Effect of Low-Immunogenic Yogurt Drinks and Probiotic Bacteria on Immunoreactivity of Cow’s Milk Proteins and Tolerance Induction—In Vitro and In Vivo Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacterial Strains and Growth Conditions
2.2. Yogurt Drinks
2.3. Immunoreactivity of the Tested Products
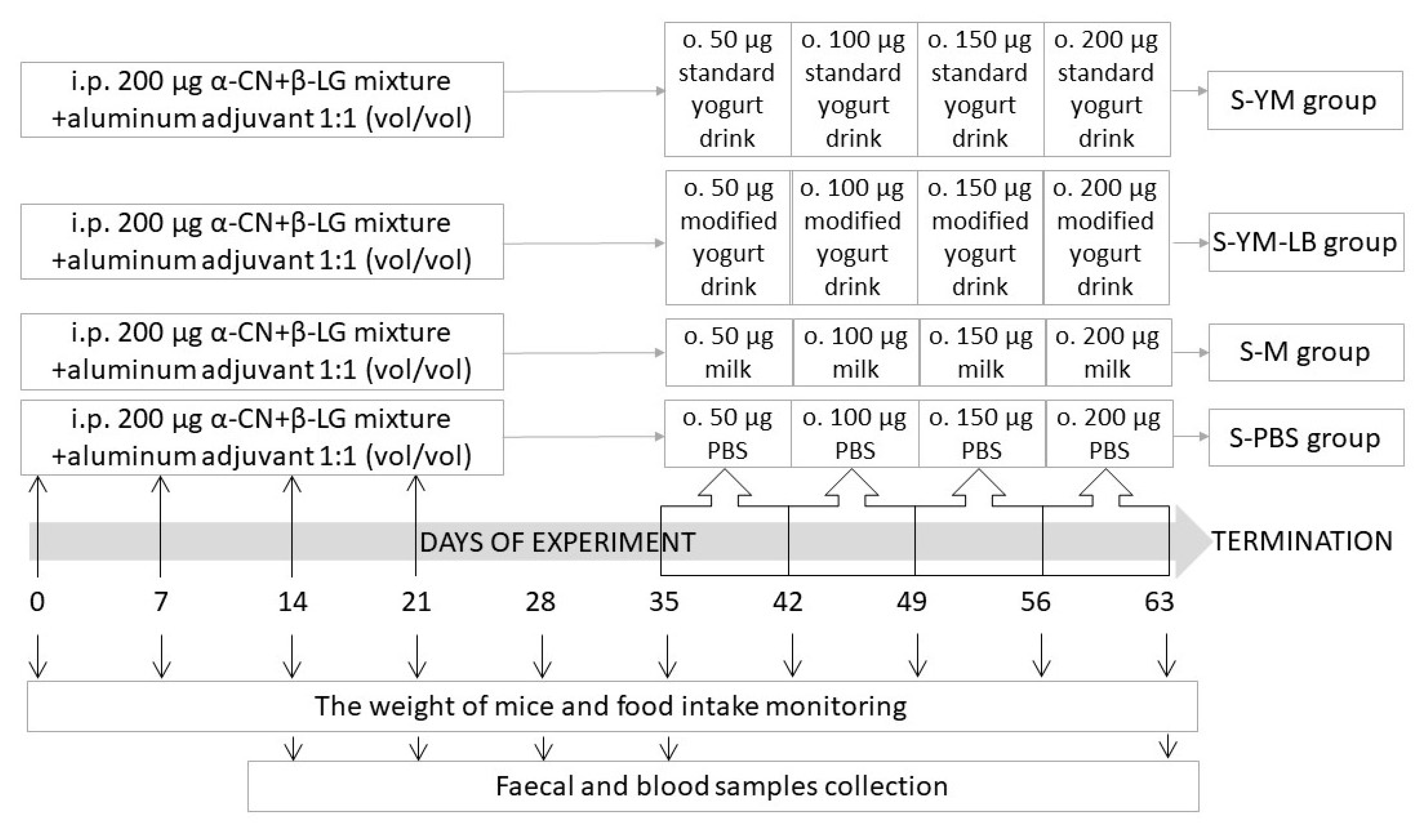
2.4. Studies in Mice with Induced Allergy to CMPs
2.4.1. Serum and Fecal Sample Collection
2.4.2. Indirect ELISA Assay of Total and Specific Antibodies
2.4.3. Lymphocyte Isolation
2.4.4. ELISpot Assay of IgA and IgG Antibody-Forming Cells (AFC) in Splenocytes
2.4.5. Cytokine Secretion Assay
2.4.6. Characteristics of Gut Microbiota
2.5. Statistical Analysis
3. Results and Discussion
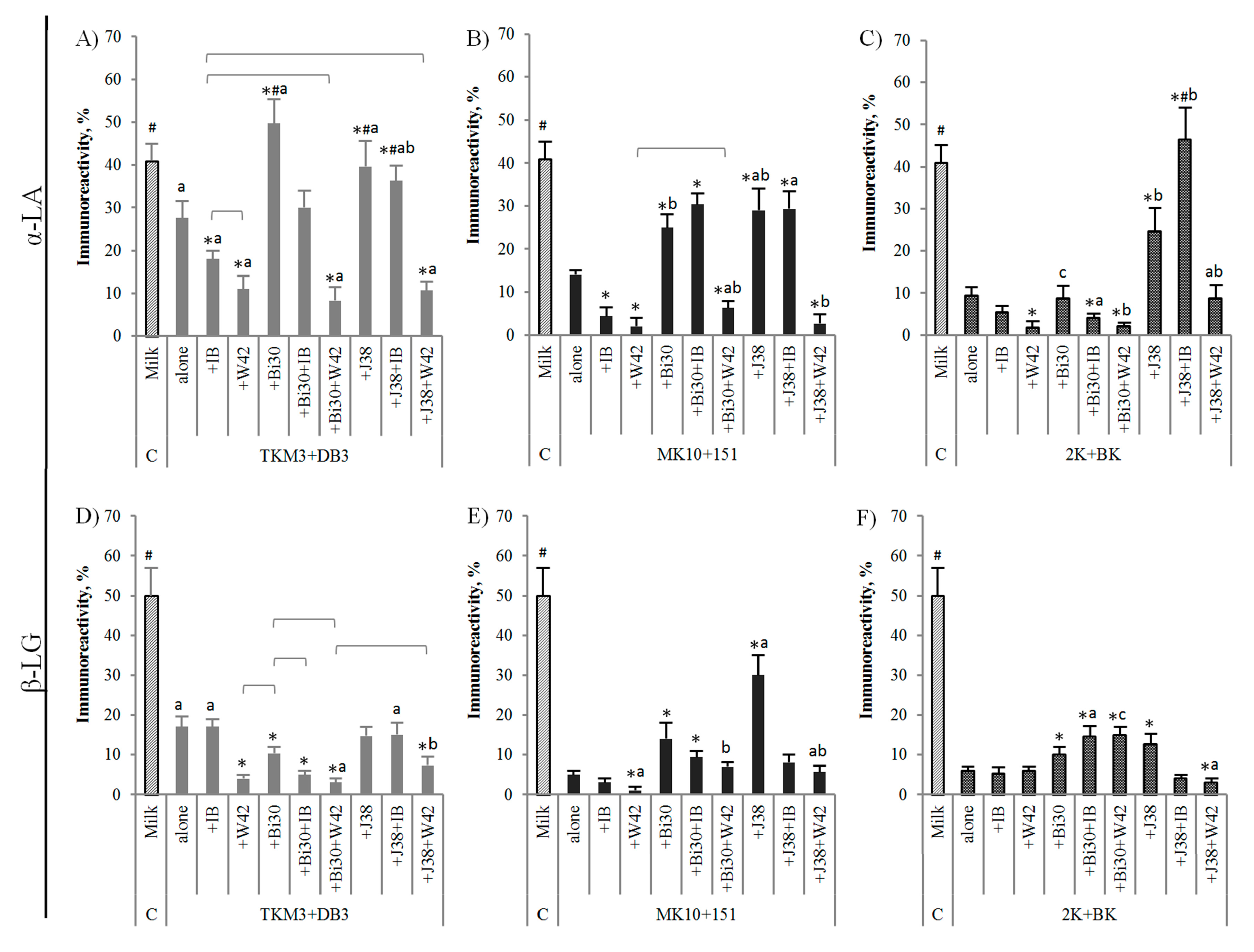
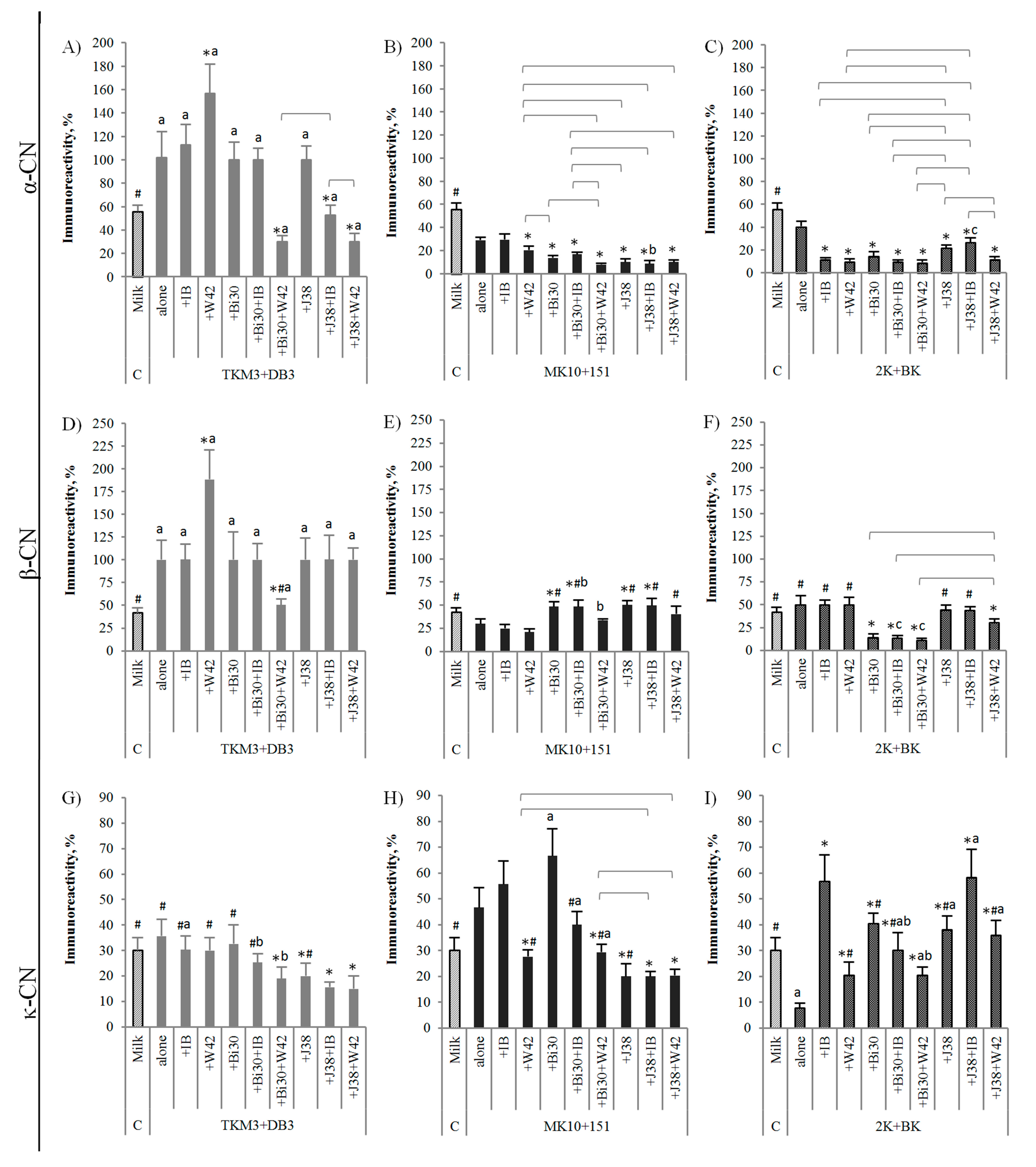
3.1. Immunoreactivity of Yogurt Drinks Fermented with Different Bacterial Sets
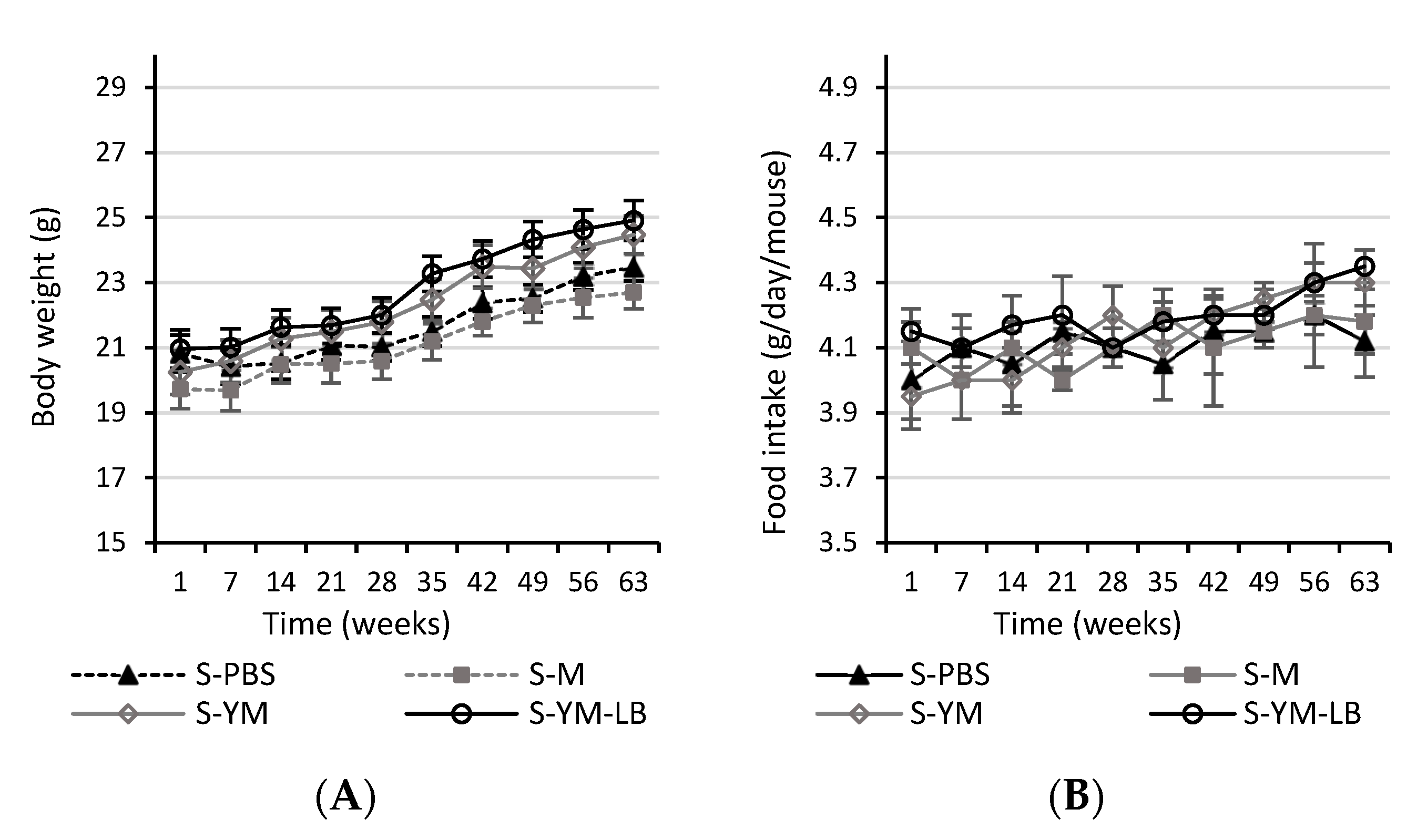
3.2. Animal Studies
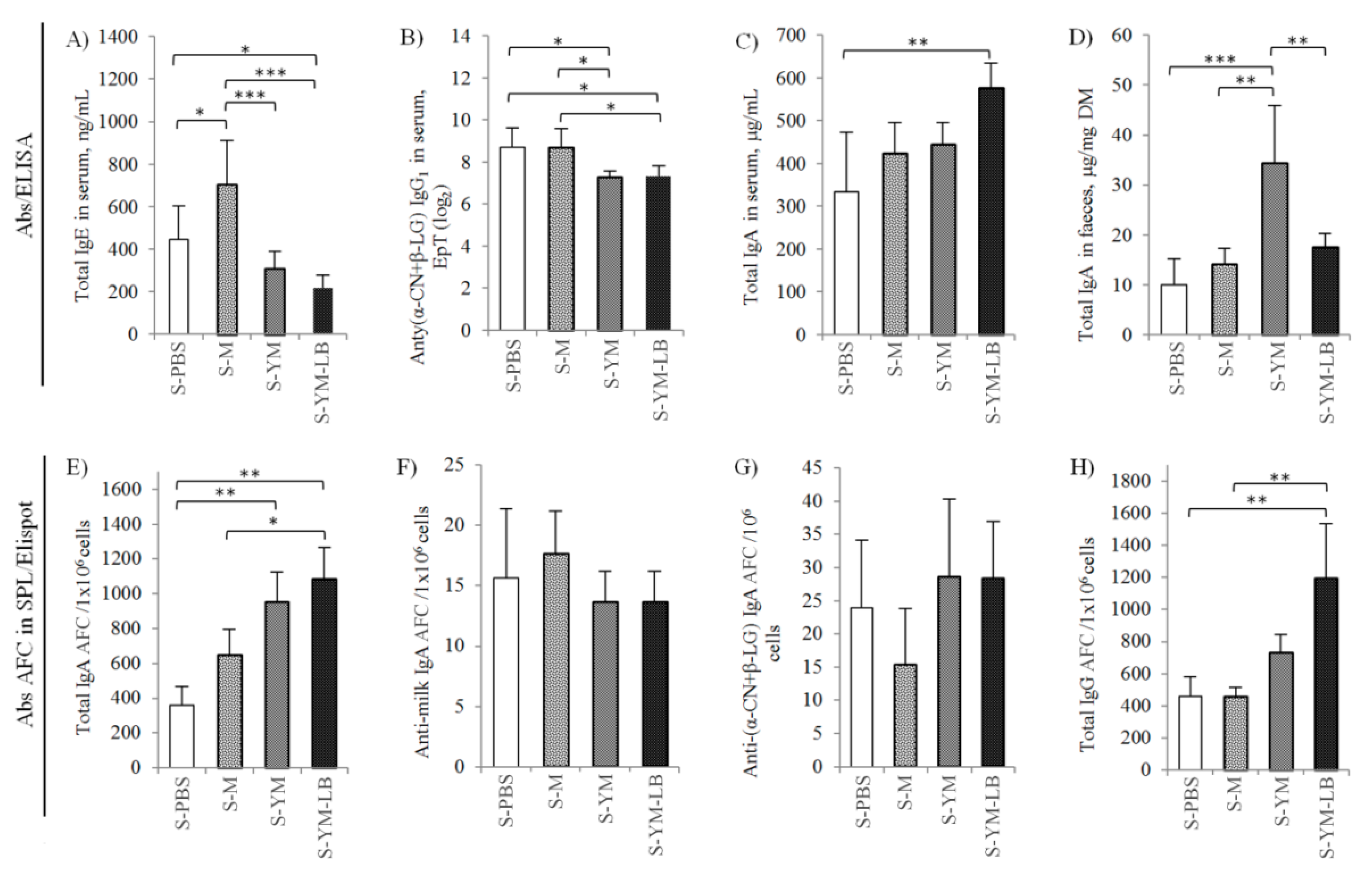
3.2.1. Humoral Response of Sensitized Mice to Yogurt Drinks
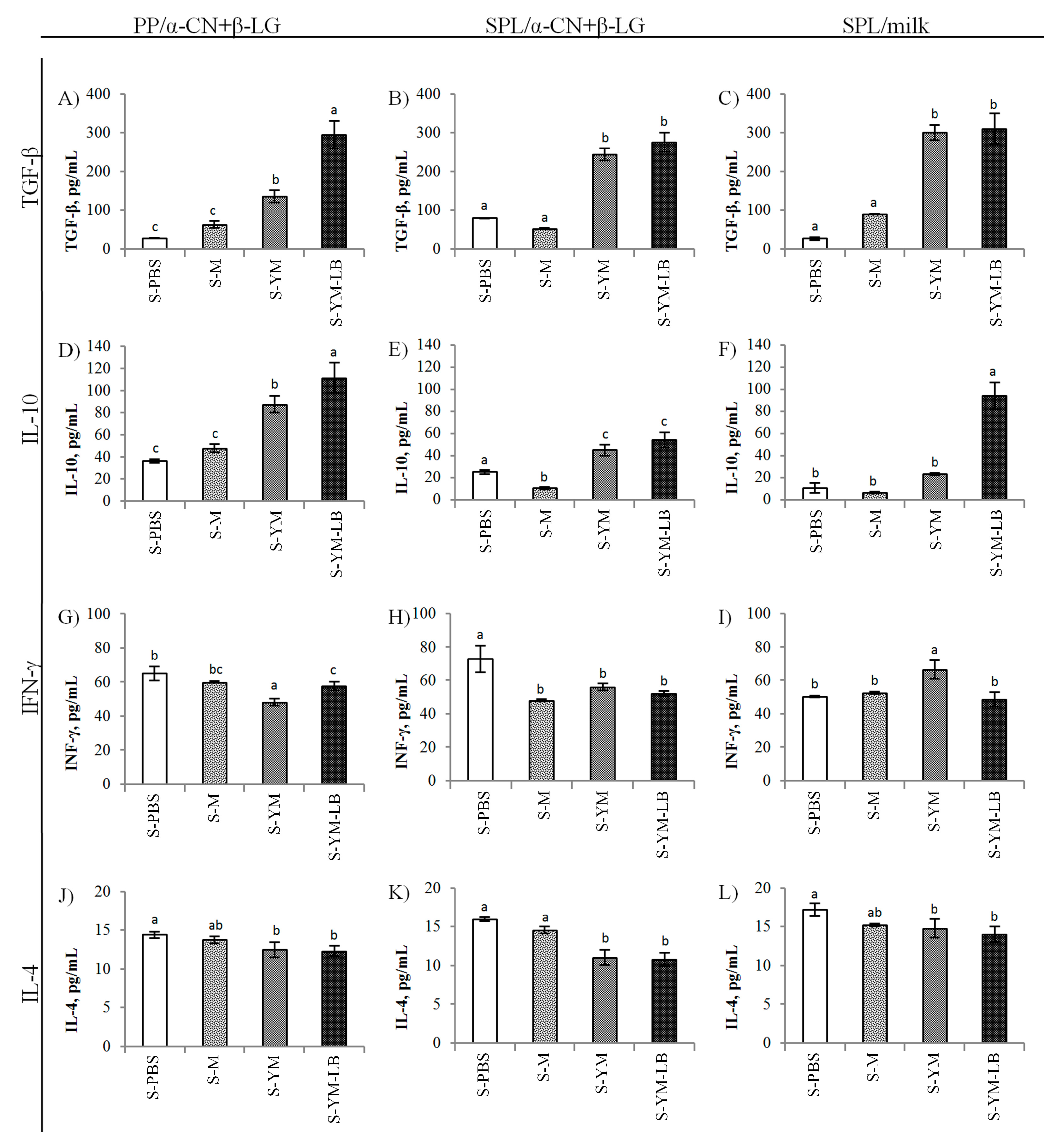
3.2.2. Cytokine Release in Splenocytes and Peyer’s Patches Cultures of the Tested Mice
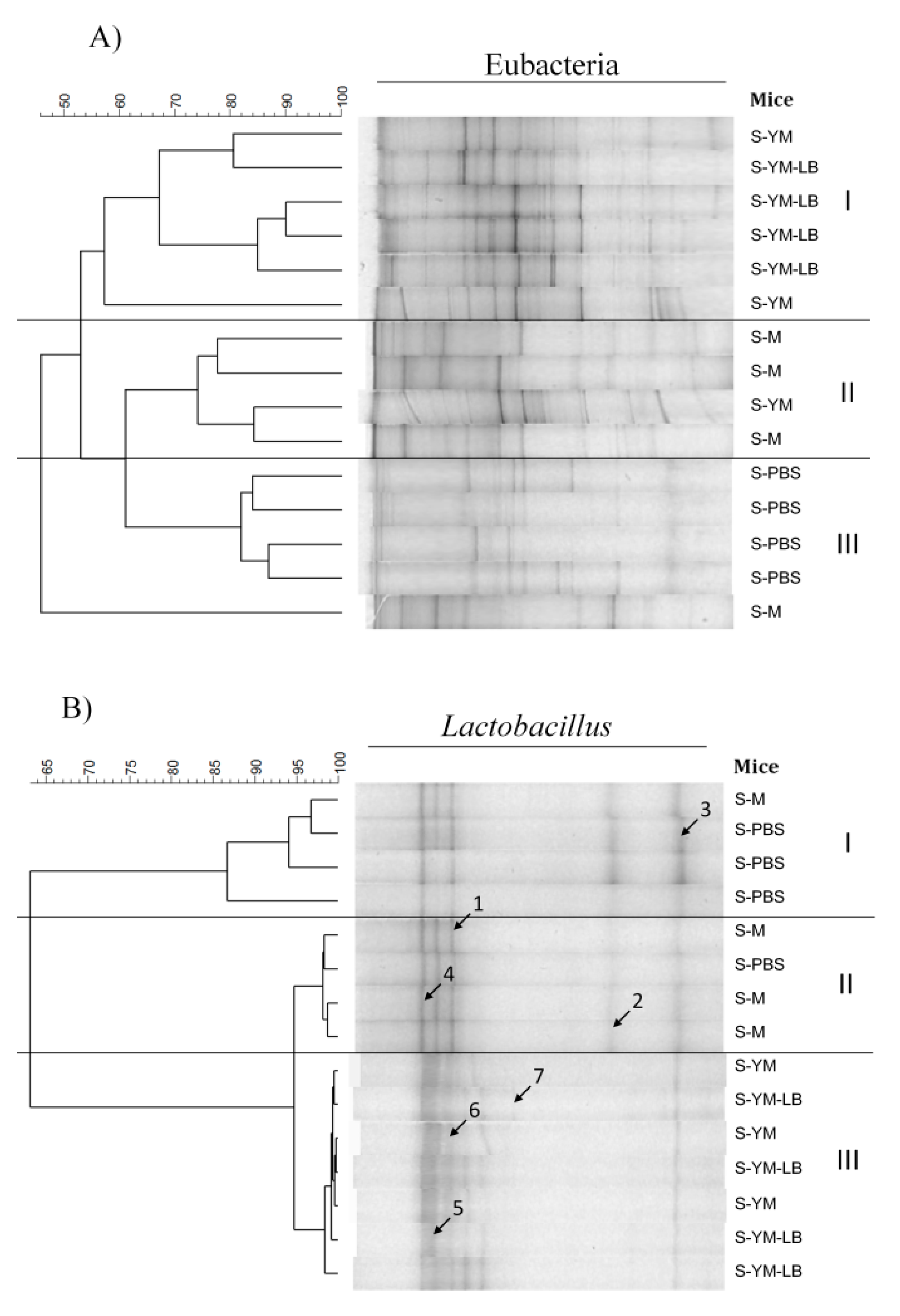
3.2.3. Effect of the Tested Yogurt Drinks on Cecal Microbiota
4. Summary
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- Brożek, J.L.; Terracciano, L.; Hsu, J.; Kreis, J.; Compalati, E.; Santesso, N.; Fiocchiand, A.; Schunemann, H.J. Oral immunotherapy for IgE-mediated cow’s milk allergy: A systematic review and meta-analysis. Clin. Exp. Allergy 2012, 42, 363–374. [Google Scholar] [CrossRef]
- Martorell Calatayud, C.; Muriel García, A.; Martorell Aragonés, A.; De La Hoz Caballer, B. Safety and efficacy profile and immunological changes associated with oral immunotherapy for IgE-mediated cow’s milk allergy in children: Systematic review and meta-analysis. J. Investig. Allergol. Clin. Immunol. 2014, 24, 298–307. [Google Scholar]
- Babaie, D.; Nabavi, M.; Arshi, S.; Mesdaghi, M.; Chavoshzadeh, Z.; Bemanian, M.H.; Tafakori, M.; Amirmoini, M.; Esmailzadeh, H.; Molatefi, R.; et al. Cow’s Milk Desensitization in Anaphylactic Patients: A New Personalized-dose Method. Iran J. Allergy Asthma Immunol. 2017, 16, 45–52. [Google Scholar]
- Perezabad, L.; Reche, M.; Valbuena, T.; Lopez-Fandino, R.; Molina, E.; Lopez-Exposito, I. Oral Food Desensitization in Children with IgE-Mediated Cow’s Milk Allergy: Immunological Changes Underlying Desensitization. Allergy Asthma Immunol. Res. 2017, 9, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Pessione, E.; Cirrincione, S. Bioactive molecules released in food by lactic acid bacteria: Encrypted peptides and biogenic amines. Front. Microbiol. 2016, 27, 876. [Google Scholar] [CrossRef]
