Predicted Skeletal Muscle Mass and 4-Year Cardiovascular Disease Incidence in Middle-Aged and Elderly Participants of IKARIA Prospective Epidemiological Study: The Mediating Effect of Sex and Cardiometabolic Factors
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Bioethics
2.3. SMI Calculation
2.4. Other Baseline Measurements
2.5. Endpoint and Follow-up Evaluation
2.6. Statistical Analysis
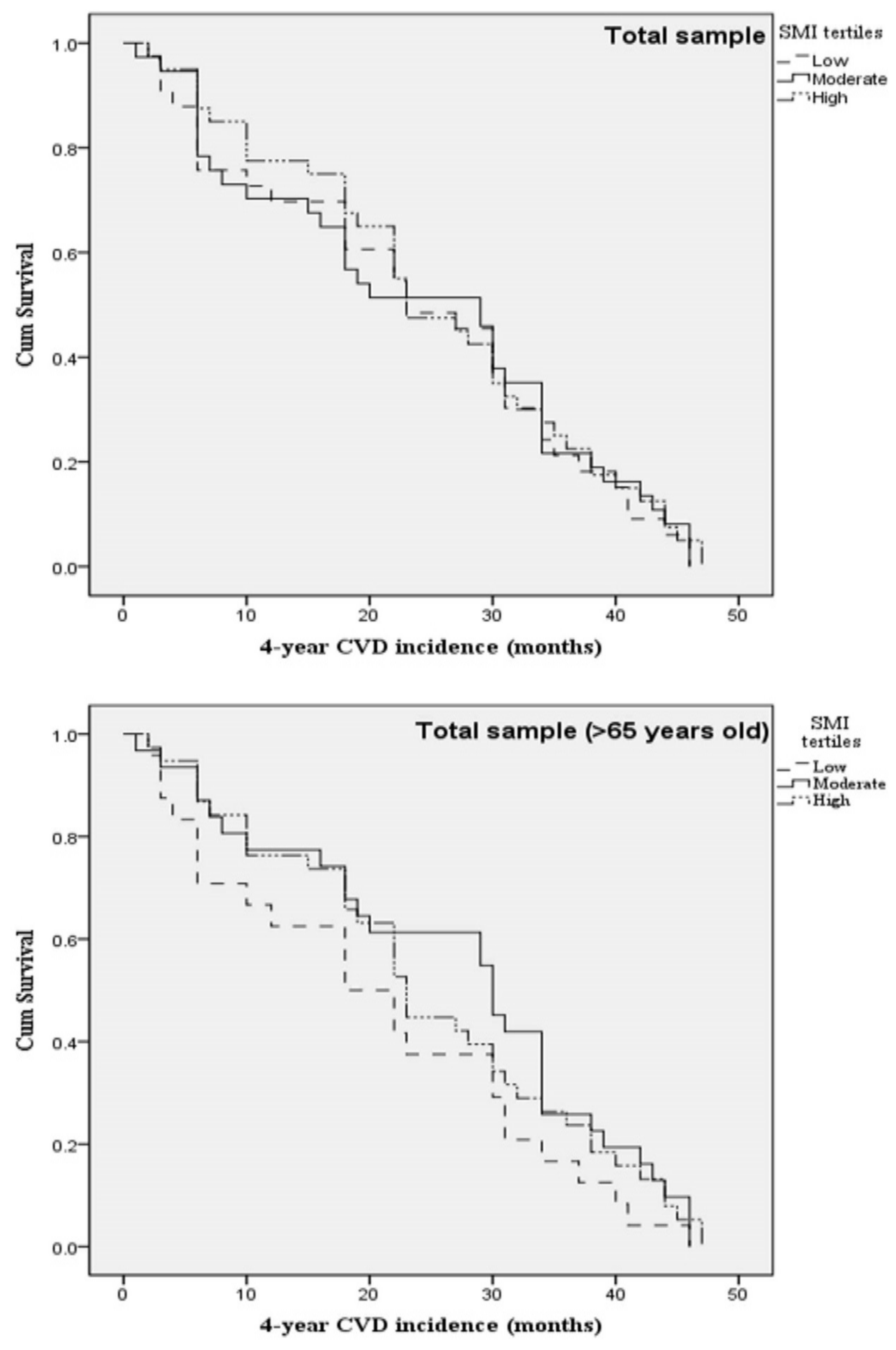
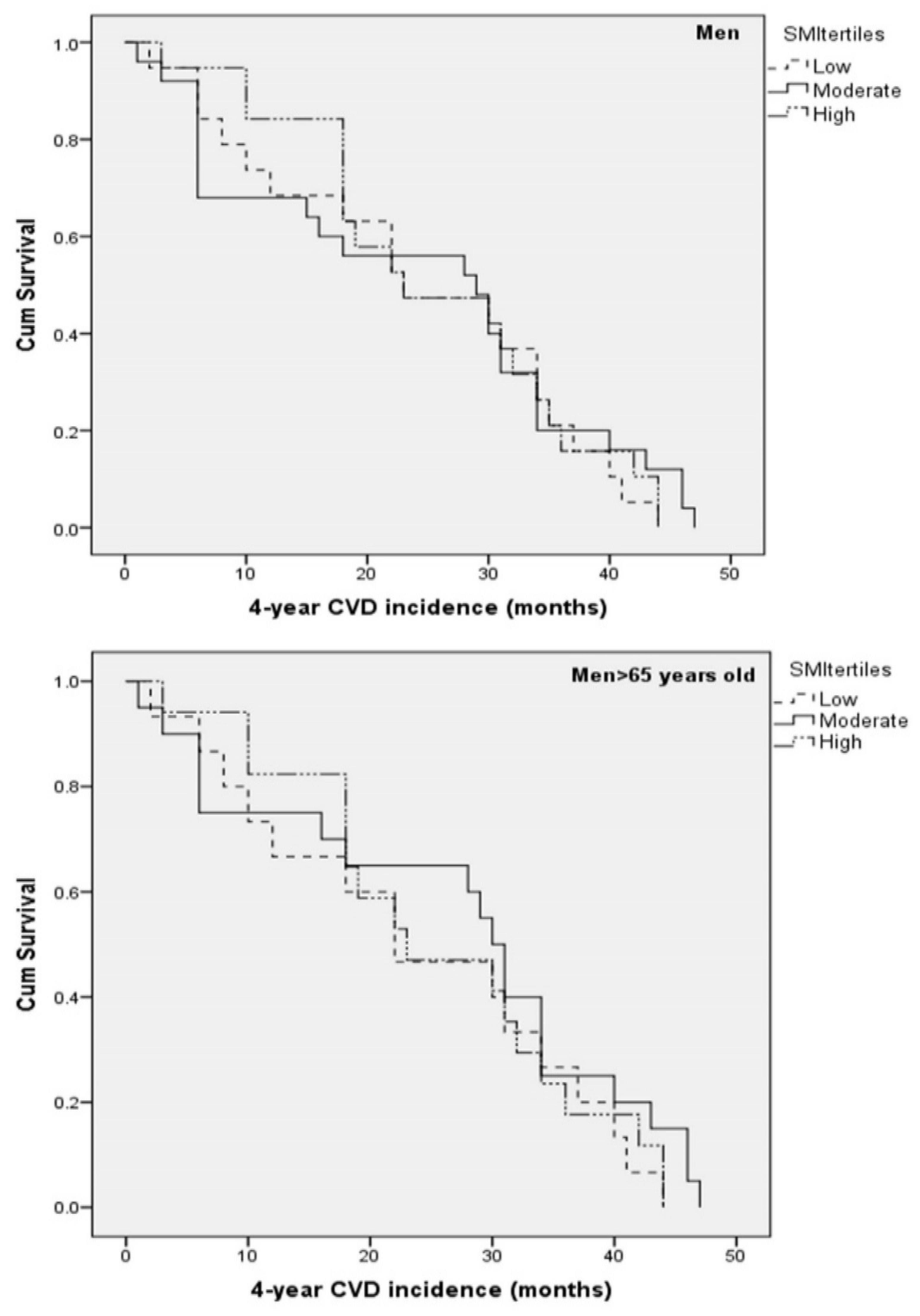
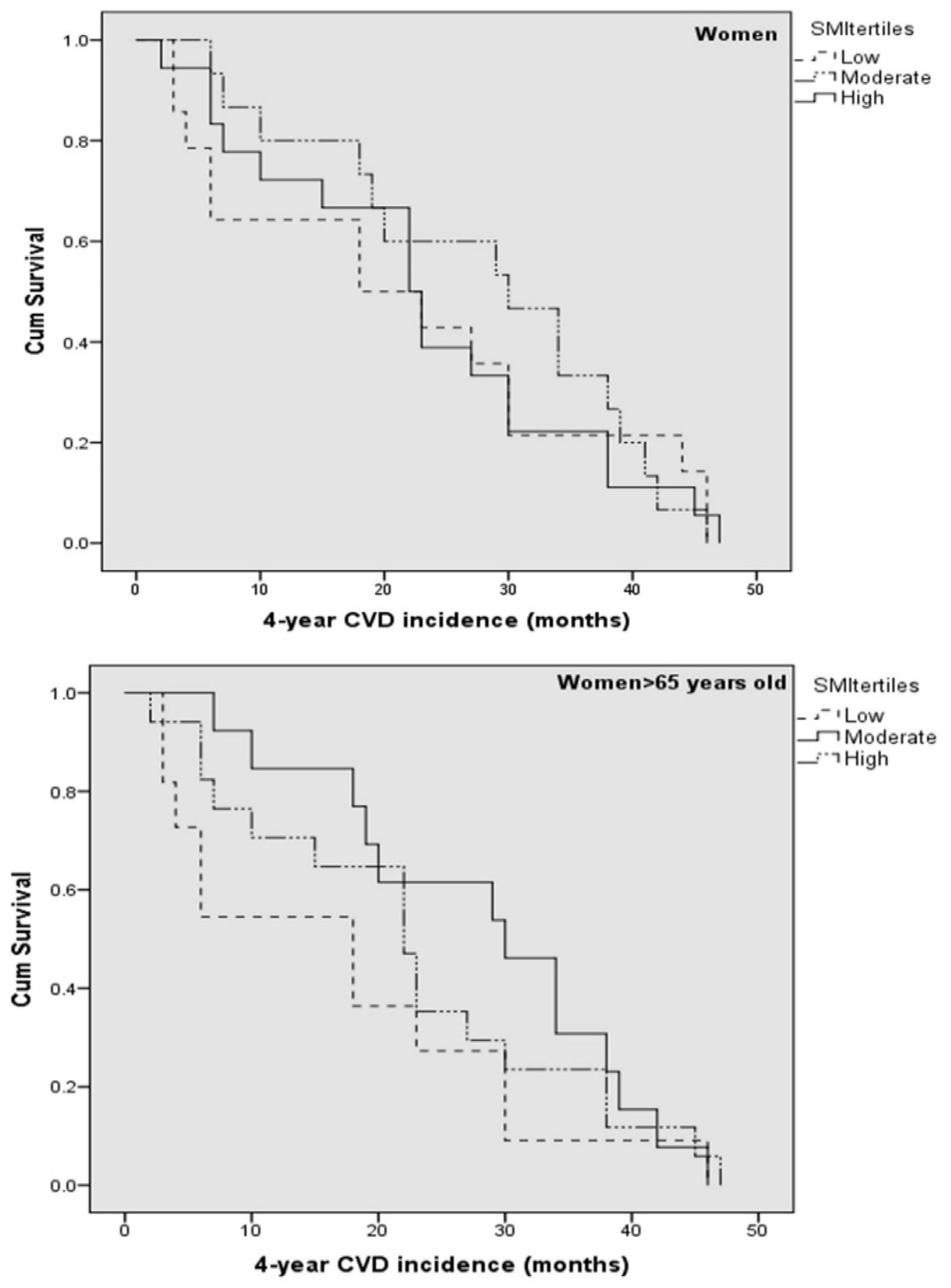
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- De Carvalho, F.G.; Justice, J.N.; Freitas, E.C.; Kershaw, E.E.; Sparks, L.M. Adipose Tissue Quality in Aging: How Structural and Functional Aspects of Adipose Tissue Impact Skeletal Muscle Quality. Nutrients 2019, 11, 2553. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Laddu, D.; Arena, R.; Ortega, F.B.; Alpert, M.A.; Kushner, R.F. Healthy Weightand Obesity Prevention: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1506–1531. [Google Scholar] [CrossRef] [PubMed]
- Srikanthan, P.; Horwich, T.B.; Tseng, C.H. Relation of Muscle Mass and Fat Mass toCardiovascular Disease Mortality. Am. J. Cardiol. 2016, 117, 1355–1360. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.P.; Teo, K.K.; Rangarajan, S.; Lopez-Jaramillo, P.; Avezum, A., Jr.; Orlandini, A.; Seron, P.; Ahmed, S.H.; Rosengren, A.; Kelishadi, R.; et al. Prognostic value of grip strength: Findings from the ProspectiveUrban Rural Epidemiology (PURE) study. Lancet 2015, 386, 266–273. [Google Scholar] [CrossRef]
- Kim, Y.; Han, B.D.; Han, K.; Shin, K.E.; Lee, H.; Kim, T.R.; Cho, K.H.; Kim, D.H.; Kim, Y.H.; Kim, H.; et al. Optimal cutoffs for low skeletal muscle mass related to cardiovascularrisk in adults: The Korea National Health and Nutrition Examination Survey 2009–2010. Endocrine 2015, 50, 424–433. [Google Scholar] [CrossRef]
- Batsis, J.A.; Mackenzie, T.A.; Jones, J.D.; Lopez-Jimenez, F.; Bartels, S.J. Sarcopenia, sarcopenic obesity and inflammation: Results from the 1999-2004 National Healthand Nutrition Examination Survey. Clin. Nutr. 2016, 35, 1472–1483. [Google Scholar] [CrossRef]
- Cleasby, M.E.; Jamieson, P.M.; Atherton, P.J. Insulin resistance and sarcopenia:mechanistic links between common co-morbidities. J. Endocrinol. 2016, 229, R67–R81. [Google Scholar] [CrossRef]
