Abstract
While human milk composition is characterised by marked dynamicity, we are far from having a clear picture of what factors drive this variation. Hormones in human milk are known to vary according to specific maternal phenotypes, but limited evidence shows the infant also has a role in determining milk composition. The present study aimed to investigate the interplay between maternal and infant characteristics in relation to human milk hormonal profile. In total, 501 human milk samples from mothers recruited in the Finnish STEPS cohort study (Steps to the healthy development) were analysed. Pre-pregnancy and pregnancy maternal data, socioeconomic status and infant characteristics at birth were collated. Leptin, adiponectin, insulin-like growth factor-1 and cyclic Glycine-Proline in milk were measured. Multivariate analysis of variance (MANOVA) and linear regression were utilised for statistical analysis. Sex-specific interactions with maternal factors were observed, as the infant sex mediated associations between gestational diabetes and milk adiponectin (p = 0.031), birth-mode and total protein (p = 0.003), maternal education and insulin-like growth factor-1: cyclic Glycine-Proline ratio (p = 0.035). Our results suggest that changes in human milk composition are associated with interactions between maternal and infant characteristics and pathophysiological factors. Future work should expand on these findings and further explore the link between hormonal profiles in human milk and infant outcomes.
1. Introduction
Biologically active compounds in human milk (HM) include different classes of hormones, such as growth [1] and satiety factors [2], that play important roles in human physiology and metabolism mediating energy intake [3] and somatic growth [4]. Extensive evidence from animal models has shown that these compounds are likely to be active in HM and, once ingested by the infant, exert a range of physiological functions [5]. Changes in HM nutritional and hormonal composition have been well documented throughout the sequential stages of lactation [6,7], per feed [8], per day [9], across mothers with different phenotypic characteristics [10,11], socioeconomic status [12] and infants of different sex [13]. Limited studies to date [11,14,15,16,17] have reported alterations in the HM bioactive, amino and fatty acid profiles of women with gestational diabetes mellitus (GDM) or elevated body mass index (BMI), suggesting that HM may have different nutritional and hormonal composition associated with individual maternal characteristics. This also suggests that certain concentrations might be more desirable than others in relation to their effects on infant growth [18], as it is well established that nutritional and hormonal exposures during the first 1000 days of life affect infant growth and metabolic health in the long term [19].
Hormones mediating metabolic function and growth are of particular importance in HM, as they influence a range of infant growth and developmental outcomes. Insulin-like growth factor 1 (IGF-1) is a key mediator of growth hormone action and the most important growth factor in the infant [20]. However, despite its importance in infant growth and regulation of fat accrual during childhood [21], only limited and outdated information is available around its role in HM and its impact on infant growth and development. In experimental animal models, cyclic Glycine-Proline (cGP), a metabolite of IGF-1 derived from cleavage of the N-terminal of IGF-1, has been shown to play a role in the regulation of IGF-1 bioavailability, with the ratio between the two compounds indicating the bioactivity of IGF-1 [22]. The presence and potential role of cGP in HM has not been investigated. Adipokines also constitute an important group of HM bioactives [23]. Amongst these, leptin is known to be involved in appetite and energy balance regulation [24] and to be altered in subjects with elevated BMI [25]. Other adipokines, such as adiponectin, are involved in the regulation of inflammatory processes and insulin sensitivity [26]. In experimental animal models, the presence of adipokines in HM has been linked to postnatal programming and may impact later metabolic health outcomes in the infant [5,27], including the development of obesity and metabolic syndrome later in life [28]. Nonetheless, with the exception of leptin, the concentration of these hormones in HM and the interplay between infant-maternal characteristics and HM composition remains poorly defined.
As both maternal and infant characteristics, particularly maternal metabolic status before and during pregnancy and infant sex, appear to be associated with HM composition, we hypothesised that interactions between the two influence HM composition, conferring a specific profile to each milk sample. Thus, we investigated the contribution of maternal factors before and during pregnancy and infant characteristics at birth with the hormonal composition of mature HM.
2. Materials and Methods
The present study is based on data and HM samples from 501 mothers and 507 children participating in a Finnish longitudinal cohort, Steps to healthy development of Children (the STEPS Study), which has previously been described in detail [29]. Briefly, all Finnish- and Swedish-speaking mothers who delivered a living child between 1 January 2008 and 31 April 2010 in the Hospital District of Southwest Finland formed the cohort population (in total 9811 mothers and their 9936 children). Altogether, 1797 mothers (18.3% of the total cohort) with 1827 neonates (including 30 pairs of twins) volunteered as participants for the intensive follow-up group of the STEPS study. Written informed consent was obtained from the participants. The study protocol was approved by the Ethics Committee of the Hospital District of South West Finland in February 2007. HM samples were collected approximately 2.6 ± 0.4 months after birth from participants who consented to provide HM. These accounted for 45% of the total sample size of the study (811/1797). In total, 310 samples were further excluded from the present study due to the lack of consent from mothers for secondary analysis on the samples, or insufficient sample volume. HM samples were collected as previously described [30] by manual expression in the morning, between 10 am and 12 pm. Before emptying the content of one breast in the provided container, mothers manually expressed the first few drops of foremilk to waste.