- Wróblewska, B.; Kaliszewska-Suchodoła, A.; Markiewicz, L.H.; Szyc, A.; Wasilewska, E. Whey prefermented with beneficial microbes modulates immune response and lowers responsiveness to milk allergens in mouse model. J. Funct. Foods 2019, 54, 41–52. [Google Scholar] [CrossRef]
- Poza-Guedes, P.; Barrios, Y.; González Pérez, R.; Sánchez-Machín, I.; Franco, A.; Matheu, V. Yogurt in the Treatment of β-Lactoglobulin–Induced Gastrointestinal Cow’s Milk Allergy. J. Investig. Allergol. Clin. Immunol. 2016, 26, 314–343. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Monaco, S.; Russo, G.; Romano, A.; Liotti, L.; Verga, M.C.; Miceli Sopo, S. Yogurt is tolerated by the majority of children with IgE-mediated cow’s milk allergy. Allergol. Immunopathol. 2018, 47, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Kucukosmanoglu, E.; Ozen, E.; Eltan, S.B.; Ozkars, M.Y.; Keskin, O. Most children who are allergic to cow’s milk tolerate yogurt. J. Int. Med. Res. 2018, 46, 5099–5106. [Google Scholar] [CrossRef]
- Codex Standards for Fermented Milk. In Codex Alimentarius. Milk and Milk Products, 2nd ed.; WHO/FAO: Rome, Italy, 2011; pp. 6–16.
- Mohajeri, M.H.; Brummer, R.J.M.; Rastall, R.A.; Weersma, R.K.; Harmsen, H.J.M.; Faas, M.; Eggersdorfer, M. The role of the microbiome for human health: From basic science to clinical applications. Eur. J. Nutr. 2018, 57, S1–S14. [Google Scholar] [CrossRef]
- Wasilewska, E.; Wroblewska, B. Effectiveness and safety of probiotic preparations in clinical treatment of inflammatory bowel disease. Postepy Hig. Med. Dosw. 2018, 72, 159–174. [Google Scholar] [CrossRef]
- Wasilewska, E.; Zlotkowska, D.; Wróblewska, B. Yogurt starter cultures of Streptococcus thermophilus and Lactobacillus bulgaricus ameliorate symptoms and modulate the immune response on mouse model of dextran sulfate sodium-induced colitis. J. Dairy Sci. 2019, 102, 37–53. [Google Scholar] [CrossRef]
- Matricardi, P.M. Probiotics against allergy: Data, doubts, and perspectives. Allergy 2002, 57, 185–187. [Google Scholar] [CrossRef]
- Kumar, B.V.; Vijayendra, S.V.N.; Reddy, O.V.S. Trends in dairy and non-dairy probiotic products—A review. J. Food Sci. Technol. 2015, 52, 6112–6124. [Google Scholar] [CrossRef]
- Lee, T.T.; Morisset, M.; Astier, C.; Moneret-Vautrin, D.A.; Cordebar, V.; Beaudouin, E.; Codreanu, F.; Bihain, B.E.; Kanny, G. Contamination of probiotic preparations with milk allergens can cause anaphylaxis in children with cow’s milk allergy. J. Allergy Clin. Immunol. 2007, 119, 746–747. [Google Scholar] [CrossRef]