- Im, I.J.; Choi, H.J.; Jeong, S.M.; Kim, H.J.; Son, J.S.; Oh, H.J. The association betweenmuscle mass deficits and arterial stiffness in middle-aged men. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 1130–1135. [Google Scholar] [CrossRef]
- Springer, J.; Springer, J.I.; Anker, S.D. Muscle wasting and sarcopenia in heartfailure and beyond: Update 2017. ESC Heart Fail. 2017, 4, 492–498. [Google Scholar] [CrossRef]
- Kouvari, M.; Yannakoulia, M.; Souliotis, K.; Panagiotakos, D.B. Challenges in Sex-andGender-Centered Prevention and Management of Cardiovascular Disease: Implicationsof Genetic, Metabolic, and Environmental Paths. Angiology 2018, 69, 843–853. [Google Scholar] [CrossRef]
- Chrysohoou, C.; Skoumas, J.; Pitsavos, C.; Masoura, C.; Siasos, G.; Galiatsatos, N.; Psaltopoulou, T.; Mylonakis, C.; Margazas, A.; Kyvelou, S.; et al. Long-term adherence to the Mediterranean diet reduces the prevalence of hyperuricaemia in elderly individuals, without known cardiovascular disease: The Ikaria study. Maturitas 2011, 70, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.C.; Wang, Z.; Heo, M.; Ross, R.; Janssen, I.; Heymsfield, S.B. Total-body skeletal muscle mass: Development and cross-validation of anthropometric prediction models. Am. J. Clin. Nutr. 2000, 72, 796–803. [Google Scholar] [CrossRef]
- Stefanadis, C.; Stratos, C.; Boudoulas, H.; Kourouklis, C.; Toutouzas, P. Distensibility of the ascending aorta: Comparison of invasive and non-invasive techniques in healthy men and in men with coronary artery disease. Eur. Heart J. 1990, 11, 990–996. [Google Scholar] [CrossRef]
- Wang, S.; Ren, J. Obesity Paradox in Aging: From Prevalence to Pathophysiology. Prog. Cardiovasc. Dis. 2018, 61, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Kastorini, C.M.; Panagiotakos, D.B. The obesity paradox: Methodological considerations based on epidemiological and clinical evidence—New insights. Maturitas 2012, 72, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Kouvari, M.; Panagiotakos, D.B.; Chrysohoou, C.; Notara, V.; Georgousopoulou, E.N.; Yannakoulia, M.; Tousoulis, D.; Pitsavos, C.; ATTICA and GREECS study Investigators. A sex-specific evaluation of predicted lean and fat mass composition andcardiovascular disease onset and progression: A combined analysis of the ATTICAand GREECS prospective epidemiological studies. Obes. Res. Clin. Pract. 2019, 13, 469–477. [Google Scholar] [CrossRef]
