Does an Age-Specific Treatment Program Augment the Efficacy of a Cognitive-Behavioral Weight Loss Program in Adolescence and Young Adulthood? Results from a Controlled Study
Abstract
1. Introduction
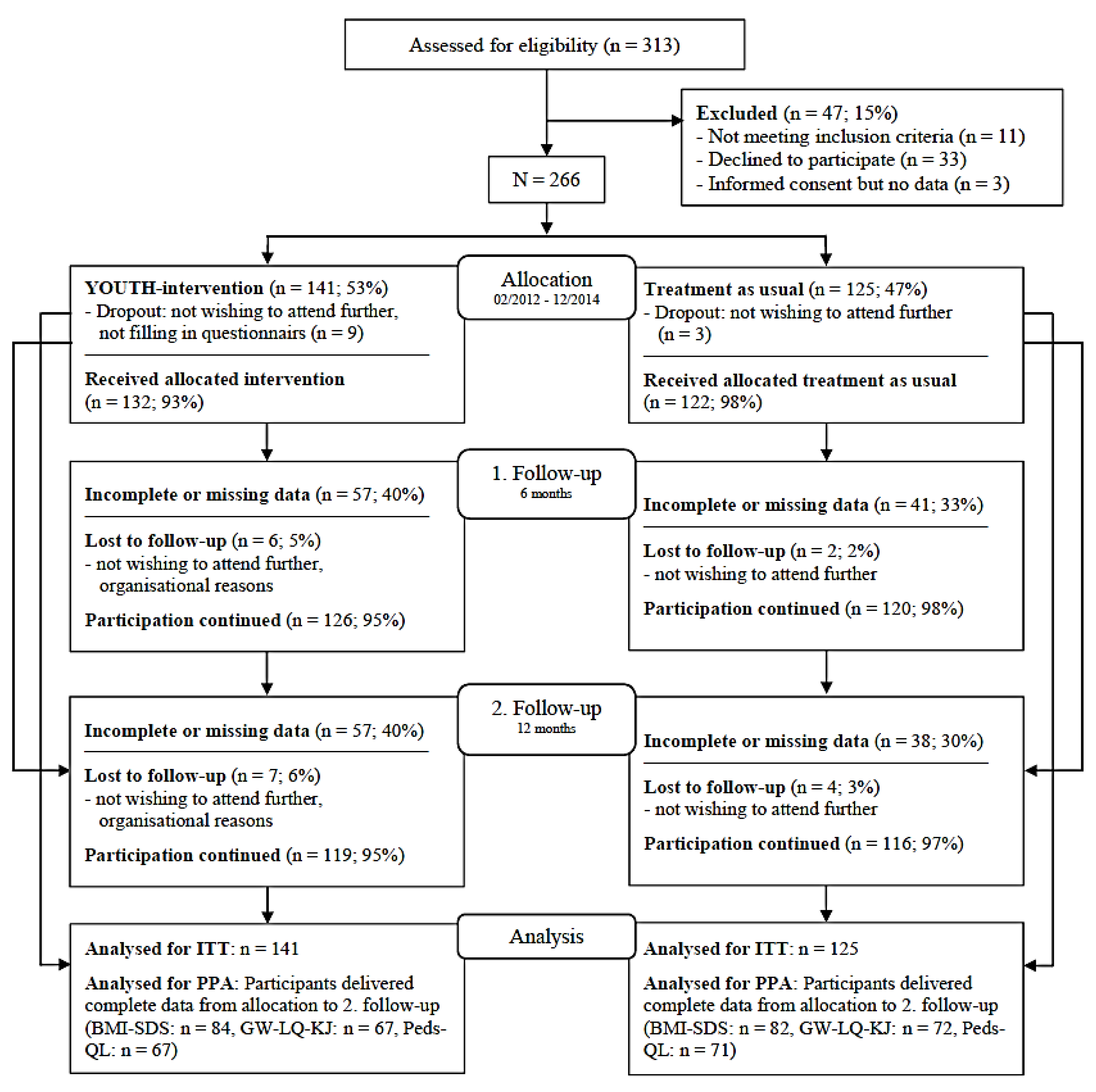
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Interventions
2.4. Measures
2.5. Data Analysis
3. Results
3.1. Participant Characteristics at Baseline
3.2. Short-and Long-Term Effects of Treatment Allocation
3.3. Changes over Time
4. Discussion
4.1. Short- and Long-Term Effects of Treatment Allocation
4.2. Changes over Time
4.3. Strengths and Limitations
5. Clinical Implications
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Schienkiewitz, A.; Brettschneider, A.-K.; Damerow, S.; Schaffrath Rosario, A. Übergewicht und Adipositas im Kindes- und Jugendalter in Deutschland – Querschnittergebnisse aus KiGGS Welle 2 und Trends. J. Health Monit. 2018, 3, 16–23. [Google Scholar] [CrossRef]
- Mensink, G.; Schienkiewitz, A.; Haftenberger, M.; Lampert, T.; Ziese, T.; Scheidt-Nave, C. Übergewicht und Adipositas in Deutschland: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1) [Overweight and obesity in Germany: Results of the German Health Interview and Examination Survey for Adults (DEGS1)]. Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 5, 786–794. [Google Scholar] [CrossRef] [PubMed]
- Lanoye, A.; Brown, K.L.; LaRose, J.G. The Transition into Young Adulthood: A Critical Period for Weight Control. Curr. Diabetes Rep. 2017, 17, 114. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.C.; Story, M.; Larson, N.I.; Neumark-Sztainer, D.; Lytle, L.A.; Neumark-Sztainer, D.; Laska, M.; Neumark-Sztainer, D. Emerging Adulthood and College-aged Youth: An Overlooked Age for Weight-related Behavior Change. Obesity 2008, 16, 2205–2211. [Google Scholar] [CrossRef] [PubMed]
- Vlassopoulos, A.; Combet, E.; Lean, M.E.J. Changing distributions of body size and adiposity with age. Int. J. Obes. 2014, 38, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Arnett, J.J.; Jensen, A.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Deforche, B.; Van Dyck, D.; Deliens, T.; De Bourdeaudhuij, I. Changes in weight, physical activity, sedentary behaviour and dietary intake during the transition to higher education: A prospective study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 16. [Google Scholar] [CrossRef]
- Finlayson, G.; Cecil, J.; Higgs, S.; Hill, A.; Hetherington, M. Susceptibility to weight gain. Eating behaviour traits and physical activity as predictors of weight gain during the first year of university. Appetite 2012, 58, 1091–1098. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.; Dee, A.; Perry, I. The lifetime costs of overweight and obesity in childhood and adolescence: A systematic review. Obes. Rev. 2018, 19, 452–463. [Google Scholar] [CrossRef]