- Taylor, A.L.; Dunstan, J.A.; Prescott, S.L. Probiotic supplementation for the first 6 months of life fails to reduce the risk of atopic dermatitis and increase the risk of allergen sensitization in high-risk children: A randomized control trial. J. Allergy Clin. Immunol. 2007, 119, 184–191. [Google Scholar] [CrossRef]
- Abbring, S.; Hols, G.; Garssen, J.; van Esch, B.C.A.M. Raw cow’s milk consumption and allergic diseases—The potential role of bioactive whey proteins. Eur. J. Pharmacol. 2019, 843, 55–65. [Google Scholar] [CrossRef]
- Restani, P.; Ballabio, C.; Di Lorenzo, C.; Tripodi, S.; Fiocchi, A. Molecular aspects of milk allergens and their role in clinical events. Anal. Bioanal. Chem. 2009, 395, 47–56. [Google Scholar] [CrossRef]
- Elsayed, S.; Hill, D.J.; Do, T.V. Evaluation of the allergenicity and antigenicity of bovine milk alphas1-casein using extensively purified synthetic peptides. Scand. J. Immunol. 2004, 60, 486–493. [Google Scholar] [CrossRef]
- Ruiter, B.; Tregoat, V.; M’Rabet, L.; Garssen, J.; Bruijnzeel-Koomen, C.A.; Knol, E.F.; Hoffen, E. Characterization of T cell epitopes in αs1-casein in cow’s milk allergic, atopic and non-atopic children. Clin. Exp. Allergy 2006, 36, 303–310. [Google Scholar] [CrossRef]
- Matsuo, H.; Yokooji, T.; Taogoshi, T. Common food allergens and their IgE-binding epitopes. Allergol. Int. 2015, 64, 332–343. [Google Scholar] [CrossRef]
- Villa, C.; Costa, J.; Oliveira, P.P.M.B.; Mafra, I. Bovine Milk Allergens: A Comprehensive Review. Compr. Rev. Food Sci. Food Saf. 2018, 17, 137–160. [Google Scholar] [CrossRef]
- Wawrzyniak, M.; O’Mahony, L.; Akdis, M. Role of regulatory cells in oral tolerance. Allergy Asthma Immunol. Res. 2017, 9, 107–115. [Google Scholar] [CrossRef]
- Markiewicz, L.H.; Biedrzycka, E.; Wasilewska, E.; Bielecka, M. Differentiation of strains identified as Bifidobacterium animalis subsp. lactis. Acta Aliment. 2009, 38, 293–301. [Google Scholar] [CrossRef]
- Markiewicz, L.H.; Biedrzycka, E.; Wasilewska, E.; Bielecka, M. Rapid molecular identification and characteristics of Lactobacillus strains. Folia Microbiol. 2010, 55, 481–488. [Google Scholar] [CrossRef]
- Wasilewska, E.; Ratowska, J.; Bielecka, M.; Zduńczyk, Z.; Jankowski, J. Mannanoligosaccharides or flavomycin in turkeys’ diets: Effect on mucosa-associated microflora and growth performance. J. Anim. Feed Sci. 2010, 19, 599–612. [Google Scholar] [CrossRef]