Self-reported height and weight before pregnancy and minimum and maximum weight during pregnancy were collected at recruitment and used to determine pre-pregnancy BMI and pregnancy weight gain. Mothers were then grouped into four categories according to their pre-pregnancy BMI (underweight < 18.5 kg/m2, normal weight 18.5–24.9 kg/m2, overweight 25–29.9 kg/m2, obese >29.9 kg/m2). Information regarding GDM (diagnosis based on the ICD-10-CM Codes O24), infant sex, birth weight and length were obtained from the Longitudinal Census Files. Birth weight Z scores were calculated using the published references specific to the Finnish population [31]. Socioeconomic information (maternal basic education, family income and main occupation of mother during pregnancy) were collected through prenatal questionnaires [29]. Information on feeding practices were collected through follow-up diaries completed by mothers [29]. Exclusive breastfeeding was defined as the infant not receiving anything other than HM, with the exception of water, supplements or medicines. Total breastfeeding was defined as the infant receiving HM and any other liquid or food.
Leptin and adiponectin analyses were performed using a commercially available enzyme-linked immunosorbent assay (ELISA) kit (human sensitive Leptin ELISA and human Adiponectin ELISA, Mediagnost, Germany). 150 µl of sample was centrifuged at 3000× g for 15 min and the skim milk under the fat layer was used for the assay. For leptin analysis, skim milk samples were diluted 1:20 and the assay performed as per manufacturer’s instructions. For adiponectin, skim milk samples were diluted 1:2 and the assay was performed as per manufacturer’s instructions.
IGF-1 was analysed using a commercially available ELISA kit (human IGF-1 ELISA, Mediagnost, Germany). Skim HM samples were collected following centrifugation at 3000× g for 15 min and diluted 1:2 with acidified dilution buffer. After dilution, samples were centrifuged to precipitate the binding proteins and then analysed as per manufacturer’s instructions.
cGP was analysed through liquid chromatography tandem mass spectrometry (LC-MS), utilising a protocol developed and optimised by our laboratory on rat milk and published previously [32]. The protocol was adapted for analysis of HM. Briefly, 35 µL of cGP-d2 internal standard (175 mg/mL) was added to each sample. Samples were then passed through phospholipid removal cartridges (Phree phospholipid removal solutions, Phenomenex, Torrance, CA, USA) by performing an extraction with 1% (1:99 v/v) formic acid in acetonitrile. Following extraction, samples were vacuum-dried for 6 h and then reconstituted in a water-methanol solution (90:10 v/v) and injected into the machine. The mass spectrometer used a Surveyor MS pump and auto sampler followed by an Ion Max APCI source on a Finnigan TSQ Quantum Ultra AM triple quadruple mass spectrometer, all controlled by FinniganX caliber software (Thermo Electron Corporation, San Jose, CA, USA.). The column used was Kinetex® 1.7 µL EVO C18 100 Å measuring 150 × 2.1 mm (Phenomenex, Torrance, CA, USA). The mobile phase was constituted by methanol-water gradient set at 95:5 (v/v) at a flow of 250 μL/min. Chromatography was performed at 40 °C. Argon was used as the collision gas at 1.2 mTorr. The concentration of cGP in samples was calculated from a standard curve generated for each assay (0.14 ng/mL–265.12 ng/mL). Inter- and intra assay variability was <10%.
HM total protein was quantified in order to normalise the hormone concentrations but also to investigate the associations with maternal-infant factors. The detection of total protein in the samples was carried out by infrared spectrometry using the Direct Detect® technology (Merck, Germany). Following dilution in 1:5 with milli-Q water, 2 µL of HM samples were transferred to the Direct Detect® Assay-free cards (Merck, Germany) and read with the Direct Detect® spectrometer as per the manufacturer’s instructions.
The adiponectin ELISA has previously been reported for use with HM [33]. Leptin ELISAs were used with antibodies previously validated for use with HM [34]. For all ELISAs, HM samples were tested for linearity (parallel displacement to the standard curve for diluted samples) and suitability of dilution/extraction method. The intra- and inter-assay coefficients of variation respectively for the ELISAs (QCs supplied) were adiponectin (5%, 6%), IGF-1 (3%, 9%) and leptin (4%, 8%). Samples were randomised for all assays.
The power provided by the sample size of the population for linear regression and multivariate analysis of variance (MANOVA) was calculated with G*Power 3.1.9.2 as greater than 90% at the 5% significance level for the detection of 10% difference across groups for all the measured main effects. HM concentration of adipokines, IGF-1 and cGP were reported as ng or mg of the total protein concentration per ml in each sample. This was done to allow a better alignment of the results across samples and across studies, by introducing a reference biomarker (protein) that is commonly used for this purpose. Normal distribution of the data was verified through the Shapiro-Wilk test. As concentrations of bioactive components were skewed, they were normalised by log10-transformation. Relationship between pairs of compounds were investigated with bivariate analysis. Simple and multiple linear regression was used to investigate relationship between bioactives concentrations in HM and scale variables such as maternal age, infant nutrition (exclusive breastfeeding, partial breastfeeding, introduction of solid foods), maternal weight gain during pregnancy, weight before pregnancy and infant gestational age, birthweight and birth length. To investigate possible predictors of HM composition amongst categorical values, we used MANOVA and tested the effect of single factors or pairs of factors on HM concentrations of all four bioactive compounds and on the ratio between IGF-1 and cGP [22]. Because some mothers did not exclusively breastfeed their infants at the time of sample collection, we used the duration of exclusive breastfeeding as a correcting factor in our analysis. Similarly, the introduction of solid foods for some infants in the cohort occurred before the milk sample was collected, and for this reason, we investigated the association between HM composition and introduction of solids. As we were specifically looking at sex-specific effects, each factor was paired with infant sex when fitting the relative MANOVA model. Other variables that were tested included maternal pre-pregnancy BMI, GDM, maternal basic education and main occupation during pregnancy, depression, birth-mode and multiple-single pregnancy. When multiple groups were compared, a Bonferroni correction was applied. All statistical analyses were performed using IBM SPSS (version 25) and the graphs generated by using GraphPad Prism 7 and RStudio.