- Tremmel, M.; Gerdtham, U.-G.; Nilsson, P.M.; Saha, S. Economic Burden of Obesity: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2017, 14, 435. [Google Scholar] [CrossRef]
- Cheng, H.L.; Medlow, S.; Steinbeck, K. The Health Consequences of Obesity in Young Adulthood. Curr. Obes. Rep. 2016, 5, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, M.M.; Zaepfel, A.; Bjornstad, P.; Nadeau, K.J. Age-Related Consequences of Childhood Obesity. Gerontology 2014, 60, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Harriger, J.A.; Thompson, J.K. Psychological consequences of obesity: Weight bias and body image in overweight and obese youth. Int. Rev. Psychiatry 2012, 24, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Loth, K.A.; Mond, J.; Wall, M.; Neumark-Sztainer, D. Weight status and emotional well-being: Longitudinal findings from Project EAT. J. Pediatric Psychol. 2011, 36, 216–225. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Story, M.; Hannan, P.J.; Perry, C.L.; Irving, L.M. Weight-Related Concerns and Behaviors Among Overweight and Nonoverweight Adolescents. Arch. Pediatr. Adolesc. Med. 2002, 156, 171–178. [Google Scholar] [CrossRef]
- Puhl, R.M.; Heuer, C.A. The Stigma of Obesity: A Review and Update. Obesity 2009, 17, 941–964. [Google Scholar] [CrossRef] [PubMed]
- Mirza, N.M.; Yanovski, J.A. Prevalence and consequences of pediatric obesity. In Handbook of Obesity: Epidemology, Etiology, and Physiopathology; Bray, G.A., Bouchard, C., Eds.; Taylor & Francis Ltd.: Boca Raton, FL, USA, 2014; pp. 55–74. [Google Scholar]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Menrath, I.; Gminder, A.; Hiort, O.; Thyen, U. Gesundheitsbezogene Lebensqualität, Selbstwert und Gesundheitsverhalten durchschnittlich 6 Jahre nach einem ambulanten Adipositastherapieprogramm [Health Related Quality of Life, Self-Esteem and Health Behaviour on Average 6 Years after an Obesity Outpatient Lifestyle Program]. Klinische Pädiatrie 2017, 229, 216–222. [Google Scholar] [CrossRef]
- Luttikhuis, H.O.; Baur, L.; Jansen, H.; Shrewsbury, V.A.; O’Malley, C.; Stolk, R.P.; Summerbell, C.D. Interventions for treating obesity in children. Cochrane Database Syst. Rev. 2009, 1, CD001872. [Google Scholar] [CrossRef]
- Thomason, D.L.; Lukkahatai, N.; Kawi, J.; Connelly, K.; Inouye, J. A Systematic Review of Adolescent Self-Management and Weight Loss. J. Pediatr. Health Care 2016, 30, 569–582. [Google Scholar] [CrossRef]
- Deutsche Rentenversicherung Bund. Statistik der Deutschen Rentenversicherung: Rehabilitation 2013; Eigenverlag: Berlin, Germany, 2014; Volume 199. [Google Scholar]
- Gokee-LaRose, J.; Gorin, A.A.; Raynor, H.A.; Laska, M.N.; Jeffery, R.W.; Levy, R.L.; Wing, R.R. Are standard behavioral weight loss programs effective for young adults? Int. J. Obes. 2009, 33, 1374–1380. [Google Scholar] [CrossRef] [PubMed]