- Bielecka, M.; Majkowska, A.; Biedrzycka, E. Selection of strain for yogurt starters regarding their antibacterial properties. Pol. J. Food Nutr. Sci. 1994, 3, 51–61. [Google Scholar]
- Bielecka, M.; Majkowska, A. Effect of spray drying temperature of yoghurt on the survival of starter cultures, moisture content and sensoric properties of yoghurt powder. Nahrung 2000, 44, 257–260. [Google Scholar] [CrossRef]
- Bielecka, M.; Majkowska, A.; Biedrzycka, E.; Biedrzycka, E. Microbiological changes in modified yoghurts during manufacture and storage. Prog. Biotechnol. 2000, 17, 283–289. [Google Scholar] [CrossRef]
- Wasilewska, E.; Markiewicz, L.H.; Bielecka, M. Bifidobacterium strains inhabiting the gastrointestinal tract of rat as potential probiotics for animals. J. Anim. Feed Sci. 2008, 17, 398–410. [Google Scholar] [CrossRef][Green Version]
- Wróblewska, B.; Karamać, M.; Amarowicz, R.; Szymkiewicz, A.; Troszyńska, A.; Kubicka, E. Immunoreactive properties of peptide fraction of cow whey milk protein after enzymatic hydrolysis. Int. J. Food Sci. Technol. 2004, 39, 839–850. [Google Scholar] [CrossRef]
- Wróblewska, B.; Kaliszewska, A. Cow’s milk protein immunoreactivity and allergenicity in processed food. Czech J. Food Sci. 2012, 30, 211–219. [Google Scholar] [CrossRef]
- Donkor, O.N.; Henriksson, A.; Vasiljevic, T.; Shah, N.P. Proteolytic activity of dairy lactic acid bacteria and probiotics as determinant of growth and in vitro angiotensin-converting enzyme inhibitory activity in fermented milk. Lait 2007, 86, 21–38. [Google Scholar] [CrossRef]
- Kleber, N.; Weyrich, U.; Hinrichs, J. Screening for lactic acid bacteria with potential to reduce antigenic response of β-lactoglobulin in bovine skim milk and sweet whey. Innov. Food Sci. Emerg. Technol. 2006, 7, 233–238. [Google Scholar] [CrossRef]
- Rui, H.; Huang, J.; Xing, G.; Zhang, Q.; Li, W.; Dong, M. Changes in soy protein immunoglobulin E reactivity, protein degradation, and conformation through fermentation with Lactobacillus plantarum strains. LWT 2019, 99, 156–165. [Google Scholar] [CrossRef]
- Snel, J.; Vissers, Y.M.; Smit, B.A.; Jongen, J.M.J.; van der Meulen, E.T.; Zwijsen, R.; Ruinemans-Koerts, J.; Jansen, A.P.H.; Kleerebezem, M.; Savelkoul, H.F.J. Strain-specific immunomodulatory effects of Lactobacillus plantarum strains on birch-pollen-allergic subjects out of season. Clin. Exp. Allergy 2010, 41, 232–242. [Google Scholar] [CrossRef]
- Fuc, E.; Złotkowska, D.; Stachurska, E.; Wróblewska, B. Immunoreactive properties of alfa-casein and kappa-casein: Ex vivo and in vivo studies. J. Dairy Sci. 2018, 101, 10703–10713. [Google Scholar] [CrossRef]