- Kouvari, M.; Chrysohoou, C.; Dilaveris, P.; Georgiopoulos, G.; Magkas, N.; Aggelopoulos, P.; Panagiotakos, D.B.; Tousoulis, D. Skeletal muscle mass in acute coronary syndrome prognosis: Gender-based analysis from Hellenic Heart Failure cohort. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Medina-Inojosa, J.R.; Somers, V.K.; Thomas, R.J.; Jean, N.; Jenkins, S.M.; Gomez-Ibarra, M.A.; Supervia, M.; Lopez-Jimenez, F. Association Between Adiposity and Lean Mass WithLong-Term Cardiovascular Events in Patients With Coronary Artery Disease: NoParadox. J. Am. Heart Assoc. 2018, 7, e007505. [Google Scholar] [CrossRef]
- Spahillari, A.; Mukamal, K.J.; DeFilippi, C.; Kizer, J.R.; Gottdiener, J.S.; Djoussé, L.; Lyles, M.F.; Bartz, T.M.; Murthy, V.L.; Shah, R.V. The association of lean and fat mass withall-cause mortality in older adults: The Cardiovascular Health Study. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 1039–1047. [Google Scholar] [CrossRef]
- Yang, L.; Smith, L.; Hamer, M. Gender-specific risk factors for incident sarcopenia: 8-year follow-up of the English longitudinal study of ageing. J. Epidemiol. Community Health 2019, 73, 86–88. [Google Scholar] [CrossRef]
- Keller, K.; Münzel, T.; Ostad, M.A. Sex-specific differences in mortality and theobesity paradox of patients with myocardial infarction ages >70 y. Nutrition 2018, 46, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Kouvari, M.; Chrysohoou, C.; Tsiamis, E.; Kosyfa, H.; Kalogirou, L.; Filippou, A.; Iosifidis, S.; Aggelopoulos, P.; Pitsavos, C.; Tousoulis, D. The "overweight paradox" inthe prognosis of acute coronary syndrome for patients with heart failure-A truth for all? A 10-year follow-up study. Maturitas 2017, 102, 6–12. [Google Scholar] [CrossRef] [PubMed]
- De Schutter, A.; Kachur, S.; Lavie, C.J.; Boddepalli, R.S.; Patel, D.A.; Milani, R.V. Theimpact of inflammation on the obesity paradox in coronary heart disease. Int. J. Obes. 2016, 40, 1730–1735. [Google Scholar] [CrossRef]
- Kalinkovich, A.; Livshits, G. Sarcopenic obesity or obese sarcopenia: A crosstalk between age-associated adipose tissue and skeletal muscle inflammation as a main mechanism of the pathogenesis. Ageing Res. Rev. 2017, 35, 200–221. [Google Scholar] [CrossRef]