- LaRose, J.G.; Tate, D.F.; Lanoye, A.; Fava, J.L.; Jelalian, E.; Blumenthal, M.; Caccavale, L.J.; Wing, R.R. Adapting evidence-based behavioral weight loss programs for emerging adults: A pilot randomized controlled trial. J. Health Psychol. 2017, 24, 870–887. [Google Scholar] [CrossRef] [PubMed]
- Lanoye, A.; Gorin, A.A.; LaRose, J.G. Young Adults’ Attitudes and Perceptions of Obesity and Weight Management: Implications for Treatment Development. Curr. Obes. Rep. 2016, 5, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Laska, M.N.; Pelletier, J.E.; Larson, N.I.; Story, M. Interventions for Weight Gain Prevention during the Transition to Young Adulthood: A review of the literature. J. Adolesc. Health 2012, 50, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Loria, C.M.; Signore, C.; Arteaga, S.S. The Need for Targeted Weight-Control Approaches in Young Women and Men. Am. J. Prev. Med. 2010, 38, 233–235. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Flynn, M.A.T.; McNeil, D.A.; Maloff, B.; Mutasingwa, D.; Wu, M.; Ford, C.; Tough, S.C. Reducing obesity and related chronic disease risk in children and youth: A synthesis of evidence with ’best practice’ recommendations. Obes. Rev. 2006, 7, 7–66. [Google Scholar] [CrossRef] [PubMed]
- Warschburger, P. Jugendliche und junge Erwachsene mit Adipositas: Wie sollte in ihren Augen, die perfekte Therapie aussehen? [Adolescents and Young Adults: What Would a “Perfect Therapy” Look Like?]. Rehabilitation 2017, 56, 1–8. [Google Scholar] [CrossRef]
- Boff, R.M.; Liboni, R.P.A.; Batista, I.P.A.; Souza, L.H.; Oliveira, M.S. Weight loss interventions for overweight and obese adolescents: A systematic review. Eat. Weight Disord. 2016, 22, 211–229. [Google Scholar] [CrossRef] [PubMed]
- Bertz, F.; Pacanowski, C.R.; Levitsky, D.A. Frequent self-weighing with electronic graphic feedback to prevent age-related weight gain in young adults. Obesity 2015, 23, 2009–2014. [Google Scholar] [CrossRef]
- LaRose, J.G.; Lanoye, A.; Tate, D.F.; Wing, R.R. Frequency of self-weighing and weight loss outcomes within a brief lifestyle intervention targeting emerging adults. Obes. Sci. Pract. 2016, 2, 88–92. [Google Scholar] [CrossRef]
- Griffiths, L.J.; Parsons, T.J.; Hill, A.J. Self-esteem and quality of life in obese children and adolescents: A systematic review. Pediatr. Obes. 2010, 5, 282–304. [Google Scholar] [CrossRef] [PubMed]
- Ligthart, K.A.M.; Paulis, W.D.; Djasmo, D.; Koes, B.W.; van Middelkoop, M. Effect of multidisciplinary interventions on quality of life in obese children: A systematic review and meta-analysis. Qual. Life Res. 2015, 24, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- Hoedjes, M.; Makkes, S.; Halberstadt, J.; Noordam, H.; Renders, C.M.; Bosmans, J.E.; Van Der Baan-Slootweg, O.H.; Seidell, J.C. Health-Related Quality of Life in Children and Adolescents with Severe Obesity after Intensive Lifestyle Treatment and at 1-Year Follow-Up. Obes. Facts 2018, 11, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Warschburger, P.; Kroeller, K.; Haerting, J.; Unverzagt, S.; Van Egmond-Fröhlich, A. Empowering Parents of Obese Children (EPOC): A randomized controlled trial on additional long-term weight effects of parent training. Appetite 2016, 103, 148–156. [Google Scholar] [CrossRef]