- Fotschki, J.; Szyc, A.; Wróblewska, B. Immunoreactivity of lactic acid-treated mare’s milk after simulated digestion. J. Dairy Res. 2015, 82, 78–85. [Google Scholar] [CrossRef]
- Van Gramberg, J.L.; de Veer, M.J.; O’Hehir, R.E.; Meeusen, E.N.; Bischof, R.J. Use of animal models to investigate major allergens associated with food allergy. J. Allergy 2013, 635695. [Google Scholar] [CrossRef]
- Scott-Taylor, T.H.; Hourihane, J.; Strobel, S. Correlation of allergen-specific IgG subclass antibodies and T lymphocyte cytokine responses in children with multiple food allergies. Pediatr. Allergy Immunol. 2010, 21, 935–944. [Google Scholar] [CrossRef]
- Schulke, S.; Albrecht, M. Mouse models for food allergies: Where do we stand? Cells 2019, 8, 546. [Google Scholar] [CrossRef] [PubMed]
- Hanane, N.; Hanane, K.; Omar, K.; Djamel, S. A model of intestinal anaphylaxis in whey sensitized Balb/c mice. Am. J. Immunol. 2009, 5, 56–60. [Google Scholar] [CrossRef]
- Escribese, M.M.; Rosace, D.; Chivato, T.; Fernández, T.D.; Corbí, A.L.; Barber, D. Alternative anaphylactic routes: The potential role of macrophages. Front. Immunol. 2017, 8, 515. [Google Scholar] [CrossRef]
- Shek, L.P.C.; Soderstrom, L.; Ahlstedt, S.; Beyer, K.; Sampson, H.A. Determination of food specific IgE levels over time can predict the development of tolerance in cow’s milk and hen’s egg allergy. J. Allergy Clin. Immunol. 2004, 114, 387–391. [Google Scholar] [CrossRef]
- Dodev, T.S.; Bowen, H.; Shamji, M.H.; Bax, H.J.; Beavil, A.J.; McDonnell, J.M.; Durham, S.R.; Sutton, B.J.; Gould, H.J.; James, L.K. Inhibition of allergen-dependent IgE activity by antibodies of the same specificity but different class. Allergy 2015, 70, 720–724. [Google Scholar] [CrossRef]
- Fernandez, M.I.; Pedron, T.; Tournebize, R.; Olivo-Marin, J.C.; Sansonetti, P.J.; Phalipon, A. Anti-inflammatory role for intracellular dimeric immunoglobulin A by neutralization of lipopolysaccharide in epithelial cells. Immunity 2003, 18, 739–749. [Google Scholar] [CrossRef]
- Frossard, C.P.; Hauser, C.; Eigenmann, P.A. Antigen-specific secretory IgA antibodies in the gut are decreased in a mouse model allergy. J. Allergy Clin. Immunol. 2004, 114, 377–382. [Google Scholar] [CrossRef]
- Weiberg, D.; Basic, M.; Smoczek, M.; Bode, U.; Bornemann, M.; Buettner, M. Participation of the spleen in the IgA immune response in the gut. PLoS ONE 2018, 13, e0205247. [Google Scholar] [CrossRef]
- Faria, A.M.C.; Weiner, H.L. Oral tolerance. Immunol. Rev. 2005, 206, 232–259. [Google Scholar] [CrossRef]