- Di Iorio, A.; Di Blasio, A.; Napolitano, G.; Ripari, P.; Paganelli, R.; Cipollone, F. High fat mass, low muscle mass, and arterial stiffness in a population offree-living healthy subjects: The "al passo con la tua salute" project. Medicine 2019, 98, e16172. [Google Scholar] [CrossRef] [PubMed]
- Pietri, P.; Vlachopoulos, C.; Chrysohoou, C.; Lazaros, G.; Masoura, K.; Ioakeimidis, N.; Tousoulis, D.; Stefanadis, C. Deceleration of Age-Related Aortic Stiffening in a Population With High Longevity Rates: The IKARIA Study. J. Am. Coll. Cardiol. 2015, 66, 1842–1843. [Google Scholar] [CrossRef] [PubMed]
- Kloner, R.A.; Carson, C., 3rd; Dobs, A.; Kopecky, S.; Mohler, E.R., 3rd. Testosterone and Cardiovascular Disease. J. Am. Coll. Cardiol. 2016, 67, 545–557. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.M.; Ratcliffe, S.J.; Reilly, M.P.; Weinstein, R.; Bhasin, S.; Blackman, M.R.; Cauley, J.A.; Sutton-Tyrrell, K.; Robbins, J.; Fried, L.P.; et al. Higher serum testosterone concentration in older women is associated with insulin resistance, metabolicsyndrome, and cardiovascular disease. J. Clin. Endocrinol. Metab. 2009, 94, 4776–4784. [Google Scholar] [CrossRef]
| Baseline Characteristics | Skeletal Muscle Mass Index Tertiles | |||
|---|---|---|---|---|
| 1st Tertile | 2nd Tertile | 3rd Tertile | p-Value | |
| N | 371 | 374 | 396 | |
| Sociodemographic factors | ||||
| Age, years | 64 (12) | 64 (13) | 63 (14) | 0.22 |
| Male sex, % | 46 | 46 | 47 | 0.97 |
| Anthropometric factors | ||||
| Body mass index, kg/m2 | 23.9 (2.1) | 28.0 (1.5) | 33.6 (3.7) | <0.001 |
| Waist circumference, cm | 91 (11) | 101 (9) | 111 (11) | <0.001 |
| Waist-to-hip ratio | 0.91 (0.09) | 0.95 (0.09) | 0.97 (0.09) | <0.001 |
| Lifestyle factors | ||||
| Physical inactivity, % | 30 | 38 | 35 | 0.93 |
| MedDietScore, range 0–55 | 34.4 (0.6) | 34.5 (0.6) | 34.3 (0.6) | 0.04 |
| Weekly alcohol consumption, % | 61 | 62 | 63 | 0.81 |
| Current smoking, % | 23 | 30 | 38 | <0.001 |
| Clinical factors | ||||
| History of hypertension, % | 30 | 44 | 53 | <0.001 |
| History of diabetes mellitus, % | 22 | 17 | 85 | <0.001 |
| History of hypercholesterolemia, % | 33 | 36 | 44 | 0.00 |
| Metabolic syndrome, % | 16 | 39 | 55 | <0.001 |
| Family CVD history, % | 40 | 37 | 40 | 0.70 |
| Inflammation/coagulation markers | ||||
| Ultra-sensitive C-Reactive Protein, mg/L | 3.4 (3.9) | 1.8 (2.1) | 3.0 (3.2) | <0.001 |
| Interleukin 6, pg/dL | 3.8 (11.5) | 4.4 (13.0) | 4.7 (24.0) | 0.87 |