- Mühlig, Y.; Scherag, A.; Bickenbach, A.; Giesen, U.; Holl, R.; Holle, R.; Kiess, W.; Lennerz, B.; Brintrup, D.L.; Moss, A.; et al. A Structured, Manual-Based Low-Level Intervention vs. Treatment as Usual Evaluated in a Randomized Controlled Trial for Adolescents with Extreme Obesity—The STEREO Trial. Obes. Facts 2017, 10, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Moss, A.; Wabitsch, M.; Kromeyer-Hauschild, K. Referenzwerte für den Body-Mass-Index für Kinder, Jugendliche und Erwachsene in Deutschland. Adipositas 2015, 9, 123–127. [Google Scholar] [CrossRef]
- Warschburger, P.; Fromme, C.; Petermann, F. Gewichtsbezogene Lebensqualität bei Schulkindern: Validität des GW-LQ-KJ. Z. Gesundh. 2004, 12, 159–166. [Google Scholar] [CrossRef]
- Landgraf, J.M.; Abetz, L.; Ware, J.A. The CHQ User Manual; The Health Institute, New England Medical Center: Boston, MA, USA, 1996. [Google Scholar]
- Seid, M.; Kurtin, P.S.; Varni, J.W. PedsQL™ 4.0: Reliability and Validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med. Care 2001, 39, 800–812. [Google Scholar]
- Varni, J.W.; Limbers, C.A.; Burwinkle, T.M. Impaired health-related quality of life in children and adolescents with chronic conditions: A comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL™ 4.0 Generic Core Scales. Health Qual. Life Outcomes 2007, 5, 43. [Google Scholar] [CrossRef]
- Varni, J.W.; Burwinkle, T.M.; Seid, M.; Skarr, D. The PedsQL™* 4.0 as a Pediatric Population Health Measure: Feasibility, Reliability, and Validity. Ambul. Pediatr. 2003, 3, 329–341. [Google Scholar] [CrossRef]
- Wilfley, D.E.; Tibbs, T.L.; Van Buren, D.J.; Reach, K.P.; Walker, M.S.; Epstein, L.H. Lifestyle Interventions in the Treatment of Childhood Overweight: A Meta-Analytic Review of Randomized Controlled Trials. Health Psychol. 2007, 26, 521–532. [Google Scholar] [CrossRef] [PubMed]
- Hoffmeister, U.; Bullinger, M.; van Egmond-Fröhlich, A.; Goldapp, C.; Mann, R.; Ravens-Sieberer, U.; Reinehr, T.; Westenhöfer, J.; Wille, N.; Holl, R.W. Übergewicht und Adipositas in Kindheit und Jugend. Evaluation der ambulanten und stationären Versorgung in Deutschland in der “EvAKuJ-Studie” [Overweight and obesity in childhood and adolescence. Evaluation of inpatient and outpatient care in Germany: The EvAKuJ study]. Bundesgesundheitsblatt Gesundh. Gesundh. 2011, 54, 128–135. [Google Scholar] [CrossRef]