3. Results
3.1. Population Characteristics
The main demographics of the study population are detailed in Table 1. Over 50% of the population presented with a normal BMI and less than 10% developed GDM (% of GDM mothers within the different BMI classes = 5.3% underweight, 4.1% normal weight, 17.6% overweight, 25.5% obese). A majority of mothers had a secondary school qualification and spent most of their pregnancy working full-time. Nearly half of the population (49%) reported exclusive breastfeeding for three months or less while the remainder (51%) reported exclusive breastfeeding for up to six and a half months. Overall, 80% of mothers reported a total breastfeeding (exclusive and partial) duration above 6 months. The introduction of solid foods occurred before 4 months of age for 42.2% of the population and after 4 months for the remaining infants (57.8%).

Table 1.
Overall characteristics of the study population for n = 501 mothers and n = 507 infants taking part in the Finnish STEPS cohort.
3.2. HM Samples
Time of HM collection (i.e., month post-partum) in the present cohort (for leptin β = −0.030 and p = 0.505, for adiponectin β = −0.019 and p = 0.667, for IGF-1 β = 0.059 and p = 0.191, for cGP β = 0.033 and p = 0.498) did not affect any of the analytes, and thus, was not included in any further analyses. Values of the five analytes across the study population are reported in Table 2. IGF-1 and adiponectin concentrations displayed correlations with leptin (β = 0.189 for IGF-1 and β = 0.089 for adiponectin). A visualization of the general hormonal composition and clustering is shown in Figure 1.

Table 2.
Characteristics of milk samples for n = 501 mothers and n = 507 infants taking part in the Finnish STEPS cohort.
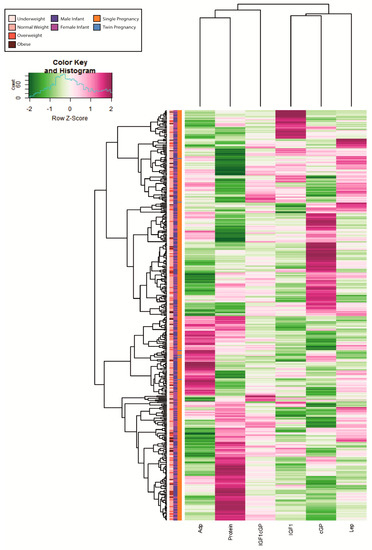
Figure 1.
Heatmap displaying hormonal composition (z-scores) for 423 samples in the Finnish STEPS cohort. Only samples with no missing information were included in the heatmap. Adp = Adiponectin, IGF1 = Insulin-like growth factor 1, cGP = cyclic-Glycine-Proline, IGF1cGP = IGF1/cGP ratio, Lep = leptin. The missing samples have been excluded due to missing information for one or more hormone measurements.
3.3. Maternal Factors and HM Composition
HM leptin concentration showed a strong association with maternal pre-pregnancy weight (Table 3) and BMI (p < 0.001, Table 4), with overweight and obese mothers having significantly higher HM leptin concentrations. Furthermore, HM IGF-1 displayed a positive correlation with maternal weight gain during pregnancy (Table 3), which was maintained when correcting for maternal pre-pregnancy weight (p = 0.009, β = 0.127). Finally, the concentration of total protein in the samples was associated with maternal basic education (p = 0.008, Table 4). No significant association was found between maternal factors and either cGP or adiponectin.

Table 3.
Simple linear regression between maternal-infant characteristics and HM adiponectin, leptin, IGF-1, cGP and total protein.

Table 4.
Associations between maternal-infant characteristics and HM adiponectin, leptin, IGF-1, cGP and protein according to MANOVA analyses.
3.4. Infant Factors and HM Composition
As shown in Table 3, adiponectin was positively correlated with infant birthweight (β = −0.106, p = 0.02). Giving birth to twins also was associated to HM adiponectin concentrations with mothers of twins secreting higher adiponectin in their milk (Table 4) as compared to mothers of singletons. As illustrated in Table 3, the total protein content of HM was correlated with infant nutritional practices and showed significant differences in association with birth mode (p = 0.003). The IGF-1/cGP ratio displayed a positive correlation with gestational age (β = 0.103, p = 0.033).