| Tumor necrosis factor-alpha, pg/mL | 1.51 (0.50) | 1.53 (0.50) | 1.62 (0.49) | 0.63 |
| White blood cells, 103 counts | 6.4 (1.6) | 5.9 (1.5) | 6.2 (1.4) | <0.001 |
| Aortic stiffness markers | ||||
| Aortic distensibility, 1000*mmHg−1 | 1.55 (1.47) | 1.70 (1.07) | 1.67 (1.46) | <0.001 |
| Pulmonary pressure, mmHg | 31 (6) | 31 (6) | 30 (6) | 0.02 |
| Liver function markers | ||||
| Alanine transaminase, U/L | 14.8 (6.8) | 15.9 (7.1) | 18.3 (10.4) | <0.001 |
| Aspartate transaminase, U/L | 22.7 (7.9) | 22.6 (11.4) | 22.0 (6.4) | 0.45 |
| Glucose/insulin homeostasis markers | ||||
| Fasting glucose, mg/dL | 96 (23) | 104 (31) | 107 (28) | <0.001 |
| HOMA-IR | 0.81 (0.67) | 1.04 (1.44) | 1.80 (3.04) | <0.001 |
| Lipid markers | ||||
| Total cholesterol, mg/dL | 205 (39) | 205 (40) | 204 (42) | 0.97 |
| High density lipoprotein cholesterol, mg/dL | 45 (10) | 46 (9) | 50 (13) | <0.001 |
| Triglycerides, mg/dL | 127 (85) | 147 (95) | 160 (91) | <0.001 |
| Low density lipoprotein cholesterol, mg/dL | 128 (34) | 129 (34) | 129 (33) | 0.89 |
| Hormones | ||||
| Total testosterone, ng/dL | 157 (19) | 177 (20) | 220 (242) | 0.05 |
| 4-year follow-up measurements | ||||
| First fatal/non-fatal cardiovascular disease incidence | 19.2 | 14.2 | 13.3 | 0.04 |
| First fatal/non-fatal cardiovascular disease incidence (excluding participants <65 years old) | 27.4 | 23.9 | 25.9 | 0.01 |
| Woman-to-man cardiovascular disease incidence ratio | 0.68 | 0.57 | 0.78 | 0.03 |
| Woman-to-man cardiovascular disease incidence ratio (excluding participants <65 years old) | 0.88 | 0.60 | 0.77 | 0.001 |
| Models | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | Model 9 |
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| SMI tertiles | |||||||||
| 1st | Ref | ref | ref | ref | Ref | ref | ref | ref | ref |
| 2nd | 0.76 (0.43, 0.91) | 0.82 (0.52, 0.91) | 0.85 (0.52, 0.93) | 0.86 (0.40, 0.93) | 0.87 (0.45, 0.99) | 0.92 (0.52, 1.08) | 1.28 (0.61, 2.65) | 1.01 (0.52, 1.92) | 1.09 (0.51, 2.32) |
| 3rd | 0.70 (0.36, 0.86) | 0.74 (0.43, 0.86) | 0.75 (0.45, 0.82) | 0.78 (0.48, 0.85) | 0.83 (0.37, 0.95) | 0.89 (0.41, 0.99) | 1.31 (0.55, 3.12) | 0.83 (0.37, 1.88) | 0.99 (0.39, 2.48) |
| Age, per 1 year | - | 1.04 (1.02, 1.06) | 1.04 (1.03, 1.06) | 1.06 (1.03, 1.08) | 1.04 (1.02, 1.06) | 1.07 (1.00, 1.13) | 1.06 (1.02, 1.10) | 1.04 (1.02, 1.07) | 1.05 (1.01, 1.10) |