- Elvsaas, I.K.Ø.; Giske, L.; Fure, B.; Juvet, L.K. Multicomponent Lifestyle Interventions for Treating Overweight and Obesity in Children and Adolescents: A Systematic Review and Meta-Analyses. J. Obes. 2017, 2017, 5021902. [Google Scholar] [CrossRef] [PubMed]
- Zolotarjova, J.; Velde, G.T.; Vreugdenhil, A.C.E. Effects of multidisciplinary interventions on weight loss and health outcomes in children and adolescents with morbid obesity. Obes. Rev. 2018, 19, 931–946. [Google Scholar] [CrossRef] [PubMed]
- Naets, T.; Vervoort, L.; Verbeken, S.; Braet, C. Enhancing Childhood Multidisciplinary Obesity Treatments: The Power of Self-Control Abilities as Intervention Facilitator. Front. Psychol. 2018, 9, 123. [Google Scholar] [CrossRef] [PubMed]
- Peirson, L.; Fitzpatrick-Lewis, D.; Morrison, K.; Warren, R.; Ali, M.U.; Raina, P. Treatment of overweight and obesity in children and youth: A systematic review and meta-analysis. CMAJ Open 2015, 3, E35–E46. [Google Scholar] [CrossRef]
- Van Der Heijden, L.B.; Feskens, E.J.M.; Janse, A.J. Maintenance interventions for overweight or obesity in children: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 798–809. [Google Scholar] [CrossRef]
- Makkes, S.; Renders, C.M.; Bosmans, J.E.; Van Der Baan-Slootweg, O.H.; Hoekstra, T.; Seidell, J.C. One-year effects of two intensive inpatient treatments for severely obese children and adolescents. BMC Pediatr. 2016, 16, 120. [Google Scholar] [CrossRef]
- Rank, M.; Wilks, D.C.; Foley, L.; Jiang, Y.; Langhof, H.; Siegrist, M.; Halle, M. Health-Related Quality of Life and Physical Activity in Children and Adolescents 2 Years after an Inpatient Weight-Loss Program. J. Pediatr. 2014, 165, 732–737.e2. [Google Scholar] [CrossRef]
- Murray, M.; Pearson, J.L.; Dordevic, A.L.; Bonham, M.P. The impact of multicomponent weight management interventions on quality of life in adolescents affected by overweight or obesity: A meta-analysis of randomized controlled trials. Obes. Rev. 2019, 20, 278–289. [Google Scholar] [CrossRef]
- Peirson, L.; Douketis, J.; Ciliska, D.; Fitzpatrick-Lewis, D.; Ali, M.U.; Raina, P. Treatment for overweight and obesity in adult populations: A systematic review and meta-analysis. CMAJ Open 2014, 2, E306–E317. [Google Scholar] [CrossRef]
- Kelly, K.P.; Kirschenbaum, D.S. Immersion treatment of childhood and adolescent obesity: The first review of a promising intervention. Obes. Rev. 2011, 12, 37–49. [Google Scholar] [CrossRef]
- Poobalan, A.S.; Aucott, L.S.; Precious, E.; Crombie, I.K.; Smith, W.C.S. Weight loss interventions in young people (18 to 25 year olds): A systematic review. Obes. Rev. 2010, 11, 580–592. [Google Scholar] [CrossRef]
- Warschburger, P.; Busch, S.; Bauer, C.P.; Kiosz, D.; Stachow, R.; Petermann, F. Health-related quality of life in children and adolescents with asthma: Results from the ESTAR Study. J. Asthma 2004, 41, 463–470. [Google Scholar] [CrossRef]