3.5. Maternal-Infant Interactions, Sex-Specificity and HM Composition
Our cohort presented evidence of sex-specific effects on HM hormonal concentrations. IGF-1/cGP ratio showed a sex-specific interaction with maternal basic education (p = 0.035, Figure 2A). Additionally, adiponectin concentrations were observed to be different for male and female infants in relation to GDM (p = 0.031, Figure 2B) and maternal work status during pregnancy (p = 0.039, Figure 2D). However, in the case of GDM, the sex-specific differences became non-significant when correcting the analysis for exclusive duration of breastfeeding (p = 0.05). Finally, total protein concentrations were elevated in mothers of males who underwent C-section (Figure 2C).
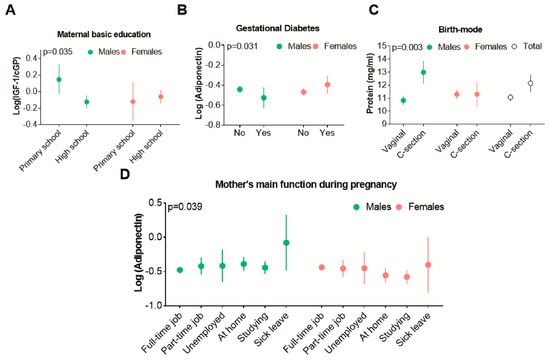
Figure 2.
Sex-specific interactions and human milk (HM) composition. p-values are relative to the interaction between the two factors and HM composition (i.e., infant sex, birth-mode and milk protein). All the graphs show that maternal factors ((A) basic education, (B) gestational diabetes, (C) birth-mode and (D) mother’s occupation during pregnancy) is associated with the concentration of HM components in a sex-specific manner. Graphs represent Mean and CIs. Mothers in the Sick Leave group were only n = 3 (two males and one female). IGF1 = Insulin-like growth factor 1, cGP = cyclic-Glycine-Proline, IGF1cGP = IGF1/cGP ratio.
4. Discussion
Our findings showed an association between pre-pregnancy BMI, pregnancy factors (pregnancy weight gain, GDM, multiple birth, birth-mode and infant gestational age) and infant characteristics at birth (infant sex and birth weight) and the concentration of bioactive compounds in HM collected three months after birth. In the present study, we also report, for the first time to our knowledge, the presence and concentrations of cGP in HM.
The contribution of maternal BMI to HM adipokines [35], particularly leptin [36], is well documented and was further confirmed by our findings. Overweight and obese mothers had significantly elevated HM leptin concentrations compared to normal weight mothers. Additionally, HM IGF-1 concentrations at the time of collection was proportional to pregnancy weight-gain. Higher pregnancy weight gain could have arisen due to higher circulating IGF-1 that would have stimulated foetal growth [37], but HM IGF-1 did not correlate to infant birthweight in our cohort despite previous studies reporting increased HM IGF-1 concentrations with GDM and macrosomia [38]. Differences in dietary intakes, and thus pregnancy weight gain, might have caused the observed increases in HM IGF-1 concentration [39], although in the absence of maternal dietary information during pregnancy we cannot explore such associations. In our cohort, we observed no correlation between time of collection (i.e., month post-partum) and HM composition. This was most likely due to the fact that the period of HM collection in the present cohort spanned predominantly between 2 and 3 months post-partum (90% of samples), when HM composition is mature and the least affected by changes in lactation stage.
HM adiponectin was higher in mothers who delivered infants small for gestational age, as reported in previous studies [36] and in mothers of twins. Although the latter group was of low sample size in our cohort, the literature reports higher circulating adiponectin during twin pregnancies [40]. Elevated concentrations of circulating adiponectin are attributed to the larger placenta carried by mothers of twins [41] but are known to reduce significantly shortly after birth [40]. Therefore, it is not clear how higher concentrations of adiponectin would remain in HM of mothers who gave birth to twins three months prior to HM sample collection.
We observed that GDM mothers of males had the lowest concentration of HM adiponectin compared to GDM mothers of females and non GDM mothers of males and females, suggesting that infant sex can have a major effect on milk composition. The existing literature reports evidence that lower circulating adiponectin concentrations during pregnancy is associated with the incidence of GDM [42]. Circulating concentrations of adiponectin are also known to be sexually dimorphic, as increasing concentrations of testosterone inhibit the production of adiponectin by adipocytes [43,44]. Notably, an increase in testosterone concentrations commonly occurs in mothers who are carrying a male foetus [45]. Although in our cohort these sex-specific correlations became statistically non-significant when corrected for exclusive breastfeeding duration, the p-value (0.05) still suggests an interesting associative trend. Considering that the number of GDM mothers in our cohort was limited to 44 and only constituted less than 10% of the study population, further studies with a larger GDM group should investigate this association and the impact of low adiponectin intakes for male babies, since low adiponectin is a risk factor for a range of metabolic and cardiovascular disorders [46,47].
