood. Prog. Pediatr. Surg. 1989, 24, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Abell, T.L.; Van Cutsem, E.; Abrahamsson, H.; Huizinga, J.D.; Konturek, J.W.; Galmiche, J.P.; VoelIer, G.; Filez, L.; Everts, B.; Waterfall, W.E.; et al. Gastric electrical stimulation in intractable symptomatic gastroparesis. Digestion 2002, 66, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Vick, L.R.; Runnels, M.J.; Gosche, J.R.; Abell, T. Gastric electrical stimulation for children with intractable nausea and gastroparesis. J. Pediatr. Surg. 2008, 43, 437–442. [Google Scholar] [CrossRef]
- Teich, S.; Mousa, H.M.; Punati, J.; Di Lorenzo, C. Efficacy of permanent gastric electrical stimulation for the treatment of gastroparesis and functional dyspepsia in children and adolescents. J. Pediatr. Surg. 2013, 48, 178–183. [Google Scholar] [CrossRef]
- Rodriguez, L.; Rosen, R.; Manfredi, M.; Nurko, S. Endoscopic intrapyloric injection of botulinum toxin A in the treatment of children with gastroparesis: A retrospective, open label study. Gastrointest. Endosc. 2012, 75, 302–309. [Google Scholar] [CrossRef]
- Nordgaard, I.; Hansen, B.S.; Mortensen, P.B. Colon as a digestive organ in patients with short bowel. Lancet 1994, 343, 373–376. [Google Scholar] [CrossRef]
- Royall, D.; Wolever, T.M.; Jeejeebhoy, K.N. Evidence for colonic conservation of malabsorbed carbohydrate in short bowel syndrome. Am. J. Gastroenterol. 1992, 87, 751–756. [Google Scholar]
| Causes of IF | Possible Mechanisms Contributing to GI Dysmotility |
|---|---|
| Necrotizing enterocolitis | Gastric hypergastrinemia and hypersecretion in extensive gut resection. Ischemic injury to the enteric nervous system or damage to the smooth muscle cells. |
| Gastroschisis | Oro-pharyngeal dysphagia. GERD. Hiatal hernia. Severe intestinal dysmotility in >30% of patients. Decreased ICC [11]. Damage of the smooth muscle cells due to bowel wall ischemia [12]. |
| Malrotation and midgut volvulus | GERD and gastric dysmotility. Small bowel dysmotility with neuropathic changes [13]. |
| Intestinal atresia | Severe dilatation of the proximal bowel with hypoperistalsis, reduction of the intramuscular nerve fibers [14]. Decreased ICC [15]. |
| Intestinal aganglionosis | Dysfunction of the ENS. Absent or sparse ICC in aganglionic and ganglionic bowel [16]. |
| PIPO | Small bowel always affected. Potential involvement of esophagus, stomach and colon, with dysphagia, gastroparesis and constipation. More severe disease course in myopathic type of PIPO. Decreased or absent ICC. |
| Symptom Triggers | Effect of IF | |
|---|---|---|
| Gastroesophageal reflux events | Number of events | Increased-Impaired gastric emptying |
| Gas/liquid composition | Liquid-Impaired gastric emptying | |
| Volume refluxed | Larger—more proximal events with longer clearance time Impaired gastric emptying | |
| Constituents of gastric juice | Acid | Gastric acid hypersecretion and hypergastrinemia |
| Bile acids | Duodeno-gastric reflux of bile acids—abnormal concentration/composition of bile acids | |
| Pepsin | Activated | |
| Symptom Modulators | ||
| Refluxate clearance | Hiatus hernia | Similar to general population |
| Hypotensive sphincter | Distortion of anatomy/Altered anatomy of the angle of His Increased frequency of TLESRs | |
| Peristaltic vigor | Slow/Absent propagation of esophageal peristalsis | |
| Tissue sensitivity | Epithelial injury | Higher incidence of GERD in gastroschisis |
| Central hypersensitivity | No data available for IF | |
| Peripheral hypersensitivity | No data available for IF | |
| Investigation | Assessment | Common Findings in IF |
|---|---|---|
| Videofluoroscopic swallow study (VFSS) | Assesses anatomic abnormalities in the upper aerodigestive tract; evaluates bolus movement during swallowing and risk of aspiration | Oro-pharyngeal dysphagia Aspiration. |
| Upper gastrointestinal contrast study | Evaluates anatomic abnormalities in the upper gastrointestinal tract | Esophageal dilatation. Hiatal hernia. Malrotation. Dilated small bowel loops, with possible contrast retention. |
| 24 h pH-impedance | Ambulatory, detects differentiates liquid, mixed, and gas GER events, acid and non-acid GER. Used as “Gold standard” in the GERD diagnostics. | Increased number of reflux episodes. Increased total acid exposure time. |