- Maukonen, M.; Mannisto, S.; Tolonen, H. A comparison of measured versus self-reported anthropometrics for assessing obesity in adults: A literature review. Scand. J. Public Health 2018, 46, 565–579. [Google Scholar] [CrossRef]
| Lessons | Topic | Contents |
|---|---|---|
| 1 | Building up motivation to life-style changes | Becoming acquainted; consequences of obesity; pros and cons of changing behavior; conveying positive prospects of moderate weight loss |
| 2 | Goalsetting | Etiology of obesity; key of success: defining adequate goals, self-monitoring, commitment to behavior change; diet and physical activity; introduction of goal-diary as weekly “home-work” |
| 3 | Diet | Vicious circle of dieting and weight-cycling; questioning of common diet myths |
| 4 | Eating behavior | Self-reflection regarding eating behavior; introduction of self-control strategies (so-called “Fit-Tricks”) and building up of alternative behavior |
| 5 | Dealing with stress and everyday problems | Identifying individual triggers for eating; introduction of coping-strategies; education on advantages of regular exercising |
| 6 | Social competence | Harassment and self-assertion: ego-strength as resource, reframing stigma experiences for self-esteem stabilization |
| 7 | Parental and social support | Sharing responsibility and task distribution (parents vs. child); autonomy; asking for parental/social support; letter to the parents |
| 8 | Profession and school | Vocational choice, application, job interview; critical questions with respect to weight status; training of social competence |
| 9 | Relapse prevention | Immunization by mental anticipation of unfavorable weight course; preventing relapse; summing up of learned strategies; long-term target tracking (goal-diary, apps); farewell |
| IG (n = 141) | TAU (n = 125) | ||||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Age (years, range: 16–21) * | 17.64 | 1.10 | 17.33 | 1.12 | |
| BMI-SDS a | 2.90 | 0.54 | 2.93 | 0.45 | |
| Perceived financial security (range: 0–6) | 4.85 | 1.17 | 5.05 | 1.17 | |
| n | % | n | % | ||
| Sex | female | 97 | 68.8 | 77 | 61.6 |
| male | 44 | 31.2 | 48 | 38.4 | |
| BMI classification a | obese | 20 | 14.2 | 13 | 10.4 |
| severely obese | 118 | 83.7 | 107 | 85.6 | |
| Education b | special school | 6 | 4.5 | 8 | 6.7 |
| general/secondary/vocational school | 97 | 72.9 | 78 | 65 | |
| schools leading to the European Baccalaureate | 30 | 22.6 | 34 | 28.3 | |
| 6-Month Follow-Up | 12-Month Follow-Up | ||||
|---|---|---|---|---|---|
| Variable | ITT/PPA | ANCOVA | ANCOVA | ANCOVA | ANCOVA |
| (main effect group) | (covariate) | (main effect group) | (covariate) | ||
| BMI-SDS | ITT | MD = 0.00, | B = 0.83, SE = 0.05, | MD = −0.07, | B = 0.75, SE = 0.05, |
| F (1, 263) = 0.00, | F (1, 263) = 262.42, | F (1, 263) = 1.74, | F (1, 263) = 193.12, | ||
| p = 0.962, partial η2 < 0.001 | p < 0.001, partial η2 = 0.499 | p = 0.188, partial η2 = 0.007 | p < 0.001, partial η2 = 0.423 | ||