Birth-mode also displayed a sex-specific effect on HM composition, as mothers of males who underwent C-section displayed the highest amount of protein in their milk compared to all other groups. In our cohort, mothers who underwent C-section generally displayed higher protein irrespective of infant sex. However, the association between C-section and mature HM composition appears to be a novel finding in the present study. As elevated protein concentrations during early life are known to increase the risk of childhood obesity [48], it is crucial to understand whether HM protein content is altered by C-section, or whether the elevated protein content of HM constitutes an adaptation to provide more nutrients to those infants with higher requirements. In our cohort, there were no elective C-sections, and most of them were performed on mothers that were past 40 weeks of gestation (n = 39) compared to mothers who were less than 37 weeks of gestation (n = 11) and mothers who were between 37 and 40 weeks of gestation (n = 12). Only four of the infants born by C-section in our cohort were classified as small for gestational age, compared to 55 infants that were classified as appropriate for gestational age and two that were classified as large for gestational age. Taken together these observations, although of low sample size, may suggest that rather than constituting an adaptation to provide small babies with higher protein, the elevated concentrations of protein in HM of mothers who underwent C-section may be the result of altered metabolic pathways and therefore warrants further investigation.
Of interest, our analysis also revealed sex-specific effects linked to socioeconomic and stress-related factors. As an example, higher concentrations of adiponectin and the IGF-1/cGP ratio were observed in male infants of mothers that experienced what would be classed as more stressful pregnancies (i.e., sickness during pregnancy) or were of lower socioeconomic status (i.e., mother only completed primary school) although the size of some subgroups in these cases was extremely limited as discussed below. We also found that the amount of protein in HM was higher for mothers with a lower education background. While these observations are purely associative, we have previously reported that social influences, including maternal educational status, impact on HM stress hormone levels [30]. Given the known link between stress hormones and changes in IGF-1 and adiponectin [49], changes in stress markers may have mediated some of the associations observed. Although due to sample size limitations, cortisol and cortisone were unable to be measured in the current cohort.
The main strength of the present study is the large sample size, although the size of certain subgroups was limited due to the fact that the study was designed retrospectively. The lack of multiple HM collection time points from individual mothers prevented the analysis of HM compositional changes within subjects. Additionally, our samples were only representative of morning HM rather than the gold standard 24-h collection and considerable time passed between sample collection (2008–2010) and the biochemical analyses (2018) presented in this study, due to the retrospective nature of the present study design. However, the compounds analysed in the present study are known to be stable at −80 °C. Furthermore, because the HM samples were collected exclusively in the morning, collection timing and procedure was relatively standardised across all mothers. Many studies previously analysed HM composition around 3 months after birth. At this time, HM composition is more stable and thus less variable, resulting in comparable samples.
Matched plasma samples and access to more detailed dietary information during pregnancy and lactation would have been useful to further delineate some of the associations detailed. Although the design of the current study does not allow any detailed mechanistic insight, previous observations in a bovine model have reported on differential programming of milk production as a function of foetal sex [50]. The study by Hinde et al. showed a marked and sustained effect of mammary function that arises as a result of foetal sex, with the female sex of the foetus enhancing milk production for multiple consequential lactations.
5. Conclusions
Overall, our findings show that maternal-infant factors, specifically maternal pregnancy and pre-pregnancy characteristics and infant sex, interact and impact upon HM compositional profiles up to three months after birth, suggesting that HM composition may be delineated during pregnancy and may have a characteristic fingerprint for every mother-baby dyad. Such a fingerprint might be used to draw maps that would serve to characterise HM composition in association with specific pathophysiological conditions. Whether the intake of HM and hormonal concentrations associated with these pathophysiological conditions impacts on postnatal outcomes and growth trajectories on the long term remains to date unknown and should be investigated in future research. This will allow a better understanding of the role played by specific nutritional and hormonal exposures during early life, in order to implement nutrition for infants who have no access to HM but also to design strategies that would help improve possibly altered HM composition due to pathological conditions. Although we had no means to investigate “cause-effect” relationships between maternal circulating hormones, dietary intakes and bioactives in HM, in the present study, the associations we observed suggest that prospective studies designed to untangle such associations and establish key determinants (and interactions therein) related to HM composition and infant outcomes are warranted.
Author Contributions
L.G. designed the research questions, carried out laboratory analysis and data interpretation and drafted the manuscript. H.L. designed sample and data collection, assisted with statistical analysis and contributed to the manuscript development. A.M.M. and C.M.R. helped design the research question and performing assay validations, and together with D.C.-S. and S.R., edited the final manuscript. M.H.V. and S.P. supervised the entire process from laboratory analysis to submission of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This analysis was funded by the Liggins Institute FRDF (Faculty Research Development Fund, grant number 3716954) and University of Auckland Foundation (grant number 3708092). The clinical trial and collection of samples was funded by the Academy of Finland (grants 121569 and 123571).