| Upper endoscopy | Anatomical and mucosal assessment of the upper GI tract. | Higher rate of esophageal erosive disease. Hiatal hernia Mucosal inflammation Proximal strictures |
| Oropharyngeal and esophageal manometry | Evaluates esophageal motor function and oro-pharyngeal coordination | Lower frequency and poor propagation of spontaneous swallows. Slow peristaltic propagation velocity. Aperistaltic esophageal body. |
| Scintigraphy for gastric emptying | Normal ranges available for liquid and solid meal in children | Delayed gastric emptying for liquid and solid meal. Abnormal gastric accommodation. |
| Antro-duodenal manometry | Evaluates motor function of the antrum and proximal small bowel. | Neuro-or myopathic small bowel. Absence of MMC (phase III complex). Abnormal postprandial phase. Antral hypomotility. |
| Motility Agent | Segments and Strength of Activity | Evidence |
|---|---|---|
| Metoclopramide | Esophagus + Stomach + Small bowel + | Not recommended in GERD or gastroparesis in children due to side effects (risk of extrapyramidal symptoms, tardive dyskinesia). Approved for short term treatment in adults with gastroparesis (US) [120]. Current literature is insufficient to either support or oppose the use of metoclopramide for gastroesophageal reflux disease in infants [121]. |
| Domperidone | Esophagus + Stomach + | Not recommended in GERD [119,122]. 4 weeks of therapy were only minimally effective infants and children with GERD [123]. Effective in children with diabetic gastroparesis [124]. |
| Cisapride | Esophagus + Stomach + Small bowel + Colon + | Withdrawn in July 2000 following cardiac adverse reactions in adults in UK. Decrease in regurgitation and acid reflux in infants [125]. Modest improvement in feeding tolerance in children with SBS and GI dysmotility [126]. |
| Erythromycin, Azithromycin | Esophagus + Stomach ++ Small bowel + | No effect on feeding tolerance or GERD in preterm infants [127]. Some evidence on improving enteral feeding in preterm infants with moderate/severe GI dysmotility [128]. Erythromycin rarely induced phase III (MMC) in patients who did not have it during fasting period [129]. |
| Amoxicillin-clavulanate | Small bowel + | Possible prokinetic effect through the release of intraluminal motilin or interaction of beta-lactam with postsynaptic gamma-aminobutyric acid receptors in myenteric plexus [130]. Induces phase III-type contractions in the duodenum in children [131]. |
| Baclofen | Esophagus + Stomach + | Reduction of reflux episodes by reducing the number of transient lower esophageal sphincter relaxations [132,133]. |
| Neostigmine, Pyridostigmine | Esophagus + Stomach + Small bowel + Colon + | Increase of GI motility by enhancing availability of acetylcholine at neuromuscular synapses, such as the myenteric plexus [134]. Case reports showing improvement in PIPO, colonic transit, esophageal motility [135,136,137]. |
| Octreotide | Stomach + Small bowel + Colon + | Induction of the phase III in the small bowel, decrease in antral motility [138]. |
| Prucalopride | Esophagus + Stomach + Small bowel + Colon + | Improvement of symptoms in adult patients with chronic pseudo-obstruction [139]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rybak, A.; Sethuraman, A.; Nikaki, K.; Koeglmeier, J.; Lindley, K.; Borrelli, O. Gastroesophageal Reflux Disease and Foregut Dysmotility in Children with Intestinal Failure. Nutrients 2020, 12, 3536. https://doi.org/10.3390/nu12113536
Rybak A, Sethuraman A, Nikaki K, Koeglmeier J, Lindley K, Borrelli O. Gastroesophageal Reflux Disease and Foregut Dysmotility in Children with Intestinal Failure. Nutrients. 2020; 12(11):3536. https://doi.org/10.3390/nu12113536
Chicago/Turabian StyleRybak, Anna, Aruna Sethuraman, Kornilia Nikaki, Jutta Koeglmeier, Keith Lindley, and Osvaldo Borrelli. 2020. "Gastroesophageal Reflux Disease and Foregut Dysmotility in Children with Intestinal Failure" Nutrients 12, no. 11: 3536. https://doi.org/10.3390/nu12113536
APA StyleRybak, A., Sethuraman, A., Nikaki, K., Koeglmeier, J., Lindley, K., & Borrelli, O. (2020). Gastroesophageal Reflux Disease and Foregut Dysmotility in Children with Intestinal Failure. Nutrients, 12(11), 3536. https://doi.org/10.3390/nu12113536