| PPA | MD = −0.1, | B = 1.09, SE = 0.06, | MD = −0.12, | B = 1.01, SE = 0.07, | |
| F (1, 163) = 2.25, | F (1, 163) = 305.89, | F (1, 163) = 3.17, | F (1, 163) = 236.43, | ||
| p = 0.136, partial η2 = 0.014 | p < 0.001, partial η2 = 0.652 | p = 0.077, partial η2 = 0.019 | p < 0.001, partial η2 = 0.592 | ||
| GW-QL-KJ | ITT | MD = 0.79, | B = 0.40, SE = 0.05, | MD = 1.96, | B = 0.31, SE = 0.05, |
| F (1, 263) = 0.13, | F (1, 263) = 52.95, | F (1, 263) = 0.93, | F (1, 263) = 36.08, | ||
| p = 0.715, partial η2 = 0.001 | p < 0.001, partial η2 = 0.168 | p = 0.337, partial η2 = 0.004 | p < 0.001, partial η2 = 0.121 | ||
| PPA | MD = 1.50, | B = 0.66, SE = 0.09, | MD = 1.06, | B = 0.58, SE = 0.09, | |
| F (1, 136) = 0.19, | F (1, 136) = 57.81, | F (1, 136) = 1.00, | F (1, 136) = 45.39, | ||
| p = 0.660, partial η2 = 0.001 | p < 0.001, partial η2 = 0.298 | p = 0.756, partial η2 = 0.001 | p < 0.001, partial η2 = 0.250 | ||
| Peds-QL: emotional functioning | ITT | MD = 2.24, | B = 0.34, SE = 0.05, | MD = 0.83, | B = 0.30, SE = 0.05, |
| F (1, 263) = 1.06, | F (1, 263) = 44.32, | F (1, 263) = 0.18, | F (1, 263) = 44.53, | ||
| p = 0.303, partial η2 = 0.004 | p < 0.001, partial η2 = 0.144 | p = 0.668, partial η2 = 0.001 | p < 0.001, partial η2 = 0.145 | ||
| PPA | MD = −1.94, | B = 0.58, SE = 0.08, | MD = −2.63, | B = 0.53, SE = 0.08, | |
| F (1, 135) = 0.32, | F (1, 135) = 54.53, | F (1, 135) = 0.56, | F (1, 135) = 43.14, | ||
| p = 0.575, partial η2 = 0.002 | p < 0.001, partial η2 = 0.288 | p = 0.458, partial η2 = 0.004 | p < 0.001, partial η2 = 0.242 | ||
| Peds-QL: social functioning | ITT | MD = 1.26, | B = 0.33, SE = 0.04, | MD = 1.81, | B = 0.26, SE = 0.04, |
| F (1, 263) = 0.52, | F (1, 263) = 78.92, | F (1, 263) = 0.16, | F (1, 263) = 49.89, | ||
| p = 0.472, partial η2 = 0.002 | p < 0.001, partial η2 = 0.231 | p = 0.282, partial η2 = 0.004 | p < 0.001, partial η2 = 0.159 | ||
| PPA | MD = 1.06, | B = 0.52, SE = 0.06, | MD = 0.76, | B = 0.41, SE = 0.06, | |
| F (1, 135) = 0.14, | F (1, 135) = 77.05, | F (1, 135) = 0.06, | F (1, 135) = 41.76, | ||
| p = 0.709, partial η2 = 0.001 | p < 0.001, partial η2 = 0.363 | p = 0.805, partial η2 < 0.001 | p < 0.001, partial η2 = 0.236 | ||
| Peds-QL: school functioning | ITT | MD = −3.33, | B = 0.39, SE = 0.05, | MD = 0.26, | B = 0.33, SE = 0.48, |
| F (1, 263) = 3.05, | F (1, 263) = 66.75, | F (1, 263) = 0.02, | F (1, 263) = 50.94, | ||
| p = 0.082, partial η2 = 0.011 | p < 0.001, partial η2 = 0.202 | p = 0.890, partial η2 < 0.001 | p < 0.001, partial η2 = 0.162 | ||
| PPA | MD = −6.04, | B = 0.63, SE = 0.08, | MD = −3.33, | B = 0.59, SE = 0.08, | |
| F (1, 135) = 3.71, | F (1, 135) = 66.97, | F (1, 135) = 1.09, | F (1, 135) = 57.32, | ||
| p = 0.056, partial η2 = 0.027 | p < 0.001, partial η2 = 0.332 | p = 0.300, partial η2 = 0.008 | p < 0.001, partial η2 = 0.298 | ||