- Sierra, S.; Lara-Villoslada, F.; Sempere, L.; Olivares, M.; Boza, J.; Xaus, J. Intestinal and immunological effects of daily oral administration of Lactobacillus salivarius CECT5713 to healthy adults. Anaerobe 2010, 16, 195–200. [Google Scholar] [CrossRef]
- Akdis, C.A.; Akdis, M. Mechanisms of immune tolerance to allergens: Role of IL-10 and Tregs. J. Clin. Investig. 2014, 124, 4678–4680. [Google Scholar] [CrossRef]
- Yu, W.; Freeland, D.M.; Nadeau, K.C. Food allergy: Immune mechanisms, diagnosis and immunotherapy. Nat. Rev. Immunol. 2016, 16, 751–776. [Google Scholar] [CrossRef]
- Mauri, C.; Ehrenstein, M.R. The ‘short’ history of regulatory B cells. Trends Immunol. 2008, 29, 34–40. [Google Scholar] [CrossRef]
- Yamazaki, S.; Dudziak, D.; Heidkamp, G.F.; Fiorese, C.; Bonito, A.J.; Inaba, K.; Nussenzweig, M.C.; Steinman, R.M. CD8+CD205+ splenic dendritic cells are specialized to induce Foxp3+ regulatory T cells. J. Immunol. 2008, 181, 6923–6933. [Google Scholar] [CrossRef]
- Dong, P.; Yang, Y.; Wang, W. The role of intestinal bifidobacteria on immune system development in young rats. Early Hum. Dev. 2010, 86, 51–58. [Google Scholar] [CrossRef]
- de Roock, S.; van Elk, M.; van Dijk, M.E.A.; Timmerman, H.M.; Rijkers, G.T.; Prakken, B.J.; Hoekstra, M.O.; de Kleer, I.M. Lactic acid bacteria differ in their ability to induce functional regulatory T cells in humans. Clin. Exp. Allergy 2009, 40, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.; Inman, M.D.; Rooijen, N.; Yang, P.; Shen, H.; Matsumoto, K.; O’Byrne, P.M. Th type-1-stimulating activity of lung macrophages inhibits Th2-mediated allergic airways inflammation by an IFN-gamma-dependent mechanism. J. Immunol. 2001, 166, 1471–1481. [Google Scholar] [CrossRef]
- Gonzales-van Horn, S.R.; Farrar, J.D. Interferon at the crossroads of allergy and viral infections. J. Leukoc. Biol. 2015, 98, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Perrier, C.; Thierry, A.C.; Mercenier, A.; Corthsy, B. Allergen-specific antibody and cytokine responses, mast cell reactivity and intestinal permeability upon oral challenge of sensitized and tolerized mice. Clin. Exp. Allergy 2009, 40, 153–162. [Google Scholar] [CrossRef]
- Enomoto, M.; Noguchi, S.; Hattori, M.; Sugiyama, H.; Suzuki, Y.; Hanaoka, A.; Okada, S.; Yoshida, T. Oral administration of Lactobacillus plantarum NRIC0380 suppresses IgE production and induces CD4+CD25+Foxp3+ cells in vivo. Biosci. Biotechnol. Biochem. 2009, 73, 457–460. [Google Scholar] [CrossRef]