| Male sex | - | 1.74 (1.16, 2.59) | 1.75 (1.15, 2.67) | 1.76 (1.13, 2.74) | 2.10 (1.22, 3.59) | 1.99 (0.91, 4.33) | 1.70 (1.91, 3.17) | 2.41 (1.40, 4.15) | 1.80 (0.65, 5.01) |
| Waist circumference, per 1 cm | - | - | 0.99 (0.97, 1.01) | 0.99 (0.97, 1.01) | 0.99 (0.97, 1.01) | 1.00 (0.95, 1.04) | 0.99 (0.96, 1.02) | 0.99 (0.96, 1.02) | 0.99 (0.96, 1.03) |
| Current smoking, y/n | - | - | - | 1.15 (0.69, 1.93) | 1.15 (0.69, 1.93) | 1.15 (0.69, 1.93) | 1.33 (0.63, 2.81) | 0.99 (0.53, 1.85) | 1.07 (0.48, 2.39) |
| Physical activity, y/n | - | - | - | 0.87 (0.65, 1.23) | 0.87 (0.65, 1.23) | 0.87 (0.65, 1.23) | 0.99 (0.71, 2.14) | 0.97 (0.73, 1.31) | 0.89 (0.68, 1.31) |
| MedDietScore, per 1 unit (0–55) | - | - | - | 0.96 (0.94, 1.02) | 0.96 (0.94, 1.02) | 0.96 (0.94, 1.02) | 0.99 (0.96, 1.05) | 0.97 (0.94, 1.02) | 0.96 (0.94, 1.02) |
| Diabetes mellitus, y/n | - | - | - | - | 1.81 (0.93, 3.52) | 2.12 (0.84, 5.33) | 1.55 (0.78, 3.07) | 1.71 (0.32, 3.18) | 1.44 (0.69, 3.01) |
| Hypertension, y/n | - | - | - | - | 1.31 (0.75, 2.29) | 1.34 (0.51, 3.17) | 1.01 (0.53, 1.92) | 1.41 (0.81, 2.47) | 1.34 (0.67, 2.68) |
| Family history of CVD, y/n | - | - | - | - | 1.55 (0.61, 1.79) | 1.57 (0.72, 3.45) | 1.34 (0.74, 2.42) | 1.01 (0.60, 1.70) | 1.19 (0.64, 2.21) |
| HDL-C, per 1 mg/dL | - | - | - | - | 0.97 (0.95, 1.01) | 1.03 (0.95, 1.05) | 1.03 (0.96, 1.06) | 1.02 (0.99, 1.04) | 1.02 (0.99, 1.06) |
| TGL, per 1 mg/dL | - | - | - | - | 0.99 (0.98, 1.01) | 1.01 (0.99, 1.02) | 1.01 (0.99, 1.02) | 1.00 (0.99, 1.01) | 1.01 (0.99, 1.02) |
| HOMA-IR, per 1 unit | - | - | - | - | - | 1.12 (1.02, 1.22) | - | - | - |
| usCRP, per 1 mg/L | - | - | - | - | - | 1.04 (1.02, 1.11) | - | - | |
| White blood cells, per 1 count | - | - | - | - | - | - | 1.20 (1.01, 1.48) | - | - |
| Arterial distensibility, per 1000 mmHg−1 | - | - | - | - | - | - | - | 0.90 (0.74, 0.96) | - |
| Total testosterone, per 1 ng/dL | - | - | - | - | - | - | - | - | 0.99 (0.97, 1.01) |
| Models | Standard Model | Standard Model Plus HOMA-IR | Standard Model Plus usCRP and WBC | Standard Model Plus Arterial Distensibility | Standard Model Plus Total Testosterone |
|---|---|---|---|---|---|
| HR (95%CI) | HR (95%CI) | HR (95%CI) | HR (95%CI) | HR (95%CI) | |
| Total sample excluding participants with age <65 years | |||||
| 2nd vs. 1st SMI tertile | 0.80 (0.45, 0.96) | 0.95 (0.36, 1.31) | 1.03 (0.59, 1.56) | 0.92 (0.45, 1.38) | 1.07 (0.52, 1.42) |