Acknowledgments
We thank the research team involved in the trial and sample and data collection and mothers who gave their milk for the current study. We also thank Eric Thorstensen, laboratory manager at the Liggins Institute, for his help with cGP assay validation in human milk and assistance with sample analysis on the LC-MS, and Christopher Triggs, senior lecturer in statistics at the University of Auckland and statistician at the Liggins Institute, for assisting with statistical analysis of the data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Blum, J.W.; Baumrucker, C.R. Insulin-like Growth Factors (IGFs), IGF Binding Proteins, and Other Endocrine Factors in Milk: Role in the Newborn. Adv. Exp. Med. Biol. 2008, 606, 397–422. [Google Scholar] [CrossRef]
- Çatlı, G.; Olgaç Dündar, N.; Dündar, B.N. Adipokines in Breast Milk: An Update. J. Clin. Res. Pediatr. Endocrinol. 2014, 6, 192–201. [Google Scholar] [CrossRef]
- Klok, M.D.; Jakobsdottir, S.; Drent, M.L. The Role of Leptin and Ghrelin in the Regulation of Food Intake and Body Weight in Humans: A Review. Obes. Rev. An Off. J. Int. Assoc. Study Obes. 2007, 8, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Murray, P.G.; Clayton, P.E. Endocrine Control of Growth. Am. J. Med. Genet. C. Semin. Med. Genet. 2013, 163C, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Picó, C.; Oliver, P.; Sánchez, J.; Miralles, O.; Caimari, A.; Priego, T.; Palou, A. The Intake of Physiological Doses of Leptin during Lactation in Rats Prevents Obesity in Later Life. Int. J. Obes. (Lond) 2007, 31, 1199–1209. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Wu, K.; Yu, Z.; Ren, Y.; Zhao, Y.; Jiang, Y.; Xu, X.; Li, W.; Jin, Y.; Yuan, J.; et al. Changes in Fatty Acid Composition of Human Milk over Lactation Stages and Relationship with Dietary Intake in Chinese Women. Food Funct. 2016, 7, 3154–3162. [Google Scholar] [CrossRef]
- Ballard, O.; Morrow, A.L. Human Milk Composition: Nutrients and Bioactive Factors. Pediatr. Clin. North Am. 2013, 60, 49–74. [Google Scholar] [CrossRef]
- Mizuno, K.; Nishida, Y.; Taki, M.; Murase, M.; Mukai, Y.; Itabashi, K.; Debari, K.; Iiyama, A. Is Increased Fat Content of Hindmilk due to the Size or the Number of Milk Fat Globules? Int. Breastfeed. J. 2009, 4, 7. [Google Scholar] [CrossRef]
- Pundir, S.; Wall, C.R.; Mitchell, C.J.; Thorstensen, E.B.; Lai, C.T.; Geddes, D.T.; Cameron-Smith, D. Variation of Human Milk Glucocorticoids over 24 Hour Period. J. Mammary Gland Biol. Neoplasia 2017, 22, 85–92. [Google Scholar] [CrossRef]
- Martin, M.A.; Lassek, W.D.; Gaulin, S.J.C.; Evans, R.W.; Woo, J.G.; Geraghty, S.R.; Davidson, B.S.; Morrow, A.L.; Kaplan, H.S.; Gurven, M.D. Fatty Acid Composition in the Mature Milk of Bolivian Forager-Horticulturalists: Controlled Comparisons with a US Sample. Matern. Child Nutr. 2012, 8, 404–418. [Google Scholar] [CrossRef]
- Panagos, P.G.; Vishwanathan, R.; Penfield-Cyr, A.; Matthan, N.R.; Shivappa, N.; Wirth, M.D.; Hebert, J.R.; Sen, S. Breastmilk from Obese Mothers Has pro-Inflammatory Properties and Decreased Neuroprotective Factors. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2016, 36, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Nayak, U.; Kanungo, S.; Zhang, D.; Ross Colgate, E.; Carmolli, M.P.; Dey, A.; Alam, M.; Manna, B.; Nandy, R.K.; Kim, D.R.; et al. Influence of Maternal and Socioeconomic Factors on Breast Milk Fatty Acid Composition in Urban, Low-Income Families. Matern. Child Nutr. 2017, 13, e12423. [Google Scholar] [CrossRef] [PubMed]
- Galante, L.; Milan, A.M.; Reynolds, C.M.; Cameron-Smith, D.; Vickers, M.H.; Pundir, S. Sex-Specific Human Milk Composition: The Role of Infant Sex in Determining Early Life Nutrition. Nutrients 2018, 10, 1194. [Google Scholar] [CrossRef]
- Klein, K.; Bancher-Todesca, D.; Graf, T.; Garo, F.; Roth, E.; Kautzky-Willer, A.; Worda, C. Concentration of Free Amino Acids in Human Milk of Women with Gestational Diabetes Mellitus and Healthy Women. Breastfeed. Med. Off. J. Acad. Breastfeed. Med. 2013, 8, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Azulay Chertok, I.R.; Haile, Z.T.; Eventov-Friedman, S.; Silanikove, N.; Argov-Argaman, N. Influence of Gestational Diabetes Mellitus on Fatty Acid Concentrations in Human Colostrum. Nutrition 2017, 36, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Andreas, N.J.; Hyde, M.J.; Herbert, B.R.; Jeffries, S.; Santhakumaran, S.; Mandalia, S.; Holmes, E.; Modi, N. Impact of Maternal BMI and Sampling Strategy on the Concentration of Leptin, Insulin, Ghrelin and Resistin in Breast Milk across a Single Feed: A Longitudinal Cohort Study. BMJ Open 2016, 6. [Google Scholar] [CrossRef]