- Schabussova, I.; Hufnagl, K.; Wild, C.; Nutten, S.; Zuercher, A.W.; Mercenier, A.; Wiedermann, U. Distinctive anti-allergy properties of two probiotic bacterial strains in a mouse model of allergic poly-sensitization. Vaccine 2011, 29, 1981–1990. [Google Scholar] [CrossRef]
- Mazmanian, S.K.; Liu, C.H.; Tzianabos, A.O.; Kasper, D.L. An immunomodulatory molecule of symbiotic bacteria directs maturation of the host immune system. Cell 2005, 122, 107–118. [Google Scholar] [CrossRef]
- Smith, P.M.; Howitt, M.R.; Panikov, N.; Michaud, M.; Gallini, C.A.; Bohlooly-Y, M.; Glickman, J.N.; Garret, W.S. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 2013, 341, 569–573. [Google Scholar] [CrossRef] [PubMed]
- Ly, N.P.; Ruiz-Perez, B.; Onderdonk, A.B.; Tzianabos, A.O.; Litonjua, A.A.; Liang, C.; Laskey, D.; DuBois, A.M.; Levy, H.; Gold, D.R.; et al. Mode of delivery and cord blood cytokines: A birth cohort study. Clin. Mol. Allergy 2006, 4, 13. [Google Scholar] [CrossRef]
| Basic Starter | Added Bacteria | Strain Composition | Set Name |
|---|---|---|---|
| TKM3 + DB3 | none (alone) | S. thermophilus TKM3, L. bulgaricus DB3 | TKM3 + DB3 |
| +IB | S. thermophilus TKM3, L. bulgaricus DB3, L. plantarum IB | TKM3 + DB3 + IB | |
| +W42 | S. thermophilus TKM3, L. bulgaricus DB3, L. plantarum W42 | TKM3 + DB3 + W42 | |
| +Bi30 | S. thermophilus TKM3, L. bulgaricus DB3, B. lactis Bi30 | TKM3 + DB3 + Bi30 | |
| +J38 | S. thermophilus TKM3, L. bulgaricus DB3, B. lactis J38 | TKM3 + DB3 + J38 | |
| +Bi30 + IB | S. thermophilus TKM3, L. bulgaricus DB3, B. lactis Bi30, L. plantarum IB | TKM3 + DB3 + Bi30 + IB | |
| +Bi30 + W42 | S. thermophilus TKM3, L. bulgaricus DB3, B. lactis Bi30, L. plantarum W42 | TKM3 + DB3 + Bi30 + W42 | |
| +J38 + IB | S. thermophilus TKM3, L. bulgaricus DB3, B. lactis J38, L. plantarum IB | TKM3 + DB3 + J38 + IB | |
| +J38 + W42 | S. thermophilus TKM3, L. bulgaricus DB3, B. lactis J38, L. plantarum W42 | TKM3 + DB3 + J38 + W42 | |
| MK10 + 151 | none (alone) | S. thermophilus MK-10, L. bulgaricus 151 | MK10 + 151 |
| +IB | S. thermophilus MK-10, L. bulgaricus 151, L. plantarum IB | MK10 + 151 + IB | |
| +W42 | S. thermophilus MK-10, L. bulgaricus 151, L. plantarum W42 | MK10 + 151 + W42 | |
| +Bi30 | S. thermophilus MK-10, L. bulgaricus 151, B. lactis Bi30 | MK10 + 151 + Bi30 | |
| +J38 | S. thermophilus MK-10, L. bulgaricus 151, B. lactis J38 | MK10 + 151 + J38 | |
| +Bi30 + IB | S. thermophilus MK-10, L. bulgaricus 151, B. lactis Bi30, L. plantarum IB | MK10 + 151 + Bi30 + IB | |
| +Bi30 + W42 | S. thermophilus MK-10, L. bulgaricus 151, B. lactis Bi30, L. plantarum W42 | MK10 + 151 + Bi30 + W42 | |