| 3rd vs. 1st SMI tertile | 1.20 (0.61, 2.35) | 1.15 (0.53, 2.53) | 1.29 (0.55, 3.06) | 1.33 (0.53, 3.38) | 1.13 (0.42, 2.71) |
| p for age interaction = 0.003 | |||||
| Men | |||||
| 2nd vs. 1st SMI tertile | 0.87 (0.56, 1.85) | 0.94 (0.30, 1.93) | 0.87 (0.30, 2.54) | 1.04 (0.43, 2.15) | 0.88 (0.29, 2.62) |
| 3rd vs. 1st SMI tertile | 0.64 (0.36, 0.99) | 0.74 (0.41, 0.98) | 0.58 (0.13, 0.89) | 0.84 (0.54, 1.42) | 0.59 (0.25, 1.55) |
| Women | |||||
| 2nd vs. 1st SMI tertile | 0.71 (0.33, 0.95) | 1.10 (0.34, 1.99) | 1.12 (0.36, 3.45) | 0.75 (0.19, 1.71) | 0.79 (0.40, 0.99) |
| 3rd vs. 1st SMI tertile | 1.42 (0.50, 4.03) | 1.10 (0.23, 4.31) | 1.91 (0.51, 4.66) | 1.52 (0.47, 4.91) | 1.89 (0.46, 4.76) |
| p for gender interaction = 0.01 | |||||
| Men excluding participants with age < 65 years | |||||
| 2nd vs. 1st SMI tertile | 0.92 (0.40, 1.07) | 1.03 (0.22, 1.89) | 1.21 (0.40, 3.71) | 1.19 (0.38, 3.80) | 0.99 (0.29, 1.35) |
| 3rd vs. 1st SMI tertile | 0.69 (0.51, 1.10) | 0.73 (0.65, 1.19) | 0.74 (0.46, 1.21) | 0.70 (0.51, 1.09) | 0.75 (0.42, 1.16) |
| Women excluding participants with age < 65 years | |||||
| 2nd vs. 1st SMI tertile | 0.59 (0.19, 0.89) | 0.58 (0.14, 0.86) | 0.89 (0.36, 1.50) | 0.63 (0.17, 1.09) | 0.53 (0.14, 1.05) |
| 3rd vs. 1st SMI tertile | 1.15 (0.45, 3.93) | 1.29 (0.67, 4.01) | 1.33 (0.68, 3.20) | 1.36 (0.46, 3.98) | 0.91 (0.30, 2.17) |
| p for gender and age interaction = 0.004 | |||||
| Total Sample | |||
|---|---|---|---|
| Total | Men | Women | |
| N | 1141 | 529 | 612 |
| Beta-Coefficient (standard error) | Beta-Coefficient (standard error) | Beta-Coefficient (standard error) | |
| usCRP, per 1 mg/L | −0.22 (0.13) | −0.27 (0.13) | −0.31 (0.13) |
| Interleukin 6, per 1 pg/dL | +0.11 (0.21) | −0.10 (0.19) | −0.12 (0.20) |
| Tumor necrosis factor-alpha, per 1 pg/mL | +0.19 (1.18) | −0.17 (1.68) | −0.18 (0.91) |
| White blood cells, per 103 counts | −0.32 (0.09) | −0.19 (0.11) | −0.25 (0.12) |
| HOMA-IR, per 1 unit | −0.67 (0.21) | −0.54 (0.71) | −0.81 (0.24) |
| Arterial distensibility, per 1000 mmHg−1 | −0.40 (0.89) | −0.61 (0.90) | −0.33 (0.77) |
| Total testosterone, per 1 ng/dL | +0.19 (0.11) | +0.27 (0.16) | +0.08 (0.10) |
| Total sample excluding participants <65 years old | |||
| Total | Men | Women | |
| N | 670 | 327 | 343 |
| usCRP, per 1 mg/L | −0.21 (0.12) | −0.15 (0.11) | −0.38 (0.15) |