- Young, B.E.; Levek, C.; Reynolds, R.M.; Rudolph, M.C.; MacLean, P.; Hernandez, T.L.; Friedman, J.E.; Krebs, N.F. Bioactive Components in Human Milk Are Differentially Associated with Rates of Lean and Fat Mass Deposition in Infants of Mothers with Normal vs. Elevated BMI. Pediatr. Obes. 2018, 13, 598–606. [Google Scholar] [CrossRef]
- Demmelmair, H.; Koletzko, B. Variation of Metabolite and Hormone Contents in Human Milk. Clin. Perinatol. 2017, 44, 151–164. [Google Scholar] [CrossRef]
- Ford, N.D.; Behrman, J.R.; Hoddinott, J.F.; Maluccio, J.A.; Martorell, R.; Ramirez-Zea, M.; Stein, A.D. Exposure to Improved Nutrition from Conception to Age 2 Years and Adult Cardiometabolic Disease Risk: A Modelling Study. Lancet. Glob. Heal. 2018, 6, e875–e884. [Google Scholar] [CrossRef]
- Bafico, A.; Aaronson, S.A. Classification of Growth Factors and Their Receptors. In Holland-Frei Cancer Medicine, 6th ed.; Kufe, D.W., Pollock, R.E., Weichselbaum, R.R., Bast, R.C., Jr., Gansler, T.S., Holland, J.F., Frei, E., III, Eds.; BC Decker: Hamilton, ON, Canada, 2003; ISBN 1-55009-213-8. [Google Scholar]
- Marcovecchio, M.L.; Chiarelli, F. Obesity and Growth during Childood and Puberty. World Rev. Nutr. Diet. 2013, 106, 135–141. [Google Scholar] [CrossRef]
- Guan, J.; Gluckman, P.; Yang, P.; Krissansen, G.; Sun, X.; Zhou, Y.; Wen, J.; Phillips, G.; Shorten, P.R.; McMahon, C.D.; et al. Cyclic Glycine-Proline Regulates IGF-1 Homeostasis by Altering the Binding of IGFBP-3 to IGF-1. Sci. Rep. 2014, 4, 4388. [Google Scholar] [CrossRef] [PubMed]
- Fantuzzi, G. Adipose Tissue, Adipokines, and Inflammation. J. Allergy Clin. Immunol. 2005, 115, 911–919. [Google Scholar] [CrossRef] [PubMed]
- Ahima, R.S.; Antwi, D.A. Brain Regulation of Appetite and Satiety. Endocrinol. Metab. Clin. North Am. 2008, 37, 811–823. [Google Scholar] [CrossRef] [PubMed]
- Farr, O.M.; Gavrieli, A.; Mantzoros, C.S. Leptin Applications in 2015: What Have We Learned about Leptin and Obesity? Curr. Opin. Endocrinol. Diabetes. Obes. 2015, 22, 353–359. [Google Scholar] [CrossRef]
- Berg, A.H.; Combs, T.P.; Scherer, P.E. ACRP30/adiponectin: An Adipokine Regulating Glucose and Lipid Metabolism. Trends Endocrinol. Metab. 2002, 13, 84–89. [Google Scholar] [CrossRef]
- Nozhenko, Y.; Asnani-Kishnani, M.; Rodríguez, A.M.; Palou, A. Milk Leptin Surge and Biological Rhythms of Leptin and Other Regulatory Proteins in Breastmilk. PLoS ONE 2015, 10, e0145376. [Google Scholar] [CrossRef][Green Version]
- Purcell, R.H.; Sun, B.; Pass, L.L.; Power, M.L.; Moran, T.H.; Tamashiro, K.L.K. Maternal Stress and High-Fat Diet Effect on Maternal Behavior, Milk Composition, and Pup Ingestive Behavior. Physiol. Behav. 2011, 104, 474–479. [Google Scholar] [CrossRef]
- Lagstrom, H.; Rautava, P.; Kaljonen, A.; Raiha, H.; Pihlaja, P.; Korpilahti, P.; Peltola, V.; Rautakoski, P.; Osterbacka, E.; Simell, O.; et al. Cohort Profile: Steps to the Healthy Development and Well-Being of Children (the STEPS Study). Int. J. Epidemiol. 2013, 42, 1273–1284. [Google Scholar] [CrossRef]
- Pundir, S.; Nuora, A.; Junttila, N.; Rosemary Wall, C.; Linderborg, K.; Cameron-Smith, D.; Lagstr, H. Maternal Influences on the Glucocorticoid Concentrations of Human Milk: The STEPS Study. Clin. Nutr. 2018, 38, 1913–1920. [Google Scholar] [CrossRef]
- Sankilampi, U.; Hannila, M.-L.; Saari, A.; Gissler, M.; Dunkel, L. New Population-Based References for Birth Weight, Length, and Head Circumference in Singletons and Twins from 23 to 43 Gestation Weeks. Ann. Med. 2013, 45, 446–454. [Google Scholar] [CrossRef]
- Singh-Mallah, G.; Singh, K.; McMahon, C.D.; Harris, P.; Brimble, M.A.; Thorstensen, E.; Guan, J. Maternally Administered Cyclic Glycine-Proline Increases Insulin-Like Growth Factor-1 Bioavailability and Novelty Recognition in Developing Offspring. Endocrinology 2018, 157, 3130–3139. [Google Scholar] [CrossRef]