| +J38 + IB | S. thermophilus MK-10, L. bulgaricus 151, B. lactis J38, L. plantarum IB | MK10 + 151 + J38 + IB | |
| +J38 + W42 | S. thermophilus MK-10, L. bulgaricus 151, B. lactis J38, L. plantarum W42 | MK10 + 151 + J38 + W42 | |
| 2K + BK | none (alone) | S. thermophilus 2K, L. bulgaricus BK | 2K + BK 1 |
| +IB | S. thermophilus 2K, L. bulgaricus BK, L. plantarum IB | 2K + BK + IB | |
| +W42 | S. thermophilus 2K, L. bulgaricus BK, L. plantarum W42 | 2K + BK + W42 | |
| +Bi30 | S. thermophilus 2K, L. bulgaricus BK, B. lactis Bi30 | 2K + BK + Bi30 | |
| +J38 | S. thermophilus 2K, L. bulgaricus BK, B. lactis J38 | 2K + BK + J38 | |
| +Bi30 + IB | S. thermophilus 2K, L. bulgaricus BK, B. lactis Bi30, L. plantarum IB | 2K + BK + Bi30 + IB | |
| +Bi30 + W42 | S. thermophilus 2K, L. bulgaricus BK, B. lactis Bi30, L. plantarum W42 | 2K + BK + Bi30 + W42 2 | |
| +J38 + IB | S. thermophilus 2K, L. bulgaricus BK, B. lactis J38, L. plantarum IB | 2K + BK + J38 + IB | |
| +J38 + W42 | S. thermophilus 2K, L. bulgaricus BK, B. lactis J38, L. plantarum W42 | 2K + BK + J38 + W42 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wróblewska, B.; Kaliszewska-Suchodoła, A.; Fuc, E.; Markiewicz, L.H.; Ogrodowczyk, A.M.; Złotkowska, D.; Wasilewska, E. Effect of Low-Immunogenic Yogurt Drinks and Probiotic Bacteria on Immunoreactivity of Cow’s Milk Proteins and Tolerance Induction—In Vitro and In Vivo Studies. Nutrients 2020, 12, 3390. https://doi.org/10.3390/nu12113390
Wróblewska B, Kaliszewska-Suchodoła A, Fuc E, Markiewicz LH, Ogrodowczyk AM, Złotkowska D, Wasilewska E. Effect of Low-Immunogenic Yogurt Drinks and Probiotic Bacteria on Immunoreactivity of Cow’s Milk Proteins and Tolerance Induction—In Vitro and In Vivo Studies. Nutrients. 2020; 12(11):3390. https://doi.org/10.3390/nu12113390
Chicago/Turabian StyleWróblewska, Barbara, Anna Kaliszewska-Suchodoła, Ewa Fuc, Lidia Hanna Markiewicz, Anna Maria Ogrodowczyk, Dagmara Złotkowska, and Ewa Wasilewska. 2020. "Effect of Low-Immunogenic Yogurt Drinks and Probiotic Bacteria on Immunoreactivity of Cow’s Milk Proteins and Tolerance Induction—In Vitro and In Vivo Studies" Nutrients 12, no. 11: 3390. https://doi.org/10.3390/nu12113390
APA StyleWróblewska, B., Kaliszewska-Suchodoła, A., Fuc, E., Markiewicz, L. H., Ogrodowczyk, A. M., Złotkowska, D., & Wasilewska, E. (2020). Effect of Low-Immunogenic Yogurt Drinks and Probiotic Bacteria on Immunoreactivity of Cow’s Milk Proteins and Tolerance Induction—In Vitro and In Vivo Studies. Nutrients, 12(11), 3390. https://doi.org/10.3390/nu12113390