| ITT | PPA | |||||||
|---|---|---|---|---|---|---|---|---|
| IG | TAU | IG | TAU | |||||
| M | SD | M | SD | M | SD | M | SD | |
| BMI-SDS | ||||||||
| T1 | 2.90 | 0.54 | 2.93 | 0.45 | 2.83 | 0.57 | 2.89 | 0.48 |
| T2 | 2.58 | 0.59 | 2.61 | 0.48 | 2.51 | 0.63 | 2.59 | 0.53 |
| T3 | 2.38 | 0.62 | 2.40 | 0.55 | 2.40 | 0.77 | 2.36 | 0.64 |
| T4 | 2.48 | 0.58 | 2.43 | 0.58 | 2.46 | 0.71 | 2.40 | 0.68 |
| GW-LQ-KJ | ||||||||
| T1 | 41.38 | 21.26 | 43.49 | 18.52 | 42.87 | 21.16 | 45.56 | 18.19 |
| T2 | 54.96 | 19.12 | 60.13 | 21.03 | 56.59 | 20.32 | 64.48 | 21.99 |
| T3 | 60.06 | 19.37 | 61.69 | 19.25 | 58.99 | 24.43 | 62.27 | 23.32 |
| T4 | 55.36 | 18.28 | 57.96 | 16.77 | 55.49 | 24.51 | 58.11 | 21.24 |
| Peds-QL: emotional | ||||||||
| T1 | 57.65 | 22.34 | 62.09 | 20.47 | 55.47 | 23.04 | 64.93 | 20.26 |
| T2 | 60.29 | 22.34 | 65.11 | 19.67 | 60.35 | 24.70 | 67.69 | 19.69 |
| T3 | 63.00 | 18.33 | 66.72 | 19.62 | 63.21 | 23.22 | 66.76 | 23.65 |
| T4 | 60.27 | 15.53 | 62.44 | 18.46 | 60.39 | 21.81 | 62.75 | 24.39 |
| Peds-QL: social | ||||||||
| T1 | 70.89 | 24.04 | 74.01 | 22.18 | 69.56 | 24.38 | 73.03 | 23.91 |
| T2 | 77.79 | 21.29 | 83.16 | 17.37 | 77.52 | 21.23 | 83.73 | 20.11 |
| T3 | 81.12 | 15.46 | 83.42 | 16.87 | 79.53 | 19.76 | 82.39 | 21.68 |
| T4 | 79.01 | 14.11 | 81.62 | 15.67 | 78.58 | 19.42 | 80.77 | 21.46 |
| Peds-QL: school | ||||||||
| T1 | 66.69 | 19.72 | 69.43 | 20.54 | 66.25 | 17.95 | 71.18 | 22.42 |
| T2 | 74.99 | 16.90 | 77.58 | 17.40 | 74.92 | 17.81 | 80.37 | 18.62 |
| T3 | 73.71 | 14.48 | 71.44 | 20.03 | 73.36 | 19.00 | 70.42 | 24.98 |
| T4 | 70.24 | 14.10 | 71.41 | 19.12 | 71.32 | 19.38 | 70.92 | 24.51 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Warschburger, P.; Zitzmann, J. Does an Age-Specific Treatment Program Augment the Efficacy of a Cognitive-Behavioral Weight Loss Program in Adolescence and Young Adulthood? Results from a Controlled Study. Nutrients 2019, 11, 2053. https://doi.org/10.3390/nu11092053
Warschburger P, Zitzmann J. Does an Age-Specific Treatment Program Augment the Efficacy of a Cognitive-Behavioral Weight Loss Program in Adolescence and Young Adulthood? Results from a Controlled Study. Nutrients. 2019; 11(9):2053. https://doi.org/10.3390/nu11092053
Chicago/Turabian StyleWarschburger, Petra, and Jana Zitzmann. 2019. "Does an Age-Specific Treatment Program Augment the Efficacy of a Cognitive-Behavioral Weight Loss Program in Adolescence and Young Adulthood? Results from a Controlled Study" Nutrients 11, no. 9: 2053. https://doi.org/10.3390/nu11092053
APA StyleWarschburger, P., & Zitzmann, J. (2019). Does an Age-Specific Treatment Program Augment the Efficacy of a Cognitive-Behavioral Weight Loss Program in Adolescence and Young Adulthood? Results from a Controlled Study. Nutrients, 11(9), 2053. https://doi.org/10.3390/nu11092053