- Savino, F.; Lupica, M.M.; Benetti, S.; Petrucci, E.; Liguori, S.A.; Cordero Di Montezemolo, L. Adiponectin in Breast Milk: Relation to Serum Adiponectin Concentration in Lactating Mothers and Their Infants. Acta Paediatr. Int. J. Paediatr. 2012, 101, 1058–1062. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Sorrenti, M.; Benetti, S.; Lupica, M.M.; Liguori, S.A.; Oggero, R. Resistin and Leptin in Breast Milk and Infants in Early Life. Early Hum. Dev. 2012, 88, 779–782. [Google Scholar] [CrossRef] [PubMed]
- Kratzsch, J.; Bae, Y.J. Adipokines in Human Breast Milk. Best Pract. Res. Clin. Endocrinol. Metab. 2018, 32, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Brunner, S.; Schmid, D.; Zang, K.; Much, D.; Knoeferl, B.; Kratzsch, J.; Amann-Gassner, U.; Bader, B.L.; Hauner, H. Breast Milk Leptin and Adiponectin in Relation to Infant Body Composition up to 2 Years. Pediatr. Obes. 2015, 10, 67–73. [Google Scholar] [CrossRef]
- Gluckman, P.D.; Pinal, C.S. Regulation of Fetal Growth by the Somatotrophic Axis. J. Nutr. 2003, 133, 1741S–1746S. [Google Scholar] [CrossRef]
- Mohsen, A.H.A.; Sallam, S.; Ramzy, M.M.; Hamed, E.K. Investigating the Relationship between Insulin-like Growth Factor-1 (IGF-1) in Diabetic Mother’s Breast Milk and the Blood Serum of Their Babies. Electron. Physician 2016, 8, 2546–2550. [Google Scholar] [CrossRef][Green Version]
- Fontana, L.; Weiss, E.P.; Villareal, D.T.; Klein, S.; Holloszy, J.O. Long-Term Effects of Calorie or Protein Restriction on Serum IGF-1 and IGFBP-3 Concentration in Humans. Aging Cell 2008, 7, 681–687. [Google Scholar] [CrossRef]
- Fuglsang, J.; Sandager, P.; Frystyk, J.; Møller, N.; Flyvbjerg, A.; Ovesen, P. Alterations in Circulating Adiponectin Levels Occur Rapidly after Parturition. Eur. J. Endocrinol. 2010, 163, 69–73. [Google Scholar] [CrossRef]
- Chen, J.; Tan, B.; Karteris, E.; Zervou, S.; Digby, J.; Hillhouse, E.W.; Vatish, M.; Randeva, H.S. Secretion of Adiponectin by Human Placenta: Differential Modulation of Adiponectin and Its Receptors by Cytokines. Diabetologia 2006, 49, 1292–1302. [Google Scholar] [CrossRef]
- Thagaard, I.N.; Krebs, L.; Holm, J.-C.; Lange, T.; Larsen, T.; Christiansen, M. Adiponectin and Leptin as First Trimester Markers for Gestational Diabetes Mellitus: A Cohort Study. Clin. Chem. Lab. Med. 2017, 55, 1805–1812. [Google Scholar] [CrossRef] [PubMed]
- Böttner, A.; Kratzsch, J.; Müller, G.; Kapellen, T.M.; Blüher, S.; Keller, E.; Blüher, M.; Kiess, W. Gender Differences of Adiponectin Levels Develop during the Progression of Puberty and Are Related to Serum Androgen Levels. J. Clin. Endocrinol. Metab. 2004, 89, 4053–4061. [Google Scholar] [CrossRef] [PubMed]
- Horenburg, S.; Fischer-Posovszky, P.; Debatin, K.-M.; Wabitsch, M. Influence of Sex Hormones on Adiponectin Expression in Human Adipocytes. Horm. Metab. Res. 2008, 40, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Meulenberg, P.M.; Hofman, J.A. Maternal Testosterone and Fetal Sex. J. Steroid Biochem. Mol. Biol. 1991, 39, 51–54. [Google Scholar] [CrossRef]
- Shibata, R.; Ouchi, N.; Murohara, T. Adiponectin and Cardiovascular Disease. Circ. J. 2009, 73, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Tsou, P.-L.; Jiang, Y.-D.; Chang, C.-C.; Wei, J.-N.; Sung, F.-C.; Lin, C.-C.; Chiang, C.-C.; Tai, T.-Y.; Chuang, L.-M. Sex-Related Differences between Adiponectin and Insulin Resistance in Schoolchildren. Diabetes Care 2004, 27, 308–313. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weber, M.; Grote, V.; Closa-Monasterolo, R.; Escribano, J.; Langhendries, J.-P.; Dain, E.; Giovannini, M.; Verduci, E.; Gruszfeld, D.; Socha, P.; et al. Lower Protein Content in Infant Formula Reduces BMI and Obesity Risk at School Age: Follow-up of a Randomized Trial. Am. J. Clin. Nutr. 2014, 99, 1041–1051. [Google Scholar] [CrossRef]
- Papargyri, P.; Zapanti, E.; Salakos, N.; Papargyris, L.; Bargiota, A.; Mastorakos, G. Links between HPA Axis and Adipokines: Clinical Implications in Paradigms of Stress-Related Disorders. Expert Rev. Endocrinol. Metab. 2018, 13, 317–332. [Google Scholar] [CrossRef]
- Hinde, K.; Carpenter, A.J.; Clay, J.S.; Bradford, B.J. Holsteins Favor Heifers, Not Bulls: Biased Milk Production Programmed during Pregnancy as a Function of Fetal Sex. PLoS ONE 2014, 9, e86169. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).