| Interleukin 6, per 1 pg/dL | +0.12 (0.22) | −0.09 (0.17) | −0.13 (0.21) |
| Tumor necrosis factor-alpha, per 1 pg/mL | +0.20 (1.17) | −0.14 (1.60) | −0.17 (0.90) |
| White blood cells, per 103 counts | −0.19 (0.25) | −0.18 (0.15) | −0.26 (0.16) |
| HOMA-IR, per 1 unit | −0.25 (0.24) | −0.25 (0.60) | −0.29 (0.27) |
| Arterial distensibility, per 1000 mmHg−1 | −0.51 (0.92) | −0.64 (0.87) | −0.45 (0.82) |
| Total testosterone, per 1 ng/dL | +0.23 (0.12) | +0.14 (0.13) | +0.19 (0.11) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chrysohoou, C.; Kouvari, M.; Lazaros, G.; Varlas, J.; Dimitriadis, K.; Zaromytidou, M.; Masoura, C.; Skoumas, J.; Kambaxis, M.; Galiatsatos, N.; et al. Predicted Skeletal Muscle Mass and 4-Year Cardiovascular Disease Incidence in Middle-Aged and Elderly Participants of IKARIA Prospective Epidemiological Study: The Mediating Effect of Sex and Cardiometabolic Factors. Nutrients 2020, 12, 3293. https://doi.org/10.3390/nu12113293
Chrysohoou C, Kouvari M, Lazaros G, Varlas J, Dimitriadis K, Zaromytidou M, Masoura C, Skoumas J, Kambaxis M, Galiatsatos N, et al. Predicted Skeletal Muscle Mass and 4-Year Cardiovascular Disease Incidence in Middle-Aged and Elderly Participants of IKARIA Prospective Epidemiological Study: The Mediating Effect of Sex and Cardiometabolic Factors. Nutrients. 2020; 12(11):3293. https://doi.org/10.3390/nu12113293
Chicago/Turabian StyleChrysohoou, Christina, Matina Kouvari, George Lazaros, John Varlas, Kyriakos Dimitriadis, Marina Zaromytidou, Constantina Masoura, John Skoumas, Manolis Kambaxis, Nikos Galiatsatos, and et al. 2020. "Predicted Skeletal Muscle Mass and 4-Year Cardiovascular Disease Incidence in Middle-Aged and Elderly Participants of IKARIA Prospective Epidemiological Study: The Mediating Effect of Sex and Cardiometabolic Factors" Nutrients 12, no. 11: 3293. https://doi.org/10.3390/nu12113293
APA StyleChrysohoou, C., Kouvari, M., Lazaros, G., Varlas, J., Dimitriadis, K., Zaromytidou, M., Masoura, C., Skoumas, J., Kambaxis, M., Galiatsatos, N., Papanikolaou, A., Xydis, P., Konstantinou, K., Pitsavos, C., Tsioufis, K., & Stefanadis, C. (2020). Predicted Skeletal Muscle Mass and 4-Year Cardiovascular Disease Incidence in Middle-Aged and Elderly Participants of IKARIA Prospective Epidemiological Study: The Mediating Effect of Sex and Cardiometabolic Factors. Nutrients, 12(11), 3293. https://doi.org/10.3390/nu12113293






